Abstract
Lateral epicondylitis, also known as ‘tennis elbow’, is a very common condition affecting mainly middle-aged patients.
The pathogenesis remains unknown but there appears to be a combination of local tendon pathology, alteration in pain perception and motor impairment.
The diagnosis is usually clinical but some patients may benefit from additional imaging for a specific differential diagnosis.
The disease has a self-limiting course of between 12 and 18 months, but in some patients, symptoms can be persistent and refractory to treatment.
Most patients are well-managed with non-operative treatment and activity modification. Many surgical techniques have been proposed for patients with refractory symptoms.
New non-operative treatment alternatives with promising results have been developed in recent years.
Cite this article: Vaquero-Picado A, Barco R, Antuña SA. Lateral epicondylitis of the elbow. EFORT Open Rev 2016;1:391-397. DOI: 10.1302/2058-5241.1.000049.
Keywords: lateral epicondylitis, tennis elbow, lateral elbow pain, conservative management, operative management
Introduction
Lateral elbow pain is one of the most common sources of medical consultation for non-traumatic elbow disorders. The most frequent diagnosis is the tendinous disorder known as lateral epicondylitis (LE) or ‘tennis elbow’. However there are many pathological conditions that may mimic LE such as intra-articular plica, osteochondritis dissecans (OCD), radiocapitellar arthritis or posterolateral rotatory instability.1
Lateral epicondylitis was first described by Runge in 1873.2 It was described as a chronic symptomatic degeneration of the wrist extensor tendons involving their attachment to the lateral epicondyle of the humerus. It is a common condition, affecting between 1% and 3% of the population,3 generally affecting the middle-aged without gender predisposition.
Despite its relatively high prevalence, there is no single effective and consistent algorithm of management. Fortunately, most cases are self-limiting and well-managed with simple pain medication, with 90% of patients recovering within one year. Patients with severe or persistent symptoms are suitable for treatment with further conservative or operative options.4
Aetiology and pathogenesis
In the majority of cases, non-obvious underlying causes can be identified.5 Extensor carpi radialis brevis (ECRB) is the most commonly affected muscle, but supinator and other wrist extensors such as extensor carpi radialis longus, extensor digitorum, extensor digiti minimi and extensor carpi ulnaris can be involved. Any activity involving excessive and repetitive use of these muscles (for example tennis, playing an instrument, typing, manual work) may cause the tendinosis.6,7 Smoking and obesity have been identified as significant risk factors.5
Though LE was classically identified as an inflammatory process, the histology does not show many inflammatory cells; most authors therefore consider LE as a tendinosis, a symptomatic degenerative process of the tendon.8
The application of tension to a tendon usually increases cross-linkage and collagen deposition.9 Tendons can stretch easily in response to gradually increasing forces. If this stress exceeds the tendon’s tolerance to stretch, a microtear may occur. Multiple microtears lead to degenerative changes within the tendon which are known as tendinosis. Histological changes such as angiofibroblastic hyperplasia (a manifestation of granulation tissue that disturbs correct collagen synthesis) can also be seen. Histopathological studies of ECRB in patients with long-standing LE have shown necrosis as well as signs of fibre regeneration. Nevertheless, additional pathophysiological mechanisms have been suggested.
Painful symptomatic LE can result in underuse of the tendon. Underuse changes the tendon structure, leading to progressive weakening and increasing the risk of injury. In conjunction with underuse, shearing forces lead to fibrocartilaginous formation at the ECRB enthesis, which contributes to weakening at the tendon-bone junction.4,10 In addition, the tendon vascularisation is deficient and sustained muscle contractions can lead to tendon ischaemia. Repetitive activities increase temperature which can lead to hyperthermic injuries of the enthesis.
Despite all of these considerations, there is a lack of knowledge to explain the great variability of symptoms among patients. Peripheral nerve irritation and local altered pain response have been proposed.11 Shoulder and neck pain are frequent symptoms in this population, but they can be associated with alterations in upper limb biomechanics.10
Clinical presentation
The majority of the patients complain of pain located just anterior to, or in, the bony surface of the upper half of the lateral epicondyle, usually radiating in line with the common extensor mass. The pain can vary from intermittent and low-grade pain to continuous and severe pain which may cause sleep disturbance. It is typically produced by wrist and finger extensor and supinator muscle contraction against resistance. The pain lessens slightly if the extensors are stressed with the elbow held in flexion.
On inspection, there is no remarkable alteration in the early stages. As the disease evolves, a bony prominence over the lateral epicondyle can be detected. Muscle and skin atrophy as well as detachment of common extensor origin can be seen as a result of corticosteroid injections or long-standing disease.4
Range of motion is not usually affected. Motion may be painful in more advanced stages where it can be elicited in full elbow extension with the forearm pronated. If limited motion exists, other concomitant pathology needs to be excluded.12
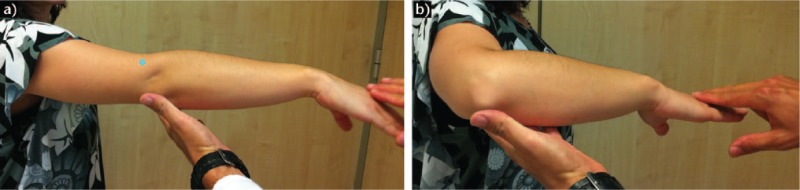
There are many tests employed in LE physical examination. Maudley’s test,13 Thomson’s manoeuvre, diminished grip strength14 and the ‘chair’ test (Fig 1a, b) are some of the tests employed to reproduce the pain of LE.
Fig. 1.
a) Patient with pain (small blue circle) on the lateral epicondyle with resisted wrist extension and with the arm in full extension, alleviated by flexing the elbow. b) The mechanism by which pain is reduced might be the decreased tension of the extensor muscles against the superolateral aspect of the capitellum.
Imaging studies
Most LE cases can be clinically diagnosed. However when clinical symptoms are not well-defined, some diagnostic studies can be helpful.
Plain anteroposterior (AP) and lateral radiographs are useful for the assessment of bone diseases such as OCD, arthropathy and loose bodies. In cases of long-standing LE, calcifications of ECRB insertion can be seen.
Ultrasound is one of the most useful tools to diagnose or rule out LE. Structural changes affecting tendons (thickening, thinning, intra-substance degenerative areas and tendon tears for example), bone irregularities or calcific deposits can be detected. Neo-vascularisation can also be assessed by colour Doppler exploration. Absence of this finding, or no changes in a greyscale ultrasound sonography (USG), can be useful to rule out LE.15
Magnetic resonance imaging (MRI) is more reproducible, reduces inter-operator variability and gives more information about intra-articular pathology (Fig. 2). Unfortunately, findings on MRI are not well correlated with the severity of clinical symptoms, and is an expensive modality to be used routinely for such a common condition.16 CT arthrography has been demonstrated to be more accurate than MRI to diagnose capsular tears.17
Fig. 2.

Coronal T-2 weighted MRI image of a right elbow showing an injury of the insertion of the extensor muscles at the lateral epicondyle.
Electromyography of the posterior interosseous nerve (PIN) and local anaesthetic injection just distal to the radial head can be useful to diagnose a PIN compression. Blood tests should be used when infection or inflammatory diseases are suspected as the cause of lateral elbow pain.
Overall, radiological findings are not always well correlated with clinical symptoms. Therefore, clinical examination cannot be substituted with these complementary studies.
Diferential diagnosis
In a middle-aged patient with pain on the lateral side of the elbow and typical symptoms and signs (Fig. 3), lateral epicondylitis should undoubtedly be the main diagnosis, but one must rule out other potential conditions which can cause lateral pain. The following should be considered (Table 1):
Fig. 3.
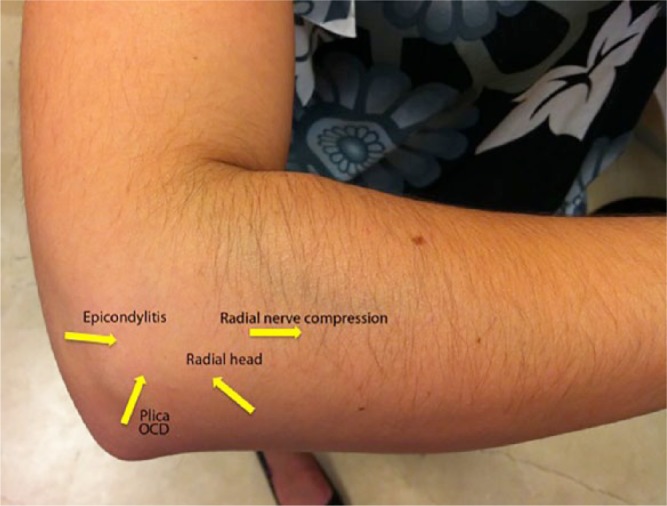
Location of the site of greatest tenderness may be helpful in defining the diagnosis for further clinical testing and/or imaging techniques.
Cervical radiculopathy with pain in the elbow and forearm.18
Elbow overuse to compensate for a disease in an adjacent joint (frozen shoulder for example).
Posterior interosseous nerve (PIN) entrapment (also known as ‘radial tunnel syndrome’). Nerve compression produces neuropathic pain in the lateral forearm. However, pain is not reproduced by wrist extension. Resisted supination can produce pain as the supinator is one of the possible areas of PIN compression. An anaesthetic block of PIN can be diagnostic, but injection should be performed selectively to avoid diffusion of the local anaesthetic to the lateral epicondyle area.19 The middle finger extension test, resisted supination of the forearm and nerve conduction studies have all been described to assist in the diagnosis of radial tunnel syndrome.20
Degenerative changes and OCD of the capitellum. It has been observed that 59% of cases of lateral elbow pain refractory to conservative treatment have some chondral changes in the radiocapitellar joint.21 OCD typically affects young individuals involved in sports and physical activities who have mild grinding and pain when performing a moving valgus test.
Inflammation and oedema of the anconeus muscle. Some studies have reported a relatively high incidence of anconeus oedema, shown in MRI of patients complaining of lateral elbow pain.22 Fasciotomy of the muscle can solve that problem.23
Posterolateral elbow instability should definitely be ruled out in every patient suffering from lateral elbow pain. The association between instability and epicondylitis has been established, following excessive use of steroids or the local pathogenic insult. The presentation is low-grade and may require examination of the patient under anesthesia to test it properly. The presence of cubitus varus, previous surgery or dislocations of the elbow should be assessed.
Other causes of pain include low-grade infection (Propionibacterium acnes)24 or other inflammatory diseases such as rheumatoid arthritis.25
Treatment
To date, no universally accepted regime of treatment exists; however some general principles of treatment should be taken into consideration. The treatment of LE should be orientated to the management of pain, preservation of movement, improvement in grip strength and endurance, return to normal function and control of further clinical deterioration.4
Non-operative treatment
Non-operative treatment includes a wide array of possibilities with a rate of improvement in 90% of cases. Several new techniques have been developed in last decade including percutaneous radiofrequency treatment and injections with different preparations of growth factors. It is wise to involve the patient and gain their commitment to the management programme as it may be months before improvement is observed:
Rest, modification or avoidance of painful activities usually leads to symptomatic relief.
-
Physiotherapy is another alternative. Some studies have reported good outcomes with physiotherapy regimes of stretching and strengthening, with more favourable results than rest and reduced activity at short-term follow-up.26 No standard regime has been established as superior to any other method. The fundamental principle is to load the tendon as close as possible to its limit but without surpassing it. Eccentric exercises and partial load-favouring tendon healing are the mainstay of physiotherapy regimes.
A stable shoulder and scapula are necessary for correct elbow function; strengthening exercises of the scapular stabilisers including the lower trapezius, serratus anterior and rotator cuff muscles is mandatory.
Epicondylar counterforce braces work by reducing tension in the wrist extensors. Elbow straps, clasps or sleeve orthoses have been demonstrated as superior for pain relief and grip strength when compared with placebo orthoses.27 However, no differences between braces were shown in a systematic review28 and we do not use them in our practice. We have seen patients with secondary nerve problems due to prolonged use of a counterforce brace.
Non-steroidal anti-inflammatory drugs (NSAIDs) can be useful for the short-term relief of symptoms. Even if their use is superior to a placebo, no differences between oral and topical NSAIDs have been established.29
Corticosteroid injections are commonly used to treat LE. The way in which they work is currently unknown; they probably help to control local inflammatory response and pain mediation.30 Corticosteroid injections seem to be superior to NSAIDs at four weeks, but no differences are observed at a later stage. Cortisone injections should be avoided in all cases, unless a short-term good result is advisable (such as a professional tennis player in mid-season), as most patients improve without corticosteroids and better long-term results can be achieved without them.31 Patients should be advised of potential side-effects including changes in colouration of the skin, fat atrophy and muscle wasting.
Autologous blood injections are thought to work by stimulating an inflammatory response which will bring in the necessary nutrients to promote healing. Short-term good results have been reported recently;32,33 however, no benefit in the long-term follow-up has been found and its use is only recommended for those recalcitrant cases when other modalities of treatment have failed.
Platelet-rich plasma injections (PRP). These preparations are thought to contain high concentrations of growth factors, which could theoretically enhance tendon healing. General technique involves patient-blood extraction, centrifugation and re-injection of the plasma into the lateral epicondyle. Good outcomes have been reported.34,35 However, no differences were seen between PRP and whole blood injections.36 Moreover, significant differences among available commercial systems and variations in the technique make it difficult to draw clear conclusions about the use of PRP in this pathology. New legal regulations could slow down the adoption of these last techniques.
Percutaneous radiofrequency thermal treatment. A radiofrequency electrode is introduced percutaneously under ultrasound guidance which produces a thermal injury when activated, inducing a microtenotomy and removing all pathological tissue. Good outcomes have been reported, and no reduction of tendon size has been observed.37
Extracorporeal shock-wave therapy (ECSW) has been proposed as an alternative to non-operative management. The mechanism of action is not fully known. A generator of specific frequency sound waves is applied directly onto the overlying skin of the ECRB tendon. It has not been demonstrated to be more beneficial than other treatment modalities.38
The use of low-level laser therapy has been proposed due to the stimulating effect of laser on collagen production in tendons. Although laser was not initially viewed as particularly useful among LE therapies, a recent study has demonstrated some short-term benefits when using an adequate dose and wavelength.39
Acupuncture has demonstrated good outcomes on short-term follow-up.40 However, long-term results remain unclear.
Botulinum toxin A injections act by diminishing muscle tone. Reducing the tension on the ECRB insertion could be beneficial for pain relief. Good short-term results have been published,41 but as yet there is no consensus on its use and the effects may be conditioned by the technique, the operator and the dose.
Operative treatment
Patients with persistent pain and disability after a course of well-performed conservative treatment are candidates for clinical re-evaluation and, possibly, operative treatment. Open, percutaneous and arthroscopic approaches have been used.
The basic principle of open surgery involves debriding the angio-fibrotic tissue of the ECRB with or without posterior tendon repair. Multiple variations of open surgery have been proposed in the literature including extensor release with intra-articular modifications, extensor fasciotomy, V-Y slide of the common extensor tendon, denervation of the lateral epicondyle, epicondylar resection with anconeus muscle transfer and lengthening of the ECRB.42,43 Basically, the ECRB insertion is approached through a standard longitudinal incision over the lateral aspect of the elbow. The insertion then can be detached, dividing its fibres longitudinally, or tendinotic tissue can be debrided (Fig. 4). After debridement, the rest of the tendon can be repaired (or not), lengthened (or not), and drilling or decortication of the epicondyle to stimulate blood flow may be performed.
Fig. 4.
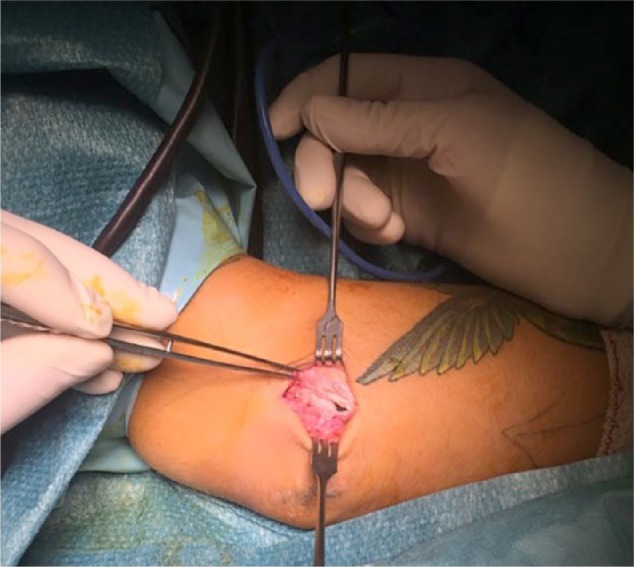
Patient with lateral epicondylitis of the right elbow undergoing an open technique. Debridement of the ECRB has been performed and the joint is visible through the capsular defect present in this case. Perforation of the lateral epicondyle and reconstruction of the extensor muscles are optional additional techniques after debridement of the typical injury.
There is no consensus on the best surgical technique to manage LE, and evidence is lacking to support or refute a specific technique.44 As a potential disadvantage, excessive release may lead to lateral instability of the elbow. Long-term good outcomes have been reported with different open techniques.45
A percutaneous approach is advocated by some authors with good mid-term outcomes.46-48 Percutaneous release may be performed in the office setting with the patient conscious. However, it generally precludes reconstruction after debridement.
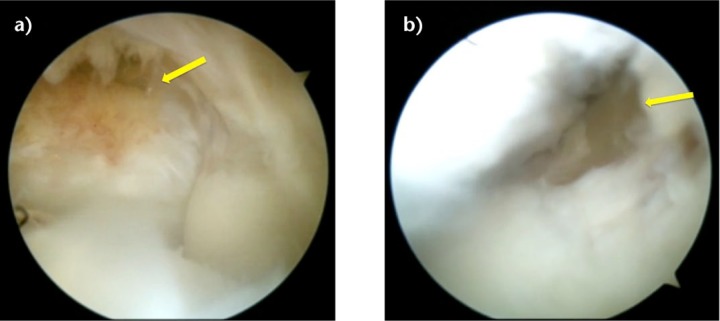
Arthroscopic treatment of LE has become more popular in recent years. It was first described in 1995 by Baker49 and has the advantage of a quick return to work and the ability to address and treat intra-articular pathology. It is performed through posterolateral and anteromedial viewing portals and an anterolateral working portal (Fig. 5a, b).
Fig. 5.
Clinical photograph of a patient with lateral epicondylitis of the right elbow undergoing an arthroscopic technique. a) A capsular injury is observed in the superolateral aspect of the joint. b) After debridement and reconstruction of the extensor muscles with the help of an anchor the capsular defect has been repaired.
Debridement and reconstruction is possible and safe but it takes slightly longer than open surgery, and there is a risk of potential damage of the radial nerve and to the lateral collateral ligament if the debridement extends posteriorly past the centre of the epicondyle. Good to excellent long-term results have been reported with this technique.50,51 Post-operatively it is usually recommended to refrain from aggravating activities for at least three months. Desk-workers can return to work immediately and manual workers are encouraged to restart work after four weeks.
Bad compliance, infections, haematoma or nerve injuries can complicate the process, but generally nine out of ten patients improve with surgical treatment.
It is important to recognise that there is a group of patients who do not improve after adequate non-operative treatment and well-performed surgical techniques. Reasons for persistent symptoms after any treatment modality include working compensation issues, misdiagnosis of an associated problem or an incorrect initial diagnosis.
Conclusions
Lateral elbow epicondylitis is frequently a self-limiting entity, with a normal course of between 12 and 18 months. In the vast majority of patients, symptoms resolve with non-operative treatment, physiotherapy and activity modification.
Multiple non-operative treatments have been proposed, but none of them has demonstrated superiority over others, therefore no specific recommendations can be made. Operative treatment is reserved for those patients with persistent symptoms who have failed a well-performed non-operative programme. However, there is no evidence to support a specific technique. New treatment alternatives have been developed in recent years, but more information is necessary to support their standard use in LE treatment.
Footnotes
Conflict of Interest: None declared.
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Antuña S, Barco R. Essentials in elbow surgery. A comprehensive approach to common elbow disorders. London: Springer Verlag, 2014. [Google Scholar]
- 2. Runge F. Zur Genese und Behandlung des schreibe Kranfes. Bed Klin Worchenschr 1873;10:245-248. (In German) [Google Scholar]
- 3. Smidt N, van der Windt DA. Tennis elbow in primary care. BMJ 2006;333:927-928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ahmad Z, Siddiqui N, Malik SS, et al. Lateral epicondylitis: a review of pathology and management. Bone Joint J [Br] 2013;95-B:1158-1164. [DOI] [PubMed] [Google Scholar]
- 5. Shiri R, Viikari-Juntura E, Varonen H, Heliövaara M. Prevalence and determinants of lateral and medial epicondylitis: a population study. Am J Epidemiol 2006;164:1065-1074. [DOI] [PubMed] [Google Scholar]
- 6. Eygendaal D, Rahussen FTG, Diercks RL. Biomechanics of the elbow joint in tennis players and relation to pathology. Br J Sports Med 2007;41:820-823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lee H-S, Park HY, Yoon JO, et al. Musicians’ medicine: musculoskeletal problems in string players. Clin Orthop Surg 2013;5:155-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Doran A, Gresham GA, Rushton N, Watson C. Tennis elbow. A clinicopathologic study of 22 cases followed for 2 years. Acta Orthop Scand 1990;61:535-538. [DOI] [PubMed] [Google Scholar]
- 9. Kraushaar BS, Nirschl RP. Tendinosis of the elbow (tennis elbow). Clinical features and findings of histological, immunohistochemical, and electron microscopy studies. J Bone Joint Surg [Am] 1999;81-A:259-278. [PubMed] [Google Scholar]
- 10. Coombes BK, Bisset L, Vicenzino B. A new integrative model of lateral epicondylalgia. Br J Sports Med 2009;43:252-258. [DOI] [PubMed] [Google Scholar]
- 11. Rath AM, Perez M, Mainguené C, Masquelet AC, Chevrel JP. Anatomic basis of the physiopathology of the epicondylalgias: a study of the deep branch of the radial nerve. Surg Radiol Anat 1993;15:15-19. [DOI] [PubMed] [Google Scholar]
- 12. Orchard J, Kountouris A. The management of tennis elbow. BMJ 2011;342:d2687–d2687. PMID: 21558359. [DOI] [PubMed] [Google Scholar]
- 13. McCallum SDA, Paoloni JA, Murrell GAC. Five-year prospective comparison study of topical glyceryl trinitrate treatment of chronic lateral epicondylosis at the elbow.Br J Sports Med 2011;45:416-420. [DOI] [PubMed] [Google Scholar]
- 14. Hsu SH, Moen TC, Levine WN, Ahmad CS. Physical examination of the athlete’s elbow. Am J Sports Med 2012;40:699-708. [DOI] [PubMed] [Google Scholar]
- 15. du Toit C, Stieler M, Saunders R, Bisset L, Vicenzino B. Diagnostic accuracy of power Doppler ultrasound in patients with chronic tennis elbow. Br J Sports Med 2008;42:872-876. [DOI] [PubMed] [Google Scholar]
- 16. Savnik A, Jensen B, Nørregaard J, et al. Magnetic resonance imaging in the evaluation of treatment response of lateral epicondylitis of the elbow. Eur Radiol 2004;14:964-969. [DOI] [PubMed] [Google Scholar]
- 17. Sasaki K, Tamakawa M, Onda K, et al. The detection of the capsular tear at the undersurface of the extensor carpi radialis brevis tendon in chronic tennis elbow: the value of magnetic resonance imaging and computed tomography arthrography. J Shoulder Elbow Surg 2011;20:420-425. [DOI] [PubMed] [Google Scholar]
- 18. Caridi JM, Pumberger M, Hughes AP. Cervical radiculopathy: a review. HSS J 2011;7:265-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Naam NH, Nemani S. Radial tunnel syndrome. Orthop Clin North Am 2012;43:529-536. [DOI] [PubMed] [Google Scholar]
- 20. Luk JK, Tsang RC, Leung H. Lateral epicondylalgia: midlife crisis of a tendon. Hong Kong Med J 2014;20:145-151. [DOI] [PubMed] [Google Scholar]
- 21. Rajeev A, Pooley J. Lateral compartment cartilage changes and lateral elbow pain. Acta Orthop Belg 2009;75:37-40. [PubMed] [Google Scholar]
- 22. Coel M, Yamada CY, Ko J. MR imaging of patients with lateral epicondylitis of the elbow (tennis elbow): importance of increased signal of the anconeus muscle. AJR Am J Roentgenol 1993;161:1019-1021. [DOI] [PubMed] [Google Scholar]
- 23. Söderberg TA. Bilateral chronic compartment syndrome in the forearm and the hand. J Bone Joint Surg [Br] 1996;78-B:780-782. [PubMed] [Google Scholar]
- 24. Jones M, Kishore MK, Redfern D. Propionibacterium acnes infection of the elbow. J Shoulder Elbow Surg 2011;20:e22-e25. [DOI] [PubMed] [Google Scholar]
- 25. Kotnis NA, Chiavaras MM, Harish S. Lateral epicondylitis and beyond: imaging of lateral elbow pain with clinical-radiologic correlation. Skeletal Radiol 2012;41:369-386. [DOI] [PubMed] [Google Scholar]
- 26. Hoogvliet P, Randsdorp MS, Dingemanse R, Koes BW, Huisstede BMA. Does effectiveness of exercise therapy and mobilisation techniques offer guidance for the treatment of lateral and medial epicondylitis? A systematic review. Br J Sports Med 2013;47:1112-1119. [DOI] [PubMed] [Google Scholar]
- 27. Jafarian FS, Demneh ES, Tyson SF. The immediate effect of orthotic management on grip strength of patients with lateral epicondylosis. J Orthop Sports Phys Ther 2009;39:484-489. [DOI] [PubMed] [Google Scholar]
- 28. Bisset L, Paungmali A, Vicenzino B, Beller E. A systematic review and meta-analysis of clinical trials on physical interventions for lateral epicondylalgia. Br J Sports Med 2005;39:411-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pattanittum P, Turner T, Green S, Buchbinder R. Non-steroidal anti-inflammatory drugs (NSAIDs) for treating lateral elbow pain in adults. Cochrane Database Syst Rev 2013;5:CD003686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet 2010;376:1751-1767. [DOI] [PubMed] [Google Scholar]
- 31. Osborne H. Stop injecting corticosteroid into patients with tennis elbow, they are much more likely to get better by themselves! J Sci Med Sport 2010;13:380-381. [DOI] [PubMed] [Google Scholar]
- 32. Creaney L, Wallace A, Curtis M, Connell D. Growth factor-based therapies provide additional benefit beyond physical therapy in resistant elbow tendinopathy: a prospective, single-blind, randomised trial of autologous blood injections versus platelet-rich plasma injections. Br J Sports Med 2011;45:966-971. [DOI] [PubMed] [Google Scholar]
- 33. Kazemi M, Azma K, Tavana B, et al. Autologous blood versus corticosteroid local injection in the short-term treatment of lateral elbow tendinopathy: a randomized clinical trial of efficacy. Am J Phys Med Rehabil 2010;89:660-667. [DOI] [PubMed] [Google Scholar]
- 34. Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med 2006;34:1774-1778. [DOI] [PubMed] [Google Scholar]
- 35. Gosens T, Peerbooms JC, van Laar W, den Oudsten BL. Ongoing positive effect of platelet-rich plasma versus corticosteroid injection in lateral epicondylitis: a double-blind randomized controlled trial with 2-year follow-up. Am J Sports Med 2011;39:1200-1208. [DOI] [PubMed] [Google Scholar]
- 36. Thanasas C, Papadimitriou G, Charalambidis C, Paraskevopoulos I, Papanikolaou A. Platelet-rich plasma versus autologous whole blood for the treatment of chronic lateral elbow epicondylitis: a randomized controlled clinical trial. Am J Sports Med 2011;39:2130-2134. [DOI] [PubMed] [Google Scholar]
- 37. Lin C-L, Lee J-S, Su W-R, et al. Clinical and ultrasonographic results of ultrasonographically guided percutaneous radiofrequency lesioning in the treatment of recalcitrant lateral epicondylitis. Am J Sports Med 2011;39:2429-2435. [DOI] [PubMed] [Google Scholar]
- 38. Buchbinder R, Green SE, Youd JM, et al. Systematic review of the efficacy and safety of shock wave therapy for lateral elbow pain. J Rheumatol 2006;33:1351-1363. [PubMed] [Google Scholar]
- 39. Bjordal JM, Lopes-Martins RA, Joensen J, et al. A systematic review with procedural assessments and meta-analysis of low level laser therapy in lateral elbow tendinopathy (tennis elbow). BMC Musculoskelet Disord 2008;9:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Trinh KV, Phillips S-D, Ho E, Damsma K. Acupuncture for the alleviation of lateral epicondyle pain: a systematic review. Rheumatology (Oxford) 2004;43:1085-1090. [DOI] [PubMed] [Google Scholar]
- 41. Placzek R, Drescher W, Deuretzbacher G, Hempfing A, Meiss AL. Treatment of chronic radial epicondylitis with botulinum toxin A. A double-blind, placebo-controlled, randomized multicenter study. J Bone Joint Surg [Am] 2007;89-A:255-260. [DOI] [PubMed] [Google Scholar]
- 42. Nirschl RP, Pettrone FA. Tennis elbow. The surgical treatment of lateral epicondylitis. J Bone Joint Surg [Am] 1979;61-A:832-839. [PubMed] [Google Scholar]
- 43. Bosworth DM. Surgical treatment of tennis elbow: a follow-up study. J Bone Joint Surg [Am] 1965;47-A:1533-1536. [PubMed] [Google Scholar]
- 44. Buchbinder R, Johnston RV, Barnsley L, et al. Surgery for lateral elbow pain. Cochrane Database Syst Rev 2011:CD003525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Dunn JH, Kim JJ, Davis L, Nirschl RP. Ten- to 14-year follow-up of the Nirschl surgical technique for lateral epicondylitis. Am J Sports Med 2008;36:261-266. [DOI] [PubMed] [Google Scholar]
- 46. Baumgard SH, Schwartz DR. Percutaneous release of the epicondylar muscles for humeral epicondylitis. Am J Sports Med 1982;10:233-236. [DOI] [PubMed] [Google Scholar]
- 47. Cho B-K, Kim Y-M, Kim D-S, et al. Mini-open muscle resection procedure under local anesthesia for lateral and medial epicondylitis. Clin Orthop Surg 2009;1:123-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Nazar M, Lipscombe S, Morapudi S, et al. Percutaneous tennis elbow release under local anaesthesia. Open Orthop J 2012;6:129-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Grifka J, Boenke S, Krämer J. Endoscopic therapy in epicondylitis radialis humeri. Arthroscopy 1995;11:743-748. [DOI] [PubMed] [Google Scholar]
- 50. Baker CL, Jr, Baker CL., III Long-term follow-up of arthroscopic treatment of lateral epicondylitis. Am J Sports Med 2008;36:254-260. [DOI] [PubMed] [Google Scholar]
- 51. Savoie FH, III, O’Brien MJ. Arthroscopic tennis elbow release. Instr Course Lect 2015;64:225-230. [PubMed] [Google Scholar]