Abstract
Anterior cruciate ligament (ACL) reconstruction is one of the most common procedures in sports medicine. Several areas of controversy exist in ACL tear management which have engaged surgeons and researchers in debates towards identifying an ideal approach for these patients.
This instructional review discusses the principles of ACL reconstruction in an attempt to provide guidelines and initiate a critical thinking approach on the most common areas of controversy regarding ACL reconstruction.
Using high-level evidence from the literature, as presented in randomised controlled trials, systematic reviews, and meta-analyses, operative versus conservative treatment, timing of surgery, and rehabilitation are discussed. Also, the advantages and disadvantages of the most common types of autografts, such as patellar tendon and hamstrings as well as allografts are presented.
Key considerations for the anatomical, histological, biomechanical and clinical data (‘IDEAL’) graft positioning are reviewed.
Cite this article: Paschos NK, Howell SM. Anterior cruciate ligament reconstruction: principles of treatment. EFORT Open Rev 2016;398-408. DOI: 10.1302/2058-5241.1.160032.
Keywords: anterior cruciate ligament, ACL tear, reconstruction, timing, rehabilitation, autograft, allograft, tunnel position
Introduction
Anterior cruciate ligament (ACL) reconstruction is one of the most common orthopaedic techniques performed worldwide. ACL injuries occur with increasing incidence, from approximately 33 cases in 100 000 in 1994 to between 40 and 60 incidents in 100 000 in 2014. Individuals participating in organised sport activities are most affected.1-4 It is estimated that approximately 200 000 ACL reconstructions are performed each year in the USA alone, a number expected to increase further as a result of increased participation in athletic activities by adolescents and young adults.1,2,5
It is of paramount importance to understand the long-term consequences that develop as a result of an ACL tear. The incidence of knee osteoarthritis (OA) increases to between approximately 15% and 20% after an ACL tear, which represents a ten-fold increase.6 It is suggested that more than 50% of patients that sustain an ACL injury will develop symptomatic OA in the following 10 to 20 years.7 When combined with a meniscectomy, an ACL tear can further increase the prevalence of OA.6 Specifically, in a cohort study with a ten year mean follow-up, the presence of intact menisci was associated with normal radiographic findings in approximately 88% of patients versus only 63% when meniscectomy was performed. When compared with meniscal injury alone, the ACL tear has been shown to cause radiographic changes at a younger age than meniscal tear, which indicates its importance.8
Despite the frequency in development of OA post-ACL injury, one of the main issues is whether ACL reconstruction can minimise the risk of osteoarthritis progression. Indeed, the reported incidence of osteoarthritis post-ACL reconstruction ranges from between 39% and 47% at seven years’ follow-up,9-11 and appears to increase to between 74% and 80% after a period of 13 to 15 years.12,13 Interestingly, of all the cases with degenerative arthritis only 40% were symptomatic.12,13 Male gender, increased BMI, time from injury to reconstruction and previous meniscectomy as well as presence of cartilage degeneration in the medial compartment at surgery were all associated with the future development of radiographic knee OA.11
A correlation between osteoarthritic changes and increased knee laxity was also suggested by some studies.13 Thus, the development of knee OA post-ACL tear is far more complex than initially suggested. ACL reconstruction appears to reduce the incidence of OA progression, but it does not fully restore knee function comparatively with the uninjured knee. Additional research is necessary to highlight further the initial phenomena that occur during knee injury, and to clarify whether the technique of ACL reconstruction can improve the prognosis and slow or reverse the natural history of the cartilage degeneration.
This review discusses the principles of ACL reconstruction in an attempt to provide guidelines and initiate a critical thinking approach on the most common areas of controversy regarding ACL reconstruction. Using information collected from systematic reviews and meta-analyses, this instructional review discusses operative versus conservative treatment, timing of surgery and rehabilitation as well as the principles of graft selection and ideal graft positioning.
Conservative versus surgical treatment
In young adults that desire to return to pre-injury activity, surgical management of an ACL tear is considered the ‘gold standard’ of care. The non-operative management of ACL-deficient knees has been proposed in the past as an alternative, but has been associated with poor functional outcome.14-18 Specifically, non-operative treatment resulted in poor and fair functional outcome scores that prevented a return to pre-injury activities in the majority of patients, as well as an increased incidence of secondary ACL and meniscus surgery.16-20 As a result, the more favourable outcome of ACL reconstruction establishes surgery as the first-line treatment for ACL-deficient knees in active patients.
While conservative treatment of ACL-deficient knees fell out of favour in the last ten to 15 years due to poor outcomes,14-20 a recent randomised controlled trial (RCT) suggested that some patients with certain characteristics can be effectively managed non-operatively.21,22 It was suggested that a structured rehabilitation programme with optional ACL reconstruction at a later stage, if needed, could result in similar outcomes to early ACL reconstruction.21 This study was criticised because of problematic design and data interpretation.23 Specifically, 23 of 59 patients (39% in the optional surgery group) underwent ACL reconstruction.21 Furthermore, an increased percentage of patients suffered from instability and meniscal complaints (32% and 22% versus 3% and 2% for optional and early ACL reconstruction groups, respectively).21 Previous reports showed a higher risk of symptomatic instability and late meniscus tear with conservative management.15,17 Therefore, the morbidity and associated risk of late knee injuries appears to significantly exceed any potential benefits of a conservative approach, especially in young active patients who wish to return to pre-injury activity levels.
The frequency of subsequent meniscal and chondral injuries in ACL-deficient patients is higher in skeletally immature patients. An association between medial meniscal tears and time to ACL reconstruction was identified early in skeletally immature patients, suggesting that a delay in treatment may be aetiologically responsible for these meniscal injuries.24 Similar studies not only confirmed the above link but also identified an increased incidence of chondral injuries in association with medial meniscal tears.25,26 In prospectively-collected MRI data, it was suggested that approximately 20% of skeletally immature ACL-deficient patients would sustain a new meniscal injury within the next four years.27 As a consequence, the decision of whether to operate or not on an ACL injury in children should take into consideration the high risk of ensuing knee injuries and their associated long-term consequences.
Principles of ACL reconstruction
In ACL reconstruction technique, there are several debates that have engaged orthopaedic surgeons and researchers. Specifically, the timing of repair and rehabilitation and the type of graft used are areas of contention.28 Also, allograft versus autograft has also been a topic of controversy. Regarding the intervention type, the description of the double-bundle technique created expectations for a more anatomical technique, but there is dispute regarding the validity of this claim.29
Timing of repair and rehabilitation
Three main factors should be considered and balanced for the timing of ACL reconstruction. The increased incidence of meniscus and chondral injuries following delayed ACL reconstruction, the risk of arthrofibrosis associated with early ACL reconstruction, and the associated loss of muscle strength due to inactivity when surgery is delayed.
The number of patients that will sustain a meniscus tear in a previously intact meniscus at the time of ACL tear ranges from between 10% and 50%.30-32 In a retrospective analysis of 205 patients, the mean time from the initial injury to meniscus tear was between 11 and 32 months for those with an injury to one or both menisci respectively.33 For chondral lesions, as discussed above, the risk of cartilage degeneration following an ACL tear increases significantly, with most reports suggesting that 20% of chondral lesions occur at the time of the ACL injury, and another 20 to 30% developing later due to ACL deficiency.31,34
Arthrofibrosis - joint stiffness that prevents restoration of full range of motion (particularly the loss of the 5°to full extension) - has been associated with early ACL reconstruction. In a large retrospective analysis, 52% of patients who were operated on within the first week following their injury developed a loss of 5o extension while only 17% of patients operated on from day eight to day 21 developed arthrofibrosis. None of the patients treated after week three had loss of extension.35 A post-operative rehabilitation programme introducing full passive extension, early motion and immediate weight-bearing was associated with a lower rate of joint stiffness in ACL reconstructed knees.35,36 Interestingly, loss of extension was also seen in ACL reconstructions performed after six months following the initial injury.37 Arthrofibrosis was also described in approximately 8% of children and adolescents post-ACL reconstruction.38 Some studies reported an extremely low incidence of arthrofibrosis when rehabilitation is used, and questioned its existence as a clinical entity.35,39,40 Orthopaedic surgeons should be aware of the possibility of arthrofibrosis, avoid reconstruction within the first weeks of injury and introduce an appropriately-designed rehabilitation protocol.
Pre-operative rehabilitation programmes are also important to retain muscle strength while waiting for reconstruction. A pre-operative quadriceps strength deficit of 20% was found to be among the most important predictors of poor clinical outcome, associated with an approximately 15% decrease at two years post-operatively, when a deficit was present.41 Furthermore, quadriceps with strength lower than 85% compared with the contralateral side was associated with a lower score in hop tests and a lower, but not statistically significant, International Knee Documentation Committee (IKDC) functional score.42 Indeed, a rehabilitation exercise programme of five weeks’ duration in patients with ACL injury was shown to significantly improve their knee functional outcome.43
Interestingly, the timing of ACL reconstruction and autograft choice can also influence rehabilitation strategy. Early ACL reconstruction has been linked with delay in quadriceps recovery. Specifically, 80% of patients treated with delayed ACL reconstruction (mean 40 days) reached a 65% quadriceps strength at two months versus 53% of patients treated with early ACL reconstruction (mean 11 days), respectively.44 By six months, 73% of patients that had delayed ACL reconstruction (mean time from injury of 40 days) exhibited 80% muscle strength versus only 47% in those reconstructed early.44 Muscle weakness can also result from autograft harvesting for ACL reconstruction. A trend towards extensor and flexor muscle strength deficit was shown in ACL reconstructions when bone-patella-tendon-bone (BPTB) and hamstring (HST) autograft was used, respectively.45 Therefore, carefully designed rehabilitation applied both pre- and post-operatively aiming to preserve quadriceps strength and retain knee range of motion appears to be a strategically important step towards a successful outcome post-ACL reconstruction.46
Type of graft
The two most commonly-used autografts for ACL reconstruction are the patellar tendon (PT) (also known as a BPTB graft) and the hamstring tendon (HT). The general notion, as indicated by most RCTs and meta-analyses, is that both grafts exhibit excellent results with no differences between them regarding functional outcome and activity level.47 Strong advocators for each graft type exist, and certain advantages and disadvantages have been suggested in the literature for each graft.
Table 1.
Advantages and disadvantages of most commonly used autografts
| Patellar tendon | Hamstrings | |
|---|---|---|
| Advantages | • Higher strength • Lower re-tear rate • Earlier graft remodeling and healing • Better knee stability |
• Smaller incision/better cosmesis • Minor functional impairment from graft harvesting • Earlier regeneration of hamstrings |
| Disadvantages | • Higher incidence of anterior knee pain and kneeling pain • Increased incidence of OA post-ACL reconstruction • Higher rate knee extension deficit due to adhesions |
• Higher incidence of tunnel widening • Electromechanical delay in knee flexors/weakness |
OA, osteoarthritis; ACL, anterior cruciate ligament
Advantages of the patellar tendon graft
Biomechanical data comparing PT graft and HT with native ACL found that PT graft had a maximum load of 2730 N or 2900 N (depending on whether the central or middle portion of BPTB was tested), and a stiffness of approximately 57 MPa that is translated as being between approximately 160 to 170% stronger and 150% stiffer than native ACL.48 In contrast, HT components - semitendinosus and gracilis tendons - were found to have 1220 N and 840 N maximum load as well as 89 MPa and 112 MPa stiffness, corresponding to 70% and 49% of native ACL for load as well as 234% and 295% of native ACL for stiffness.48 Notably, the use of multiple stands resulted in doubling of maximum load and stiffness for both semitendinosus and gracilis tendons, and therefore the exact technique needs to be considered and related to the expected outcome.49 In summary, both grafts used in ACL reconstruction exceed the biomechanical strength and stiffness of native ACL and this has been proven to be a safe approach in an attempt to eliminate the risk of graft tear.28
One of the main advantages of the PT graft is the lower re-tear rate reported in comparison with hamstring graft. PT graft is believed to be associated with lower failure rate, with a meta-analysis showing an incidence of 1.9% graft failure versus 4.9% for HT graft.50 This was also confirmed in a meta-analysis of only level-I studies that showed a 7.2% and 15.8% failure rate for PT and HT, respectively. Another meta-analysis reported a lower rate, but it failed to show significance (2.5% vs 3.3%, RR 0.78, 95% CI 0.41 to 1.50) for PT and HT, respectively,28 while other analyses demonstrated no significance between the groups regarding failure rate.28,51,52
This led to the suggestion that graft fixation is also an important aspect of surgical failure. It is suggested that, depending on the graft used, the type of fixation should be adjusted accordingly.53-57 Specifically, it was found that interference screws offer the maximum load and stiffness properties for PT grafts, resembling those of native ACL.56 This is extremely important since PT graft is suggested to promote graft remodeling and healing due to the presence of the bone plug. In an animal study, maximum failure load was higher in PT grafts at three weeks in comparison with flexor tendon grafts, suggesting that PT graft may undergo earlier ligamentisation and revascularisation and that this may allow earlier return to activity.58-60 Biological strategies that may enhance graft healing are becoming popular; however additional research is needed before making any definite conclusions about their effectiveness.61-63
Finally, in some reports, PT graft was shown to be able to restore knee stability more closely. Indeed, in a meta-analysis the percentage of patients that exhibited a KT-1000 arthrometer side-to-side difference of < 3 mm was 73.8% versus 79% for hamstring patients (p < 0.05).50 Another meta-analysis of 22 studies with approximately 2000 patients showed a lower risk of positive pivot shift (RR = 0.7, 95% CI, 0.53 to 0.93; p = 0.01).52 Analysing eight studies with 550 patients, it was shown that PT was associated with a higher chance to return to pre-injury level of activity (OR = 1.48, 95% CI, 1.03 to 2.12; p = 0.03).52 The same trend was shown in a recent long-term RCT with follow- up at 15 years, suggesting that a higher percentage of patients reconstructed with PT grafts participated in sports-related activities (p = 0.05). This finding was in accordance with similar reports favouring the patellar graft for Lachman and pivot shift tests.28,51
Disadvantages of patellar tendon graft
Patellar tendon is associated with a higher percentage of anterior knee pain and kneeling pain. A recent meta-analysis of 12 studies, with data from approximately 850 patients, showed a significantly higher incidence of anterior knee pain in PT grafts (RR = 1.71, 95% CI, 1.35 to 2.16; p < 0.01).52 Kneeling pain was also worse in PT patients (RR = 2.05, 95% CI, 1.51 to 2.77; p < 0.01).52 In another meta-analysis, the patellar tendon group suffered from anterior knee pain in 17.4% versus 11.5% in the hamstrings group.50 The increased incidence of anterior knee pain and kneeling pain, as part of PT graft harvest morbidity is a consistent finding from multiple reports.51
Apart from pain during kneeling, another concern with PT grafts was the increased incidence of OA reported with PT compared with hamstring grafts (45% versus 14% of patients, respectively (p = 0.002).10 This was confirmed in a meta-analysis of studies with > five-year follow-up, where patellar graft was associated with higher incidence of radiographic osteoarthritis.64 Specifically, in four studies that included 290 patients, patellar tendon graft had a higher incidence of degenerative arthritis. (RR = 1.61, 95% CI, 1.08 to 2.4; p = 0.02).64 However, a higher incidence of meniscus surgery was present in the patellar tendon group, and not all studies were randomised.64 This finding has not been confirmed from other long-term reports,28,65,67 and it may be associated with the increased laxity found in the PT group at seven years versus two-year follow-up.10 However, further research with long-term follow-up studies is necessary in order to clarify whether this association exists.
Finally, patellar grafts were found to be associated with a higher rate of adhesions that would lead to manipulation under anaesthesia.50 This complication is probably related to the significant percentage of extension deficits found in patellar tendon graft patients. Specifically, in a meta-analysis sub-group of more than 1000 patients the risk of patellar tendon patients having an extension deficit > 3°was higher (1.71, 95% CI 1.25 to 2.33; p < 0.01). All of the above disadvantages are associated with a high degree of morbidity, also associated with PT graft reconstruction that could potentially lead to a lower performance and level of activity in PT graft-treated, high-performance athletes.49 As a consequence, it is suggested that the lower re-tear rate may be a result of lower participation in sports post-operatively.
Advantages of hamstring tendon
The main advantage of the hamstring tendon graft is the lower donor site morbidity associated with its harvesting. Indeed, hamstring harvesting may be a technically challenging technique, but it causes a smaller incision which results in better cosmetic appearance of the wound, an outcome that may be important in young female patients. Also, it causes significantly less anterior knee pain and less incidence of kneeling pain, as described above.28,50,52 Complications associated with hamstring graft are rather minor (for example, electromechanical delay in knee flexors and weakness) and are not proven to cause a functional impairment.68,69 Interestingly, most reports suggest a regeneration of hamstrings within two years from surgery, while patellar tendon reconstitution may be a more prolonged process.68,70-72
Disadvantages of hamstring tendon
Tunnel widening is reported more frequently with hamstring grafts. This was against the initial belief that, since hamstring graft fills the drilled tunnels completely, it would be associated with less tunnel widening. Specifically, it was found that tunnel increase was approximately double compared with patellar tendon graft (~20% versus ~10% and 25% versus 15% increase in tibial tunnel increase for anteroposterior and lateral views, p = 0.003 and p = 0.01, respectively). An animal study highlighted the importance of graft stiffness and graft hypertrophy due to remodeling for the development of tunnel widening.73 Three randomised controlled studies showed a higher percentage of femoral tunnel widening in patients treated with hamstring graft;14,47,74 however, only one of them reported significantly higher knee laxity in the hamstring group.47 Compaction of an autologous bone dowel into the tibial tunnel was shown to reduce the cross-sectional area of the tibial tunnel and prevent tunnel expansion in approximately 90% of patients after one to two years post-operatively.75
Allograft versus autograft
Allograft choices for ACL reconstruction are the patellar, Achilles, and tibialis tendon. The main advantages of allografts are the lack of donor site morbidity, shorter surgical time and the guarantee of adequate graft tissue. In contrast, allografts are associated with risk of disease transmission, potential delayed incorporation and immune response, while increased cost may be also a concern.
Table 2.
Advantages and disadvantages of allografts
| Allografts | |
|---|---|
| Advantages | • No donor site morbidity • Shorter surgical time • Ensure adequate graft length and diameter |
| Disadvantages | • Higher failure rate • Higher cost • Worse knee stability measured in some studies • Potential disease transmission and higher infection rate |
Advantages of allografts
Allografts have no associated donor site morbidity, which may be an important limitation for autografts, as seen in the percentage of anterior knee pain that affects up to 40% of patients.47,76 Furthermore, the operative time when allograft was used was significantly shorter compared with autograft, as shown in a meta-analysis comparing hamstring allograft and soft-tissue allograft (59 mins vs 77 mins, p = 0.008 respectively). Finally, in certain cases, the length and diameter of tissue used as an autograft can be variable and inadequate for the intended reconstruction.77 These issues are addressed with the use of an allograft. The importance of these factors can be underestimated in clinical assessment analysis, but all need to be considered; donor morbidity can adversely affect patient subjective outcome and the patient—physician relationship, while shorter surgical time is typically translated into the ability for the surgeon to perform an additional ACL reconstruction per day.
Disadvantages of allografts
Higher failure rate remains the main concern for allografts. In a prospective cohort design, ACL reconstructions using an allograft were demonstrated to have up to a four times higher failure rate when compared to those using an autograft.78 In a meta-analysis that included more than 5000 patients with patellar tendon allograft/autograft, it was also shown that allograft resulted in a three-fold increase in the re-rupture rate. In a meta-analysis including more than 500 patients, PT allografts were shown to have a higher risk of re-rupture compared with PT autografts (OR = 5.03, p = 0.01). Recently, a meta-analysis of nine RCTs and ten systematic reviews reported lower clinical failure for autograft (RR, 0.47; p = 0.0007).79 Two other meta-analyses failed to show a difference in clinical failure and re-operation rate between allografts and autografts.80,81 Interestingly, this difference was abolished when grafts processed with irradiation or chemicals were excluded,82 suggesting that graft irradiation and chemical processing is a critical factor for graft failure. Indeed, when analysed separately, BPTB non-irradiated allograft had a similar graft failure rate to autograft (8.8% and 6.1%, respectively).83 Despite the trend indicating a better performance for autograft, additional randomised controlled studies are important to resolve the existing controversies between allografts and autografts.
In terms of knee stability, the literature is extremely controversial. Allografts were shown to be associated with a higher percentage of unstable knee measurements compared with autografts (14% vs 5.3%) respectively.84 A meta-analysis of 38 studies that included data for more than 2500 patients showed that the percentage of patients with a side-to-side difference < 3 mm was 75.3% and 60.2% for autograft and allograft, respectively.85 Interestingly, functional outcomes were also in favour of autograft with better Lachman test (RR, 1.18; p = 0.03), and Tegner score (WMD, 0.36; p = 0.004).79 However, other reports found no difference; a meta-analysis of hamstring autograft versus soft-tissue allograft favoured slightly allograft for KT arthrometer laxity < 3 mm, (RR = 1.1, 95% CI 0.89 to 1.39), and Lachman negative (RR = 1.37, 95% CI 0.88 to 2.14) (81). A meta-analysis of six studies analysing approximately 650 patients also found no difference (RR = 1.19, CI 95% 0.63 to 2.24;p = 0.59, favouring allograft).80
ACL allograft has also been associated with higher costs and a higher infection rate. A statistically higher cost was reported for PT allograft with a total mean cost per case being US$4147 versus US$3154 for the PT autograft (p < 0.001).86 Another report that compared hamstring autograft and tibialis anterior allograft also showed a higher cost of approximately US$1000 for allograft (US$5195 vs US$4072, p < 0.001).87 However, some reports suggest that the cost of hospital stay may increase as a result of the higher possibility of overnight hospitalisation due to autograft donor site morbidity and increased surgical time.87 In a cost-effectiveness analysis, allografts were found to be the less cost-effective option.88 When evaluating cost, one should consider the risk of infection which is reported as higher in allografts.89 However, this finding was not confirmed in similar reports, showing no increased risk of infection with allograft tissue.88,90
IDEAL position characteristics
Proper positioning of the ACL graft has been proven to be of paramount importance for graft longevity. Malposition of the ACL graft, for example in anterior placement of the tibial tunnel, was associated with roof impingement.91 Roof impingement of the reconstructed ACL graft was recognised early as a significant factor that leads to graft failure.91-94 Furthermore, the degree of impingement was associated with an increased risk of ACL graft failure at two year-follow-up (100% in severe impingement vs 29% in moderate impingement).91 Therefore, it is reasonable to suggest that every attempt should be made to avoid malposition of the ACL graft.
The identification of the importance of proper placement of the ACL graft led to extensive study of the anatomical characteristics of the native ACL over the last decades, in an attempt to imitate these anatomical features during ACL reconstruction. The tibial and femoral osseous attachments of the ACL have been widely studied, and despite traditionally having an oval and crescent-like shape respectively, potential variations in their shape have been suggested.95,96 The anatomical characteristics of the attachments, in conjunction with the tendency to avoid impingement, led to interesting operative concepts, such as the meticulous placement of the ACL graft within the tibial and femoral footprints, i.e. complete footprint restoration.97
Following the same concept of anatomical ACL reconstruction based on the osseous attachments, the use of a double-bundle graft was proposed to replicate anteromedial and posterolateral bundles, as described in the native ACL.98,99 However, this technique did not clinically confirm the biomechanical findings, which suggested better rotational knee stability would result.100 Furthermore, the tension at the PL bundle in knee extension could be so high that could cause early graft rupture or attenuation.101 Currently, double-bundle reconstruction is rarely performed.5,102-104
Apart from the study of the attachments an increasing interest has developed with regard to the anatomical characteristics and shape of the ACL mid-substance. Specifically, it was recognised that the ACL has a smaller cross-sectional area at its mid-substance in comparison to that of its attachments.105 Furthermore, it was described that the ACL has a band-like shape along its length, and close to its tibial attachment it fans out like a trumpet to attach to the tibia.106 It is important to recognise the surgical implications rising from these observations, especially when realising that the posterior cruciate ligament occupies most of the area of the notch, leaving only a 5 mm slot for the ACL graft.106 Therefore, a more complex process is essential for ACL graft positioning in an attempt to incorporate the above anatomical, histological, isometric, and biomechanical features when making the decisions during ACL reconstruction.
Recently, useful guidance-instructions were described using the acronym IDEAL to summarise the important features of the ACL femoral tunnel position: I- isometric, D – direct, E- eccentric, A- anatomical, and L- low tension/flexion pattern which occurs in a full cycle of knee motion.
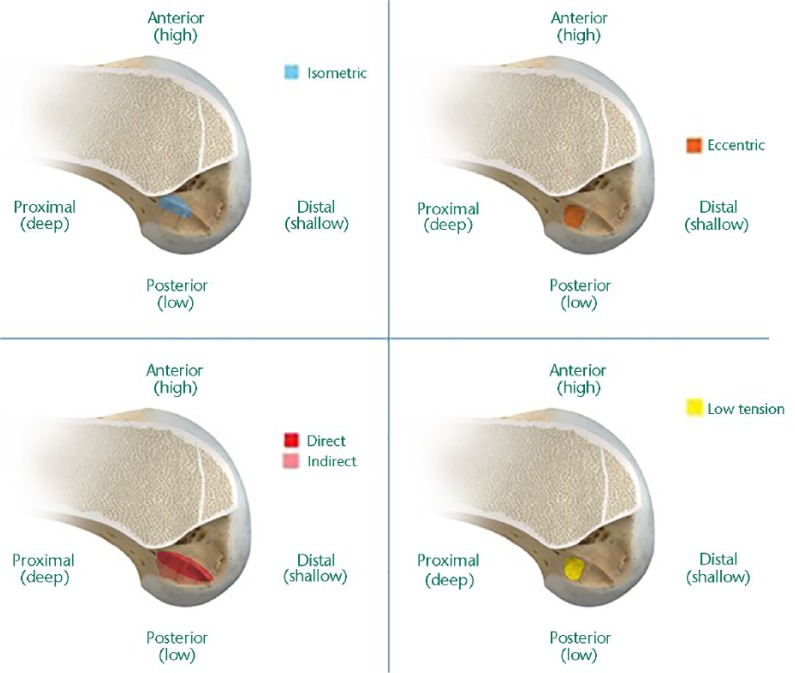
During knee flexion and extension, not all fibres of the ACL are under tension throughout a full cycle of flexion/extension.107,108 This is due to the changes in length observed during flexion, which results in the AM bundle being relaxed (elongated) and PL bundle being tight (shortened) at knee flexion.108,109. The AM bundle is considered the centre of rotation of the ACL, which suggests a more isometric behaviour of this bundle.109 Isometric studies suggested that the position at the femoral footprint that could potentially ensure isometry is located eccentrically, at the most anterior and superior (proximal) portion of the footprint, at the junction of the anteromedial and intermediate bundles (Fig. 1).108,110,111 This position was demonstrated that could ensure reproduction of the normal tension-flexion behaviour of the native ACL.5
Fig. 1.
Topographies at the femoral footprint that ensure isometric, eccentric, direct placement of the graft at a low-tension location.5
The collagen fibres at the femoral attachment belong to two distinct categories: the direct fibres, which are directly attached at the anterior portion of the osseous ACL insertion along the lateral intercondylar ridge, as well as the indirect fibres, that are less dense, lack the traditional four-layered structure of the ligamentous-bone attachment, and are located at the posterior portion of the ACL footprint.96 Due to their histological characteristics, indirect fibres are considered a weaker mechanical link than the direct ones, and, therefore, it is suggested that the femoral tunnel should be placed at the area of the direct fibre insertion (Fig. 1).5,96 Therefore, an area that 1) fulfills the above criteria of isometry, 2) is located within the footprint to avoid impingement, 3) restores the low flexion extension ACL pattern and 4) is located at the region of direct fibre insertion should be targeted for femoral tunnel position (Fig. 2).
Fig. 2.
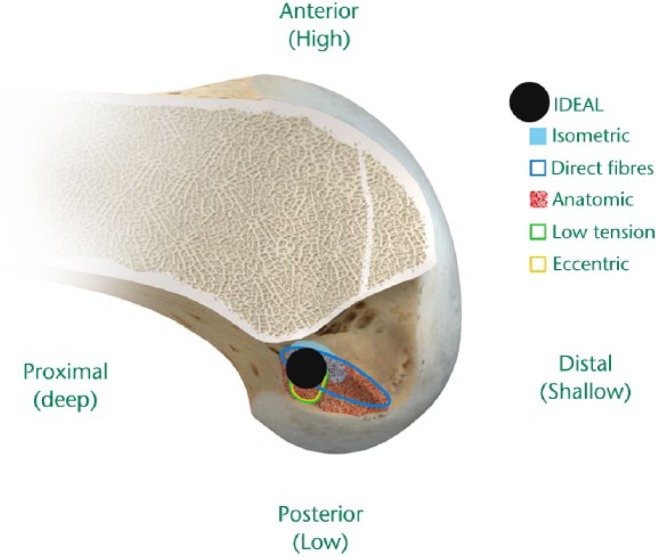
The correct or IDEAL location for the femoral tunnel (see black circle) is shown superimposed on the topographic outline of the five characteristics that should be fulfilled when judging where to position the femoral tunnel.
As discussed above, avoiding impingement is critical for graft survival. A graft that is positioning outside the anatomical margins of the footprints has a greater risk of impingement and, therefore, will eventually fail. Two different types of impingement exist: roof impingement and posterior cruciate ligament (PCL) impingement that occur differently and should be treated differently. For roof impingement, it is critical to make sure that the tibial tunnel entrance is just posterior to the intercondylar roof with the knee at maximum passive hyperextension position. Roof impingement is a clinical problem presenting in extension with two consequences, ie a loss of extension and/or increased laxity. PCL impingement occurs in knee flexion where the ACL graft lies on top of the PCL graft. In order to address this problem, the surgeon should ensure that there is adequate triangular space between the lateral edge of the graft and the medial border of the PCL. If adequate space exists, then the PCL impingement phenomenon cannot take place post-110° in knee flexion. Placing the graft within the native ACL footprints is suggested in order to ensure correct positioning of the graft with minimal risk of both roof and PCL impingement. It was shown that positioning the femoral tunnel at 60° in the coronal plane could lower graft tension by minimising the risk of the ACL graft impinging on the PCL during terminal flexion.112 As a result, the graft should be equidistant between the edge of the PCL and the lower edge of the femoral condyle notch to allow for this condition to exist (Fig. 1).
Finally, an important characteristic that is associated with high survival of the ACL graft is the avoidance of high loading experienced from the graft through the flexion—extension motion of the knee. It has been shown that a graft placed posteriorly experiences high loading forces in extension.101 In addition, positioning the graft low in the femoral condyle edge can cause high tension in extension. This explains the higher revision rate that has been shown in registry data with the AM portal technique, in comparison to the transtibial technique.113 In contrast, positioning of the graft anteriorly resulted in force patterns resembling those of the native ACL in both anterior translation and internal torque application.101 Therefore, low tension positioning means that the graft should be placed in an area of low tension, so that the graft will not be exposed to forces that can exceed its strength and cause it to fail (Fig. 1).
Summary
Anterior cruciate ligament tear is a detrimental event for every patient, and appropriate management is important in order to ensure return to pre-injury activity but also to prevent long-term complications due to the knee injury. Despite the presence of several controversies in ACL reconstruction, systematic research was able to provide answers to important questions. Surgical management of ACL tear appears to be the answer in patients who wish to restore their pre-injury activity level. Timing of reconstruction and rehabilitation are extremely important for a successful outcome. Each type of graft has specific advantages and disadvantages; therefore, careful selection of the graft for each patient is important. Finally, the surgical technique should follow the basic principles of ACL biomechanics and anatomy, ensuring ideal graft positioning and a successful clinical outcome.
Footnotes
Conflict of Interest: S. Howell reports personal fees from Zimmer Biomet, unconnected to this work.
Funding Statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Griffin LY, Agel J, Albohm MJ, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg 2000;8:141-150. [DOI] [PubMed] [Google Scholar]
- 2. Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med 2014;42:2363-2370. [DOI] [PubMed] [Google Scholar]
- 3. Parkkari J, Pasanen K, Mattila VM, Kannus P, Rimpelä A. The risk for a cruciate ligament injury of the knee in adolescents and young adults: a population-based cohort study of 46 500 people with a 9 year follow-up. Br J Sports Med 2008;42:422-426. [DOI] [PubMed] [Google Scholar]
- 4. Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy 2007;23:1320-5 e6. [DOI] [PubMed] [Google Scholar]
- 5. Pearle AD, McAllister D, Howell SM. Rationale for strategic graft placement in anterior cruciate ligament reconstruction: I.D.E.A.L. femoral tunnel position. Am J Orthop (Belle Mead NJ) 2015;44:253-258. [PubMed] [Google Scholar]
- 6. Gillquist J, Messner K. Anterior cruciate ligament reconstruction and the long-term incidence of gonarthrosis. Sports Med 1999;27:143-156. [DOI] [PubMed] [Google Scholar]
- 7. Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med 2007;35:1756-1769. [DOI] [PubMed] [Google Scholar]
- 8. Roos H, Adalberth T, Dahlberg L, Lohmander LS. Osteoarthritis of the knee after injury to the anterior cruciate ligament or meniscus: the influence of time and age. Osteoarthritis Cartilage 1995;3:261-267. [DOI] [PubMed] [Google Scholar]
- 9. Järvelä T, Paakkala T, Kannus P, Järvinen M. The incidence of patellofemoral osteoarthritis and associated findings 7 years after anterior cruciate ligament reconstruction with a bone-patellar tendon-bone autograft. Am J Sports Med 2001;29:18-24. [DOI] [PubMed] [Google Scholar]
- 10. Roe J, Pinczewski LA, Russell VJ, et al. A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: differences and similarities. Am J Sports Med. 2005;33:1337-1345. [DOI] [PubMed] [Google Scholar]
- 11. Li RT, Lorenz S, Xu Y, et al. Predictors of radiographic knee osteoarthritis after anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39:2595-2603. [DOI] [PubMed] [Google Scholar]
- 12. Oiestad BE, Holm I, Aune AK, et al. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med 2010;38:2201-2210. [DOI] [PubMed] [Google Scholar]
- 13. Salmon LJ, Russell VJ, Refshauge K, et al. Long-term outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft: minimum 13-year review. Am J Sports Med 2006;34:721-732. [DOI] [PubMed] [Google Scholar]
- 14. Aglietti P, Giron F, Buzzi R, Biddau F, Sasso F. Anterior cruciate ligament reconstruction: bone-patellar tendon-bone compared with double semitendinosus and gracilis tendon grafts. A prospective, randomized clinical trial. J Bone Joint Surg [Am] 2004;86-A:2143-2155. [PubMed] [Google Scholar]
- 15. Fithian DC, Paxton EW, Stone ML, et al. Prospective trial of a treatment algorithm for the management of the anterior cruciate ligament-injured knee. Am J Sports Med 2005;33:335-346. [DOI] [PubMed] [Google Scholar]
- 16. Hawkins RJ, Misamore GW, Merritt TR. Follow up of the acute nonoperated isolated anterior cruciate ligament tear. Am J Sports Med 1986;14:205-210. [DOI] [PubMed] [Google Scholar]
- 17. Kannus P, Järvinen M. Conservatively treated tears of the anterior cruciate ligament. Long-term results. J Bone Joint Surg [Am] 1987;69-A:1007-1012. [PubMed] [Google Scholar]
- 18. Mizuta H, Kubota K, Shiraishi M, et al. The conservative treatment of complete tears of the anterior cruciate ligament in skeletally immature patients. J Bone Joint Surg [Br] 1995;77-B:890-894. [PubMed] [Google Scholar]
- 19. Casteleyn PP, Handelberg F. Non-operative management of anterior cruciate ligament injuries in the general population. J Bone Joint Surg [Br] 1996;78-B:446-451. [PubMed] [Google Scholar]
- 20. Kessler MA, Behrend H, Henz S, et al. Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc 2008;16:442-448. [DOI] [PubMed] [Google Scholar]
- 21. Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med 2010;363:331-342. [DOI] [PubMed] [Google Scholar]
- 22. Linko E, Harilainen A, Malmivaara A, Seitsalo S. Surgical versus conservative interventions for anterior cruciate ligament ruptures in adults. Cochrane Database Syst Rev 2005;:CD001356. [DOI] [PubMed] [Google Scholar]
- 23. Richmond JC, Lubowitz JH, Poehling GG. Prompt operative intervention reduces long-term osteoarthritis after knee anterior cruciate ligament tear. Arthroscopy 2011;27:149-152. [DOI] [PubMed] [Google Scholar]
- 24. Millett PJ, Willis AA, Warren RF. Associated injuries in pediatric and adolescent anterior cruciate ligament tears: does a delay in treatment increase the risk of meniscal tear? Arthroscopy 2002;18:955-959. [DOI] [PubMed] [Google Scholar]
- 25. Dumont GD, Hogue GD, Padalecki JR, Okoro N, Wilson PL. Meniscal and chondral injuries associated with pediatric anterior cruciate ligament tears: relationship of treatment time and patient-specific factors. Am J Sports Med 2012;40:2128-2133. [DOI] [PubMed] [Google Scholar]
- 26. Lawrence JT, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med 2011;39:2582-2587. [DOI] [PubMed] [Google Scholar]
- 27. Moksnes H, Engebretsen L, Risberg MA. Prevalence and incidence of new meniscus and cartilage injuries after a nonoperative treatment algorithm for ACL tears in skeletally immature children: a prospective MRI study. Am J Sports Med 2013;41:1771-1779. [DOI] [PubMed] [Google Scholar]
- 28. Mohtadi NG, Chan DS, Dainty KN, Whelan DB. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev 2011;:CD005960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tiamklang T, Sumanont S, Foocharoen T, Laopaiboon M. Double-bundle versus single-bundle reconstruction for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev 2012;11:CD008413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Karlsson J, Kartus J, Magnusson L, et al. Subacute versus delayed reconstruction of the anterior cruciate ligament in the competitive athlete. Knee Surg Sports Traumatol Arthrosc 1999;7:146-151. [DOI] [PubMed] [Google Scholar]
- 31. Indelicato PA, Bittar ES. A perspective of lesions associated with ACL insufficiency of the knee. A review of 100 cases. Clin Orthop Relat Res 1985;198:77-80. [PubMed] [Google Scholar]
- 32. de Roeck NJ, Lang-Stevenson A. Meniscal tears sustained awaiting anterior cruciate ligament reconstruction. Injury 2003;34:343-345. [DOI] [PubMed] [Google Scholar]
- 33. Tayton E, Verma R, Higgins B, Gosal H. A correlation of time with meniscal tears in anterior cruciate ligament deficiency: stratifying the risk of surgical delay. Knee Surg Sports Traumatol Arthrosc 2009;17:30-34. [DOI] [PubMed] [Google Scholar]
- 34. Fithian DC, Paxton LW, Goltz DH. Fate of the anterior cruciate ligament-injured knee. Orthop Clin North Am 2002;33:621-636, vv. [DOI] [PubMed] [Google Scholar]
- 35. Shelbourne KD, Wilckens JH, Mollabashy A, DeCarlo M. Arthrofibrosis in acute anterior cruciate ligament reconstruction. The effect of timing of reconstruction and rehabilitation. Am J Sports Med 1991;19:332-336. [DOI] [PubMed] [Google Scholar]
- 36. Noyes FR, Berrios-Torres S, Barber-Westin SD, Heckmann TP. Prevention of permanent arthrofibrosis after anterior cruciate ligament reconstruction alone or combined with associated procedures: a prospective study in 443 knees. Knee Surg Sports Traumatol Arthrosc 2000;8:196-206. [DOI] [PubMed] [Google Scholar]
- 37. Wasilewski SA, Covall DJ, Cohen S. Effect of surgical timing on recovery and associated injuries after anterior cruciate ligament reconstruction. Am J Sports Med 1993;21:338-342. [DOI] [PubMed] [Google Scholar]
- 38. Nwachukwu BU, McFeely ED, Nasreddine A, et al. Arthrofibrosis after anterior cruciate ligament reconstruction in children and adolescents. J Pediatr Orthop 2011;31:811-817. [DOI] [PubMed] [Google Scholar]
- 39. Dandy DJ, Edwards DJ. Problems in regaining full extension of the knee after anterior cruciate ligament reconstruction: does arthrofibrosis exist? Knee Surg Sports Traumatol Arthrosc 1994;2:76-79. [DOI] [PubMed] [Google Scholar]
- 40. Marcacci M, Zaffagnini S, Iacono F, Neri MP, Petitto A. Early versus late reconstruction for anterior cruciate ligament rupture. results after five years of followup. Am J Sports Med 1995;23:690-693. [DOI] [PubMed] [Google Scholar]
- 41. Eitzen I, Holm I, Risberg MA. Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br J Sports Med 2009;43:371-376. [DOI] [PubMed] [Google Scholar]
- 42. Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 2012;42:750-759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Eitzen I, Moksnes H, Snyder-Mackler L, Risberg MA. A progressive 5-week exercise therapy program leads to significant improvement in knee function early after anterior cruciate ligament injury. J Orthop Sports Phys Ther 2010;40:705-721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Shelbourne KD, Foulk DA. Timing of surgery in acute anterior cruciate ligament tears on the return of quadriceps muscle strength after reconstruction using an autogenous patellar tendon graft. Am J Sports Med 1995;23:686-689. [DOI] [PubMed] [Google Scholar]
- 45. Xergia SA, McClelland JA, Kvist J, Vasiliadis HS, Georgoulis AD. The influence of graft choice on isokinetic muscle strength 4-24 months after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2011;19:768-780. [DOI] [PubMed] [Google Scholar]
- 46. Grindem H, Granan LP, Risberg MA, et al. How does a combined preoperative and postoperative rehabilitation programme influence the outcome of ACL reconstruction 2 years after surgery? A comparison between patients in the Delaware-Oslo ACL Cohort and the Norwegian National Knee Ligament Registry. Br J Sports Med 2015;49:385-389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Feller JA, Webster KE. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med 2003;31:564-573. [DOI] [PubMed] [Google Scholar]
- 48. Noyes FR, Butler DL, Grood ES, Zernicke RF, Hefzy MS. Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg [Am] 1984;66:344-352. [PubMed] [Google Scholar]
- 49. Hamner DL, Brown CH, Jr, Steiner ME, Hecker AT, Hayes WC. Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg [Am] 1999;81:549-557. [DOI] [PubMed] [Google Scholar]
- 50. Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR., Jr Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med 2003;31:2-11. [DOI] [PubMed] [Google Scholar]
- 51. Li S, Chen Y, Lin Z, Cui W, Zhao J, Su W. A systematic review of randomized controlled clinical trials comparing hamstring autografts versus bone-patellar tendon-bone autografts for the reconstruction of the anterior cruciate ligament. Arch Orthop Trauma Surg 2012;132:1287-1297. [DOI] [PubMed] [Google Scholar]
- 52. Xie X, Liu X, Chen Z, Yu Y, Peng S, Li Q. A meta-analysis of bone-patellar tendon-bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee 2015;22:100-110. [DOI] [PubMed] [Google Scholar]
- 53. Spindler KP, Kuhn JE, Freedman KB, et al. Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. Am J Sports Med 2004;32:1986-1995. [DOI] [PubMed] [Google Scholar]
- 54. Smith CK, Howell SM, Hull ML. Anterior laxity, slippage, and recovery of function in the first year after tibialis allograft anterior cruciate ligament reconstruction. Am J Sports Med 2011;39:78-88. [DOI] [PubMed] [Google Scholar]
- 55. Eagar P, Hull ML, Howell SM. How the fixation method stiffness and initial tension affect anterior load-displacement of the knee and tension in anterior cruciate ligament grafts: a study in cadaveric knees using a double-loop hamstrings graft. J Orthop Res 2004;22:613-624. [DOI] [PubMed] [Google Scholar]
- 56. Steiner ME, Hecker AT, Brown CH, Jr, Hayes WC. Anterior cruciate ligament graft fixation. Comparison of hamstring and patellar tendon grafts. Am J Sports Med 1994;22:240-246. [DOI] [PubMed] [Google Scholar]
- 57. Prodromos CC, Fu FH, Howell SM, Johnson DH, Lawhorn K. Controversies in soft-tissue anterior cruciate ligament reconstruction: grafts, bundles, tunnels, fixation, and harvest. J Am Acad Orthop Surg 2008;16:376-384. [DOI] [PubMed] [Google Scholar]
- 58. Tomita F, Yasuda K, Mikami S, et al. Comparisons of intraosseous graft healing between the doubled flexor tendon graft and the bone-patellar tendon-bone graft in anterior cruciate ligament reconstruction. Arthroscopy 2001;17:461-476. [DOI] [PubMed] [Google Scholar]
- 59. Feller J, Webster KE. Return to sport following anterior cruciate ligament reconstruction. Int Orthop 2013;37:285-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Marumo K, Saito M, Yamagishi T, Fujii K. The “ligamentization” process in human anterior cruciate ligament reconstruction with autogenous patellar and hamstring tendons: a biochemical study. Am J Sports Med 2005;33:1166-1173. [DOI] [PubMed] [Google Scholar]
- 61. Sánchez M, Anitua E, Azofra J, Prado R, Muruzabal F, Andia I. Ligamentization of tendon grafts treated with an endogenous preparation rich in growth factors: gross morphology and histology. Arthroscopy 2010;26:470-480. [DOI] [PubMed] [Google Scholar]
- 62. Steiner ME, Murray MM, Rodeo SA. Strategies to improve anterior cruciate ligament healing and graft placement. Am J Sports Med 2008;36:176-189. [DOI] [PubMed] [Google Scholar]
- 63. Ménétrey J, Duthon VB, Laumonier T, Fritschy D. “Biological failure” of the anterior cruciate ligament graft. Knee Surg Sports Traumatol Arthrosc 2008;16:224-231. [DOI] [PubMed] [Google Scholar]
- 64. Xie X, Xiao Z, Li Q, et al. Increased incidence of osteoarthritis of knee joint after ACL reconstruction with bone-patellar tendon-bone autografts than hamstring autografts: a meta-analysis of 1,443 patients at a minimum of 5 years. Eur J Orthop Surg Traumatol 2015;25:149-159. [DOI] [PubMed] [Google Scholar]
- 65. Ahldén M, Kartus J, Ejerhed L, Karlsson J, Sernert N. Knee laxity measurements after anterior cruciate ligament reconstruction, using either bone-patellar-tendon-bone or hamstring tendon autografts, with special emphasis on comparison over time. Knee Surg Sports Traumatol Arthrosc 2009;17:1117-1124. [DOI] [PubMed] [Google Scholar]
- 66. Barenius B, Ponzer S, Shalabi A, et al. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med 2014;42:1049-1057. [DOI] [PubMed] [Google Scholar]
- 67. Webster KE, Feller JA, Hartnett N, Leigh WB, Richmond AK. Comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction: a 15-year follow-up of a randomized controlled trial. Am J Sports Med 2016;44:83-90. [DOI] [PubMed] [Google Scholar]
- 68. Kartus J, Movin T, Karlsson J. Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy. 2001;17:971-980. [DOI] [PubMed] [Google Scholar]
- 69. Ristanis S, Tsepis E, Giotis D, et al. Electromechanical delay of the knee flexor muscles is impaired after harvesting hamstring tendons for anterior cruciate ligament reconstruction. Am J Sports Med 2009;37:2179-2186. [DOI] [PubMed] [Google Scholar]
- 70. Ferretti A, Conteduca F, Morelli F, Masi V. Regeneration of the semitendinosus tendon after its use in anterior cruciate ligament reconstruction: a histologic study of three cases. Am J Sports Med 2002;30:204-207. [DOI] [PubMed] [Google Scholar]
- 71. Nixon RG, SeGall GK, Sax SL, Cain TE, Tullos HS. Reconstitution of the patellar tendon donor site after graft harvest. Clin Orthop Relat Res 1995;317:162-171. [PubMed] [Google Scholar]
- 72. Bernicker JP, Haddad JL, Lintner DM, DiLiberti TC, Bocell JR. Patellar tendon defect during the first year after anterior cruciate ligament reconstruction: appearance on serial magnetic resonance imaging. Arthroscopy 1998;14:804-809. [DOI] [PubMed] [Google Scholar]
- 73. Neddermann A, Willbold E, Witte F, et al. Tunnel widening after anterior cruciate ligament reconstruction: an experimental study in sheep. Am J Sports Med 2009;37:1609-1617. [DOI] [PubMed] [Google Scholar]
- 74. Samuelsson K, Andersson D, Karlsson J. Treatment of anterior cruciate ligament injuries with special reference to graft type and surgical technique: an assessment of randomized controlled trials. Arthroscopy 2009;25:1139-1174. [DOI] [PubMed] [Google Scholar]
- 75. Matsumoto A, Howell SM, Liu-Barba D. Time-related changes in the cross-sectional area of the tibial tunnel after compaction of an autograft bone dowel alongside a hamstring graft. Arthroscopy 2006;22:855-860. [DOI] [PubMed] [Google Scholar]
- 76. Röpke M, Becker R, Urbach D, Nebelung W. [Semitendinosus tendon vs.patellar ligament. Results of a prospective randomized study after anterior cruciate ligament reconstruction]. Unfallchirurg. 2001;104:312-316. (In German) [DOI] [PubMed] [Google Scholar]
- 77. Goyal S, Matias N, Pandey V, Acharya K. Are pre-operative anthropometric parameters helpful in predicting length and thickness of quadrupled hamstring graft for ACL reconstruction in adults? A prospective study and literature review. Int Orthop 2016;40:173-181. [DOI] [PubMed] [Google Scholar]
- 78. Kaeding CC, Aros B, Pedroza A, et al. Allograft versus autograft anterior cruciate ligament reconstruction: predictors of failure from a MOON prospective longitudinal cohort. Sports Health 2011;3:73-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Zeng C, Gao SG, Li H, Yang T, Luo W, Li YS, et al. Autograft versus allograft in anterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials and systematic review of overlapping systematic reviews. Arthroscopy 2016;32:153-63.e18. [DOI] [PubMed] [Google Scholar]
- 80. Hu J, Qu J, Xu D, Zhou J, Lu H. Allograft versus autograft for anterior cruciate ligament reconstruction: an up-to-date meta-analysis of prospective studies. Int Orthop 2013;37:311-320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Cvetanovich GL, Mascarenhas R, Saccomanno MF, et al. Hamstring autograft versus soft-tissue allograft in anterior cruciate ligament reconstruction: a systematic review and meta-analysis of randomized controlled trials. Arthroscopy 2014;30:1616-1624. [DOI] [PubMed] [Google Scholar]
- 82. Krych AJ, Jackson JD, Hoskin TL, Dahm DL. A meta-analysis of patellar tendon autograft versus patellar tendon allograft in anterior cruciate ligament reconstruction. Arthroscopy 2008;24:292-298. [DOI] [PubMed] [Google Scholar]
- 83. Mohammadi F, Salavati M, Akhbari B, et al. Comparison of functional outcome measures after ACL reconstruction in competitive soccer players: a randomized trial. J Bone Joint Surg [Am] 2013;95:1271-1277. [DOI] [PubMed] [Google Scholar]
- 84. Prodromos C, Joyce B, Shi K. A meta-analysis of stability of autografts compared to allografts after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2007;15:851-856. [DOI] [PubMed] [Google Scholar]
- 85. Kraeutler MJ, Bravman JT, McCarty EC. Bone-patellar tendon-bone autograft versus allograft in outcomes of anterior cruciate ligament reconstruction: a meta-analysis of 5182 patients. Am J Sports Med 2013;41:2439-2448. [DOI] [PubMed] [Google Scholar]
- 86. Barrera Oro F, Sikka RS, Wolters B, et al. Autograft versus allograft: an economic cost comparison of anterior cruciate ligament reconstruction. Arthroscopy 2011;27:1219-1225. [DOI] [PubMed] [Google Scholar]
- 87. Cooper MT, Kaeding C. Comparison of the hospital cost of autograft versus allograft soft-tissue anterior cruciate ligament reconstructions. Arthroscopy 2010;26:1478-1482. [DOI] [PubMed] [Google Scholar]
- 88. Genuario JW, Faucett SC, Boublik M, Schlegel TF. A cost-effectiveness analysis comparing 3 anterior cruciate ligament graft types: bone-patellar tendon-bone autograft, hamstring autograft, and allograft. Am J Sports Med 2012;40:307-314. [DOI] [PubMed] [Google Scholar]
- 89. Crawford C, Kainer M, Jernigan D, et al. Investigation of postoperative allograft-associated infections in patients who underwent musculoskeletal allograft implantation. Clin Infect Dis 2005;41:195-200. [DOI] [PubMed] [Google Scholar]
- 90. Katz LM, Battaglia TC, Patino P, et al. A retrospective comparison of the incidence of bacterial infection following anterior cruciate ligament reconstruction with autograft versus allograft. Arthroscopy 2008;24:1330-1335. [DOI] [PubMed] [Google Scholar]
- 91. Howell SM, Taylor MA. Failure of reconstruction of the anterior cruciate ligament due to impingement by the intercondylar roof. J Bone Joint Surg [Am] 1993;75:1044-1055. [DOI] [PubMed] [Google Scholar]
- 92. Howell SM. Principles for placing the tibial tunnel and avoiding roof impingement during reconstruction of a torn anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 1998;6(suppl 1):S49-S55. [DOI] [PubMed] [Google Scholar]
- 93. Howell SM, Clark JA. Tibial tunnel placement in anterior cruciate ligament reconstructions and graft impingement. Clin Orthop Relat Res 1992;283:187-195. [PubMed] [Google Scholar]
- 94. Amis AA, Jakob RP. Anterior cruciate ligament graft positioning, tensioning and twisting. Knee Surg Sports Traumatol Arthrosc 1998;6(suppl 1):S2-S12. [DOI] [PubMed] [Google Scholar]
- 95. Guenther D, Irarrázaval S, Nishizawa Y, et al. Variation in the shape of the tibial insertion site of the anterior cruciate ligament: classification is required. Knee Surg Sports Traumatol Arthrosc 2015[Epub ahead of print] PMID:26658565. [DOI] [PubMed] [Google Scholar]
- 96. Sasaki N, Ishibashi Y, Tsuda E, et al. The femoral insertion of the anterior cruciate ligament: discrepancy between macroscopic and histological observations. Arthroscopy 2012;28:1135-1146. [DOI] [PubMed] [Google Scholar]
- 97. Siebold R. The concept of complete footprint restoration with guidelines for single- and double-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2011;19:699-706. [DOI] [PubMed] [Google Scholar]
- 98. Colombet P, Robinson J, Christel P, et al. Morphology of anterior cruciate ligament attachments for anatomic reconstruction: a cadaveric dissection and radiographic study. Arthroscopy 2006;22:984-992. [DOI] [PubMed] [Google Scholar]
- 99. Fu FH, Jordan SS. The lateral intercondylar ridge–a key to anatomic anterior cruciate ligament reconstruction. J Bone Joint Surg [Am] 2007;89:2103-2104. [DOI] [PubMed] [Google Scholar]
- 100. Yagi M, Wong EK, Kanamori A, et al. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med 2002;30:660-666. [DOI] [PubMed] [Google Scholar]
- 101. Markolf KL, Park S, Jackson SR, McAllister DR. Anterior-posterior and rotatory stability of single and double-bundle anterior cruciate ligament reconstructions. J Bone Joint Surg [Am] 2009;91:107-118. [DOI] [PubMed] [Google Scholar]
- 102. Järvelä T. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective, randomize clinical study. Knee Surg Sports Traumatol Arthrosc 2007;15:500-507. [DOI] [PubMed] [Google Scholar]
- 103. Meredick RB, Vance KJ, Appleby D, Lubowitz JH. Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med 2008;36:1414-1421. [DOI] [PubMed] [Google Scholar]
- 104. Muneta T, Koga H, Mochizuki T, et al. A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy 2007;23:618-628. [DOI] [PubMed] [Google Scholar]
- 105. Iriuchishima T, Yorifuji H, Aizawa S, et al. Evaluation of ACL mid-substance cross-sectional area for reconstructed autograft selection. Knee Surg Sports Traumatol Arthrosc 2014;22:207-213. [DOI] [PubMed] [Google Scholar]
- 106. Triantafyllidi E, Paschos NK, Goussia A, et al. The shape and the thickness of the anterior cruciate ligament along its length in relation to the posterior cruciate ligament: a cadaveric study. Arthroscopy 2013;29:1963-1973. [DOI] [PubMed] [Google Scholar]
- 107. Paschos NK, Gartzonikas D, Barkoula NM, et al. Cadaveric study of anterior cruciate ligament failure patterns under uniaxial tension along the ligament. Arthroscopy 2010;26:957-967. [DOI] [PubMed] [Google Scholar]
- 108. Amis AA, Dawkins GP. Functional anatomy of the anterior cruciate ligament. Fibre bundle actions related to ligament replacements and injuries. J Bone Joint Surg [Br] 1991;73-B:260-267. [DOI] [PubMed] [Google Scholar]
- 109. Sonnery-Cottet B, Chambat P. Arthroscopic identification of the anterior cruciate ligament posterolateral bundle: the figure-of-four position. Arthroscopy 2007;23:1128e1-3. [DOI] [PubMed] [Google Scholar]
- 110. Hefzy MS, Grood ES, Noyes FR. Factors affecting the region of most isometric femoral attachments. Part II: the anterior cruciate ligament. Am J Sports Med 1989;17:208-216. [DOI] [PubMed] [Google Scholar]
- 111. Sidles JA, Larson RV, Garbini JL, Downey DJ, Matsen FA., III Ligament length relationships in the moving knee. J Orthop Res 1988;6:593-610. [DOI] [PubMed] [Google Scholar]
- 112. Simmons R, Howell SM, Hull ML. Effect of the angle of the femoral and tibial tunnels in the coronal plane and incremental excision of the posterior cruciate ligament on tension of an anterior cruciate ligament graft: an in vitro study. J Bone Joint Surg [Am] 2003;85-A:1018-1029. [DOI] [PubMed] [Google Scholar]
- 113. Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind MC. Increased risk of revision after anteromedial compared with transtibial drilling of the femoral tunnel during primary anterior cruciate ligament reconstruction: results from the Danish Knee Ligament Reconstruction Register. Arthroscopy 2013;29:98-105. [DOI] [PubMed] [Google Scholar]