Abstract
There are three main patterns of complex elbow instability: posterolateral (terrible triad), varus posteromedial (anteromedial coronoid fracture with lateral collateral ligament complex disruption), and trans-olecranon fracture dislocations.
Radial head fractures, in the setting of complex elbow instability, often require internal fixation or arthroplasty; the outcome of radial head replacement is dictated by adequate selection of the head diameter, correct restoration of radial length, and proper alignment and tracking.
Small coronoid fractures can be ignored. Larger coronoid fractures, especially those involving the anteromedial facet, require fixation or graft reconstruction, particularly in the presence of incongruity.
The lateral collateral ligament complex should be repaired whenever disrupted. Medial collateral ligament disruptions seem to heal reliably without surgical repair provided all other involved structures are addressed.
The most common mistakes in the management of trans-olecranon fracture dislocations are suboptimal fixation, lack of fixation of coronoid fragments, and lack of restoration of the natural dorsal angulation of the ulna.
Cite this article: Sanchez-Sotelo J, Morrey M. Complex elbow instability. EFORT Open Rev 2016;1:183-190.
Keywords: elbow, radial head, instability, coronoid
Introduction
Traumatic elbow injuries commonly result in damage to several of the elbow structures involved in joint stability. Persistent elbow instability after injury often results in pain, poor function and progressive joint degeneration. To prevent persistent instability after these injuries, the surgeon must decide which structures require surgical repair or reconstruction and how to best deal with each of these.1
The term ‘complex elbow instability’ was introduced to emphasise the fact that many elbow fracture-dislocations or fracture-subluxations require the addressing of two or more structures surgically in order to re-establish stability and function, and to avoid rapid onset of osteoarthritis (Fig. 1).2-4
Fig. 1.

Lateral radiograph obtained after a posterolateral fracture dislocation (a). Fracture comminution of the radial head and coronoid are best appreciated by computed tomography (b).
Complexity exists at multiple levels: decision-making, surgical techniques and post-operative management. Deciding which elements need to be fixed can be challenging: on the one hand, failure to repair or reconstruct a given structure may be very unforgiving; while on the other, fixing all injured structures may add complexity and morbidity to the case. Deciding how to fix each specific structure may also be a challenge, and post-operative rehabilitation needs to take into account the nature of the injury as well as the type of surgery performed.
When confronted with an elbow fracture-dislocation, many surgeons ask themselves the same questions: is the radial head fractured? Is it best to fix it or replace it? Do I have to fix or reconstruct all coronoid fractures, and if so how? When do I need to repair the medial collateral ligament? What is the best exposure for the more complex cases? What is the role of external fixation, and should it be dynamic or static? What if there is an associated Essex-Lopresti injury? Do I add prophylaxis to prevent heterotopic ossification? How do I balance protection against recurrent instability and efforts to regain motion?
In this review article, we will try to clarify how to best use current knowledge and evidence to answer some of these questions. Longitudinal instability of the forearm adds another level of complexity and exceeds the scope of this article.
A few basic concepts
The biomechanics of the elbow joint, with simulation of various injury patterns, have been studied in detail by many authors.5-7 Interestingly, a number of studies have found conflicting evidence. In this study, we will summarise our interpretation of the available literature on the basic science of elbow stability.
Elbow loads with daily activities
Use of the elbow joint for various activities results in different loads. When we position the upper extremity in space to perform activities with our hands (typing on a keyboard, picking up an object from the floor, for example), the elbow is positioned such that the lateral aspect is facing up and the medial aspect facing down. In this position, the weight of the forearm and hand plus any object held will lead to tensile stresses laterally and compressive stresses medially (Fig. 2). In this position, the lateral collateral ligament complex resists lateral tensile stresses leading to elbow subluxation or dislocation, whereas contact between the medial trochlea and anteromedial coronoid resists compressive loads.
Fig. 2.
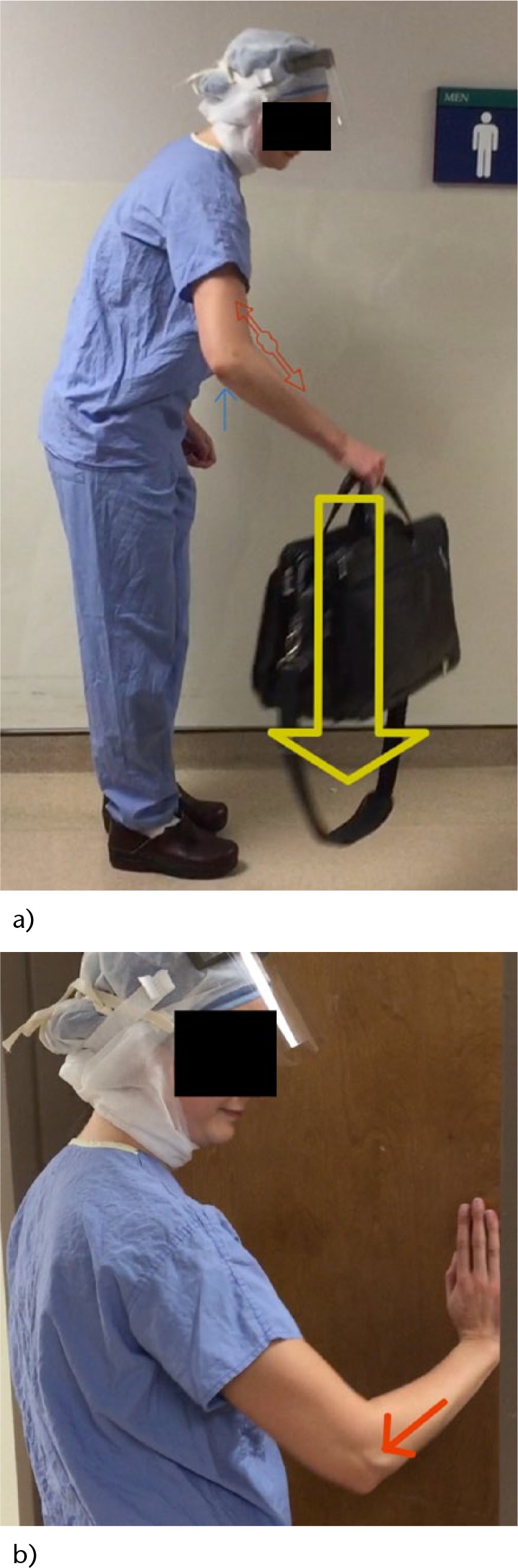
a) Gravitational stresses tend to stretch the lateral collateral ligament complex (red arrow-heads) and shear or compress the anteromedial coronoid (blue arrow); b), the radial head transmits a fair amount of load when the upper extremity is used to push an object.
Consideration of these gravitational stresses on the elbow joint is paramount to understand how to protect the lateral collateral ligament after injury or surgery, and it also explains how relatively small anteromedial coronoid fractures may lead to substantial biomechanical abnormalities that can only be detected with gravity-assisted varus or forced varus stress.
Let us consider a completely different set of activities, such as pushing open a door, supporting the body weight when performing push-ups or riding a bicycle, or getting up from a seat pushing with the arms. In these activities, the radial head transmits at least 60% of the load to the humerus, the medial collateral ligament complex resists pure valgus loads, and the lateral collateral ligament complex resists posterolateral forearm rotation in relationship to the distal humerus. In these circumstances, the radial head and medial collateral ligament help each other to avoid excessive displacement with valgus stress, the radial head and the lateral collateral ligament contribute to stability against posterolateral subluxation, and the radial head is mostly responsible for longitudinal stability of the forearm along with the interosseous membrane and the distal radio-ulnar joint.
Individual elements of elbow stability
In the presence of an intact distal humerus, a number of bones, ligaments and muscle-tendon units contribute to elbow stability. The contribution of each of these structures depends on the nature (severity and location) of the injury, the loading mode, and their complex interplay with other injured structures. The radial head and the coronoid can be visualised as a single anterior wall preventing anterior escape of the distal humerus (posterior escape of the forearm). The radial head becomes especially important against pure axial loads, posterolateral and valgus stress, whereas the coronoid becomes especially important against varus and posteromedial rotation.
The relative contributions of the anterior, lateral or posterior aspects of the radial head will depend on the position of forearm rotation. Since fixation of radial head fractures restores the whole radial head, the question is what to do when the radial head is unfixable: does it need to be replaced or can it be excised? As a general rule, excision is only acceptable in the truly isolated radial head fracture, i.e. in the absence of complex instability. Otherwise, the radial head can be left alone when either non-fractured or when fracture displacement is under 2 mm, or it needs to be fixed or replaced.
Defining the critical size of a coronoid fracture that needs to be fixed in order to avoid persistent instability has been much more elusive and controversial.8 Early studies prior to the widespread use of CT based that decision on plain lateral radiographs; internal fixation was recommended when the amount of fracture exceeded 50% of the height of the coronoid. With the advent of CT with three-dimensional rendering, the understanding of coronoid fracture patterns has been re-defined.9 Fractures involving the tip of the coronoid are typically seen as a consequence of posterolateral injury patterns, and may not lead to persistent instability provided the lateral column and lateral collateral ligament complex are intact. Fractures involving the anteromedial coronoid often result from a posteromedial injury pattern and may be well tolerated provided there is no incongruity and the lateral collateral ligament complex is intact; they can also lead to rapid progression of joint degeneration when incongruous.
The lateral collateral ligament complex seems to be important to resist both gravitational stresses and axial loading, and most authors agree on the need to repair it in all patients undergoing surgery for complex elbow instability. Commonly overlooked is the effect of the radial head on tension of the lateral collateral ligament: absence of the radial head will de-tension these ligamentous fibres by allowing relative collapse of the lateral column of the elbow, and also by absence of the bulk of the radial head width. The anterior band of the medial collateral ligament is different: substantial stress requires almost pure valgus load, such as with throwing, and this short, flat ligament, not subjected to gravitational stresses, seem to heal more reliably than its lateral counterpart.
Patterns of complex elbow instability
Loads across the elbow joint at the time of injury seem to lead to specific patterns of complex elbow instability.
Posterolateral rotatory injuries: the terrible triad
In this injury pattern, the forearm is axially loaded while rotating posterolaterally relative to the humerus. If the degree of rotation is large enough for the radial head and coronoid to clear underneath the distal humerus, a simple dislocation occurs. Otherwise, the distal humerus shears off and fractures the radial head and coronoid. The resultant injury is known as elbow ‘terrible triad’ (Fig. 1): three elements are injured (radial head, coronoid and lateral collateral ligament complex) and the outcome is poor when not perfectly managed. The medial collateral ligament is injured in many but not all cases (sometimes the elbow will hinge around an intact medial collateral ligament). Not uncommonly there are traumatic injuries to the capitellum, either small osteochondral injuries or larger posterior impaction fractures.
Posteromedial rotatory injuries: anteromedial coronoid fractures
This injury pattern is less common and easy to miss on plain radiographs. Loads at the time of injury lead to posteromedial rotation of the forearm relative to the distal humerus combined with excessive varus. The medial trochlea fractures the anteromedial coronoid with distal displacement and various degrees of impaction and comminution.10 Most of the time, the coronoid fracture line exits at the level of the anterior aspect of the sublime tubercle (Fig. 3). Tensile stresses lead to concomitant avulsion of the humeral origin of the lateral collateral ligament complex and disruption of the posterior band of the medial collateral ligament. Most of the time, the radial head is intact.
Fig. 3.
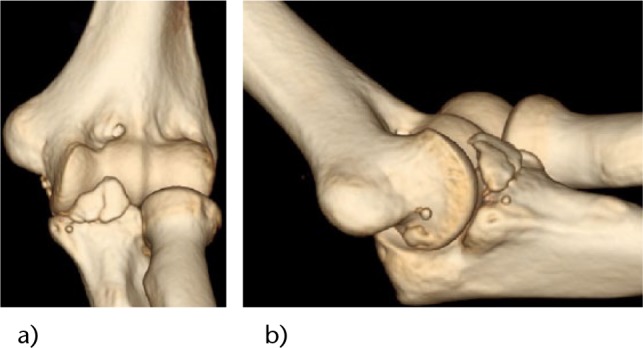
A displaced anteromedial coronoid fracture with an intact radial head; an avulsion of the lateral collateral ligament complex occurs through a varus posteromedial mechanism.
Trans-olecranon fracture-dislocations
In this particular pattern, the distal humerus is driven across the greater sigmoid of the ulna, resulting in a fracture of the olecranon with various degrees of extension into the coronoid or the proximal ulnar shaft (Fig. 4).
Fig. 4.

Lateral radiograph after a trans-olecranon fracture-dislocation.
The radius may migrate posteriorly with the distal forearm or it may disassociate from the ulna (Monteggia equivalent). Most of the time, ligamentous disruption occurs through bone fragments, so that once the bones are fixed, ligament repair or reconstruction is not required.
Management of individual structures
Radial head
In general, radial head fractures may be treated conservatively, with resection of the fractured fragments (partial resection) or the whole radial head, or with internal fixation or arthroplasty. In the setting of complex elbow instability, fracture displacement typically exceeds the limits of conservative treatment, and resection of part or the whole radial head aggravates instability. Usually, only one question remains: internal fixation or replacement?11,12 Factors influencing this decision include fracture comminution, bone loss, age and bone quality.
Internal fixation seems to be reliable when the number of fractured fragments does not exceed three, especially if at least a portion of the radial head is still intact in continuity with the neck. Replacement is considered for fractures with four or more fragments, when the head is completely fractured off the neck, as well as in older patients with poor bone quality.
Internal fixation
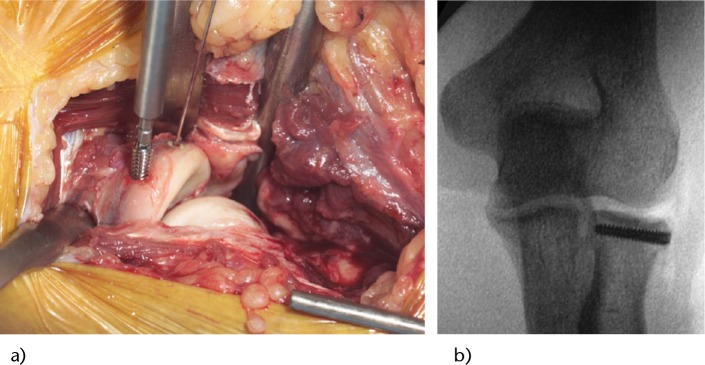
Since only relatively more simple radial head fractures are considered for internal fixation, screw fixation is most of the time the modality of choice. Most surgeons prefer headless compression screws of various sizes (Fig. 5). In the younger patient with a fracture of the whole humeral head, plate fixation may be considered, but it seems to be associated with worse forearm rotation; alternatively, oblique ‘tripod’ screw fixation may be considered. Comminution at the head-neck junction may require structural bone grafting.
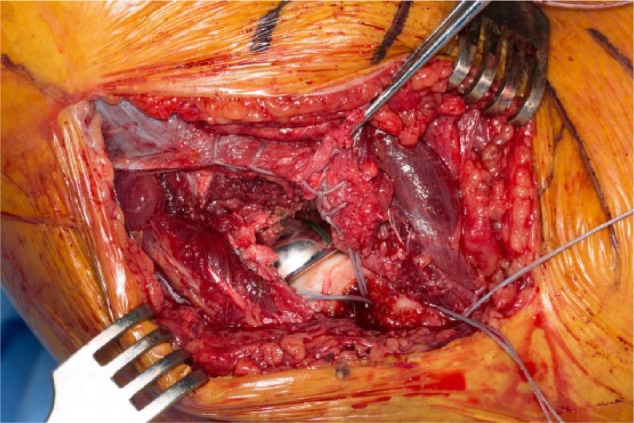
Fig. 5.
Internal fixation of radial head fractures is commonly performed using headless compression screws. a) Intra-operative photograph; b). intra-operative fluoroscopy.
Radial head replacement
When internal fixation is anticipated to be unreliable, a stable lateral column is recreated with implantation of an arthroplasty. Controversy remains regarding the ideal features of radial head implants.13 Five technical aspects require specific attention: diameter, length, alignment and tracking, and fixation:
Diameter
Poor selection of the diameter of the radial head will lead to issues with tracking and stability. A relatively narrow radial head will lead to point contact pressures on the capitellar cartilage, poor tracking, and incomplete tensioning of the lateral collateral ligament complex. Excessively large heads abut against the lesser sigmoid notch and lateral trochlear ridge: the laterally-displaced head tracks poorly and may lead to capitellar damage and restricted motion. Since the radial head is oval, and not circular, sizing of circular implants may be tricky. Currently, use of the smaller diameter of the removed radial head to select the diameter or circular implants is recommended. Anatomical implants are sized to the two dimensions of the non-circular radial head, selecting the smaller size when in doubt.
Length
Currently, a number of implants allow adjustments of length independent of the diameter selected. The most common reported mistake has been using too long a prosthesis, resulting in radial overlengthening (‘overstuffing’) which gaps open the elbow joint, lengthens the lateral collateral ligament complex, and leads to increased pressure on the capitellum, limited motion and pain (Fig. 6).
Fig. 6.

Radiograph obtained after radial head replacement with excessive lengthening of the radius will lead to a poor outcome.
Multiple methods have been recommended to get the radial length correct, such as:
Implant dish should be at the level of the lateral coronoid
Implant height should be co-linear with the lesser sigmoid notch (consider intra-operative use of an angled dental mirror)
The trial implant should contact the capitellum without distraction of the lateral ulno-humeral joint line (consider use of specific guides)
Intra-operative fluoroscopy should confirm parallel subchondral lines at the medial and lateral sides of the ulnohumeral joint (compare with opposite side).
Alignment and tracking
The axis of forearm rotation is accepted to bisect the radial head proximally and the ulnar styloid distally. The radial neck cut and prosthesis should be aligned perpendicular to this line. Some systems provide guides to confirm the overall alignment; others base alignment on use of a planer inserted tight into the radius. Once the trial is believed to be properly sized and aligned, proper tracking should be confirmed intra-operatively by visual inspection during flexion, extension, pronation and supination. If tracking is poor, sizing, length and alignment need to be reassessed and corrected. Alternatively, a bipolar prosthesis may be used.5 However, bipolar implants may be more prone to elbow subluxation14 and also carry the risk of polyethylene wear. Our preference is to use monopolar implants whenever possible.
Fixation
Cementless fixation is successfully achieved in other diaphyseal bones, such as the humerus or femur. Successful bone ingrowth requires intimate contact, limited micromotion, and a bone-friendly surface (Fig. 7). Unfortunately, to obtain adequate press-fit at the radius, bone preparation may create cracks and lead to poor early implant stability. Cemented fixation is thus favoured by some authors. Some surgeons favour the use of an implant with a polished stem that floats in the canal. Thus loose-fitting implants can self-align with motion but may lead to forearm pain. Our current preference is to aim for cementless fixation, but have a low threshold to cement the implant if concerns arise intra-operatively.
Fig. 7.
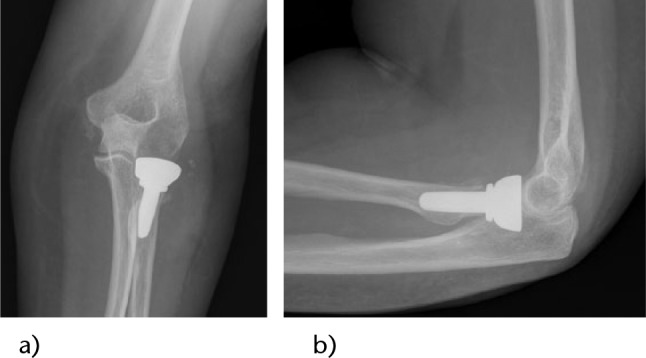
Anteroposterior a) and lateral b) radiographs after radial head replacement using an uncemented implant.
Coronoid fractures
The key questions to answer regarding coronoid fractures are threefold: is the remaining unfractured coronoid large enough to prevent instability?6 What is the best approach to get to specific patterns of coronoid fracture? What are the best options to fix or re-construct the coronoid?15
When to address the coronoid surgically
In terrible triad injuries, the fracture line is either transverse or oblique towards the lateral side.16 We tend to ignore fractures affecting up to 30% of the height and fix or reconstruct all others, but each patient is assessed individually and the recommendation may change based on body habitus, associated injuries, and intra-operative assessment.17 In valgus posteromedial injuries, fracture fixation is recommended if there is incongruity with the elbow in 90° of flexion, if there is grinding with motion under gravity-assisted varus stress or if the fractured fragment exceeds 5 mm, and is also considered for fragments larger than 2.5 mm.18 In trans-olecranon fracture-dislocations, most associated coronoid fractures are large and require fixation to the rest of the ulna.
Options for exposure
In trans-olecranon fracture-dislocations, coronoid fragments can usually be exposed through the fracture site before fixing the olecranon piece. Only fractures with severe comminution and large anterior cortical extension may require extension of the exposure medially to add a second anteromedial buttress plate.
Anteromedial coronoid fractures secondary to valgus posteromedial rotation with an intact radial head are best approached medially.19 Our current preference is to selectively decompress but not transpose the ulnar nerve, and expose the fracture by splitting the common flexor group in line with the anterior margin of the medial epicondyle and anterior fibres of the medial collateral ligament complex. The anterior portion of the common flexor-pronator group is mobilised anteriorly and distally.
Coronoid fractures in the setting of terrible triads can often be approached laterally: injury to the lateral collateral ligament complex allows the surgeon to ‘book-open’ the elbow. Exposure is substantially easier if the radial head needs to be replaced: resection of the fractured fragments provide good working space. Additional medial exposure is considered only if the medial collateral ligament will be repaired or if buttress plate fixation is deemed necessary.
Fixation and reconstruction
Fixation of the fractured fragments is preferred; however, sometimes stable fixation cannot be achieved due to either severe comminution or osteopenia. In these circumstances, the coronoid may be reconstructed in the acute setting with a graft. If the radial head is to be resected and replaced, a fragment of the fractured radial head can be used as autograft. Otherwise autograft may be obtained from the tip of the olecranon or a costochondral joint, or allograft radial head or coronoid may be considered.20,21
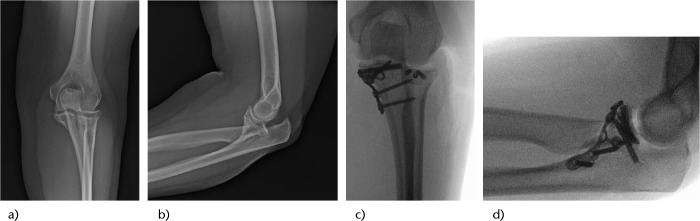
Retrograde fixation with threaded Kirschner wires or cannulated screws is our modality of choice for both fixation of fractured fragments or grafts (Fig. 8). A small incision is placed over the subcutaneous border of the ulna and wires or screws are inserted towards the fracture site. Aiming guides are useful. Plates are considered for larger fragments requiring buttressing, most commonly large anteromedial fractures.
Fig. 8.
Large coronoid fractures may require a medial exposure for reduction and plate fixation. Radiographs: a) pre-operative AP; b) pre-operative lateral; c) post-operative AP; d) post-operative lateral.
Lateral collateral ligament
The lateral collateral ligament complex seems to be injured in most ‘terrible triads’ and varus posteromedial injuries. In the acute setting, repair seems to work well and reconstruction with a tendon graft is seldom considered. The key is to perform a secure repair (Fig. 9). We favour the use of non-absorbable sutures placed along the course of the lateral collateral ligament complex in a locking-running fashion and re-attached slightly proximal and anterior to the centre of the lateral epicondyle using transosseous sutures or an anchor.
Fig. 9.
Formal repair of the lateral collateral ligament complex using heavy non-absorbable suture through bone tunnels.
Medial collateral ligament and external fixation
In our experience, most elbows are stable once the coronoid, radial head and lateral collateral ligament complex are addressed surgically. However, in some patients with severe soft-tissue stripping off the humerus, the elbow may tend to subluxate as it is brought into progressive extension in the operating room. If the subluxation occurs despite keeping the elbow at 60°, we consider a medial soft-tissue repair or adding a temporary external fixator.
Medial exposure of the elbow does add some morbidity. Soft-tissue disruption often includes not only the medial collateral ligament but also the common flexor pronator group. All disrupted soft tissues are repaired to the medial epicondyle as described for the lateral side.
Alternatively, a fixator may be used for a few weeks.22,23 Aligning a dynamic external fixator with the axis of flexion and extension of the elbow is not easy. If there are concerns regarding the axis, a static fixator may be used or the dynamic fixator may be locked with an additional bar. However, if a dynamic fixator can be placed properly, the patient can initiate motion exercises while in the fixator immediately or once the soft tissues have calmed down.
Proximal ulnar shaft and olecranon
The most common mistakes in the management of trans-olecranon fracture-dislocations are failure to obtain a stable fixation, failure to include coronoid fragments in the fixation strategy, and failure to re-establish the posterior angulation of the dorsal cortex of the ulna.
Plate fixation is required almost universally for the ulnar component of this injury; tension-band wiring provides inadequate fixation most of the time. As mentioned before, substantial coronoid fragments must be included in the fixation strategy, either using screws through the plates, screws outside of the plate, a second dedicated coronoid plate or a combination.
Use of a straight plate posteriorly will head to an abnormally straight proximal ulna that may lead to anterior subluxation or dislocation of the radius. Modern pre-contoured plates incorporate certain angulation, but intra-operative plate bending may still be required.
If the fracture-dislocation has an associated fracture of the radial head, fixation or replacement of the radial head can be performed through the fracture site or through a separate lateral exposure. We favour a separate lateral exposure when replacement is selected in order to get the radial length correct. The trial radial head prosthesis is inserted first through a lateral approach in order to have a stable lateral column, fixation of the ulna is completed next, and the length of the neck of the prosthesis can be adjusted just prior to implantation. The radius can actually be slightly shortened to facilitate inter-fragmentary compression of the ulna in severely comminuted fractures.
Post-operative management
Management of complex elbow instability after surgery requires a fine balance between protection of all repaired structures and restoration of motion. In general, elbows prone to residual instability are more stable in flexion. Immediately after surgery, the elbow is immobilised typically using a splint in 90° of flexion for the first two to three post-operative weeks.
Active and active-assisted range of motion exercises are preferred over passive exercises: contraction of the muscles around the elbow creates a joint reaction force that increases elbow stability. It is important to avoid unnecessary gravitational stresses that may stretch the lateral collateral ligament complex repair or contribute to shear of anteromedial coronoid fractures. The patient is shown how to perform active-assisted flexion and extension lying supine and with the arm overhead. Pronation and supination are practiced with the elbow in 90° of flexion keeping the arm by the side of the trunk.
Use of radiation or a non-steroidal drug to prevent heterotopic ossification may carry some risk of fracture nonunion or interfere with bone ingrowth when cementless prostheses are used. It can be considered selectively in patients with a very high risk, such as open fracture-dislocations, severe associated chest injuries or delay in surgical treatment for a few days.24
Conclusions
Management of elbow fracture dislocations requires understanding the complex interaction of all structures involved in elbow stability. There are specific patterns of complex instability that result in predictable injuries of these various structures. Improved techniques and implants for fracture fixation and radial head replacement, combined with awareness of the importance of dedicated ligament repair, have translated into much better outcomes currently.
Footnotes
Conflict of Interest: JSS has received financial support outside the current work in the form of consultancy fees from Wright Medical Tornier.
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Athwal GS, Ramsey ML, Steinmann SP, Wolf JM. Fractures and dislocations of the elbow: a return to the basics. Instr Course Lect 2011;60:199-214. PMID:21553774. [PubMed] [Google Scholar]
- 2. de Haan J, Schep N, Tuinebreijer W, den Hartog D. Complex and unstable simple elbow dislocations: a review and quantitative analysis of individual patient data. Open Orthop J 2010;4:80-6. PMID:20361035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Morrey BF. Current concepts in the management of complex elbow trauma. Surgeon 2009;7:151-61. [DOI] [PubMed] [Google Scholar]
- 4. Tashjian RZ, Katarincic JA. Complex elbow instability. J Am Acad Orthop Surg 2006;14:278-86. PMID:16675621. [DOI] [PubMed] [Google Scholar]
- 5. Hartzler RU, Morrey BF, Steinmann SP, Llusa-Perez M, Sanchez-Sotelo J. Radial head reconstruction in elbow fracture-dislocation: monopolar or bipolar prosthesis? Clin Orthop Relat Res 2014;472:2144-50. PMID:24867446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hartzler RU, Llusa-Perez M, Steinmann SP, Morrey BF, Sanchez-Sotelo J. Transverse coronoid fracture: when does it have to be fixed? Clin Orthop Relat Res. 2014;472:2068-74. PMID:24585321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jeon IH, Sanchez-Sotelo J, Zhao K, An KN, Morrey BM. The contribution of the coronoid and radial head to the stability of the elbow. J Bone Joint Surg [Br]. 2012;94:86-92. [DOI] [PubMed] [Google Scholar]
- 8. Papatheodorou LK, Rubright JH, Heim KA, Weiser RW, Sotereanos DG. Terrible triad injuries of the elbow: does the coronoid always need to be fixed? Clin Orthop Relat Res 2014;472:2084-91. PMID:24474322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mellema JJ, Doornberg JN, Dyer GS, Ring D. Distribution of coronoid fracture lines by specific patterns of traumatic elbow instability. J Hand Surg Am 2014;39:2041-6. PMID:25070699. [DOI] [PubMed] [Google Scholar]
- 10. Sanchez-Sotelo J, O’Driscoll SW, Morrey BF. Medial oblique compression fracture of the coronoid process of the ulna. J Shoulder Elbow 2005;14:60-4. [DOI] [PubMed] [Google Scholar]
- 11. Watters TS, Garrigues GE, Ring D, Ruch DS. Fixation versus replacement of radial head in terrible triad: is there a difference in elbow stability and prognosis? Clin Orthop Relat Res 2014;472:2128-35. PMID:24136807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pike JM, Grewal R, Athwal GS, Faber KJ, King GJ. Open reduction and internal fixation of radial head fractures: do outcomes differ between simple and complex injuries? Clin Orthop Relat Res 2014;472:2120-7. PMID:24585322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Acevedo DC, Paxton ES, Kukelyansky I, Abboud J, Ramsey M. Radial head arthroplasty: state of the art. J Am Acad Orthop Surg 2014;22:633-42. PMID:25281258. [DOI] [PubMed] [Google Scholar]
- 14. Chanlalit C, Shukla DR, Fitzsimmons JS, Thoreson AR, An KN, O’Driscoll SW. Radiocapitellar stability: the effect of soft tissue integrity on bipolar versus monopolar radial head prostheses. J Shoulder Elbow 2011;20:219-25. [DOI] [PubMed] [Google Scholar]
- 15. Rouleau DM, Sandman E, van Riet R, Galatz LM. Management of fractures of the proximal ulna. J Am Acad Orthop Surg 2013;21:149-60. PMID:23457065. [DOI] [PubMed] [Google Scholar]
- 16. Adams JE, Sanchez-Sotelo J, Kallina CFt, Morrey BF, Steinmann SP. Fractures of the coronoid: morphology based upon computer tomography scanning. J SShoulder Elbow 2012;21:782-8. [DOI] [PubMed] [Google Scholar]
- 17. Chan K, MacDermid JC, Faber KJ, King GJ, Athwal GS. Can we treat select terrible triad injuries nonoperatively? Clin Orthop Relat Res 2014;472:2092-9. PMID:24549776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pollock JW, Brownhill J, Ferreira L, McDonald CP, Johnson J, King G. The effect of anteromedial facet fractures of the coronoid and lateral collateral ligament injury on elbow stability and kinematics. J Bone Joint Surg [Am] 2009;91:1448-58. PMID:19487524. [DOI] [PubMed] [Google Scholar]
- 19. Huh J, Krueger CA, Medvecky MJ, Hsu JR. Medial elbow exposure for coronoid fractures: FCU-split versus over-the-top. J Orthop Trauma 2013;27:730-4. PMID:23412510. [DOI] [PubMed] [Google Scholar]
- 20. Alolabi B, Gray A, Ferreira LM, Johnson JA, Athwal GS, King GJ. Reconstruction of the coronoid process using the tip of the ipsilateral olecranon. J Bone Joint Surg [Am] 2014. 2;96:590-6. PMID:24695926. [DOI] [PubMed] [Google Scholar]
- 21. Ring D, Guss D, Jupiter JB. Reconstruction of the coronoid process using a fragment of discarded radial head. J Hand Surg Am 2012;37:570-4. PMID:22305734. [DOI] [PubMed] [Google Scholar]
- 22. Sorensen AK, Sojbjerg JO. Treatment of persistent instability after posterior fracture-dislocation of the elbow: restoring stability and mobility by internal fixation and hinged external fixation. J Shoulder Elbow 2011;20:1300-9. [DOI] [PubMed] [Google Scholar]
- 23. Schep NW, De Haan J, Iordens GI, et al. A hinged external fixator for complex elbow dislocations: a multicenter prospective cohort study. BMC Musculoskelet Disord 2011;12:130. PMID:21658252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Foruria AM, Augustin S, Morrey BF, Sanchez-Sotelo J. Heterotopic ossification after surgery for fractures and fracture-dislocations involving the proximal aspect of the radius or ulna. J Bone Joint Surg [Am]. 2013;95:e66. [DOI] [PubMed] [Google Scholar]