Abstract
Adult spinal deformity (ASD) is a very diverse condition that affects the quality of life of the involved individuals deeply. There is an ongoing discussion as to whether treatment should be surgical (which is potentially dangerous) or non-surgical.
In addition to a systematic review of literature on the surgical treatment of ASD with special emphasis on complications, a decision-analysis was performed using the patient information within a European multi-centric database of ASD.
The probabilities of improvement and complications as well as associated disease burden (utility) were calculated at the baseline and at first-year follow-up.
Decision-analysis suggests that the chances of clinical improvement are significantly higher with surgical treatment. Though surgical treatment is significantly more prone to complications, the likelihood of improvement remains higher than that offered by non-surgical treatment.
Surgical treatment of ASD appears to be associated with a higher likelihood of clinical improvement. Future work needs to focus on refining the criteria for appropriate patient selection and decreasing the incidence of complications.
Cite this article: Acaroglu E, European Spine Study Group. Decision-making in the treatment of adult spinal deformity. EFORT Open Rev 2016;1:167-176. DOI: 10.1302/2058-5241.1.000013.
Keywords: spinal deformity, adults, treatment, decision-making, complications, surgery
Adult spinal deformity (ASD) is a very complex and diverse disorder that was largely neglected until the last decade. The general reaction of healthcare providers, including surgeons, has mostly been one of denial, on the basis that this is the natural history of the spinal column and very seldom requires any treatment at all, and that even when treatment may be required, surgery should be avoided at all costs because of the risks and complications associated with it.
First, ASD is a real health problem as demonstrated by several reports. Previous work has demonstrated that this population is very non-homogeneous in terms of perceived problems as well as expectations, based on patient age as well as diagnosis.1
As an example, we may try to compare a 34-year-old woman with idiopathic scoliosis (Fig. 1a and b) with a 45-year-old male with degenerative scoliosis (Fig. 1c and d) and with a 75-year-old woman with degenerative coronal and sagittal plane deformity (Fig. 1e and f). Apparently the problems associated with these patients are fundamentally different. Furthermore, radiological parameters such as sagittal balance may well be responsible for the decreased health-related quality of life (HRQoL) in this population.2 This study by Pellise et al has also demonstrated that the deteriorative impact of ASD on HRQoL might even be larger than many other chronic health conditions that are more readily recognised as serious problems and threats.2
Fig. 1a and b.

A 34-year-old female patient presenting with a sense of progression in her deformity and mild back pain over the last three years. Her ODI score is 12%; VAS score is 2-3/10.
Fig. 1c and d.
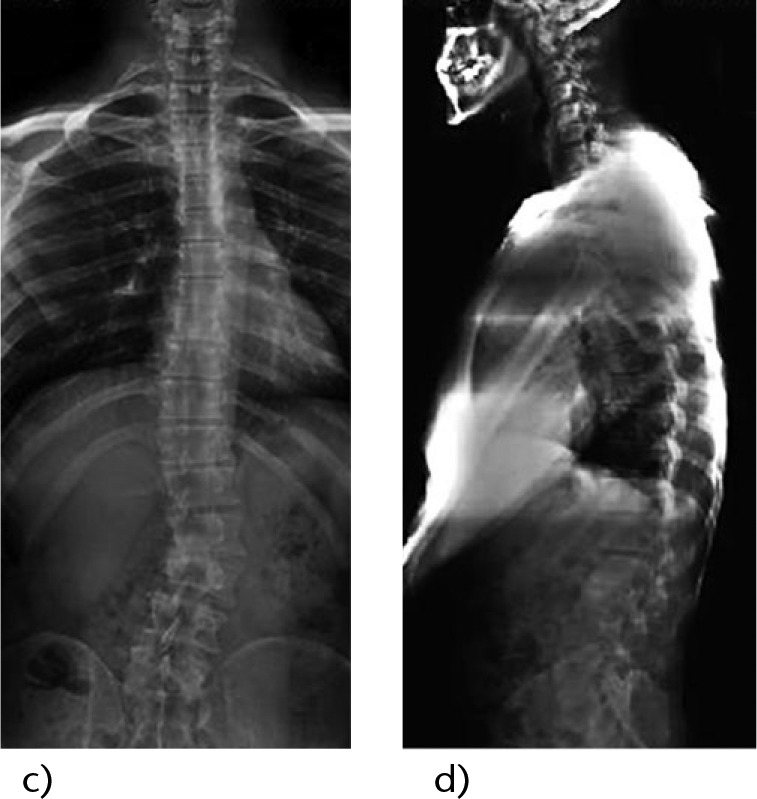
A 45-year-old male blue collar worker presenting with increasing back pain that interferes with his work and daily life over the last years. His ODI score is 25%; VAS score is 5/10.
Fig 1e and f.
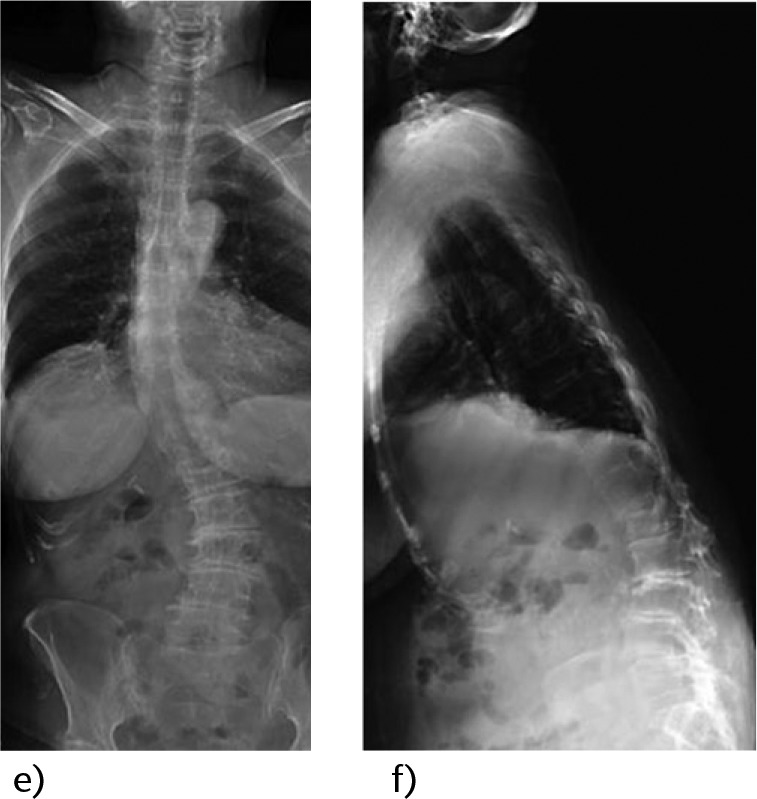
A 75-year-old female patient presenting with increasing deformity, severe back and leg pain and difficulty in walking. She has a walking capacity of 50 m, standing capacity of 4 min, ODI score of 82% and VAS score of 10/10.
ASD may occur as a result of a number of conditions, and patients may present with a different group of symptoms that are related to progressive degeneration and neural element compression. These heterogeneous symptoms and clinical presentation vary and may be related to progressive deformity, axial back pain, and/or neurological symptoms. As the percentage of elderly people in the population increases, more patients are expected to present with painful spinal conditions potentially requiring treatment. The decision between operative and non-operative treatment for ASD may be difficult for surgeons and patients. It should be based on multiple factors, including the severity of the patient’s symptoms and the potential risk of intervention. These are weighed against the potential risks and complications related to the proposed non-surgical and/or surgical treatment.3,4
The ‘ideal’ treatment for ASD is very difficult to identify with the present level of research in this field. Although this disorder is gaining recognition as a genuine health problem in an ever-ageing population, well-structured clinical trials comparing different approaches and treatment modalities are very difficult to find. A key reason for this may be the diversity of the population as mentioned above, making valid comparisons very difficult to achieve. Recognising this, several research groups have established large registries of patients, thereby making the accumulation of data and experience feasible.
In a recent systematic review of clinical studies evaluating conservative treatment, the authors concluded that because of high complication rates, surgeons mostly prefer conservative treatment for adult scoliosis patients. However, there is no consensus on the indications for conservative treatment for adult spinal deformity. Additionally, the same authors have demonstrated that current evidence is indeterminate with level IV evidence on the role of physical therapy, chiropractic treatment and bracing, and level III evidence on the use of injections for treatment of adult deformity.4 On the other hand, in a prospective multi-centre study, 160 consecutive adult scoliosis patients treated with either operative or conservative treatment were followed for two years. Quality of life measures including Oswestry Disability Index (ODI) and Scoliosis Research Society (SRS) scores and numerical back and leg pain scores were obtained. These authors reported that non-operative patients did not improve during the two-year period, whereas significant improvement in quality of life scores was detected in the operative group.5
Another problem in decision-making is the potential influence of complications on the outcomes of treatment, especially surgery. Surgery-related factors like blood loss, surgical time, length of hospital stay and length of overall recovery as well as complication rates may be increased in these patients. Analysing the results of surgery even in the larger ASD population (from 18 years of age and older) reveals that the complication rates may be even higher. These rates need to be considered as underestimations though, as younger patients should be expected to have a significantly lower number of comorbidities or other associated health problems and therefore be less prone to complications. In line with this, from a recent study of 46 patients over the age of 60 years who underwent thoracic or lumbar arthrodesis of five or more levels, with a mean follow-up of 4.2 years, it was concluded that the overall complication rate in this patient population was 37% (with a major complication rate of 20%), and patients over the age of 69 years had higher complication rates. In spite of this, clinical outcomes at final follow-up were significantly improved in ODI scores.6 Another important point in the discussion of the potential impact of complications on treatment results is, interestingly, that it is fairly common for the physicians involved in the care of patients with adult spinal deformity to assume that surgical treatment alone is associated with dire complications, and their non-surgical alternatives are immune to any adverse effects. It is correct that these complications have not been specifically investigated for this patient population but it also would be reasonable to assume that non-surgical treatments such as NSAID use, epidural and/or facet injections should be as prone to complications as when they are performed under other more common indications.
Based on these points, the two major open questions in the treatment of ASD at this time appear to be:
Which treatment modality (i.e., surgical versus non-surgical) offers higher chances of clinical improvement and lower chances of clinical deterioration?
What is the effect of treatment complications (in both surgical and non-surgical treatment) on the clinical outcomes?
The purpose of this review is to look for answers to these questions using best available evidence including recent work by the author.
What is the ‘ideal’ treatment for ASD: surgical or non-surgical?
The first thing to be discussed in this respect would be the definition of the ‘ideal’ treatment. This may be fairly dependent on the point of view of the involved people, that is, patients versus medical personnel including surgeons, versus health insurance providers. Two recent studies on a group of surgically treated ASD patients demonstrated that the perception of adverse events (and potentially treatment results) may be significantly different between patients and surgeons.7,8
Until recently, the most quantifiable aspect of treatment (radiological parameters) had been the milestone in defining the success or failure of a given treatment. On the other hand, our understanding of any health condition has now evolved into measuring the HRQoL status and/or changes provided by the treatment thereof, and this approach will be used in the definition of what is ‘ideal’.
This problem has been tackled by several authors. A systematic review by Everett and Patel on the results of non-surgical treatment failed to demonstrate any evidence better than level III for any non-surgical treatment modality.4 Bridwell and co-workers retrospectively analysed the clinical results of symptomatic adult lumbar scoliosis patients and concluded that while non-surgical treatment was hardly associated with any real change in HRQoL, surgery on the other hand provided significant improvement in this regard at two years follow-up.5 A recent study by Scheer and co-workers has investigated the effect of treatment (surgical versus non-surgical) on the quality adjusted life years (QALY) incurred by the treatment and concluded that surgical treatment provided significantly better QALYs compared to non-surgical treatment.9
Decision-analysis
We have also looked for a possible definitive answer to the problem of identifying the ideal treatment in ASD using a decision-analysis tool. From a multi-centric prospective database, the patient population consisted of a total of 535 patients who had completed the one-year follow-up, with 371 treated non-surgically and 164 treated surgically. Surgical treatment consisted of any combination of anterior and posterior surgery, fusion, instrumentation and decompression, whereas non-surgical treatment referred to follow-up under observation and/or analgesic or NSAID prescriptions in the majority of patients, with 12 out of 371 patients having been referred to a structured physical therapy programme and only six to injections or other forms of invasive treatment. All of these patients had complete radiological data in addition to records of all complications and unplanned hospitalisations as well as HRQL measures (SRS22, ODI and SF-36) taken at baseline (entry to the registry) and at six and 12 months. For the purposes of the present study, out of a bank of four years’ data collection, a 12-month set of patient data having at least one year of follow-up was used, so as to construct the decision-analysis model. Demographic characteristics as well as HRQoL data of the enrolled patients can be seen in Table 1.
Table 1.
Demographic characteristics and baseline and follow-up ODI data
| Conservative | Surgical | Total | |
|---|---|---|---|
| No. of patients in database | 630 | 338 | 968 |
| No. of patients with 1 year FU | 371 | 164 | 535 |
| Etiology of patients | |||
| Congenital | 15 | 11 | 26 |
| Degenerative | 46 | 44 | 90 |
| Idiopathic | 283 | 73 | 356 |
| Failed back | 5 | 15 | 20 |
| Neuromascular | 8 | 5 | 13 |
| Post-traumatic | 1 | 3 | 4 |
| Scheuermann | 1 | 9 | 10 |
| Syndromic | 1 | 0 | 1 |
| Other | 9 | 4 | 13 |
| Gender | |||
| Females | 315 (85 %) | 123 (75 %) | 438 (82%) |
| Males | 56 | 41 | 97 |
| Mean baseline ODI | 23.77 | 39.10 | |
| Mean 1 year ODI | 25.42 | 29.56 | |
| No. of patients with baseline and 1 year ODI measured | 309 | 123 | 432 |
| Favourable outcome (improvement of > 8 points) | 21 (6.7%) | 52 (42 %) | 73 (16.8%) |
| Unfavourable outcome (others) | 288 (93.3%) | 71 (58%) | 359 (83.2%) |
The methodology of decision-analysis consisted of investigating the likelihood (probability) of certain outcomes, for example improvement, no change or deterioration (improvement defined as a decrease in the ODI score by 8 or more points and deterioration as an increase by 8 or more points) and the burden associated with treatment quantified as the ‘utility’ of this treatment, ranging between 0 and 1.0 (0 being the highest burden, i.e. death or total paralysis; 1.0 being perfect health). These are then incorporated in a decision tree that demonstrates the QALY associated with each possible outcome.
The results of this study demonstrated that the likelihood of improvement was significantly higher for patients treated surgically, compared to those treated non-surgically (Table 2; Table 4) to the extent that the likelihood of improvement in the ODI score was 54.2% in the surgical group compared to the 9.7% in the non-surgical group. It can easily be argued that this is to be expected, after all, as most patients in the non-surgical groups tend to be patients who did not receive any significant treatment at all; how can we expect them to get better by themselves? This argument being very accurate, the more interesting finding in this analysis was the probability of ending up with significant deterioration by the end of the first year post-treatment. As can be seen in Table 2, unexpectedly, the probability of deterioration appears to be higher in the non-surgical group. As a summary at this stage, we can say that surgical treatment of ASD results in a significantly higher probability of improvement, and a lesser chance of deterioration.
Table 2.
Overall treatment results of the entire study population regardless of complications, diagnosis, patient age and pre-treatment level of disability
| Treatment | N | Deterioration | No change | Improvement |
|---|---|---|---|---|
| Surgical | 161 | 11 (9.2%) | 44 (36.7%) | 65 (54.2%) |
| Non-surgical | 311 | 54 (13.4%) | 311 (77.0%) | 39 (9.7%) |
For the definitions of improvement, no change and deterioration, please see text.
Table 4.
Baseline and final utilities and final QALE for a) patients aged > = 50 years, b) patients aged < 50 years, c) degenerative deformity, d) idiopathic deformity, and e) patients with baseline ODI>25
| Treatment | Baseline utility | Final utility | p value (baseline vs final) | QALE* (healthy years) |
|---|---|---|---|---|
| a) Patient age > = 50 years | ||||
| Surgical | 0.532 | 0.581 | 0.002 | 58 |
| Non-surgical | 0.605 | 0.618 | 0.192 | 62 |
| p value | <0.0001 | 0.040 | 0.040 | |
| b) Patient age < 50 years | ||||
| Surgical | 0.593 | 0.679 | 0.001 | 68 |
| Non-surgical | 0.646 | 0.677 | 0.752 | 68 |
| p value | <0.0001 | 0.078 | 0.078 | |
| c) Degenerative etiology | ||||
| Surgical | 0.409 | 0.579 | <0.001 | 58 |
| Non-surgical | 0.532 | 0.544 | 0.746 | 54 |
| p value | 0.015 | 0.384 | 0.384 | |
| d) Idiopathic etiology | ||||
| Surgical | 0.496 | 0.66 | <0.001 | 66 |
| Non-surgical | 0.619 | 0.63 | 0.666 | 63 |
| p value | <0.001 | 0.201 | 0.201 | |
| e) Patients with base ODI > 25 | ||||
| Surgical | 0.544 | 0.581 | 0.002 | 58 |
| Non-surgical | 0.543 | 0.556 | 0.088 | 56 |
| p value | 0.934 | 0.1010 | 0.1010 | |
Default life expectancy accepted as 100; thereby the QALE = final utility *100
It has to be kept in mind, though, that another very important facet of this discussion is the burden associated with these treatment modalities. If the burden associated with surgery is much higher than that of non-surgical treatment, and the procedure itself (and the follow-up) does not effectively decrease this burden, one may argue that the higher rates of improvement can only be achieved with considerable suffering. This is a valid argument and we have to revert to the utility part of decision-analysis in order to provide an accurate answer to it. As described above, ‘utility’ is a measure of the burden of any disease at a given time (as it is mapped from SF36), and may range between 0 (extremely bad health, death or total paralysis by definition) and 1.0 (perfect health). Tables 3 and 4 summarise the utilities calculated for the general population (Table 3) and for specific subsets based on age, disability level at the time of enrolment and diagnosis (Table 4).
Table 3.
Baseline and final utilities and final QALE for an entire patient population
| Treatment | Baseline utility | Final utility | p value (baseline vs final) | QALE* (healthy years) |
|---|---|---|---|---|
| Surgical | 0.56 | 0.60 | <0.0001 | 60 |
| Non-surgical | 0.65 | 0.65 | 0.2692 | 65 |
| p value | <0.0001 | 0.0038 | 0.0038 |
Default life expectancy accepted as 100; thereby the QALE = final utility *100
As can be seen from this study, it appears that the surgical group started with a significantly higher burden compared to the non-surgical, and finished with a significantly higher burden at the first year. But it is only in this group that the burden of the disease could be significantly decreased, while the overall disease burden in the non-surgical group had not changed. In the light of these results, returning to the discussion referred to above, we can conclude that at the end of the follow-up period, surgical patients carried a higher burden of disease compared to non-surgical patients, but this disadvantage has probably been decreased from a significantly higher proportion to a lesser (but still significant) proportion.
In summary, analysis of the relevant literature as well as the decision-analysis suggests that surgery may be more akin to being the ‘ideal’ treatment for ASD compared to non-surgical treatment. But then, this may lead to a subsequent set of questions on identifying the sub-populations in whom there may be differences; for example could surgery be associated with a higher burden in the older population? Should it be reserved for the relatively younger patients as a result? What about patients with significant disability at the time of presentation - does surgery help them at all? What about the degenerative deformity patients compared with those with so-called idiopathic deformity?
Table 4 summarises the answers to these questions based on the decision-analysis performed. As can be expected, older patients had been presenting with a higher burden but ended up at a significantly improved and almost similar burden level to the group of patients who had surgical treatment. Non-surgical patients did not demonstrate any significant changes in time regardless of their age group (Table 4a and b). A recent study by Sciubba and co-workers has also reported similar findings in regard to the outcomes of surgical or non-surgical treatment in patients over 75 years of age, and concluded “in elderly patients greater than 75 years of age, reconstructive surgery provides significant improvements in pain and disability over a two-year period. Furthermore, surgically treated patients were more likely to reach MCID than non-operative patients”.10
When analysed for the effect of diagnosis (degenerative deformity versus idiopathic) it was seen that an almost similar pattern arises here as well, with the exception that in both sub-groups, surgical treatment not only provided significant decreases in disease burden but also a better level at the end of the follow-up (Table 4c and d). Finally for patients with significant disability at the time of enrolment (defined as ODI > 25%), it was seen that although both groups had started the treatment at the same level of disease burden, significant improvement could only be achieved in the surgical group and, in fact, this group had achieved a better (although not significant) burden level at the end of the follow-up period (Table 4e). Based on these findings, we can state that under the light of current evidence (level III), surgical treatment of ASD appears to yield a better chance in terms of both the HRQoL and overall disease burden, albeit being associated with a higher burden at time points at both ends.
To what extent do the complications affect outcomes?
Complications have always been the major concern with regard to any treatment modality in ASD, and have very commonly been defined as a major parameter in decision-making. As discussed above, interestingly, when treatment complications are evaluated, most care providers and decision-makers think of the complications of surgical treatment and very commonly visualise non-surgical treatments (including observation) as devoid of any adverse effects and/or complications. As this is probably not the case, we tend to think that a more holistic approach, following up both surgically- and non-surgically-treated patients, and reporting all complications and their effects on the outcomes, is needed.
In order to achieve this and understand the magnitude of the problem of complications, a critical review of literature pertaining to ASD with special emphasis to treatment complications was performed as an integral component of our decision-analysis. A computerised query of the PubMed and Scopus databases was performed to identify any articles published between 1950 and 2014 that were pertinent to the aforementioned clinical questions. An initial search using the keywords ‘adult spine deformity’, ‘adult spine deformity surgery’, ‘adult spine surgery complications’, ‘adult scoliosis’, ‘adult scoliosis surgery’ and ‘adult scoliosis surgery complications’ was performed. This query provided 8441 potentially applicable studies. We restricted our work by using only English language articles and clinical studies. Based on this, after all abstracts were reviewed, 149 articles were selected for detailed review. In the full text assessment, we excluded studies which include case reports, small series (< 20 patients reported), single anatomical region deformity studies, revision case series, series in which complication incidences and results were not clearly documented and studies which did not meet the inclusion criteria. Additionally, review articles were excluded if they did not add significantly over an ‘expert opinion’ level of evidence. Using these criteria, 98 studies were excluded and 52 studies were identified so as to be evaluated for a detailed review of methodology and results.6,11-61 For each article, the study design (retrospective or prospective), year of publication, number of patients, mean patient age, mean follow-up, complication types (pre-op, intra-op and post-op) and incidences were analysed and noted. In addition, clinical outcome data, based on complications that can be classified as life-threatening (LT)/non-life-threatening (NLT) or major/minor, were also recorded when available. Of the 52 studies that met inclusion criteria, none were randomised controlled trials; the majority were retrospective database case series, and all were on surgical treatment. Summarised cumulative probabilities for LT and NLT complications from these studies and specifically from studies that were selected as focussing on complications29,52,55,58 can be viewed in Table 5. As can be seen, there is a very wide variance in the incidences reported, especially with regard to pseudoarthrosis and implant failures (ranging between 0.5% and 54.0%).
Table 5.
The probability table for life-threatening (LT) and non-life-threatening (NLT) complications obtained through the systematic review of the literature for surgical intervention
| All studies |
Specific studies on complications |
||
|---|---|---|---|
| Complication | Type | Median (Min-Max) | Median |
| Death | - | 0.25% (0.0% - 2.2%) | 0 |
| Myocardial infarction | LT | 1.20% (0.0% - 9.5%) | 0.6 % |
| Neurological loss | LT | 1.78% (0.1% - 12.5%) | 1.7 % |
| Deep infection | LT | 4.19% (0.3% - 19.0%) | 3.5% |
| Upper GI bleeding | NLT | 3.44% (2.1% - 4.8%) | Not reported |
| Stroke | NLT | 5.00% (0.0% - 10.0%) | Not reported |
| ARDS | LT | 4.24% (1.3% - 7.8%) | Not reported |
| PE | LT | 1.22% (0.1% - 9.5%) | 0.7% |
| Systemic infection/Sepsis | LT | 1.66% (0.0% - 11.4%) | Not reported |
| Combined probability LT | 2.61 (0.0% - 19.0%) | 1.64% | |
| DVT | NLT | 2.00% (0.0% - 7.3%) | 2% |
| Pseudoarthrosis/Implant failure | NLT | 3.15% (0.5% - 54.0%) | 12.40% |
| CSF leak, Fistula | NLT | 4.67% (0.3% - 15.0%) | 1.38 % |
| Nerve root | NLT | 1.66% (0.1% - 6.7%) | 2.28% |
| Combined probability NLT | 2.58% (0.3% - 54.0%) | 2.28% (0.9%-24.4%) |
Apart from these, three recent papers have specifically reported on the effects of complications on treatment outcomes. Daubs et al have investigated the complications and outcomes of 46 patients over the age of 60 years, who underwent thoracic or lumbar arthrodesis of five or more levels, with a mean follow-up of 4.2 years. They concluded that the overall complication rate in this patient population was 37% (with a major complication rate of 20%), and patients over the age of 69 years had yet higher complication rates. In spite of this, clinical outcomes at final follow-up were significantly improved in ODI scores.6 Glassman et al have also reported on the effect of treatment complications on 46 adult deformity patients undergoing surgery. There were 47 major and 62 minor complications, and it was seen that major complications had adversely affected the outcome as evidenced by the SF12 general health scores at one year follow-up.55 In another study, Scheer et al have investigated the effect of complication on the recovery of patients using an integrated health score (IHS) and concluded, “[T]here was a significantly protracted mental recovery phase associated with patients that had at least one complication, as well as either a minor and major complication. The addition of a reoperation also adversely affected the mental recovery as well as overall satisfaction”.62 Likewise, a study by Ayhan et al focusing on spinal osteotomies in ASD patients demonstrated that complications do not necessarily affect the clinical outcomes in this sub-population of patients.63 It needs to be noted that, again, both of these studies as well as the studies referred to above have not compared the treatment modalities for complications. That being the status of the available base of knowledge, the second part of our decision-analysis was performed with the specific questions of whether complications affect the outcomes of treatment and if so, to what extent.
Using the same patient population and methodology described above, it was seen that in this group of 535 patients (371 non-surgical, 164 surgical), there were 78 (14.6%) NLT 12 (2.2%) LT complications and three (0.6%) deaths/paralyses (1 death, 2 patients with total paralysis). Surgical treatment was significantly more prone to complications (31.7% versus 11.1%, p < 0.001) (Table 6). In addition, as can be expected, the rate of LT was much higher in patients treated surgically (p < 0.001) and there were no deaths or progression to paralysis in the non-surgical group. Based on these findings we can conclude that although non-surgical treatment is also associated with complications, surgical treatment of ASD is more prone to complications in general and much more prone to major and devastating complications.
Table 6.
Incidences of complications in surgical and non-surgical patient groups
| Complications | Surgical n (%) | Non-surgical n (%) | Total n (%) |
|---|---|---|---|
| None | 112 (68.3) | 330 (89.0) | 442 (82.6) |
| NLT | 39 (23.8) | 39 (10.5) | 78 (14.6) |
| LT | 10 (6.1) | 2 (0.5) | 12 (2.2) |
| Death | 3 (1.8) | 0 | 3 (0.6) |
| TOTAL | 52 (31.7) | 41 (11.1) | 535 |
NLT = non-life threatening complications; LT= life-threatening complications; Death = death or paralysis.
Clinical outcomes of patient groups stratified by complications can be seen in Table 7. These findings are important in underlining that for patients who had surgical treatment, complications do have an effect on the clinical outcomes. The probability of improvement decreases by the presence of complications, especially if these complications are LT whereas likewise, the probability of clinical deterioration increases with the presence and severity of complications. On the other hand, on the non-surgical side we see that the presence and/or severity of complications have little if any effect on clinical outcomes (with the exception of LT complications which is a statistical error secondary to less populated cells).
Table 7.
Overall treatment results of the entire study population grouped by complications regardless of diagnosis, patient age and pre-treatment level of disability
| Surgical |
Non-surgical |
|||||||
|---|---|---|---|---|---|---|---|---|
| N | Deterioration | No change | Improvement | N | Deterioration | No change | Improvement | |
| None | 112 | 8 (9.4%) | 27 (31.8%) | 50 (58.8%) | 330 | 47(17.5%) | 184 (68.7%) | 37 (13.8%) |
| NLT | 39 | 2 (7.4%) | 13 (48.1%) | 12 (44.4%) | 39 | 6 (15.4%) | 26 (66.7%) | 2 (17.9%) |
| LT | 10 | 1 (12.5%) | 4 (50%) | 3 (37.5%) | 2 | 1 (50%) | 1 (50%) | 0 |
For the definitions of improvement, no change and deterioration please see text.
Finally, the utilities and associated QALY values for all possible outcomes (that is, three possible clinical outcomes, two groups and three potential complication statuses) can be seen in Table 8.
Table 8.
Final table with clinical outcomes in three categories and probabilities and utilities associated with these outcomes
| Outcomes group/complication | Utilities (range) | QALE |
|---|---|---|
| Deterioration | ||
| Surgical/No complication | 0.57 (0.41-0.66) | 57 |
| Surgical/ NLT complication | 0.58 (0.56-0.59) | 58 |
| Surgical/ LT complication | 0.38 (-) | 38 |
| Non-surgical/No complication | 0.54 (0.33-0.79) | 54 |
| Non-surgical/NLT complication | 0.40 (0.30-0.54) | 40 |
| Non-surgical/LT complication | - | - |
| No change | ||
| Surgical/No complication | 0.65 (0.41-0.85) | 65 |
| Surgical/ NLT complication | 0.62 (0.45-0.87) | 62 |
| Surgical/ LT complication | 0.49 (0.38-0.58) | 49 |
| Non-surgical/No complication | 0.68 (0.36-0.97) | 68 |
| Non-surgical/NLT complication | 0.70 (0.37-0.97) | 70 |
| Non-surgical/LT complication | - | - |
| Improvement | ||
| Surgical/No complication | 0.62 (0.36-0.88) | 62 |
| Surgical/ NLT complication | 0.63 (0.40-0.89) | 63 |
| Surgical/ LT complication | 0.61 (0.59-0.64) | 61 |
| Non-surgical/No complication | 0.62 (0.40-0.89) | 62 |
| Non-surgical/NLT complication | 0.61 (0.40-0.85) | 61 |
| Non-surgical/LT complication | - | - |
Based on this, it can be seen that the LT complications in particular add a very heavy burden for the involved patients in both groups. This burden is even heavier in patients who had experienced deterioration, and in this regard it might be more reasonable to state that the presence of LT complications may have played an integral role in the clinical deterioration of these patients.
Based on these findings we can state that any treatment in ASD is prone to complications, and complications can affect surgical outcomes adversely. Patients with complications have a decreased likelihood of getting better compared to those with no complications, and they carry a heavier burden of the disease; potentially even heavier than their baseline status. Specifically, surgical treatment is significantly more prone to complications and therefore the above-mentioned effects of complications are probably more pronounced in the surgical patients. On the other hand, when we compare the probability of getting clinically better at the end of the first year of treatment between the surgical and non-surgical patients, we can see that surgical patients who had encountered complications during their treatment still have a higher chance of improvement compared to their non-surgical counterparts.
Conclusions
In summary, the end result of the decision-analysis study suggests that the two facets of treatment outcomes, improvement versus no change/deterioration and the burden of the disease (utilities) may affect the eventual decision-making in different directions. When we look at the probability of getting better by treatment, surgery appears to be the obvious treatment of choice. On the other hand, surgery is more prone to complications (which affect the outcome) and associated with a heavier treatment burden as well. Stated in a different way, analysis of the results of this study as well as the others in the literature enables the drawing of several conclusions:
Treatment of ASD is prone to complications; more so in surgical treatment (31.7%) than non-surgical treatment (11.1%).
These complications affect the clinical outcomes of treatment regardless of whether it is surgical or non-surgical. However, as the complication rate is higher in the surgical group, this effect may be more pronounced.
Further, complications are associated with a heavier disease burden. This burden may be even heavier in surgical patients who were found to start the treatment with significantly higher burdens.
On the other hand, it appears that only surgical treatment can decrease the burden of this specific medical condition.
The chance of improvement following treatment is significantly higher in patients who have undergone surgery. This effect is more pronounced in patients without any complications but still persists in those who have had complications as well.
Future directions
Although the level of evidence is not beyond level III, all controlled and non-controlled studies on the treatment of ASD uniformly suggest that at this point in time, surgical treatment may provide better chances of improvement when compared with non-surgical treatment. That being said, much work needs to be done to improve our understanding of ASD and how to evaluate and treat patients with this condition. In this regard, future work should focus on:
Investigating non-surgical treatment modalities that may effectively change the natural history of the disease for longer periods of time, if not permanently.
Providing better definition of surgical indications. Which sets/subsets of patients benefit more from surgery? What type of surgery for whom?
Providing a better definition of the timing of surgery/interventions. When is a good time for a patient with ASD and clinical disability to have treatment, rather than leaving the patient to the natural history of the disease?
- Establishing means to decrease the rate of complications radically. In order to achieve this goal:
- − We need to identify patients who would be more prone to complications with certain treatment modalities and divert these patients to other treatment modalities.
- − We need to stratify our patients for their risks and interventions for their aggressiveness so as to be able to match them.
- − We need to keep on working on new surgical technologies that would improve patient safety and decrease complications. The priority in this regard may be developing new fusion and implant technologies as the rates of mechanical failure are still unacceptably high in ASD.
Acknowledgments
The authors extend their gratitude to all those who contributed to the decision-analysis project: Umit Ozgur Guler MD, Aysun Cetinyurek-Yavuz PhD, Selcen Yuksel PhD and Yasemin Yavuz PhD.
Footnotes
Note on the authors: In addition to Emre Acaroglu, the European Spine Study Group consists of Ahmet Alanay MD, Ferran Pellise MD and Francesco Sanchez Perez-Grueso MD as executive members, and Frank Kleinstück MD and Ibrahim Obeid MD as core members.
Conflict of Interest: The ESSG is funded by a research grant from Depuy Synthes.
Funding
The decision-analysis project referred to in this manuscript was funded by the Spine Society of Europe (Eurospine).
References
- 1. Acaroglu E, Guler UO, Olgun DZ, et al. ; European Spine Study Group. Multiple regression analysis of factors affecting HRQL in adult spinal deformity (ASD). Spine Deformity 2015;3:360-6. [DOI] [PubMed] [Google Scholar]
- 2. Pellisé F, Vila-Casademunt A, Ferrer M, et al. ; European Spine Study Group, ESSG. Impact on health related quality of life of adult spinal deformity (ASD) compared with other chronic conditions. Eur Spine J 2015;24:3-11. [DOI] [PubMed] [Google Scholar]
- 3. Good CR, Auerbach JD, O’Leary PT, Schuler TC. Adult spine deformity. Curr Rev Musculoskelet Med 2011;4:159-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Everett CR, Patel RK. A systematic literature review of nonsurgical treatment in adult scoliosis. Spine (Phila Pa 1976) 2007;32:S130-S134. [DOI] [PubMed] [Google Scholar]
- 5. Bridwell KH, Glassman S, Horton W, et al. Does treatment (nonoperative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: a prospective multicenter evidence-based medicine study Spine (Phila Pa 1976) 2009;34:2171-8. [DOI] [PubMed] [Google Scholar]
- 6. Daubs MD, Lenke LG, Cheh G, Stobbs G, Bridwell KH. Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine (Phila Pa 1976) 2007;32:2238-44. [DOI] [PubMed] [Google Scholar]
- 7. Hart RA, Cabalo A, Bess S, et al. ; International Spine Study Group. Comparison of patient and surgeon perceptions of adverse events after adult spinal deformity surgery. Spine (Phila Pa 1976) 2013;38:732-6. [DOI] [PubMed] [Google Scholar]
- 8. Roitberg BZ, Thaci B, Auffinger B, et al. Comparison between patient and surgeon perception of degenerative spine disease outcomes–a prospective blinded database study. Acta Neurochir (Wien) 2013;155:757-64. [DOI] [PubMed] [Google Scholar]
- 9. Scheer JK, Hostin RA, Schwab F, et al. ; International Spine Study Group. Operative Management of Adult Spinal Deformity Results in Significant Increases in QALYs Gained Compared With Nonoperative Management: Analysis of 479 Patients With Minimum 2-Year Follow-up. http://journals.lww.com/neurosurgery/_layouts/15/oaks.journals.mobile/articleviewer.aspx?year=2015&issue=08001&article=00109 (date last accessed 16 February 2016). [DOI] [PubMed]
- 10. Sciubba DM, Scheer JK, Yurter A, et al. , The International Spine Study Group (ISSG). Patients with spinal deformity over the age of 75: a retrospective analysis of operative versus non-operative management. Eur Spine J 2015. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 11. Bekelis K, Desai A, Bakhoum SF, Missios S. A predictive model of complications after spine surgery: the National Surgical Quality Improvement Program (NSQIP) 2005-2010. Spine J 2014;14:1247-55. [DOI] [PubMed] [Google Scholar]
- 12. McCormack RA, Hunter T, Ramos N, et al. An analysis of causes of readmission after spine surgery. Spine (Phila Pa 1976) 2012;37:1260-6. [DOI] [PubMed] [Google Scholar]
- 13. Hellsten EK, Hanbidge MA, Manos AN, et al. An economic evaluation of perioperative adverse events associated with spinal surgery. Spine J 2013;13:44-53. [DOI] [PubMed] [Google Scholar]
- 14. Bridwell KH, Baldus C, Berven S, et al. Changes in radiographic and clinical outcomes with primary treatment adult spinal deformity surgeries from two years to three- to five-years follow-up. Spine (Phila Pa 1976) 2010;35:1849-54. [DOI] [PubMed] [Google Scholar]
- 15. Hassanzadeh H, Jain A, El Dafrawy MH, et al. Clinical results and functional outcomes in adult patients after revision surgery for spinal deformity correction: patients younger than 65 years versus 65 years and older. Spine Deform 2013;1:371-6. [DOI] [PubMed] [Google Scholar]
- 16. Hassanzadeh H, Jain A, El Dafrawy MH, et al. Clinical results and functional outcomes of primary and revision spinal deformity surgery in adults. J Bone Joint Surg [Am] 2013;95-A:1413-19. [DOI] [PubMed] [Google Scholar]
- 17. Booth KC, Bridwell KH, Lenke LG, Baldus CR, Blanke KM. Complications and predictive factors for the successful treatment of flatback deformity (fixed sagittal imbalance). Spine (Phila Pa 1976) 1999;24:1712-20. [DOI] [PubMed] [Google Scholar]
- 18. Yagi M, Patel R, Boachie-Adjei O. Complications and unfavorable clinical outcomes in obese and overweight patients treated for adult lumbar or thoracolumbar scoliosis with Combined anterior/posterior surgery. J Spinal Disord Tech 2013;28:E368-E376. [DOI] [PubMed] [Google Scholar]
- 19. Cho KJ, Suk SI, Park SR, et al. Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine (Phila Pa 1976) 2007;32:2232-7. [DOI] [PubMed] [Google Scholar]
- 20. Rihn JA, Radcliff K, Hilibrand AS, et al. Does obesity affect outcomes of treatment for lumbar stenosis and degenerative spondylolisthesis? Analysis of the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976) 2012;37:1933-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kasliwal MK, Smith JS, Shaffrey CI, et al. Does prior short-segment surgery for adult scoliosis impact perioperative complication rates and clinical outcome among patients undergoing scoliosis correction? J Neurosurg Spine 2012;17:128-33. [DOI] [PubMed] [Google Scholar]
- 22. Schoenfeld AJ, Herzog JP, Dunn JC, Bader JO, Belmont PJ., Jr Patient-based and surgical characteristics associated with the acute development of deep venous thrombosis and pulmonary embolism after spine surgery. Spine (Phila Pa 1976) 2013;38:1892-8. [DOI] [PubMed] [Google Scholar]
- 23. Yadla S, Malone J, Campbell PG, et al. Early complications in spine surgery and relation to preoperative diagnosis: a single-center prospective study. J Neurosurg Spine 2010;13:360-6. [DOI] [PubMed] [Google Scholar]
- 24. Cloyd JM, Acosta FL, Jr, Cloyd C, Ames CP. Effects of age on perioperative complications of extensive multilevel thoracolumbar spinal fusion surgery. J Neurosurg Spine 2010;12:402-8. [DOI] [PubMed] [Google Scholar]
- 25. Masuda K, Chikuda H, Yasunaga H, et al. Factors affecting the occurrence of pulmonary embolism after spinal surgery: data from the national administrative database in Japan. Spine J 2012;12:1029-34. [DOI] [PubMed] [Google Scholar]
- 26. Hartin NL, Mehbod AA, Joglekar SB, Transfeldt EE. Fusion risk score: evaluating baseline risk in thoracic and lumbar fusion surgery. Spine (Phila Pa 1976) 2013;38:E1616-E1623. [DOI] [PubMed] [Google Scholar]
- 27. Schairer WW, Carrer A, Deviren V, et al. Hospital readmission after spine fusion for adult spinal deformity. Spine (Phila Pa 1976) 2013;38:1681-9. [DOI] [PubMed] [Google Scholar]
- 28. Fineberg SJ, Ahmadinia K, Patel AA, Oglesby M, Singh K. Incidence and mortality of cardiac events in lumbar spine surgery. Spine (Phila Pa 1976) 2013;38:1422-9. [DOI] [PubMed] [Google Scholar]
- 29. Pull ter Gunne AF, van Laarhoven CJ, Cohen DB. Incidence of surgical site infection following adult spinal deformity surgery: an analysis of patient risk. Eur Spine J 2010;19:982-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pull ter Gunne AF, Cohen DB. Incidence, prevalence, and analysis of risk factors for surgical site infection following adult spinal surgery. Spine (Phila Pa 1976) 2009;34:1422-8. [DOI] [PubMed] [Google Scholar]
- 31. Guerin P, El Fegoun AB, Obeid I, et al. Incidental durotomy during spine surgery: incidence, management and complications. A retrospective review. Injury 2012;43:397-401. [DOI] [PubMed] [Google Scholar]
- 32. Lapp MA, Bridwell KH, Lenke LG, et al. Long-term complications in adult spinal deformity patients having combined surgery a comparison of primary to revision patients. Spine (Phila Pa 1976) 2001;26:973-83. [DOI] [PubMed] [Google Scholar]
- 33. Jo DJ, Jun JK, Kim KT, Kim SM. Lumbar interbody fusion outcomes in degenerative lumbar disease : comparison of results between patients over and under 65 years of age. J Korean Neurosurg Soc 2010;48:412-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Röllinghoff M, Schlüter-Brust K, Groos D, et al. Mid-range outcomes in 64 consecutive cases of multilevel fusion for degenerative diseases of the lumbar spine. Orthop Rev (Pavia) 2010;2:e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Acosta FL, Jr, McClendon J, Jr, O’Shaughnessy BA, et al. Morbidity and mortality after spinal deformity surgery in patients 75 years and older: complications and predictive factors. J Neurosurg Spine 2011;15:667-74. [DOI] [PubMed] [Google Scholar]
- 36. Bhagat S, Vozar V, Lutchman L, Crawford RJ, Rai AS. Morbidity and mortality in adult spinal deformity surgery: Norwich Spinal Unit experience. Eur Spine J 2013;22:S42-S46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Fu KM, Smith JS, Polly DW, Jr, et al. Morbidity and mortality in the surgical treatment of 10,329 adults with degenerative lumbar stenosis. J Neurosurg Spine 2010;12:443-6. [DOI] [PubMed] [Google Scholar]
- 38. Sansur CA, Reames DL, Smith JS, et al. Morbidity and mortality in the surgical treatment of 10,242 adults with spondylolisthesis. J Neurosurg Spine 2010;13:589-93. [DOI] [PubMed] [Google Scholar]
- 39. Campbell PG, Yadla S, Nasser R, et al. Patient comorbidity score predicting the incidence of perioperative complications: assessing the impact of comorbidities on complications in spine surgery. J Neurosurg Spine 2012;16:37-43. [DOI] [PubMed] [Google Scholar]
- 40. Schoenfeld AJ, Carey PA, Cleveland AW, III, Bader JO, Bono CM. Patient factors, comorbidities, and surgical characteristics that increase mortality and complication risk after spinal arthrodesis: a prognostic study based on 5,887 patients. Spine J 2013;13:1171-9. [DOI] [PubMed] [Google Scholar]
- 41. Carreon LY, Puno RM, Dimar JR, II, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg [Am] 2003;85-A:2089-92. [DOI] [PubMed] [Google Scholar]
- 42. Raffo CS, Lauerman WC. Predicting morbidity and mortality of lumbar spine arthrodesis in patients in their ninth decade. Spine (Phila Pa 1976) 2006;31:99-103. [DOI] [PubMed] [Google Scholar]
- 43. Pateder DB, Gonzales RA, Kebaish KM, et al. Pulmonary embolism after adult spinal deformity surgery. Spine (Phila Pa 1976) 2008;33:301-5. [DOI] [PubMed] [Google Scholar]
- 44. Hamilton DK, Smith JS, Sansur CA, et al. ; Scoliosis Research Society Morbidity and Mortality Committee. Rates of new neurological deficit associated with spine surgery based on 108,419 procedures: a report of the scoliosis research society morbidity and mortality committee. Spine (Phila Pa 1976) 2011;36:1218-28. [DOI] [PubMed] [Google Scholar]
- 45. Guyot JP, Cizik A, Bransford R, Bellabarba C, Lee MJ. Risk factors for cardiac complications after spine surgery. Evid Based Spine Care J 2010;1:18-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Schoenfeld AJ, Ochoa LM, Bader JO, Belmont PJ., Jr Risk factors for immediate postoperative complications and mortality following spine surgery: a study of 3475 patients from the National Surgical Quality Improvement Program. J Bone Joint Surg [Am] 2011;93-A:1577-1582. [DOI] [PubMed] [Google Scholar]
- 47. Schwab FJ, Hawkinson N, Lafage V, et al. ; International Spine Study Group. Risk factors for major peri-operative complications in adult spinal deformity surgery: a multi-center review of 953 consecutive patients. Eur Spine J 2012;21:2603-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Lee MJ, Hacquebord J, Varshney A, et al. Risk factors for medical complication after lumbar spine surgery: a multivariate analysis of 767 patients. Spine (Phila Pa 1976) 2011;36:1801-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lee MJ, Konodi MA, Cizik AM, et al. Risk factors for medical complication after spine surgery: a multivariate analysis of 1,591 patients. Spine J 2012;12:197-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Baker GA, Cizik AM, Bransford RJ, et al. Risk factors for unintended durotomy during spine surgery: a multivariate analysis. Spine J 2012;12:121-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Pateder DB, Gonzales RA, Kebaish KM, et al. Short-term mortality and its association with independent risk factors in adult spinal deformity surgery. Spine (Phila Pa 1976) 2008;33:1224-8. [DOI] [PubMed] [Google Scholar]
- 52. Blamoutier A, Guigui P, Charosky S, Roussouly P, Chopin D; Groupe d’Étude de la Scoliose (GES). Surgery of lumbar and thoracolumbar scolioses in adults over 50. Morbidity and survival in a multicenter retrospective cohort of 180 patients with a mean follow-up of 4.5 years. Orthop Traumatol Surg Res 2012;98:528-35. [DOI] [PubMed] [Google Scholar]
- 53. Abdul-Jabbar A, Takemoto S, Weber MH, et al. Surgical site infection in spinal surgery: description of surgical and patient-based risk factors for postoperative infection using administrative claims data. Spine (Phila Pa 1976) 2012;37:1340-5. [DOI] [PubMed] [Google Scholar]
- 54. Mannion AF, Fekete TF, O’Riordan D, et al. The assessment of complications after spine surgery: time for a paradigm shift? Spine J 2013;13:615-24. [DOI] [PubMed] [Google Scholar]
- 55. Glassman SD, Hamill CL, Bridwell KH, et al. The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976) 2007;32:2764-70. [DOI] [PubMed] [Google Scholar]
- 56. Wu JC, Chen YC, Liu L, et al. The risk of stroke after spinal fusion surgery: a national cohort study. Spine J 2012;12:492-9. [DOI] [PubMed] [Google Scholar]
- 57. Lonergan T, Place H, Taylor P. Acute complications following adult spinal deformity surgery in patients aged 70 years and older. J Spinal Disord Tech 2012. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 58. Charosky S, Guigui P, Blamoutier A, Roussouly P, Chopin D; Study Group on Scoliosis. Complications and risk factors of primary adult scoliosis surgery: a multicenter study of 306 patients. Spine (Phila Pa 1976) 2012;37:693-700. [DOI] [PubMed] [Google Scholar]
- 59. Auerbach JD, Lenke LG, Bridwell KH, et al. Major complications and comparison between 3-column osteotomy techniques in 105 consecutive spinal deformity procedures. Spine (Phila Pa 1976) 2012;37:1198-1210. [DOI] [PubMed] [Google Scholar]
- 60. Patel N, Bagan B, Vadera S, et al. Obesity and spine surgery: relation to perioperative complications. J Neurosurg Spine 2007;6:291-7. [DOI] [PubMed] [Google Scholar]
- 61. Drazin D, Shirzadi A, Rosner J, et al. Complications and outcomes after spinal deformity surgery in the elderly: review of the existing literature and future directions. Neurosurg Focus 2011;31:E3. [DOI] [PubMed] [Google Scholar]
- 62. Scheer JK, Mundis GM, Klineberg E, et al. ; International Spine Study Group (ISSG). Recovery following adult spinal deformity surgery: the effect of complications and reoperation in 149 patients with 2-year follow-up.). Eur Spine J 2015. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 63. Ayhan S, Aykac B, Yuksel S, et al. ; ESSG European Spine Study Group. Safety and efficacy of osteotomies in adult spinal deformity: what happens in the first year? Eur Spine J 2015. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]


