Abstract
Tibial plateau fractures are complex injuries produced by high- or low-energy trauma. They principally affect young adults or the ‘third age’ population.
These fractures usually have associated soft-tissue lesions that will affect their treatment. Sequential (staged) treatment (external fixation followed by definitive osteosynthesis) is recommended in more complex fracture patterns. But one should remember that any type of tibial plateau fracture can present with soft-tissue complications.
Typically the Schatzker or AO/OTA classification is used, but the concept of the proximal tibia as a three-column structure and the detailed study of the posteromedial and posterolateral fragment morphology has changed its treatment strategy.
Limb alignment and articular surface restoration, allowing early knee motion, are the main goals of surgical treatment. Partially articular factures can be treated by minimally-invasive methods and arthroscopy is useful to assist and control the fracture reduction and to treat intra-articular soft-tissue injuries.
Open reduction and internal fixation (ORIF) is the gold standard treatment for these fractures. Complex articular fractures can be treated by ring external fixators and minimally-invasive osteosynthesis (EFMO) or by ORIF. EFMO can be related to suboptimal articular reduction; however, outcome analysis shows results that are equal to, or even superior to, ORIF. The ORIF strategy should also include the optimal reduction of the articular surface.
Anterolateral and anteromedial surgical approaches do not permit adequate reduction and fixation of posterolateral and posteromedial fragments. To achieve this, it is necessary to reduce and fix them through specific posterolateral or posteromedial approaches that allow optimal reduction and plate/screw placement.
Some authors have also suggested that primary total knee arthroplasty could be an option in specific patients and with specific fracture patterns.
Cite this article: Prat-Fabregat S, Camacho-Carrasco P. Treatment strategy for tibial plateau fractures: an update. EFORT Open Rev 2016;1:225-232. DOI: 10.1302/2058-5241.1.000031.
Keywords: tibial plateau fractures, three-column concept, posteromedial knee approach, posterolateral knee approach, staged sequential surgical treatment
Tibial plateau fractures (TPFs) are common and difficult-to-manage injuries that can be due to high- or low-energy trauma and can affect young adults or third-age patients. When faced with one of these injuries there are some questions to be answered. They are discussed in detail below.
Is it a high- or a low-energy trauma?
Both high- and low-energy trauma can cause TPFs. Usually complex knee fractures are seen in pedestrians struck by vehicles and also in work-related accidents.1 In general, one should expect a more complex fracture pattern in higher-energy trauma. But the quality of the osteoporotic bone, particularly in third-age people, can lead to complex fracture patterns with low-energy injuries. In the same way, surrounding soft-tissue involvement is to be expected even in low-energy fractures (Fig. 1). This suggests that every single fracture has to be carefully evaluated in order to identify the exact pattern, the shape, size and location of the different fragments, and must be carefully managed to prevent or anticipate soft-tissue complications.
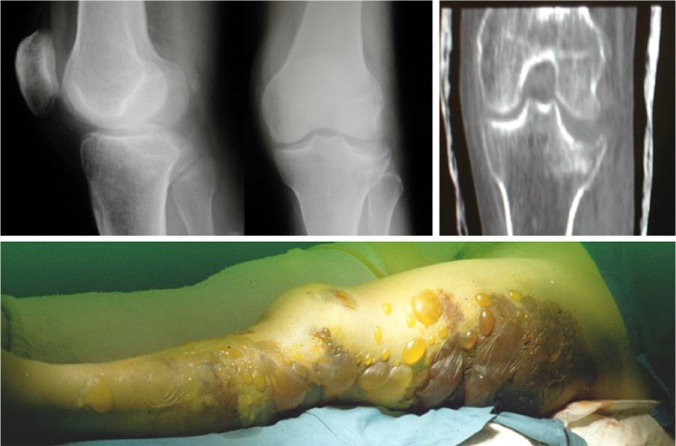
Fig. 1.
Substantial soft tissue injuries with a broken bone inside. Extensive haemorrhagic and serous blisters 36 hours after injury in an obese female patient who suffered a low-energy trauma and sustained a partial articular fracture (Schatzker 3/ AO OTA 41B2).
Does age matter in determining management?
The age of the patient and his/her previous functional status can be critical in deciding the type of treatment to be applied. The main objectives when treating articular fractures of the knee are the restoration of articular congruity and stability, the axial and rotational alignment of the limb, and stability and early motion of the joint. All three are critical, especially in the young patient, but there is some evidence that limb alignment and knee stability are most crucial, whereas non-anatomical reduction is less important regarding functional results.2 Actually, it is not difficult to find patients with sub-optimal lateral plateau articular surface reductions and acceptable functional results in the clinical setting.
What is the state of the soft tissues surrounding the fracture?
Soft-tissue damage in fractures around the knee is of critical importance. One should think that the fracture will not change but soft tissue will, and therefore, especially in high-energy injuries, fractures should be considered as ‘substantial soft-tissue injuries with a broken bone inside’ (Fig. 1).3 The oedema and inflammation associated with the trauma can easily lead to local venous compromise, dermal hypoxia, and additional soft-tissue injury.4 This commonly leads to blistering of the skin and in some cases dermal and even muscle necrosis.5 Blood-filled blisters should be expected to be associated with a worse outcome than clear fluid-filled ones. Management in the early stages of treatment should focus on preventing further soft-tissue injury while waiting to repair the fracture. Immobilisation of the knee and cryotherapy are the most commonly-used methods to diminish the inflammatory response.1 Knee immobilisation can be achieved by splinting or by external fixation. The use of a staged approach using external fixation is recommended in complex patterns and high-energy trauma, especially in cases of axial instability. Knee-spanning external fixators can be used to approximate the fracture fragments by the process of ligamentotaxis.1,6 A common frame consists of two 4.5 to 5.0 mm pins placed anteriorly in the middle third femoral shaft and another two in the middle or distal third of the tibial shaft. Bars should be configured in two planes, in order to control varus-valgus and flexion-extension forces, and tightened in slight traction to reduce the fracture fragments.
Analysis of the infection risk of the fracture fixation site after pin site-plate overlap shows controversial results. Even though one recent paper concludes that, with an infection rate of 7.6%, this ‘common fear does not appear to be clinically grounded’,7 an even more recent paper analysing proximal and distal tibial fractures8 supports the view that, with an infection rate of 12% in proximal tibia fractures, the risk of infection when there is overlapping is clearly higher. According to these reports we should place the external fixator pins in the optimal situation to control the fracture7 and in a position that does not interfere with the definitive osteosynthesis plan.8
Compartment syndrome can be a devastating complication affecting proximal tibia fractures. Its incidence can rise to 17% of closed and 18.7% of open complex pattern proximal tibia fractures.6 One should be aware of the four ‘p’ rule (pain, pallor, paresthaesia and pain with passive stretch) in the initial phase of treatment to identify this condition and treat it as soon as possible.
Diagnosis and classification of the fracture
Traditionally, initial radiograph diagnosis should include anteroposterior (AP), lateral and oblique views. But single radiographs do not allow an exact fragment identification and the initial fracture classification can change in 5% to 24% (mean 12%) of cases and treatment can change in up to 26% of cases after CT scan imaging.9 These findings and the wider availability of CT scanning have made the oblique views less important in the diagnosis. Intra- and peri-articular soft-tissue structures can be affected even in less complex fracture patterns and some X-ray or CT scan data can also suggest the existence of a lateral or medial meniscal tear. Articular depression > 6 mm and/or articular widening > 5 mm are associated with the existence of lateral meniscus, lateral collateral ligament (LCL) or posterior cruciate ligament injuries.10,11 The identification of soft-tissue injuries with MRI can change the surgical treatment and/or rehabilitation plan. In a study of 103 patients with various Schatzker type fractures, a total of 99% presented associated soft-tissue injuries and 77% a complete anterior cruciate ligament (ACL) or LCL injury, whereas 81% presented with a significant lateral meniscal tear and 44% a medial meniscus tear.12 MRI can adequately identify soft-tissue injuries, but its cost and lack of availability make its systematic use problematic.
What is the nature of the fracture?
Tibial plateau fractures are usually classified with the six-type Schatzker fracture classification.13 The AO/OTA14 proximal tibia fracture classification (segment 41) is partially based on it, and includes extra-articular (a), partial articular (b) and complete articular (c) fractures. Schatzker Type I-II-III-IV should correspond to 41B fractures and Type V-VI to 41C fractures. Both 41B and C have different sub-types according to fragment morphology and comminution. But biplanar analysis of these fractures has been demonstrated to be insufficient to identify the fracture pattern and to guide treatment strategy. The idea of the proximal tibia as a three-column structure15 opens the door to a new fracture understanding.
Pure articular depression (Schatzker Type III) should be a ‘zero-column fracture’. Most of the simple lateral split and split depression fractures (Schatzker Types I and II) should be a ‘one-column (lateral column) fracture’. The posterior shearing fracture,16 an articular depression in the posterior column with a break of the posterior wall, is a ‘one-column (posterior column) fracture’ (not included in Schatzker classification). There are two common types of two-column fractures. An anterolateral fracture and a separate posterior–lateral articular depression with a break of the posterior wall is a ‘two-column (lateral and posterior column) fracture’. The other typical ‘two-column fracture’ is the anteromedial fracture with a separate posteromedial fragment (medial and posterior column fracture), which traditionally belongs to Schatzker Type IV (medial condylar fracture). The ’three-column fracture’ is defined as at least one independent articular fragment in each column. The most common three-column fracture is a traditional ‘bicondylar fracture’ (Schatzker Type V or Type VI) combined with a separate posterolateral articular fragment. Bicondylar fracture (A0-OTA C type) analysis shows the existence of a posteromedial fragment in 30%17 to nearly 65%18 of fractures, affecting 23% of the medial plateau articular surface as a mean.17 The existence of a posterolateral fragment in AO-OTA type B and C fractures has been detected in about 44% of cases and affects nearly one-third of the lateral tibial plateau surface.19 The three-column concept and knowledge about these posteromedial and posterolateral fragments have changed the understanding of fractures and strategies for treatment.
What are the indications for surgical treatment?
In general, tibial plateau fractures are to be operated on, but the decision whether to operate or not on a specific fracture should be based on the fracture morphology, the soft tissues and the patient’s general condition, and the expected limb axis and articular surface restoration. Usual indications for surgical treatment are:20
Intra-articular displacement of ⩾ 2 mm
Metaphyseal-diaphyseal translation of > 1 cm
Angular deformity of > 10° in the coronal (varus-valgus) or sagittal plane
Open fracture
Associated compartment syndrome
Associated ligament injury requiring repair
Associated fractures of the ipsilateral tibia or fibula
The main contra-indications to surgery are: an unfit patient or a patient unable to follow the rehabilitation protocol, and soft-tissue complications. Surgical treatment is best considered for partial and complete articular fractures.
In partial articular fractures (AO/OTA 41B1,B2,B3/ Schatzker I,II,III and some IV), articular surface restoration can be achieved via an open or a percutaneous technique. The percutaneous reduction technique includes fragment(s) elevation and surface restoration through an epiphyso-metaphyseal window, using conventional techniques with a bone impactor. Recently, the use of an inflatable bone tamp, known as inflation osteoplasty,21,22 has been described as a minimally-invasive technique. There are no clinical results available that can support the use of this technique. Once the articular surface is restored, the remaining underlying bone defect can be filled up with autologous or heterologous bone graft or with bone cement. To date there is insufficient evidence about the best method, but autologous bone graft use, probably the gold standard in young patients, is related to troublesome donor site pain. This supports the use of heterologous bone graft or bone cements.23
Arthroscopy can be useful to control articular surface reduction and to diagnose and treat soft-tissue articular lesions, which can be as many as as 42% of meniscal tears and up to 21% of ACL injuries.24,25 Functional results are rated as excellent or good in 90% of patients with a low rate of severe complications, despite one post-operative compartment syndrome being reported.24 Using our preferred technique (percutaneous, arthroscopically-assisted or open technique) we must ensure the goal of the surgery: to obtain anatomical reduction and a fracture fixation stable enough to allow early/immediate knee motion.
In complete/complex articular fractures (AO/OTA 41 C1,C2,C3/ Schatzker IV,V,VI) open reduction and internal fixation (ORIF) treatment is the gold standard. But they can also be treated with ring external fixators and minimal osteosynthesis (EFMO). In ORIF, a staged approach is recommended in order to prevent soft-tissue complications.6,26
Usually ORIF has been practised from an anterolateral or a medial approach depending on the fracture type. But the three-column concept15 and fracture fragment analysis17,19 have changed the treatment strategy. Adequate fixation of the posterolateral and/or posteromedial fragments cannot usually be achieved through traditional anterolateral and medial approaches. Despite this, in some cases with slight displacement, the posteromedial fragment can be big enough to be reduced percutaneously and fixed from anterior to posterior, and the posterolateral depression can be elevated through a metaphyseal window on the anterolateral aspect of the tibia (Fig. 2). In general, posterolateral and posteromedial fragments need to be buttress-plated and/or fixed from posterior to anterior. As shown in Fig. 3, the use of a medial plate when a coronal fracture exists will not provide adequate fragment stability. Especially with small fragments, the adequate reduction and fixation of the fracture requires a posteromedial approach. When using locking lateral proximal tibial plates (LISS),27,28 the screw direction does not achieve an adequate posteromedial fragment fixation.17.
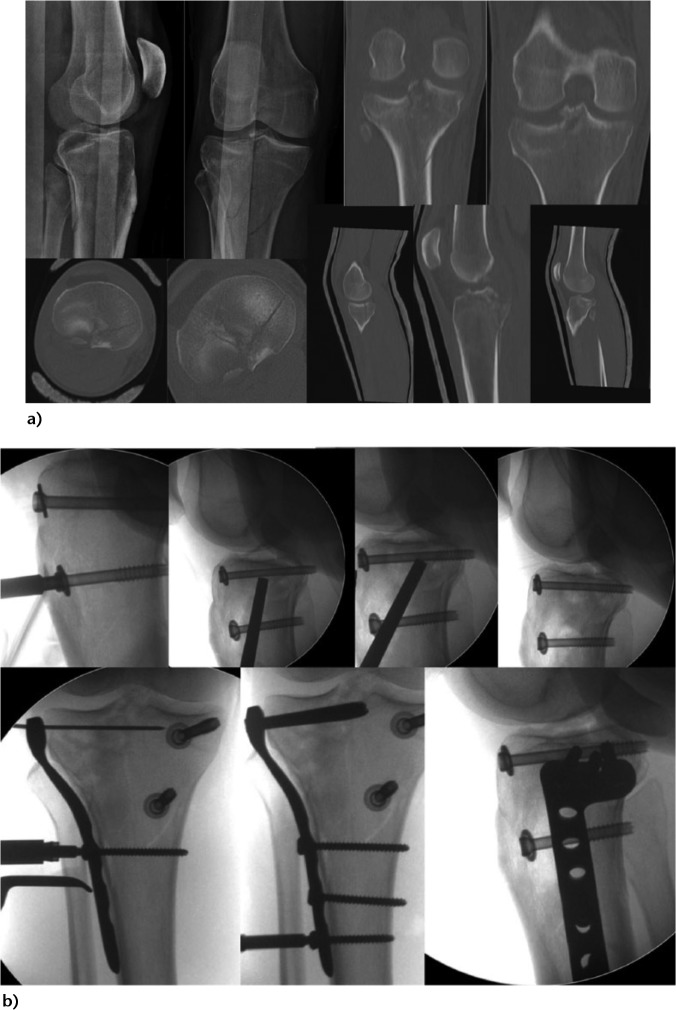
Fig. 2.
40-year-old patient who sustained a motorcycle injury. (a) Posterolateral fracture comminution and posteromedial fracture fragment; (b) Percutaneous medial fracture reduction and fixation with two cannulated screws. Through an anterolateral approach and an epiphysio-metphyseal window the posterolateral fracture was reduced with a bone elevator. Filling of the bone defect with bone allograft, L-shaped proximal tibia plate.
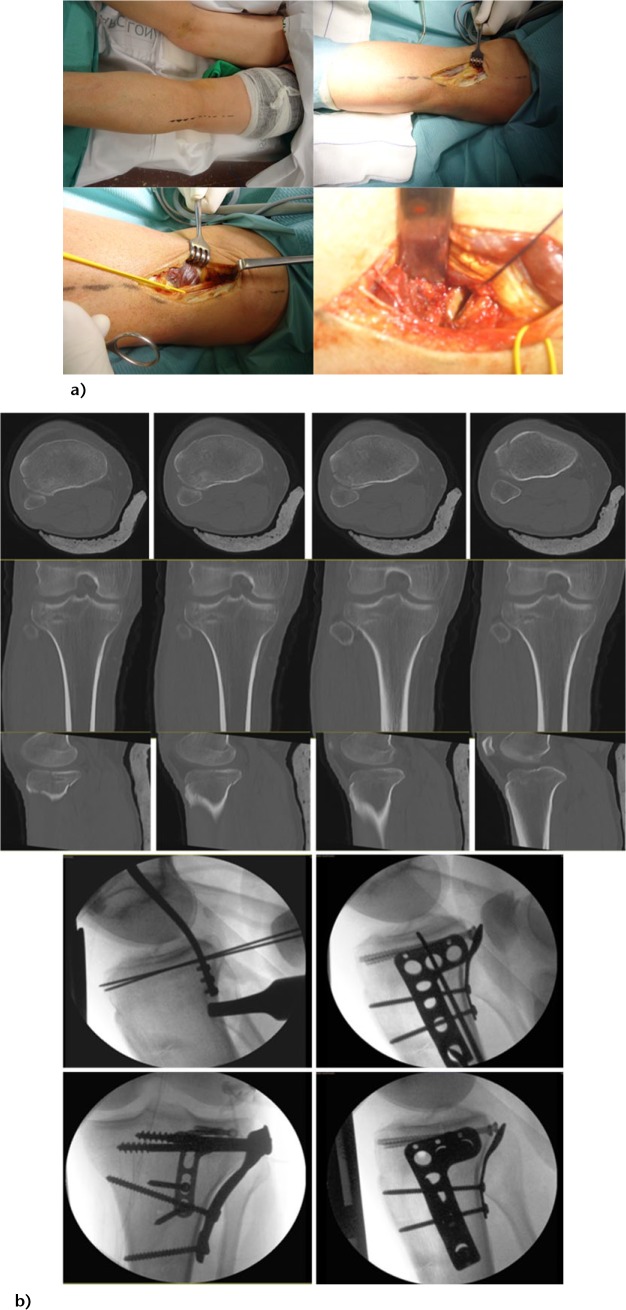
Fig. 3.
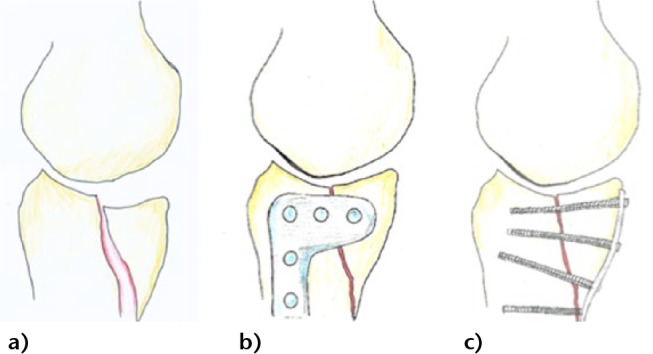
Posteromedial coronal fracture. (a) Scheme of the typical coronal posteromedial fragment displacement; (b) even if adequate reduction can be achieved from an anteromedial approach, the fixation obtained from the medial aspect of the tibia is suboptimal; (c) optimal reduction and fixation with a posteromedial approach using an adequately placed buttress plate and appropriate direction of the screws.
Adequate posteromedial fragment reduction and buttress plating requires a direct dorsal approach. It can be achieved both in supine29,30 or in prone position.31,32 The posteromedial approach in the supine position with the leg externally rotated has the advantage of allowing the approach to the lateral plateau through a separate incision, when necessary, without moving the patient. With this approach, located in the posteromedial aspect of the knee, 2 cm posterior to the medial approach, the saphenous vein has to be dissected and the pes anserinus tendons need to be mobilised in order to access the posterior aspect of the tibia. Galla and Lobenhoffer31 described the posteromedial approach with the patient in prone position: through a longitudinal approach, located over the medial gastrocnemius, not crossing the popliteal crease, the muscle is lateralised and the posteromedial aspect of the tibia can be reached. Luo15 described a posterior inverted L-shaped approach with the patient in a lateral decubitus floating position that permits changing to the lateral aspect of the knee when necessary. This approach permits, by lateralising the medial head of the gastrocnemius, the visualisation of the entire posterior aspect of the tibia without cutting the medial head of the gastrocnemius. Bhattacharyya16 uses an S-shaped direct dorsal approach, proximally centred and distally medialised, with a section of the tendon of the medial head of the gastrocnemius to treat the posterior shearing fractures. Through it, the lateral fracture fragments can also be reached when necessary.
Isolated posterolateral fragments require also specific approaches. These fragments can be reached and reduced through a posterolateral prone approach with or without fibular head osteotomy after common peroneal nerve (CPN) dissection (Fig. 4).33-35. These approaches, made in the prone position, require an additional lateral approach when we need to fix the lateral column.
Fig. 4.
Patient prone. Posterolateral fracture and posterolateral approach without fibular osteotomy. (a) Approach location. Identification and dissection of the CPN. Visualisation and approach to the articular fracture fragments. (b) Posterolateral fracture. Reduction and fixation with K-wires of the posterolateral fragments. Buttress plating. Fixation of the lateral column through an anterolateral approach.
A direct posterolateral approach with fibular head osteotomy in the supine position has been described36 and would permit the posterolateral fragment reduction and the lateral column fixation from the same incision when necessary.37 This approach allows the preservation of the lateral tibial condyle blood supply and has not been related to CPN or fibular head osteotomy (re-attached with a screw) complications. When compared with the anterolateral approach, the quality and maintenance of the reduction of the posterior fragment are substantially better.38 An anterolateral approach with femoral epicondyle osteotomy has been recently reported, together with a sub-meniscal arthrotomy, to reduce the posterolateral fracture and to treat intra-articular injuries. The lateral epicondyle is re-attached with a cortical screw.39,40 Potential problems with this osteotomy consolidation could produce residual posterolateral instability. The two latter approaches facilitate articular fracture reduction because a bigger varus can be obtained, but present difficulties adequately fixing the posterolateral fragments.40
The use of minimally-invasive osteosynthesis and an Ilizarov-type ring fixator has been advocated as a way to minimize ORIF complications.20 Despite this EFMO is usually related to a worse articular reduction; a randomised study comparing ORIF versus EFMO in type C fractures shows that EFMO is associated with less blood loss, fewer unplanned re-operations and a shorter hospital stay.20 There were no differences in two-year functional results and in reduction between groups.20
A recent review by McNamara et al41 evaluating four randomised and two quasi-randomised trials, comparing ORIF with EFMO, did not find enough evidence to ascertain the best method of fixation. Current evidence does not contradict the idea of the best results obtained when using limited exposures to treat these fractures.
Patients with a tibial plateau fracture have a risk five times higher of needing a total knee arthroplasty (TKA) when compared with a matched cohort population.42 This risk is related to age and to the complexity of the fracture. Knee instability or malunion increases the need for a TKA.43 Some authors44,45 suggest that, in some specific patients, TKA could be the primary procedure. Age > 65 years, local osteopaenia, corticoid use and pre-existing osteoarthritis are identified as the main reasons indicating a primary arthroplasty.
What outcomes can be expected?
Evaluation of long-term outcomes after a tibial plateau fracture should include assessment of pain, function/quality of life and osteoarthritis (OA). Function and quality of life are usually evaluated through specific knee questionnaires, but there is no satisfactory specific post-fracture evaluation system. Analysis of the results of a group of 71 surgically-treated TPF patients to whom the Knee Injury and Osteoarthritis Outcome Score (KOOS) was applied, at a mean follow-up of 6.17 years,46 showed no correlation between anatomical/non-anatomical reduction and function. Scoring referring to pain, activities of daily living, sports-recreation and quality of life shows worse results in partial articular than in complete articular fractures. This has been explained, according to the authors, by the greater outcome expectations of the less complex fracture patients. Only half of the patients that played sport went back to their previous sporting activity level. TKA was required in 7.3% and implant removal in 41.6% of patients. By contrast, TKA was required in up to 22% of patients in a series of 82 TPF at a mean follow-up of 6.8 years.47 In this group, persistent pain is related to high-energy trauma injuries. Another study48 comparing OA signs at 3 and at 22 years in a group of 31 patients with surgically treated TPF, showed that there is a deterioration of radiological OA signs between 3 and 22 years of follow-up and that there are differences in the evolution of the OA signs between the operated and the healthy knee in the same patient. TKA was required in 13% of patients in this study. Valgus malalignment > 5º is usually related to severe radiological osteoarthritis49,50 but this does not directly correlate with bad functional results.
Conclusions
In summary, tibial plateau fractures are serious injuries, usually associated with soft-tissue complications. Staged treatment is recommended in severe cases. Minimally-invasive osteosynthesis, when possible, is recommended in partial articular fractures. Arthroscopy can assist fracture reduction and makes possible the repair of meniscal/ligament tears. Complete articular fractures can be treated by ORIF or by wire fixators and minimally-invasive osteosynthesis techniques. Anatomical reduction and stable fixation of posteromedial and posterolateral fracture fragments is very important to avoid secondary malreductions. TKA can be the primary treatment of complex patterns in specific third-age patients. Osteoarthritis is a frequent complication of these fractures. Patients suffering a tibial plateau fracture should be aware of the residual pain and functional limitations that can appear in the mid- and long-term.
Footnotes
Conflict of Interest: None declared.
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Borrelli J., Jr Management of soft tissue injuries associated with tibial plateau fractures. J Knee Surg 2014;27:5-9. [DOI] [PubMed] [Google Scholar]
- 2. Hall JA, Beuerlein MJ, McKee M, Canadian Orthopaedic Trauma Society. Open Reduction and Internal Fixation Compared with Circular Fixator Application for Bicondylar Tibial Plateau Fractures. J Bone Jt Surg 2009;91:74-8. [DOI] [PubMed] [Google Scholar]
- 3. Lowe JA, Tejwani N, Yoo B, Wolinsky P. Surgical techniques for complex proximal tibial fractures. J Bone Joint Surg [Am] 2011;93-A:1548-59. [PubMed] [Google Scholar]
- 4. Südkamp NP. Soft-tissue injury: pathophysiology and its influence on fracture management. In: Reudi TP, Murphy WM, eds. AO Principles of Fracture Management Stuttgart, Germany: Thieme, 2000:59-77. [Google Scholar]
- 5. Giordano CP, Koval KJ, Zuckerman JD, Desai P. Fracture blisters. Clin Orthop Relat Res 1994;307:214-21. [PubMed] [Google Scholar]
- 6. Egol KA, Tejwani NC, Capla EL, Wolinsky PL, Koval KJ. Staged management of high-energy proximal tibia fractures (OTA types 41): the results of a prospective, standardized protocol. J Orthop Trauma 2005;19:448-55. [DOI] [PubMed] [Google Scholar]
- 7. Laible C, Earl-Royal E, Davidovitch R, Walsh M, Egol KA. Infection after spanning external fixation for high-energy tibial plateau fractures: is pin site-plate overlap a problem? J Orthop Trauma 2012;26:92-7. [DOI] [PubMed] [Google Scholar]
- 8. Shah CM, Babb PE, McAndrew CM, et al. Definitive plates overlapping provisional external fixator pin sites: is the infection risk increased? J Orthop Trauma 2014;28:518-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chan PS, Klimkiewicz JJ, Luchetti WT, et al. Impact of CT scan on treatment plan and fracture classification of tibial plateau fractures. J Orthop Trauma 1997;11:484-9. [DOI] [PubMed] [Google Scholar]
- 10. Gardner MJ, Yacoubian S, Geller D, et al. Prediction of soft-tissue injuries in Schatzker II tibial plateau fractures based on measurements of plain radiographs. J Trauma 2006;60:319-23. [DOI] [PubMed] [Google Scholar]
- 11. Spiro AS, Regier M, Novo de Oliveira A, et al. The degree of articular depression as a predictor of soft-tissue injuries in tibial plateau fracture. Knee Surg Sports Traumatol Arthrosc 2013;21:564-70. [DOI] [PubMed] [Google Scholar]
- 12. Gardner MJ, Yacoubian S, Geller D, et al. The incidence of soft tissue injury in operative tibial plateau fractures: a magnetic resonance imaging analysis of 103 patients. J Orthop Trauma 2005;19:79-84. [DOI] [PubMed] [Google Scholar]
- 13. Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The Toronto experience 1968–1975. Clin Orthop Relat Res 1979;138:94-104. [PubMed] [Google Scholar]
- 14. Müller ME, Nazarian S, Koch P, Schatzker J, Heim U. The Comprehensive Classification of Fractures of Long Bones. Berlin: Springer,1990. [Google Scholar]
- 15. Luo CF, Sun H, Zhang B, Zeng BF. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma 2010;24:683-92. [DOI] [PubMed] [Google Scholar]
- 16. Bhattacharyya T, McCarty LP, III, Harris MB, et al. The posterior shearing tibial plateau fracture: treatment and results via a posterior approach. J Orthop Trauma 2005;19:305-10. [PubMed] [Google Scholar]
- 17. Barei DP, O’Mara TJ, Taitsman LA, Dunbar RP, Nork SE. Frequency and fracture morphology of the posteromedial fragment in bicondylar tibial plateau fracture patterns. J Orthop Trauma 2008;22:176-82. [DOI] [PubMed] [Google Scholar]
- 18. Higgins TF, Kemper D, Klatt J. Incidence and morphology of the posteromedial fragment in bicondylar tibial plateau fractures. J Orthop Trauma 2009;23:45-51. [DOI] [PubMed] [Google Scholar]
- 19. Sohn HS, Yoon YC, Cho JW, et al. Incidence and fracture morphology of posterolateral fragments in lateral and bicondylar tibial plateau fractures. J Orthop Trauma 2015;29:91-7. [DOI] [PubMed] [Google Scholar]
- 20. Hall JA, Beuerlein MJ, McKee MD; Canadian Orthopaedic Trauma Society. Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures. Surgical technique. J Bone Joint Surg [Am] 2009;91:74-88. [DOI] [PubMed] [Google Scholar]
- 21. Broome B, Mauffrey C, Statton J, Voor M, Seligson D. Inflation osteoplasty: in vitro evaluation of a new technique for reducing depressed intra-articular fractures of the tibial plateau and distal radius. J Orthop Traumatol 2012;13:89-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Heiney JP, Kursa K, Schmidt AH, Stannard JP. Reduction and Stabilization of Depressed Articular Tibial Plateau Fractures: Comparison of Inflatable and Conventional Bone Tamps: Study of a Cadaver Model. J Bone Joint Surg [Am] 2014;96-A:1273-9. [DOI] [PubMed] [Google Scholar]
- 23. Goff T, Kanakaris NK, Giannoudis PV. Use of bone graft substitutes in the management of tibial plateau fractures. Injury 2013;44:S86-S94. [DOI] [PubMed] [Google Scholar]
- 24. Chen XZ, Liu CG, Chen Y, et al. Arthroscopy-assisted surgery for tibial plateau fractures. Arthroscopy 2015;31:143-53. [DOI] [PubMed] [Google Scholar]
- 25. Ruiz-Ibán MÁ, Diaz-Heredia J, Elías-Martín E, Moros-Marco S, Cebreiro Martinez Del Val I. Repair of meniscal tears associated with tibial plateau fractures: a review of 15 cases. Am J Sports Med 2012;40:2289-95. [DOI] [PubMed] [Google Scholar]
- 26. Parekh AA, Smith WR, Silva S, et al. Treatment of distal femur and proximal tibia fractures with external fixation followed by planned conversion to internal fixation. J Trauma 2008;64:736-9. [DOI] [PubMed] [Google Scholar]
- 27. Ricci WM, Rudzki JR, Borrelli J., Jr Treatment of complex proximal tibia fractures with the less invasive skeletal stabilization system. J Orthop Trauma 2004;18:521-7. [DOI] [PubMed] [Google Scholar]
- 28. Weaver MJ, Harris MB, Strom AC, et al. Fracture pattern and fixation type related to loss of reduction in bicondylar tibial plateau fractures. Injury 2012;43:864-9. [DOI] [PubMed] [Google Scholar]
- 29. Weil YA, Gardner MJ, Boraiah S, Helfet DL, Lorich DG. Posteromedial supine approach for reduction and fixation of medial and bicondylar tibial plateau fractures. J Orthop Trauma 2008;22:357-62. [DOI] [PubMed] [Google Scholar]
- 30. Kandemir U, Maclean J. Surgical approaches for tibial plateau fractures. J Knee Surg 2014;27:21-9. [DOI] [PubMed] [Google Scholar]
- 31. Galla M, Lobenhoffer P. [The direct, dorsal approach to the treatment of unstable tibial posteromedial fracture-dislocations]. Unfallchirurg 2003;106:241-7.[Article in German] [DOI] [PubMed] [Google Scholar]
- 32. Fakler JK, Ryzewicz M, Hartshorn C, et al. Optimizing the management of Moore type I postero-medial split fracture dislocations of the tibial head: description of the Lobenhoffer approach. J Orthop Trauma 2007;21:330-6. [DOI] [PubMed] [Google Scholar]
- 33. Yu GR, Xia J, Zhou JQ, Yang YF. Low-energy fracture of posterolateral tibial plateau: treatment by a posterolateral prone approach. J Trauma Acute Care Surg 2012;72:1416-23. [DOI] [PubMed] [Google Scholar]
- 34. Frosch KH, Balcarek P, Walde T, Stürmer KM. A new posterolateral approach without fibula osteotomy for the treatment of tibial plateau fractures. J Orthop Trauma 2010;24:515-20. [DOI] [PubMed] [Google Scholar]
- 35. Carlson DA. Posterior bicondylar tibial plateau fractures. J Orthop Trauma 2005;19:73-8. [DOI] [PubMed] [Google Scholar]
- 36. Tscherne H, Lobenhoffer P. Tibial plateau fractures. Management and expected results. Clin Orthop Relat Res 1993;292:87-100. [PubMed] [Google Scholar]
- 37. Solomon LB, Stevenson AW, Baird RP, Pohl AP. Posterolateral transfibular approach to tibial plateau fractures: technique, results, and rationale. J Orthop Trauma 2010;24:505-14. [DOI] [PubMed] [Google Scholar]
- 38. Solomon LB, Stevenson AW, Lee YC, Baird RPV, Howie DW. Posterolateral and anterolateral approaches to unicondylar posterolateral tibial plateau fractures: a comparative study. Injury 2013;44:1561-8. [DOI] [PubMed] [Google Scholar]
- 39. Yoon YC, Sim JA, Kim DH, Lee BK. Combined lateral femoral epicondylar osteotomy and a submeniscal approach for the treatment of a tibial plateau fracture involving the posterolateral quadrant. Injury 2015;46:422-6. [DOI] [PubMed] [Google Scholar]
- 40. Garner MR, Warner SJ, Lorich DG. Surgical Approaches to Posterolateral Tibial Plateau Fractures. J Knee Surg 2016;29:12-20. [DOI] [PubMed] [Google Scholar]
- 41. McNamara IR, Smith TO, Shepherd KL, et al. Surgical fixation methods for tibial plateau fractures. Cochrane Database Syst Rev 2015;9:CD009679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wasserstein D, Henry P, Paterson JM, Kreder HJ, Jenkinson R. Risk of Total Knee Arthroplasty After Operatively treated tibial plateau fractures. J Bone Joint Surg [Am] 2014;96-A:144-150. [DOI] [PubMed] [Google Scholar]
- 43. Scott CE, Davidson E, MacDonald DJ, White TO, Keating JF. Total knee arthroplasty following tibial plateau fracture: a matched cohort study. Bone Joint J 2015;97-B:532-8. [DOI] [PubMed] [Google Scholar]
- 44. Malviya A, Reed MR, Partington PF. Acute primary total knee arthroplasty for peri-articular knee fractures in patients over 65 years of age. Injury 2011;42:1368-71. [DOI] [PubMed] [Google Scholar]
- 45. Kini SG, Sathappan SS. Role of navigated total knee arthroplasty for acute tibial fractures in the elderly. Arch Orthop Trauma Surg 2013;133:1149-54. [DOI] [PubMed] [Google Scholar]
- 46. van Dreumel RL, van Wunnik BP, Janssen L, Simons PC, Janzing HM. Mid- to long-term functional outcome after open reduction and internal fixation of tibial plateau fractures. Injury 2015;46:1608-12. [DOI] [PubMed] [Google Scholar]
- 47. Timmers TK, van der Ven DJ, de Vries LS, van Olden GD. Functional outcome after tibial plateau fracture osteosynthesis: a mean follow-up of 6 years. Knee 2014;21:1210-15. [DOI] [PubMed] [Google Scholar]
- 48. Mattiassich G, Foltin E, Scheurecker G, et al. Radiographic and clinical results after surgically treated tibial plateau fractures at three and twenty two years postsurgery. Int Orthop 2014;38:587-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Parkkinen M, Madanat R, Mustonen A, et al. Factors predicting the development of early osteoarthritis following lateral tibial plateau fractures: mid-term clinical and radiographic outcomes of 73 operatively treated patients. Scand J Surg 2014;103:256-62. [DOI] [PubMed] [Google Scholar]
- 50. Rademakers MV, Kerkhoffs GM, Sierevelt IN, Raaymakers EL, Marti RK. Operative treatment of 109 tibial plateau fractures: five- to 27-year follow-up results. J Orthop Trauma 2007;21:5-10. [DOI] [PubMed] [Google Scholar]