Abstract
Patellar instabilities are the most common knee pathologies during growth. Congenital dislocations are rare. Extensive, early soft tissue releases relocate the extensor mechanism and may enable normal development of the femoro-patellar anatomy.
Conservative management is the preferred strategy after a ‘first-time’ traumatic dislocation. In cases with concomitant anatomical predisposing factors such as trochlear dysplasia, malalignment, malrotation or ligamentous laxity, surgical reconstruction must be considered. The same applies to recurrent dislocations with pain, a sense of instability or re-dislocations which may also lead to functional compensatory mechanisms (quadriceps-avoiding gait in knee extension) or cartilaginous lesions with subsequent patello-femoral osteoarthritis. The decision-making process guiding surgical re-alignment includes analysis with standard radiographs and MRI of the trochlear groove, joint cartilage and medial patello-femoral ligament (MPFL). Careful evaluation of dynamic and static stabilisers is essential: the medial patello-femoral ligament provides stability during the first 20° of flexion, and the trochlear groove thereafter.
Excessive femoral anteversion, general ligamentous laxity with increased femoro-tibial rotation, patella alta and increased distance between the tibial tuberosity and the trochlear groove must also be taken into account and surgically corrected.
In cases with ongoing dislocations during skeletal immaturity, soft tissue procedures must suffice: reconstruction of the medial patello-femoral ligament as a standalone procedure or in conjuction with more complex distal realignment of the quadriceps mechanism may lead to a permanent stable result, or at least buys time until a definitive bony procedure is performed.
Cite this article: Hasler CC, Studer D. Patella instability in children and adolescents. EFORT Open Rev 2016;1:160-166. DOI: 10.1302/2058-5241.1.000018.
Keywords: patellar dislocation (habitual; recurrent), medial patellofemoral ligament, dysplasia, trochlea
Epidemiology and history
Patellar instabilities account for the most prevalent knee problems during growth. The overall incidence is around 50 in 100 000 children and adolescents per year with a peak at the age of 15 years.1,2 Most patellae displace laterally. Medial dislocations are usually iatrogenic due to extensive lateral retinacular release. After the first occurrence about 40% end up as recurrent dislocations, where two-thirds have open physes which limit the type of stabilising interventions to those which respect the integrity of the growth plates.3 A non-specific, non-contact trauma mechanism with a history of sudden ‘giving way’ or ‘locking’ under load in the stance phase, in combination with a movement of valgus–flexion–external rotation, occurs in more than 80% of primary patellar dislocations. Spontaneous patellar dislocation is common in skeletally immature girls, and locked dislocation is common in skeletally mature men.4 Many patients report that they felt the patella displacing medially.
Clinical presentation and examination
Careful appreciation of the dynamics of patellar tracking and thorough orthopaedic examination to define all of the involved predisposing static factors is of paramount importance. A positive ‘apprehension sign’ with tenderness and quadriceps activation when pushing the patella laterally in early flexion is characteristic for instability. Increased medio-lateral motion is quantified in different degrees of flexion. Tenderness over the medial facet and lateral condyle follows acute dislocations or in cases with chondral lesions. In contrast to general thought, the Q-angle is often decreased in cases with patellar lateralization.5 Gait analysis in patients with chronic instability typically reveals quadriceps-avoiding gait with increased foot plantar-flexion, hyperextension of the knee without loading response and anterior shift of the centre of gravity (plantar-flexion–knee extension couple). A minority of patients display increased knee flexion during stance.
Types of dislocation
Congenital dislocation is a rare condition. In such cases, a small dysplastic patella is dislocated at birth. The laterally displaced extensor mechanism leads to a progressive valgus-flexion deformity which – in contrast to other congenital pathologies such as deficient cruciates or discoid menisci – becomes obvious at an early stage. This condition is often bilateral and associated with underlying general pathologies such as nail-patella syndrome. Hence, it must be differentiated from neuromuscular dislocations which occur later in life owing to high lateral-pulling muscle forces, for example in spastic tetraparesis. Surgical reconstruction is challenging during growth but becomes even more so in neglected cases. Conservative treatment is therefore not a valid option. Early surgery includes vastus lateralis releases combined with medial shortening and patellar tendon re-routing. In cases where the vastus approach does not provide adequate soft tissue length to allow medial relocation of the patella, one may consider Z-lengthening of the quadriceps tendon or the patellar ligament dependent on the craniocaudal position of the patella. Quadriceps lengthening is used for patella alta; patellar ligament lengthening is used for patella baja.
In acute traumatic dislocations, the patella almost always moves laterally, caused by a combination of knee flexion, valgus and external rotation of the knee. In cases of a complete, easy to diagnose dislocation, the knee is locked in flexion. Reduction is achieved by gentle knee extension. Spontaneous reduction occurs frequently. Knee effusion and tenderness over the medial patello-femoral region and at the border of the lateral femoral condyle are typical findings. Patellar dislocations are the main cause for knee haemarthrosis during growth, and secondary causes are ACL injuries.6 Osteochondral fragments are found in about every sixth acute dislocation (15%), mostly following spontaneous relocation of the patella.1 They usually arise from the medial patellar facet or lateral femoral condyle when the patella hits against the lateral condyle as it relocates into the trochlear groove. Simultaneous femoral and patellar fragments are rare. Re-fixation can prove difficult if the bony portion is too small (< 1.5 cm) or in neglected cases. Over time the hydrophilic cartilage of the fragment attracts fluid and hence loses its original shape. Such fragments will require removal and eventually cartilage resurfacing. Extra-articular bony avulsions of the medial patello-femoral ligament more often occur at the patellar than at the femoral insertion7 (Fig. 1). Primary ligamentous repair after a first dislocation does not give better results than conservative treatment. However, in patients with clear anatomical predisposing factors such as malalignment and malrotation, re-alignment surgery including MPFL repair and correction of the underlying biomechanical pathologies should be considered. Primary surgery should also be considered in cases with associated osteochondral fractures.8,9
Acute constitutional dislocations happen without proportionate trauma and show few concomitant injuries, but the patient presents with multiple predisposing factors. A positive family history and general joint laxity are commonly found. Such dislocations almost always progress to a chronic habitual form. In practice, at first presentation of a patient complaining about long-standing patellar instability and pain, it is not easy to draw a clear line between recurrent post-traumatic and habitual dislocations since the start of the history often remains obscure. There are more predisposing factors in habitual cases, whereas a clear first acute episode without previous history of patellar problems and without obvious anatomical features indicates post-traumatic recurrent dislocation. Those beginning in early childhood are usually congenital. However, at the end of the diagnostic pathway all contributing factors (ligamentous, muscular, bony, lower limb malalignment and malrotation) have to be considered and taken into the therapeutic – mostly surgical – strategy.
Chronic permanent dislocations are found in patients with significant ligamentous laxity and small patella embedded in a short, laterally displaced extensor mechanism which acts as a knee flexor with consequent lack of active and passive knee extension and crouching gait.
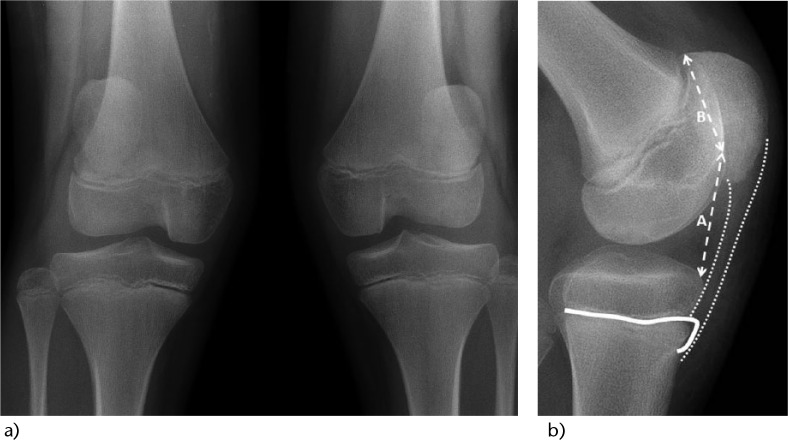
Fig. 1.
14-year-old boy with acute first-time dislocation during soccer play. The MRI shows a knee effusion (haemarthrosis marked with asterisk), a shallow trochlear groove (dotted line) and an avulsion fracture of the MPFL at its patellar insertion (arrow).
Anatomical considerations and predisposing factors
Identifying the presence of isolated or combined pre-disposing anatomical factors and weighing up their influence on patellar instability is crucial in determining the optimal, individualised treatment pathway. Many individuals (60%) show multiple factors.10 Finite element models of the patello-femoral joint analysing the influence of sulcus angle, Insall-Salvati ratio, tibial tubercle-trochlear groove distance and femoral anteversion in over 100 combinations showed that the sulcus angle is the most important factor.11 Apart from a routine orthopaedic appraisal of lower limb alignment and rotation, the patello-femoral joint requires careful dynamic and static examination. Patellar tracking is observed during active and passive knee motion in the supine position. Patellar position and tilt are assessed in the sitting patient with knees 90° flexed, with and without activation of the quadriceps muscle. The patella is carefully pushed in a lateral direction in various degrees of flexion. Local tenderness on palpation over the medial retinacula and on the lateral and medial patellar facets, and pain with manipulation in mediolateral and craniocaudal direction, with and without pressure, may indicate chondral lesions. The younger the child, the more often an underlying dysplasia of the patella (flattening of the cross-section) and the condylar surfaces if found.
General ligamentous laxity based on the Beighton scale is commonly found in female patients or in individuals with a collagen disorder. Apart from its direct influence on patellar stability, it may also indirectly impact on the patello-femoral tracking by increasing the intra-articular range of femoro-tibial rotation, clinically evident as postero-lateral rotational instability. Care must be taken when including the tibial tuberosity-trochlear groove distance (TT-TG) in the decision-making process with regard to surgical transposition of the TT: lateralisation of the tubercle may be more affected by knee rotation than by its anatomical position on the tibia, particularly in habitual dislocators.12 Also the degree of knee flexion influences TT-TG.13 At 120° knee flexion forces of up to 4600 N are pulling laterally on the patella.14 Genu valgum and/or recurvatum (which indicates increased ligamentous laxity), excessive femoral anteversion and external torsion of the tibia lead to an increase of that vector. Rotational anomalies are of more predisposing importance than axial deviations.
Patients with recurrent dislocation have rates of around three-fold higher of patella alta.10 Wasting of the quadriceps muscle is usually present after recurrent dislocations. Moreover, fibrosis in the vastus lateralis may be present.15 Increased Q-angle is generally believed to contribute to a patella-lateralising vector, and various surgical techniques aim at decreasing it. However, there is poor correlation between clinical and radiographic measurements, and the Q-angle in dislocating knees may even be decreased.5 True lateral radiographs allow classification of the type and degree of trochlear dysplasia, most commonly according to the principles stated by Déjour: shallow or missing sulcus (crossing sign), a flat or convex proximal sulcus or even a step-off between trochlea and anterior cortex of the distal femur and flattening of the lateral femoral condyle16,17 (Fig. 2). According to Insall, in patients with closed physis, standard lateral radiographs in 45° flexion determine whether there is a patella baja or alta position. In cases with open proximal tibia growth plates, the Insall reference point at the tuberosity is not reliable. Hence, in individuals who are still growing, the Caton-Deschamps index is preferred (length ratio of A. anterior proximal tibial plateau corner to most inferior point of patellar articular surface to B. length of patellar articular surface). Skeletal immaturity and trochlear dysplasia are the dominating factors for patellar instability, and a CD-index > 1.45 (patella alta) provides an important additional predictive factor18,19 (Fig. 3). A skyline view of the patella in 30° to 90° flexion may reveal free fragments, a shallow sulcus, patellar dysplasia and extra-articular avulsion fragments of the medial patello-femoral ligament at the patella. A CT scan allows for measurements of the bony trochlear groove angle, patellar tilt and height. Femoral anteversion and tibial torsion are assessed clinically or by a CT scan which still represents the ‘gold standard’. However, MRI and low-dose stereoradiography (EOS) are valuable alternatives, although the availability of the latter is limited. Ultrasound or MRI is helpful to distinguish between the cartilaginous and the osseous anatomy of the knee which is particularly important when it comes to the assessment of the morphology of the trochlear groove.20,21
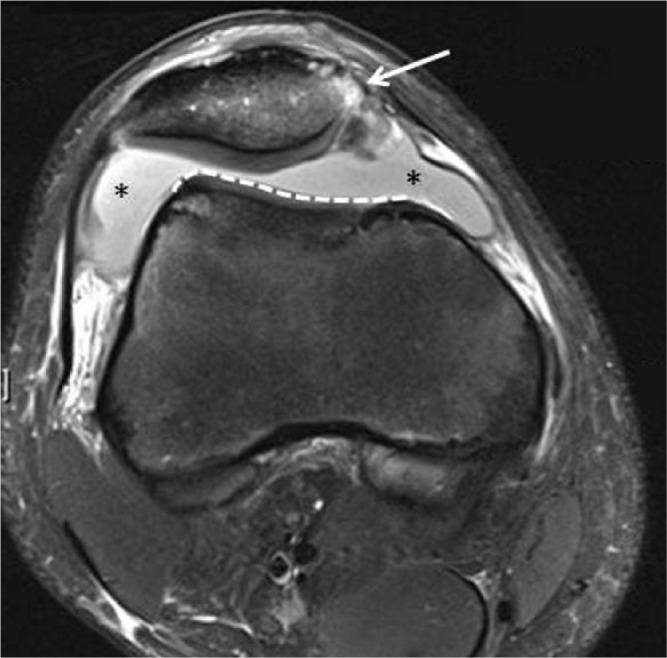
Fig. 2.
18-year-old boy with Down syndrome and recurrent painful dislocations of his left patella. Apart from syndrome-associated ligamentous laxity as a major predisposing factor, he displays significant trochlear dysplasia: 1) positive crossing sign (trochlear line crosses anterior femoral cortex line); 2) osseous bump (spur) at the upper border of the trochlea which misguides the patella into a lateral position when the patient is flexing his knee.
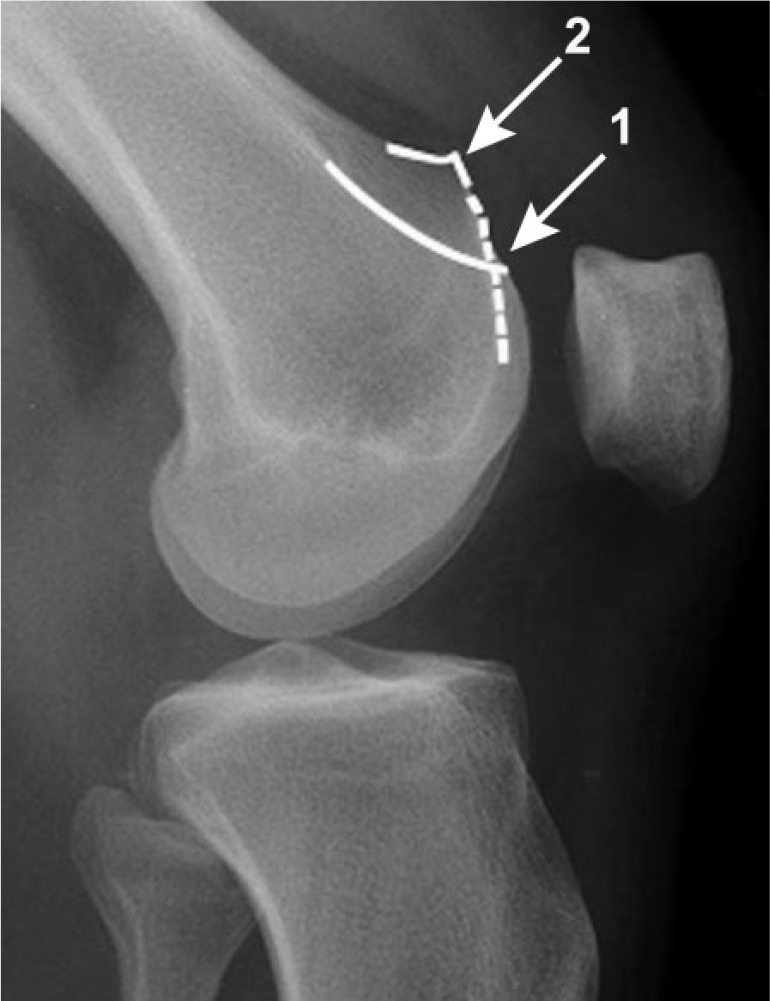
Fig. 3.
12-year-old boy with chronic habitual bilateral patellar dislocations. A concomitant predisposing factor was a moderate valgus deformity, young age and a trochlear dysplasia of both knees (a). The lateral view of the left knee shows the difficulty to objectify the patella position (alta, normal or baja): the growth plate with its anterior tongue (white line) has not ossified yet. Hence, there is no distinct insertion area of the patellar ligament (dotted line) and no clear osseous reference to assess the Insall index as in skeletally mature patients. The Caton-Deschamps ratio (A/B) is more appropriate but still difficult to assess in a patella which is subluxed (b). Moreover, longstanding lateralisation of the extensor mechanism led to a knee flexion contracture which omits a standard lateral radiograph.
Therapeutic considerations
It is an ongoing debate whether or not to leave congenitally displaced patellae alone. However, once the child reaches walking age, the lateral displacement of the extensor mechanism and the flexion-valgus deformity represent a significant biomechanical burden, particularly if the dislocation is part of a syndromic complex. A stepwise surgical à la carte approach may comprise a vastus lateralis release including the lateral ilio-tibial band, the vastus lateralis muscle and lengthening of the quadriceps (rectus snip). Also, doubling (shortening) of the medial structures over the patella including advancement of the oblique vastus medialis fibres and eventually re-routing of the lateral part of the patellar tendon with reinsertion (suture) under the pes anserinus is required. It aims at keeping the mostly cartilaginous, small disc-like patella on a flat trochlea in all degrees of flexion. Isolated procedures such as extensive medial transfer of the quadriceps muscle (Stanisavljevic procedure) has shown limited success rates.22 In adolescents with residual instabilities, targeted procedures such as trochleaplasties may be indicated.
Though prognosis is difficult to determine after initial acute patellofemoral dislocation, conservative treatment is the current best evidence strategy if significant maltracking factors and concomitant osteochondral fractures are ruled out.23 In mixed cohorts which were not divided into subgroups with different risk patterns, the 3–5-year recurrence rate varied between 35% and 70%, but the long-term functional and subjective results were satisfactory in most patients.24,25 A positive family history and instability of the contralateral patella are risk factors for recurrence. Skeletally immature patients with trochlear dysplasia carry the highest risk (69%) after non-operative treatment, compared with a 62% success rate if no major predisposing factor is present.3
First-time dislocators are at high risk of not returning to their previous level of sports activity. There is no evidence regarding the superiority of one rehabilitation programme over another, but it is common sense to involve patients in a three to four month exercise programme that is well-supervised by a physiotherapist through the specific functional stages: The first aim is to resolve pain and swelling, followed by restoration of joint motion, muscle strengthening and finally sport-specific exercises with return to sports activities and prevention of further episodes of instability. The programmes start with isometric general quadricep-strengthening exercises, specific distal vastus medialis muscle strengthening, building to the level of complex dynamic stabilisation of the lower extremity including the pelvic and lateral trunk stabilisers, and include proprioceptive tasks of increasing complexity. The ‘green light’ for a safe return to full activity should only be given when the patient is pain-free, without knee effusion, shows a complete range of motion of the knee, and when all sport-specific functional criteria are fulfilled. Adhesive tapes and proprioceptive braces can support this process, and may be applied through the first weeks after return to full sports activities. Despite focussed rehabilitation, quadriceps weakness may persist over years. Therefore patients should be motivated to continue exercising within a personalised fitness and sports programme, particularly if ligamentous laxity is present. In these cases, the importance of muscular competence – both strength and proprioception – cannot be overemphasised, particularly when the patient enters the process of ageing-related tissue degeneration and loss of muscle mass in later adulthood.26
In cases of failed conservative treatment with established disabling instability, operative treatment should be discussed depending on the level of suffering and functional impairment. Repeated ’giving way’ may cause cartilaginous lesions and chronic hyperpression with the risk of the later development of patellofemoral osteoarthritis. The goal of surgery is perfect tracking by restoration of the local bony and non-bony anatomy, and by the correction of more remote factors such as torsional and axial malalignment. Many isolated or combined procedures have been described to stabilise the patella:
In children with still open physes, severe patellar maltracking and predisposing factors for future re-dislocations, MPFL reconstruction, lateral release and correction of any malrotation and malalignment, for example by growth guidance (temporary hemiepiphysiodesis), should be considered first.
Lateral release can be performed arthroscopically, via mini-open surgery or through the main incision in major reconstructions. It is not indicated as an isolated procedure for recurrent dislocations. Moreover, extensive release in mild lateral instabilities can over-correct them into an iatrogenic medial dislocation. Medial, distal and anterior displacement of the tibial tuberosity is a ’no go’ in the growing child (boys up to 16 years, girls up to 14 years) because of the risk of partial growth arrest with subsequent progressive, fixed genu recurvatum. Nevertheless, the morphology of the anterior tongue of the proximal tibial physis allows lateral transposition of the non-osseous part of the distal extensor mechanism as originally described by Grammont in 1985 and modified later, for example by sharp dissection of the distal patellar tendon insertion and periosteal split along the tibial crest without affecting the growth plate.27,28
Ligamentum patellae (Roux-Goldthwait) distal re-alignment is an option for children. It requires adequate tension in the medial direction and secure fixation. Muscle forces support stability in 30°-40° knee flexion, but do not guarantee optimal patellar tracking. Passive bony and ligamentous stabilisers are considered more important: the patella enters the trochlea in early knee flexion guided by the medial patello-femoral ligamentous (MPFL) restraints, which tighten in knee extension and slacken with flexion. Adequate trochlear shape and sulcus depth are major stabilisers in knee flexion greater than 20°.29 Hence, MPFL reconstruction has become one of the most important surgical techniques for chronic patellar instability. This ligament has a tensile strength up to 200 N. It reaches from the medial femoral epicondyle to the superomedial border of the patella. In normal controls it is 40–60 mm long and 330 mm wide but was found to be thinner, only 14 mm, elongated and with lack of tension in dislocators.30,31 It is covered by the distal part of the vastus medialis obliquus muscle with fibres connecting both structures. MPFL reconstruction has mostly substituted previous medial repair with retinaculum doubling, which is not sufficient. The same holds true for first-time dislocations and primary surgical repair of the torn medial structures which does not give any better results than primary conservative treatment but often leaves unsightly scars or puts the infrapatellar nerve at risk. Isolated MPFL reconstruction with a hamstring tendon graft or adductor magnus is safe and beneficial if the anatomy of the limb and knee is normal. If obligatory (every time) dislocations occur in patients with ligamentous laxity, a combination with more extensive soft tissue procedures as described above is warranted and may show higher success rates.22,23,26
As a supplement to MPFL reconstruction or soft tissue techniques, the extensor mechanism can be realigned further distally in various ways depending on the state of the physis, the often under-appreciated proximal or distal malposition of the patella (alta or baja) and the localisation of the tibial tuberosity (TT). A laterally shifted tuberosity can be a consequence of a long-standing dislocation. Using osteotomy, the TT can be shifted medially (Hauser, Elmslie), distally (Roux, Magnussen) or ventrally (Maquet). In the unstable patello-femoral joint a deficient trochlea and high-riding patella often co-exist. A patella alta can either be corrected by shortening of the patellar ligament (open physis) or distalisation of the TT. Trochleoplasties are only applicable after closure of the distal femoral growth plate. Two-thirds of patients with recurrent dislocations display a trochlear dysplasia, compared with 6% in the stable cohort.10 Surgery either elevates the upper part of the lateral femoral condyle or deepens the intercondylar sulcus. Both strategies have a high success rate in terms of prevention of further dislocations. However, development of anterior knee pain and patellofemoral osteoarthritis is less predictable and data about mid- and long-term outcomes are limited.32 Moreover, it is not clear to what extent and to what age limit a dysplastic patella and reconstructed trochlea may remodel to congruency.
Conclusions
Patellar instability during growth is a challenge since many congenital and acquired factors may cause it. Therefore careful assessment and a thorough understanding of a patient’s anatomy, biomechanics, growth dynamics and development are crucial to define a targeted surgical strategy. In cases with still open physes, osteotomies for the correction of juxta-articular bony deformities and trochlear dysplasia need to be delayed, and soft tissue buy-time procedures may be indicated. Counselling regarding second-stage definitive surgery after the end of growth is mandatory. The incidence and time of occurrence of second-stage osteoarthritis after surgical treatment of patellar instabilities is not clear, nor is the natural history of untreated instabilities. However, recurrent dislocations in childhood lead to superficial cartilaginous signal changes in MRI scans of young adults,33 and an improvement of chondral status at ‘second-look’ arthroscopy an average of one year post-operatively has been documented after MPFL repair.34
Footnotes
Conflict of Interest: CH has received financial support outside of the current work in the form of consultancy fees from DePuy Synthes.
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Nietosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop 1994;14:513-5. PMID: 8077438. [DOI] [PubMed] [Google Scholar]
- 2. Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 2004;32:1114-21. PMID: 15262631. [DOI] [PubMed] [Google Scholar]
- 3. Lewallen LW, McIntosh AL, Dahm DL. Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med 2013;41:575-81. PMID: 23339838. [DOI] [PubMed] [Google Scholar]
- 4. Nikku R, Nietosvaara Y, Aalto K, Kallio PE. The mechanism of primary patellar dislocation: trauma history of 126 patients. Acta Orthop 2009;80:432-4. PMID: 19593720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sanfridsson J, Arnbjornsson A, Friden T, Ryd L, Svahn G, Jonsson K. Femorotibial rotation and the Q-angle related to the dislocating patella. Acta Radiol 2001;42:218-24. PMID: 11259951. [PubMed] [Google Scholar]
- 6. Abbasi D, May MM, Wall EJ, Chan G, Parikh SN. MRI findings in adolescent patients with acute traumatic knee hemarthrosis. J Pediatr Orthop 2012;32:760-4. [DOI] [PubMed] [Google Scholar]
- 7. Zheng L, Shi H, Feng Y, Sun BS, Ding HY, Zhang GY. Injury patterns of medial patellofemoral ligament and correlation analysis with articular cartilage lesions of the lateral femoral condyle after acute lateral patellar dislocation in children and adolescents: An MRI evaluation. Injury 2015;46:1137-44. PMID: 25724397. [DOI] [PubMed] [Google Scholar]
- 8. Erickson BJ, Mascarenhas R, Sayegh ET, et al. Does operative treatment of first-time patellar dislocations lead to increased patellofemoral stability? A systematic review of overlapping meta-analyses. Arthroscopy 2015;31:1207-15. PMID: 25636989. [DOI] [PubMed] [Google Scholar]
- 9. Khormaee S, Kramer DE, Yen YM, Heyworth BE. Evaluation and management of patellar instability in pediatric and adolescent athletes. Sports Health 2015;7:115-23. PMID: 25984256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Steensen RN, Bentley JC, Trinh TQ, Backes JR, Wiltfong RE. The prevalence and combined prevalences of anatomic factors associated with recurrent patellar dislocation: a magnetic resonance imaging study. Am J Sports Med 2015;43:921-7. PMID: 25587185. [DOI] [PubMed] [Google Scholar]
- 11. Fitzpatrick CK, Steensen RN, Tumuluri A, Trinh T, Bentley J, Rullkoetter PJ. Computational analysis of factors contributing to patellar dislocation. Journal of Orthopaedic Research 2015. September 1. PMID: 26331373. [DOI] [PubMed] [Google Scholar]
- 12. Tensho K, Akaoka Y, Shimodaira H, et al. What components comprise the measurement of the tibial tuberosity-trochlear groove distance in a patellar dislocation population? J Bone Joint Surg [Am] 2015;97:1441-8. PubMed PMID: 26333740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Camathias C, Pagenstert G, Stutz U, Barg A, Muller-Gerbl M, Nowakowski AM. The effect of knee flexion and rotation on the tibial tuberosity-trochlear groove distance. Knee Surg Sports Traumatol Arthrosc 2015; 21 January. PMID: 25605559. [DOI] [PubMed] [Google Scholar]
- 14. Reilly DT, Martens M. Experimental analysis of the quadriceps muscle force and patello-femoral joint reaction force for various activities. Acta Orthop Scand 1972;43:126-37. PMID: 5079747. [DOI] [PubMed] [Google Scholar]
- 15. Lai KA, Shen WJ, Lin CJ, Lin YT, Chen CY, Chang KC. Vastus lateralis fibrosis in habitual patella dislocation: an MRI study in 28 patients. Acta Orthop Scand 2000;71:394-8. PMID: 11028889. [DOI] [PubMed] [Google Scholar]
- 16. Dejour H, Walch G, Neyret P, Adeleine P. La dysplasie de la trochlee femorale. [Dysplasia of the femoral trochlea]. Rev Chir Orthop Repar Appar Mot 1990;76:45-54. PMID: 2140459. [PubMed] [Google Scholar]
- 17. Galland O, Walch G, Dejour H, Carret JP. An anatomical and radiological study of the femoropatellar articulation. Surg Radiol Anat 1990;12:119-25. PMID: 2396177. [DOI] [PubMed] [Google Scholar]
- 18. Thevenin-Lemoine C, Ferrand M, Courvoisier A, et al. Is the Caton-Deschamps index a valuable ratio to investigate patellar height in children? J Bone Joint Surg [Am] 2011;93:e35. PMID: 21508270. [DOI] [PubMed] [Google Scholar]
- 19. Jaquith BP, Parikh SN. Predictors of recurrent patellar instability in children and adolescents after first-time dislocation. Journal Pediatr Orthop 2015; October 21. PMID: 26491910. [DOI] [PubMed] [Google Scholar]
- 20. Staubli HU, Durrenmatt U, Porcellini B, Rauschning W. Anatomy and surface geometry of the patellofemoral joint in the axial plane. J Bone Joint Surg [Br] 1999;81:452-8. PMID: 10872365. [DOI] [PubMed] [Google Scholar]
- 21. Nietosvaara Y, Aalto K. The cartilaginous femoral sulcus in children with patellar dislocation: an ultrasonographic study. Journal of Pediatr Orthop 1997;17:50-3. PMID: 8989701. [PubMed] [Google Scholar]
- 22. Camathias C, Rutz E, Gotze M, Brunner R, Vavken P, Gaston MS. Poor outcome at 7.5 years after Stanisavljevic quadriceps transposition for patello-femoral instability. Arch Orthop Trauma Surg 2014;134:473-8. PMID: 24509939. [DOI] [PubMed] [Google Scholar]
- 23. Vavken P, Wimmer MD, Camathias C, Quidde J, Valderrabano V, Pagenstert G. Treating patella instability in skeletally immature patients. Arthroscopy 2013;29:1410-22. PMID: 23714402. [DOI] [PubMed] [Google Scholar]
- 24. Regalado G, Lintula H, Kokki H, Kroger H, Vaatainen U, Eskelinen M. Six-year outcome after non-surgical versus surgical treatment of acute primary patellar dislocation in adolescents: a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc 2016;24:6-11. PMID: 25193570. [DOI] [PubMed] [Google Scholar]
- 25. Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg [Am] 2008;90:463-70. PMID: 18310694. [DOI] [PubMed] [Google Scholar]
- 26. Niedzielski KR, Malecki K, Flont P, Fabis J. The results of an extensive soft-tissue procedure in the treatment of obligatory patellar dislocation in children with ligamentous laxity: a post-operative isokinetic study. Bone Joint J 2015;97-B:129-33. PMID: 25568426. [DOI] [PubMed] [Google Scholar]
- 27. Grammont PM, Latune D, Lammaire IP. Die behandlung der subluxation und luxation der kniescheibe beim kind. technik von elmslie mit beweglichem weichteilstiel (8-jahres-ubersicht) [Treatment of subluxation and dislocation of the patella in the child. Elmslie technic with movable soft tissue pedicle (8 year review)]. Der Orthopade 1985;14:229-38. PMID: 4069700. [PubMed] [Google Scholar]
- 28. Kraus T, Lidder S, Svehlik M, Rippel K, Schneider F, Eberl R, et al. Patella re-alignment in children with a modified Grammont technique. Acta Orthop 2012;83:504-10. PMID: 23039166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP. Anatomy and biomechanics of the medial patellofemoral ligament. Knee 2003;10:215-20. PMID: 12893142. [DOI] [PubMed] [Google Scholar]
- 30. de Oliveira V, de Souza V, Cury R, et al. Medial patellofemoral ligament anatomy: is it a predisposing factor for lateral patellar dislocation? Int Orthop 2014;38:1633-9. PMID: 24817023. P [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Arai Y, Nakagawa S, Higuchi T, et al. Comparative analysis of medial patellofemoral ligament length change pattern in patients with patellar dislocation using open-MRI. Knee Surg Sports Traumatol Arthrosc 2015; July 8. PMID: 26154483. [DOI] [PubMed] [Google Scholar]
- 32. Von Knoch F, Bohm T, Burgi ML, von Knoch M, Bereiter H. Trochleaplasty for recurrent patellar dislocation in association with trochlear dysplasia. A 4- to 14-year follow-up study. J Bone Joint Surg [Br] 2006;88:1331-5. PMID: 17012423. [DOI] [PubMed] [Google Scholar]
- 33. Bengtsson Mostrom E, Lammentausta E, Finnbogason T, Weidenhielm L, Janarv PM, Tiderius CJ. Pre- and postcontrast T1 and T2 mapping of patellar cartilage in young adults with recurrent patellar dislocation. Magnet Reson Med 2015;74:1363-9. PMID: 25421491. [DOI] [PubMed] [Google Scholar]
- 34. Kita K, Tanaka Y, Toritsuka Y, et al. Patellofemoral chondral status after medial patellofemoral ligament reconstruction using second-look arthroscopy in patients with recurrent patellar dislocation. J Orthop Sci 2014;19:925-32. PMID: 25104603. [DOI] [PubMed] [Google Scholar]