Abstract
Ankle sprains fall into two main categories: acute ankle sprains and chronic ankle instability, which are among the most common recurrent injuries during occupational activities, athletic events, training and army service.
Acute ankle sprain is usually managed conservatively and functional rehabilitation failure by conservative treatment leads to development of chronic ankle instability, which most often requires surgical intervention.
Enhancing the in-depth knowledge of the ankle anatomy, biomechanics and pathology helps greatly in deciding the management options.
Cite this article: Al-Mohrej OA, Al-Kenani NS. Acute ankle sprain: conservative or surgical approach? EFORT Open Rev 2016;1:34-44. DOI: 10.1302/2058-5241.1.000010.
Keywords: ankle, acute sprain, ankle instability, anatomy, aetiology, diagnosis, rehabilitation, surgical techniques
Introduction
Among musculoskeletal injuries, the incidence of ankle sprains is between 15% and 20% of sports injuries.1,2 The ankle is supported laterally by the anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL) and posterior talofibular ligament (PTFL), whilst the medial aspect is supported by the deltoid ligament.3 Ankle sprains can be either acute sprains, which can be further classified into three grades depending on the severity of the injury, or chronic instability.4
Epidemiology
Among all ankle injuries, ankle sprains are the most common and account for approximately 80%,5,6 of which 77% are lateral sprains. 73% of lateral ankle sprains are due to rupture or tear of the ATFL.7
Ankle sprain incidence rates range from to 5.3-7.0 sprained ankles per 1000 person-years in Europe.6 The ankle sprain incidence rate in the United States is 2.15 per 1000 person-years with no significant differences in gender.8 Furthermore, acute ankle sprains account for between 3% and 10% of all emergency department attendances in the United Kingdom.9
In sports injuries, the ankle is the most traumatised joint and accounts for between 10% and 30% of all injuries.10 A total of 227 epidemiological studies were conducted from 1977 to 2005 involving 70 sports in 38 countries. 32 509 ankle injuries were included, of which 11 847 were ankle sprains.10
Anatomy
An in-depth knowledge of ankle anatomy is imperative for both diagnosis and treatment. Anatomically, the ankle is the connection between the segments of the foot and the leg. The tibio-talar joint, the subtalar joint, and the distal tibiofibular syndesmosis make up the ankle complex.
These articulations work together, co-ordinating the hind-foot movement, which occurs in the sagittal plane, the frontal plane and the transverse plane.11 Mechanically, the three joints produce co-ordinated movement for the hind-foot to rotate around an axis obliquely. As such, the hind-foot movements can be organized kinetically as either supination or pronation: in open kinetic movement inversion, internal rotation and plantar flexion make up supination, and external rotation, eversion and dorsiflexion make up pronation.12
Tibio-talar joint
The tibio-talar joint is made up by the articulation of the dome of the talus, the medial malleolus, the tibial plafond, and the lateral malleolus. Torque is transmitted by the tibio-talar joint shape from the lower leg (rotation) to the foot (pronation and supination) when bearing weight. The axis of rotation of the tibio-talar joint passes through the centre of the medial and lateral malleoli. The tibio-talar joint isolated movement takes place mainly in the sagittal plane but minimal/little transverse and frontal plane motions are also possible.13 The articular surfaces function as the main stabilisers against extra-talar rotation when full load is taken on the ankle complex.14 At this point, the three lateral collateral ligaments provide the joint support.
Subtalar joint
The articulations between the calcaneus and the talus make up the subtalar joint, which transmits torque between the lower leg (rotation) and the foot (pronation and supination).13 The subtalar joint consists of the anterior subtalar joint and the posterior subtalar joint.12 The anterior subtalar joint is made up from the concave proximal surface of the tarsal navicular, the sustentaculum tali of the calcaneus, the anterior-superior facets and the talar head, whilst the posterior subtalar joint is made up between the superior posterior facet of the calcaneus and the inferior-posterior facet of the talus. As such, the anterior subtalar joint and the posterior subtalar joint along with ligaments form an articulation like a ball-and-socket joint. The anterior subtalar joint and the posterior subtalar joint have a common rotation axis, but they are separated from each other by the sinus tarsi and tarsal canal. Hence there are four significant subtalar joint ligaments. First, the lateral talocalcaneal ligament. This is short and descends obliquely from the lateral talar process to the lateral calcaneal surface. Second, the medial talocalcaneal ligament connects the medial talar tubercle with the back of the sustentaculum tali and the medial surface of the calcaneus. The third is the interosseous talocalcaneal ligament which is a broad and flat band in the sinus tarsi. When in eversion, the interosseous talocalcaneal ligament is taut. The fourth, the cervical ligament, is lateral to the sinus tarsi and attached to the superior calcaneal surface. When in eversion, the cervical ligament is taut.
Distal tibiofibular syndesmosis
The distal tibiofibular joint, which is between the tibia and fibula, allows a limited movement between the tibia and the fibula with supportive glide that is mechanically important for the ankle complex.15 The stable roof of the tibio-talar joint mortise is formed by the structure of the distal tibiofibular joint, which is supported by the tibiofibular ligaments and a thick interosseous membrane.
Ankle ligaments
The ankle ligaments fall into three groups: the lateral collateral ligaments (LCLs), medial collateral ligament (MCL), and the ligaments of the tibiofibular syndesmosis. The anterior talofibular ligament (ATFL), the calcaneofibular ligament (CFL), and the posterior talofibular ligament (PTFL) form the LCL (lateral collateral) complex, while the medial collateral ligament is divided into superficial and deep fibres.16
Lateral collateral ligaments
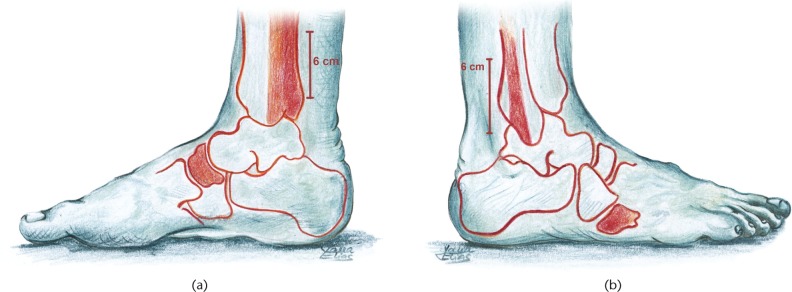
Three ligaments – the ATFL, CFL, and PTFL at the lateral aspect – support the tibio-talar joint, which is a hinge joint that allows dorsiflexion and plantarflexion (Fig. 1).
Fig. 1.
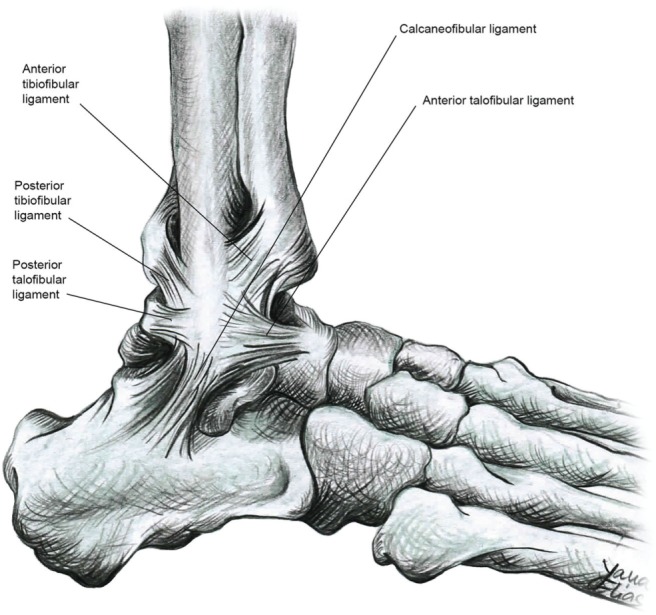
The lateral collateral ligaments of the ankle joint. The tibiofibular ligament is also shown.
Anterior talofibular ligament (ATFL)
The ATFL controls the anterior displacement and the plantar flexion of the talus. It starts at the anterior aspect of the lateral malleolus and is directly connected to the ankle joint capsule. The ATFL is horizontal in a neutral position to the ankle and passes to the intersection on the talar body anterior to the joint surface. In dorsiflexion, the ATFL runs upwards, whilst it inclines downwards in plantar flexion where it is likely to be injured (Fig. 2a).
Fig. 2.
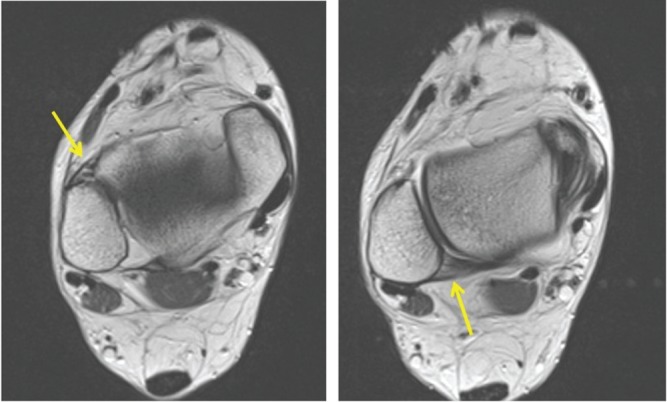
MRI of lateral aspect of the ankle. a) ATFL is identified by the yellow arrow; b) PTFL is identified by the yellow arrow.
The anatomy of the ATFL reveals that it is 10 mm in length, 2 mm in thickness and between 6 and 10 mm in width. The ATFL is 1 cm proximal to the distal tip of the fibula and contiguous with the ankle joint capsule.13,17
Since the ATFL is the weakest of the 3 ligaments, with the lowest ultimate load along with anatomical positions and insertions, it is most commonly injured in a lateral ankle sprain.18
Calcaneofibular ligament (CFL)
This ligament starts from the anterior aspect of the lateral malleolus resting below the lower band of the ATFL. When the ankle is positioned neutrally, the CFL is directed downwards and backwards obliquely. The peroneal tendons and sheaths cross the CFL superficially. The CFL is replaced by an anterior talocalcaneal ligament in about 42% of cases.19
The CFL is rounded in shape, has a 6-8 mm diameter and is roughly 20 mm in length. It is closely connected with the posteromedial section of the peroneal tendon sheath and separated from the ankle joint capsule. The ligament is unique since it is the only ligament that connects the subtalar joint and the tibio-talar joint. Fig. 3 shows a tear of the CFL on MRI scan.
Fig. 3.
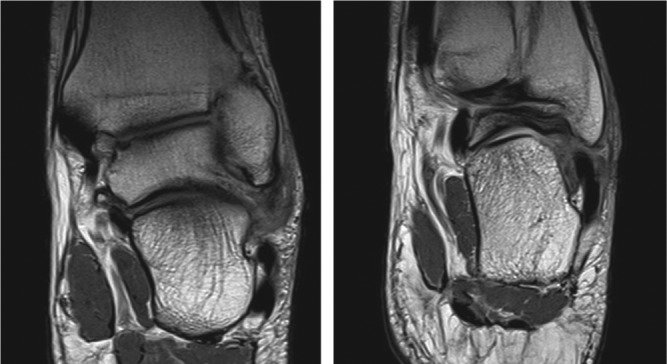
MRI of lateral aspect of the ankle, showing a tear of the CFL.
Posterior talofibular ligament (PTFL)
It starts from the malleolar fossa and runs horizontally to enter into posterolateral aspect of the talus. The ligament is relaxed in the neutral position of the ankle and in plantar flexion, whilst it is tense in dorsiflexion (Fig. 2b). The PTFL is thick and strong and is rarely injured. It is a trapezoidal ligament and lies in a horizontal plane.20 The PTFL seldom undergoes injury in ankle inversion sprains. The ligament is just 10 mm proximal to the distal tip of the fibula.13,17,20
Medial collateral ligament (MCL)
The medial collateral ligament (MCL), which is known as the deltoid ligament, consists of two layers: deep and superficial.17 The MCL, which is multi-fascicular, runs from the medial malleolus passing alongside the talus, calcaneus and then to the navicular bone. Most of the MCL is covered by tendons and extends to the bony foot insertions. The ligament consists of six bands, which vary in the extent of their presence16 (Figs 4 and 5).
Fig. 4.
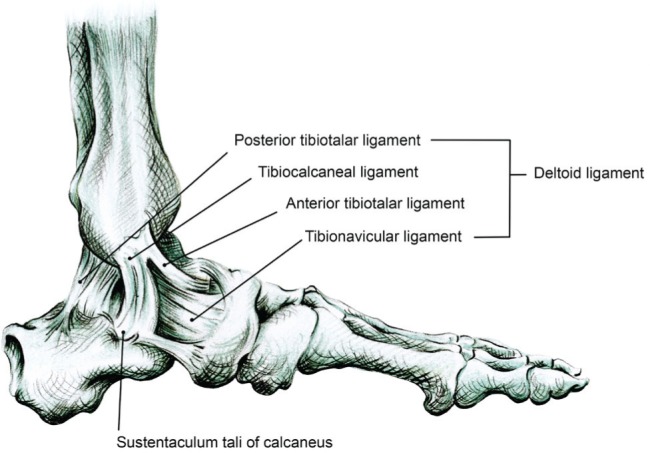
The medial ligament of the ankle (deltoid ligament).
Fig. 5.

MRI of the deltoid ligament.
Muscles and tendons
The joints are supported by groups of muscles and tendons. Muscles can be concentric or eccentric due to their different behavioural actions.13 The peroneal brevis and peroneal longus are significant factors in the protection against lateral ankle sprain and in hind-foot supination control.21 The lateral ankle complex is also supported and stabilised by the peroneus tertius, extensor digitorum brevis, extensor digitorum longus and tibialis anterior. In addition, they can prevent lateral ligament injury by slowing the plantar-flexion supination.22 CFL is closely connected with the posteromedial peroneal tendon sheaths.23 The tunnel for the flexor hallucis longus tendon is formed partially by some fibres, and the middle and posterior parts of the MCL are covered by the tendon sheath of the tibialis posterior muscle.
Innervation
The sacral and lumbar plexuses provide the sensory and motor support to the ankle complex. The sensory supply to the muscles is provided by the superficial peroneal, deep peroneal, sural, saphenous and tibial nerves, while the motor supply to the muscles is provided by the superficial peroneal, deep peroneal and tibial nerves.13
The innervation of the joint capsule and that of the lateral ligaments of the subtalar and tibio-talar joints is by mechanoreceptors.24 The peroneal muscles are of high significance for proprioception of the ankle complex.25
Aetiology and classification
Understanding the mechanism of ankle sprains is seminal to diagnosis, management and prevention.
Ankle sprains are mostly the result of damage to LCLs, including ATFL, CFL, PTFL. The ankle sprain occurs chiefly in inversion, foot internal twisting, and plantarflexion, associated with adduction of the ankle (Fig. 6). Many ankle sprains occur when the foot is in systematic loading and unloading.13 Mechanically, the ATFL is injured due to forced supination in plantarflexion movement and the CFL is injured when the foot is in dorsiflexion.26 In detail, sprain is characterised by inversion and adduction (internal twisting) whilst the tibio-talar joint is in plantarflexion. Conversely, forced supination merely results in a subtalar sprain.27 Ankle sprains mostly involving the LCL are known as inversion sprains. The weakest of the ligaments is the ATFL, and when the mechanism of injury occurs around the lateral aspect of the ankle and CFL damage occurs followed by the PTFL in sequence. The occurrence of combined rupture of the ATFL and CFL is reported as 20%, and the PTFL injury does not occur unless the ankle joint undergoes dislocation.28 A hyperdorsiflexion trauma might cause damage to the syndesmosis and an eversion injury will cause injury to the deltoid ligaments.29
Fig. 6.
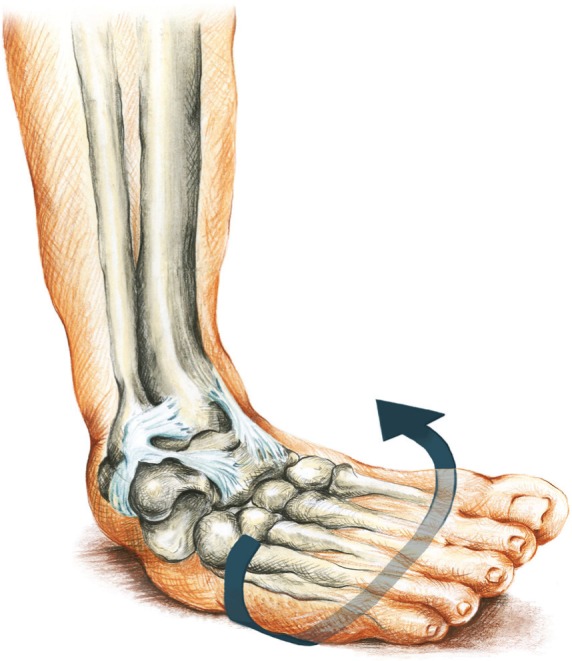
Inversion of the ankle is the main mechanism in lateral sprains.
‘Ankle sprain’ refers to diverse morphological and pathological conditions that range from ligamentous overstretching to complete rupture with joint instability. Depending on the nature of severity, the scheme of ankle sprains falls into three grades. Classification helps in identifying the damage level and correct treatment.31 Table 1 shows the three grades of acute ankle sprain. Practically, acute ankle sprain can be classified as stable or unstable according to the findings on physical examination.
Table I.
Classification of acute ankle sprain according to its grade, severity, pathophysiology and clinical findings
| Grade | Severity | Pathophysiology | Clinical findings |
|---|---|---|---|
| Grade 1 | Mild | Stretch of the ATFL, causing tear of the ligament fibres. | Mild swelling, no laxity, little ecchymosis, and difficulty in full weight bearing. |
| Grade 2 | Moderate | Moderate injury to the lateral ligamentous complex with a complete tear of the ATFL ± Partial tear of the CFL. | Localised swelling, hemorrhage ecchymosis, and anterolateral tenderness. Abnormal laxity may be mild or absent. |
| Grade 3 | Severe | Complete disruption of the ATFL along with CFL and PTFL. | Tenderness, swelling and ecchymosis on the lateral ankle and heel side with marked laxity. |
Ankle instability
Ankle instability is either mechanical or functional instability, or both. Mechanical instability may occur following certain anatomical defects such as ligamentous tear, synovial irritation, arthrokinematic changes, or degenerative pathological laxity.32-34 Functional instability means the occurrence of recurrent ankle instability and the sensation of joint instability due to the contributions of two factors: proprioceptive and neuromuscular deficits.35
Clinical evaluation
Detailed history and careful physical examination are crucial for diagnosis and management of ankle sprains, as they reveal the severity of the ankle sprain the patient has experienced. The ligament injury can be assessed by observing swelling and weight-bearing ability. Therefore, a thorough history is essential to evaluate the ankle injury. It can help identify a whole set of important diagnostic clues, such as:
The patient’s ability to walk after the injury, which helps to grade the level of injury.
The patient’s injury mechanism, which can help guide the ankle sprain examination.
The fact of whether the same ankle was injured before or not, because patients who have undergone ankle sprains are prone to being re-injured.
Patients who may have undergone ankle sprains should be physically examined by various methods such as checking the patient’s ability to bear weight, visual and hands-on inspection, injury-specific physical diagnostic tests, and palpation. The physician should also check for swelling and ecchymosis and should palpate the fibula to feel fractures, if any. In addition, if a tissue deficit or tenderness can be found, then the Thompson Test should be carried out to exclude a tendo Achilles injury. Tenderness should be also checked using the sites of Ottawa Ankle Rules (Fig. 7) since distal tibial or fibular tenderness may reveal a fracture accompanying an eversion or inversion strain. An osteochondral talar dome fracture may be inferred by pain and tenderness on tibio-talar joint line palpation. The physician should also check for pain on passive gentle eversion and inversion.
Fig. 7.
Lateral (a) and medial (b) views of the ankle showing the regions of Ottawa ankle rules.
a) Bone tenderness at the distal 6 cm of the posterior edge of the tibia or tip of the medial malleolus; b) Bone tenderness at the distal 6 cm of the posterior edge of the fibula or tip of the lateral malleolus.
Specific examinations should be carried out to manoeuvre and identify the nature of the ankle sprain through certain tests, such as:
Talar-Tilt test: helps to identify excessive ankle inversion. The patient sits with their knees extended and the clinician supports the leg with both hands behind the fibula and the tibia away from the site of pain. The clinician then squeezes the fibula and the tibia together adding more pressure gradually.
Anterior ‘drawer’ test: helps to identify excessive anterior displacement of the talus on the tibia. The ankle should be placed in a neutral position and the leg should be stabilised over the distal tibia with the patient relaxed. The clinician cups the heel with one hand and pulls the foot forward.
Anterolateral ‘drawer’ test: This test reveals an isolated laxity of the lateral ankle joint by holding the lateral malleolus and the lateral talus when anterolateral rotatory force is applied resulting in subluxation. The anterolateral drawer test shows a higher degree of accuracy and sensitivity in the determination of lateral ankle laxity in cadaveric specimens. Also, the test has been shown to have higher linear correlation with the Telos stress device.36
Figures 8 and 9 show how the ‘talar-tilt’ test and anterior ‘drawer’ test are performed. Comparison with the contralateral ankle is essential for both tests.
Fig. 8.
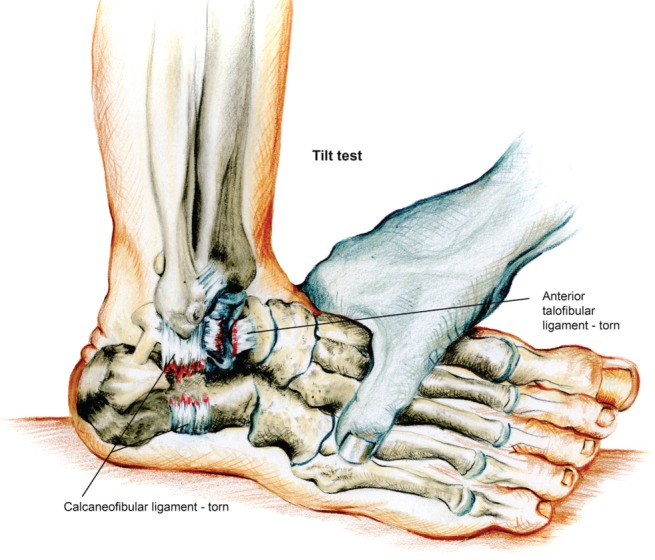
‘Talar-tilt’ test.
Fig. 9.
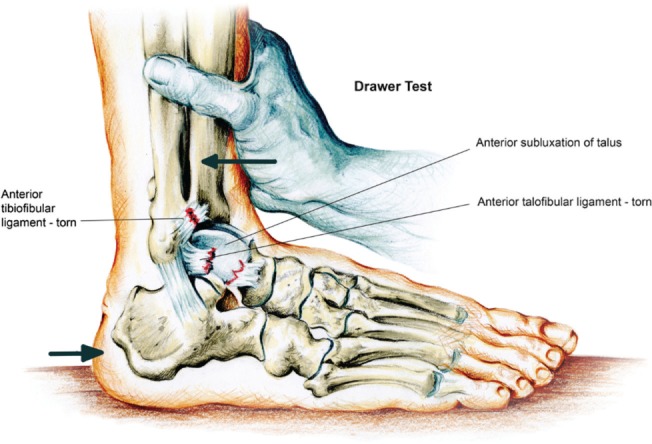
Anterior ‘drawer’ test.
The Squeeze test and External Rotation Stress test can be performed according to the findings and to exclude associated injuries. However, patients with acute ankle injury can be successfully triaged without deferring the examination.
Imaging assessments
Plain radiographs should include anteroposterior, lateral weight-bearing and mortise views. In the mortise view, the Menard-Shenton line can be used. X-rays can be used to diagnose ankle sprains and associated injuries, including distal fibular fractures, malleolar fractures, syndesmosis separation, and talar dome fractures. Stress radiography is an important tool to diagnose the laxity. The Telos device is helpful in the performance of the stress radiography. However, the device is not available in many hospitals.
Historically, the Ottawa Ankle Rules (OAR) were developed to reduce the unnecessary radiographs and decide when radiographic studies are indicated in patients who undergo ankle trauma.37
The OAR were first tested on adult patients with ankle sprains from acute injuries, revealing almost perfect results for adult and young populations.37 A previous study revealed that the OAR were significantly sensitive in excluding ankle fractures.38 As such, the OAR reduced unnecessary radiographs by 30-40%. Ottawa Rules can be summarized by the matrix in Table 2.
Table II.
Ottawa Ankle and Foot Rules
| Ottawa Ankle Rules | Ottawa Foot Rules |
|---|---|
| An ankle radiograph is required only if pain is indicated in the malleolar part and any of these is present: | A foot radiograph is required only if pain is indicated in the mid-foot and any of these is present: |
| • Bone tenderness at lateral malleolus or posterior edge | • Bone tenderness at the 5th metatarsal base |
| • Bone tenderness at medial malleolus or posterior edge | • Navicular bone tenderness |
| • Unable to bear weight | • Unable to bear weight |
Whilst ultrasound can be a valuable technique, it is user-dependent;39 Magnetic Resonance Imaging (MRI) can be also helpful to rule out associated lesions and degenerative changes and assess ligamentous injuries.40 However, MRI is equivalent to plain radiographs in acute injury and is more useful in assessing painful ankle sprains after a 6-8 week period of therapy.41
If a patient experiences more than one injury, CT and MRI scans are necessary.
Acute ankle sprain
Presentation
The history of acute ankle instability indicates whether it is a single injury, or a repetitive or multiple injury. Patients who experience acute ankle instability are most often unable to rely on their injured ankle and do not get involved in strenuous everyday or occupational activities.
On examination, swelling and the ability to weight-bear are checked. For tenderness, the CFL, ATFL and PTFL, deltoid, and malleoli are examined along with the peroneal tendons and Achilles tendon as the physician becomes more focussed on the location and the severity of the ankle injury. For example, a fracture might be excluded by the patient’s ability to weight-bear. Yet, weight-bearing alone is not a criterion to exclude a lateral ankle fracture which may occur particularly in SE type II fractures, whilst a history of an audible snap accompanied by swelling and pain indicates a Grade III ankle sprain. Lateral malleolar tenderness is generally not present if there is no fracture. Through meticulous palpation, the structures affected by the ankle injury can be identified reasonably accurately. Clinical reports reveal that 72% of patients experiencing CFL insertional tenderness had a ruptured CFL while 52% of patients experiencing ATFL tenderness had a ruptured ligament.42
Associated lesions
Acute ankle sprain can possibly give rise to a high incidence of associated lesions.43,44 The injuries associated with acute ankle sprain can be classified into four main groups: nerve injuries, soft-tissue injuries, intra-articular injuries and bony injuries.
However, these lesions are more associated with chronic ankle instability than acute ankle sprain. The patient becomes unable to maintain balance on the injured ankle and postural sway of the patient can be observed.45 Furthermore, lateral ankle sprain can be evidenced by the inability of the patient to sense joint position.46 In addition, the peroneal muscles show delayed reaction in response to any sudden inversion stress of the ankle.47
Lateral ankle sprain is also sometimes accompanied by an injury to the peroneal nerve.48 In lateral ankle sprain, 17% of Grade II injuries revealed slowed nerve conduction velocity while 86% were seen in those with Grade III. Slowed nerve conduction velocity of the tibial nerve accompanied 10% of Grade II injuries and 83% of Grade III injuries.49
Strength deficit is also evidenced in acute ankle sprain.50 Muscle weakness responsible for the eversion and pronation of the ankle complex contributes to functional instability in the lateral ankle sprain.51 Lateral ankle sprain can possibly be followed by reduced dorsiflexion which is part of overall functional instability.52 Other associated lesions should be considered (though rare), including lesion of the peroneus brevis tendon, osteochondral lesions of the tibial plafond, false aneurysm of the peroneal artery, sinus tarsi syndrome, anterolateral impingement syndrome and superior peroneal retinacular laxity.53
Bone contusions, osteochondral lesions and ligamentous lesions including syndesmotic injuries are diagnosed by MRI scan.54 In a study conducted on 261 ankle MRI scans of athletes who had acute ankle sprains, acute osteochondral lesions of the lateral talar dome were seen in 20 ankles (7.7%) whilst chronic lateral osteochondral lesions were 1.1%. Of note, talar bone contusion risk increased more than three times for ankles with complete lateral ligament ruptures, but this increase was not seen in ankles that had syndesmotic involvement.55 Acute osteochondral talar lesions are areas of diffuse hyper-intensity of the lateral talar dome adjacent directly to the subchondral plate with or without cartilage surface damage. On the other hand, a chronic osteochondral lesion is a well-demarcated or partially cystic lesion in the same site with or without surrounding bone oedema.56 The study also showed that acute osteochondral lesions of the lateral talar dome were seen in 20 (7.7%) ankles: 55% of these ankles had intact cartilage and only 45% showed cartilage damage while the chronic lateral osteochondral lesions were only 1.1%.
As for traumatic acute osteochondral lesions in the talus with subchondral bone contusions, these were seen in about 8% of ankles with or without articular surface damage. In an arthroscopic study, lateral talar osteochondral lesions were seen in 71% of ankles with fractures: the study revealed that most lesions were traumatic in origin.57
Compartment syndrome following ankle sprain was reported in the case of a 23-year-old soldier who suffered from an injury playing basketball which resulted in an acute compartment syndrome.58 Only five previous cases similar to this have been reported. The study concluded that compartment syndrome may develop after an ankle sprain, probably due to a tear of the peroneus longus muscle or an injury to the peroneal artery.59
Management
Conservative approach
Acute ankle injury can be managed conservatively using various by RICE protocols of immobilisation and rehabilitation.
RICE protocol
The acronym stands for the four main procedural methods of treatment of the ankle: Rest, Ice, Compression and Elevation, which can be performed in the first 2-3 days.
Patients are provided with crutches to help them walk until they can walk normally. Weight-bearing is limited to light weight-bearing.
As part of cryotherapy, ice immersion is recommended for up to 20 minutes every 2-3 hours.
To apply compression, the patient is provided with a flexible bandage to reduce swelling.
To facilitate a reduction in swelling and for better venous and lymphatic drainage, the injured ankle should be elevated at a level higher than the heart.
Mild ankle sprains can be managed by using cryotherapy that can potentially decrease secondary hypoxia.60 It is highly recommended that the patient’s ankle temperature should be maintained at about 12 °C by placing ice cubes onto the injured site, which should be cooled for 15 minutes every couple of hours over the first two days, until stabilised.61 However, in 2014, Mirkin recanted part of his RICE guidelines, stating that it seems that ice and rest may delay healing.62 In the inflammatory stage of the acute ankle injuries, non-steroidal anti-inflammatory medications can be used instead.
Immobilisation
Ankle injuries of Grade I do not need immobilisation since they can be treated well by using a flexible or elastic wrap for a few days.63 However, Grade II ankle injuries are likely to require support by using a flexible wrap and a splint for the first few days until they are pain-free. In Grade III, controlling the range of the patient’s motion is recommended. Patients are also recommended to use an ankle rigid support or a plaster cast to reduce pain and injury during a short period (1 week) of immobilisation. Conversely, casting is recommended using a below-knee cast, air-cast brace, tubular compression bandage or ‘Bledsoe’ immobilisation boot.40 Casting, however, has been shown to yield inferior functional results by many authors compared with orthosis and early weight-bearing.63
Though many patients prefer cast immobilisation, we suggest starting physiotherapy as early as possible for the following reasons: to give time for the ice application to control pain and swelling; to improve and maintain the range of motion; and to minimize the risk of stiffness and muscle wasting, two factors which can delay the patient from returning to their usual activities.
Rehabilitation
After ankle injury, functional rehabilitation has a highly positive effect, and in addition can help patients perform normal activities and prevent the possibility of chronic instability of the ankle. Semi-rigid ankle braces can be used in order to create appropriate foot support. Motion exercises such as foot circles, mild tendon stretching, alphabet exercises, dorsiflexion, eversion, inversion, picking up marbles with the toes, and toe curling and walking are encouraged to assist lymphatic drainage.61 It is also recommended to wrap the ankle with an elastic bandage to control the oedema.61 After injury, patients can be provided with crutches to facilitate mobility when the ankle sprain is painful. Weight-bearing is possible if tolerated. To facilitate rehabilitation, ankle-foot orthoses can be used along with ankle braces filled with air or gel, which can be used to limit plantarflexion-dorsiflexion.64 The patient often needs a proprioceptive training programme, as proprioception is likely to be affected. Occupational and sports activities that require strenuous physical efforts are restricted over the first period of time to prevent pain and poor outcomes. For ankle injuries of Grade I and II, patients should start functional rehabilitation when swelling and pain decrease so that they can start simple exercises when they feel that the activities are pain-free. To prevent recurrence, the rehabilitation programme should last between 3 and 6 weeks. During the functional rehabilitation programme, braces, elastic bandages, taping or splints are recommended in order to decrease ankle instability and control swelling.65
Surgical approach
Acute ankle injuries are almost always managed by non-operative methods. A previous study revealed that patients who underwent acute surgical treatment took longer to return to work.66,67 Also, studies revealed that surgery was not helpful in reducing additional complications, costs and risks.66,68 Previously, in ankle sprains of Grade I and Grade II, the emphasis was placed on early application of RICE guidelines, while ankle sprains of Grade III might require surgical intervention.66 However, evidence of benefit by surgical intervention has not been forthcoming. Regardless of severity, surgery for acute ankle sprain is not recommended anymore.69
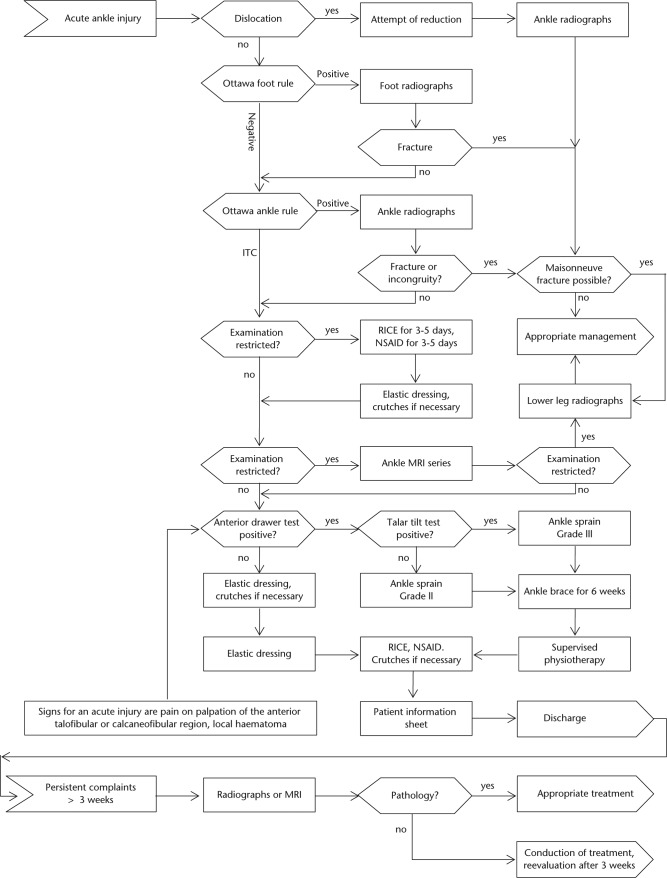
In the authors’ opinion, successful treatment of acute ankle sprain can be achieved with individualised, aggressive and non-operative measures. Surgery should always be indicated on an individual basis. Indications for the surgery are usually associated with unstable ankle fractures, OCD (osteochondral defects), loose bodies, or peroneal tendon tears. Based on the best available literature, the evidence-based algorithm shown in Figure 10 summarises the diagnosis and treatment of acute ankle injuries.70
Fig. 10.
Evidence-based algorithm for the diagnosis and treatment of acute ankle injuries.
Prognosis
Although classified into grades, the prognosis of ankle injuries is not determined by any schemata. Meticulous diagnosis and treatment is highly likely to determine prognosis. Prognosis is also be affected by many factors such as the history of the ankle instability and associated lesions.71-73 In our opinion, the most important prognostic factor for acute ankle sprain is the efficiency of the physiotherapy programme.
Conclusions
Acute ankle sprain is a very common injury which comprises 80% of all ankle injuries.
Acute ankle sprain affects almost exclusively the lateral ligamentous complex including ATFL followed by CFL, while PTFL is rarely of clinical significance.
The injury is mostly produced by excessive inversion and plantarflexion of the ankle.
Careful history taking and physical examination is crucial to guide imaging assessment, management and prognosis.
Ottawa Ankle Rules are commonly used in assessing ankle sprains and can also help in deciding when radiographic studies are indicated in patients who undergo ankle trauma.
Starting a physiotherapy programme as early as possible is essential to control pain and swelling, to improve and maintain the range of motion, and to minimize the risk of stiffness and muscle wasting, which are the two decisive factors which delay patients from returning to their normal activities.
Cast immobilisation has a limited role and should be considered only in cases of fractures and inability to weight-bear.
Regardless of severity, surgery for acute ankle sprain is not recommended anymore.
Acknowledgments
The authors would like to duly express their heart-felt appreciation and gratitude to Ms. Jana Elias, Cambridge School of Art (BA [Hons] Illustration, 3rd year) Cambridge, UK, together with colleague artists, for meticulously providing this manuscript with its artwork.
Footnotes
Conflict of Interest: None declared
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Ekstrand J, Gillquist J. Soccer injuries and their mechanisms: a prospective study. Med Sci Sports Exerc 1983;15:267-270. [DOI] [PubMed] [Google Scholar]
- 2. Junge A, Engebretsen L, Mountjoy ML, et al. Sports injuries during the Summer Olympic Games 2008. Am J Sports Med 2009;37:2165-2172. [DOI] [PubMed] [Google Scholar]
- 3. Bozkurt M, Doral MN. Anatomic factors and biomechanics in ankle instability. Foot Ankle Clin 2006;11:451-463. [DOI] [PubMed] [Google Scholar]
- 4. Clanton TO. Athletic injuries to the soft tissues of the foot and ankle. In: Coughlin MJ, Mann RA, eds. Surgery of the foot and ankle. 7th ed. St Louis: Mosby; 1999:1101-1106. [Google Scholar]
- 5. Berson BL, Rolnick AM, Ramos CG, Thornton J. An epidemiologic study of squash injuries. Am J Sports Med 1981;9:103-106. [DOI] [PubMed] [Google Scholar]
- 6. Hølmer P, Søndergaard L, Konradsen L, Nielsen PT, Jørgensen LN. Epidemiology of sprains in the lateral ankle and foot. Foot Ankle Int 1994;15:72-74. [DOI] [PubMed] [Google Scholar]
- 7. Woods C, Hawkins R, Hulse M, Hodson A. The Football Association Medical Research Programme: an audit of injuries in professional football: an analysis of ankle sprains. Br J Sports Med 2003;37:233-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ., Jr The epidemiology of ankle sprains in the United States. J Bone Joint Surg [Am] 2010;92-A:2279-2284. [DOI] [PubMed] [Google Scholar]
- 9. Bridgman SA, Clement D, Downing A, et al. Population based epidemiology of ankle sprains attending accident and emergency units in the West Midlands of England, and a survey of UK practice for severe ankle sprains. Emerg Med J 2003;20:508-510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med 2007;37:73-94. [DOI] [PubMed] [Google Scholar]
- 11. Huson A. Joints and movements of the foot: terminology and concepts. Acta Morphol Neerl Scand 1987;25:117-130. [PubMed] [Google Scholar]
- 12. Rockar PA., Jr The subtalar joint: anatomy and joint motion. J Orthop Sports Phys Ther 1995;21:361-372. [DOI] [PubMed] [Google Scholar]
- 13. Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train 2002;37:364-375. [PMC free article] [PubMed] [Google Scholar]
- 14. Stormont DM, Morrey BF, An KN, Cass JR. Stability of the loaded ankle. Relation between articular restraint and primary and secondary static restraints. Am J Sports Med 1985;13:295-300. [DOI] [PubMed] [Google Scholar]
- 15. Mulligan BR. Manual Therapy: “NAGS”, “SNAGS”, “MWMS”, Etc. Third edition Wellington, New Zealand: Plane View Services LTD, 1995. [Google Scholar]
- 16. Milner CE, Soames RW. Anatomy of the collateral ligaments of the human ankle joint. Foot Ankle Int 1998;19:757-760. [DOI] [PubMed] [Google Scholar]
- 17. Golanó P, Vega J, de Leeuw PA, et al. Anatomy of the ankle ligaments: a pictorial essay. Knee Surg Sports Traumatol Arthrosc 2010;18:557-569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ferran NA, Maffulli N. Epidemiology of sprains of the lateral ankle ligament complex. Foot Ankle Clin 2006;11:659-662. [DOI] [PubMed] [Google Scholar]
- 19. Trouilloud P, Dia A, Grammont P, Gelle MC, Autissier JM. [Variations in the calcaneo-fibular ligament (lig. calcaneofibulare). Application to the kinematics of the ankle]. Bull Assoc Anat (Nancy) 1988;72:31-35.[Article in French] [PubMed] [Google Scholar]
- 20. Taser F, Shafiq Q, Ebraheim NA. Anatomy of lateral ankle ligaments and their relationship to bony landmarks. Surg Radiol Anat 2006;28:391-397. [DOI] [PubMed] [Google Scholar]
- 21. Ashton-Miller JA, Ottaviani RA, Hutchinson C, Wojtys EM. What best protects the inverted weightbearing ankle against further inversion? Evertor muscle strength compares favorably with shoe height, athletic tape, and three orthoses. Am J Sports Med 1996;24:800-809. [DOI] [PubMed] [Google Scholar]
- 22. Sinkjaer T, Toft E, Andreassen S, Hornemann BC. Muscle stiffness in human ankle dorsiflexors: intrinsic and reflex components. J Neurophysiol 1988;60:1110-1121. [DOI] [PubMed] [Google Scholar]
- 23. Sarrafian SK. Anatomy of the foot and ankle. Descriptive, topographic, functional. 2nd edition. Philadelphia: Lippincott Williams and Wilkins;1993:159-217. [Google Scholar]
- 24. Takebayashi T, Yamashita T, Minaki Y, Ishii S. Mechanosensitive afferent units in the lateral ligament of the ankle. J Bone Joint Surg [Br] 1997;79-B:490-493. [DOI] [PubMed] [Google Scholar]
- 25. Khin-Myo-Hla, Ishii T, Sakane M, Hayashi K. Effect of anesthesia of the sinus tarsi on peroneal reaction time in patients with functional instability of the ankle. Foot Ankle Int 1999;20:554-559. [DOI] [PubMed] [Google Scholar]
- 26. Bennett WF. Lateral ankle sprains. Part I: Anatomy, biomechanics, diagnosis, and natural history. Orthop Rev 1994;23:381-387. [PubMed] [Google Scholar]
- 27. Meyer JM, Garcia J, Hoffmeyer P, Fritschy D. The subtalar sprain. A roentgenographic study. Clin Orthop Relat Res 1988;226:169-173. [PubMed] [Google Scholar]
- 28. Dijk CNv. On diagnostic strategies in patients with severe ankle sprain. The Netherlands: University of Amsterdam, 1994. [Google Scholar]
- 29. Clanton TO, Paul P. Syndesmosis injuries in athletes. Foot Ankle Clin 2002;7:529-549. [DOI] [PubMed] [Google Scholar]
- 30. Inman VT. The joints of the ankle. Baltimore: Williams & Wilkins, 1976. [Google Scholar]
- 31. Chorley JN, Hergenroeder AC. Management of ankle sprains. Pediatr Ann 1997;26:56-64. [DOI] [PubMed] [Google Scholar]
- 32. Kim JS, Young KW, Cho HK, et al. Concomitant syndesmotic instability and medial ankle instability are risk factors for unsatisfactory outcomes in patients with chronic ankle instability. Arthroscopy 2015;31:1548-1556. [DOI] [PubMed] [Google Scholar]
- 33. Lohrer H, Nauck T, Gehring D, et al. Differences between mechanically stable and unstable chronic ankle instability subgroups when examined by arthrometer and FAAM-G. J Orthop Surg Res 2015;10:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Knupp M, Lang TH, Zwicky L, Lötscher P, Hintermann B. Chronic ankle instability (Medial and Lateral). Clin Sports Med 2015;34:679-688. [DOI] [PubMed] [Google Scholar]
- 35. Freeman MA. Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg [Br] 1965;47-B:669-677. [PubMed] [Google Scholar]
- 36. Phisitkul P, Chaichankul C, Sripongsai R, et al. Accuracy of anterolateral drawer test in lateral ankle instability: a cadaveric study. Foot Ankle Int 2009;30:690-695. [DOI] [PubMed] [Google Scholar]
- 37. Stiell IG, McKnight RD, Greenberg GH, et al. Implementation of the Ottawa ankle rules. JAMA 1994;271:827-832. [PubMed] [Google Scholar]
- 38. Bachmann LM, Kolb E, Koller MT, Steurer J, ter Riet G. Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot: systematic review. BMJ 2003;326:417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Jacobson JA. Musculoskeletal sonography and MR imaging. A role for both imaging methods. Radiol Clin North Am 1999;37:713-735. [DOI] [PubMed] [Google Scholar]
- 40. Lamb SE, Marsh JL, Hutton JL, Nakash R, Cooke MW; Collaborative Ankle Support Trial (CAST Group). Mechanical supports for acute, severe ankle sprain: a pragmatic, multicentre, randomised controlled trial. Lancet 2009;373:575-581. [DOI] [PubMed] [Google Scholar]
- 41. Kaminski TW, Hertel J, Amendola N, et al. ; National Athletic Trainers’ Association. National Athletic Trainers’ Association position statement: conservative management and prevention of ankle sprains in athletes. J Athl Train 2013;48:528-545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Funder V, Jørgensen JP, Andersen A, et al. Ruptures of the lateral ligaments of the ankle. Clinical diagnosis. Acta Orthop Scand 1982;53:997-1000. [DOI] [PubMed] [Google Scholar]
- 43. Fallat L, Grimm DJ, Saracco JA. Sprained ankle syndrome: prevalence and analysis of 639 acute injuries. J Foot Ankle Surg 1998;37:280-285. [DOI] [PubMed] [Google Scholar]
- 44. Mattacola CG, Dwyer MK. Rehabilitation of the ankle after acute sprain or chronic instability. J Athl Train 2002;37:413-429. [PMC free article] [PubMed] [Google Scholar]
- 45. Bernier JN, Perrin DH, Rijke A. Effect of unilateral functional instability of the ankle on postural sway and inversion and eversion strength. J Athl Train 1997;32:226-232. [PMC free article] [PubMed] [Google Scholar]
- 46. Hertel J. Functional instability following lateral ankle sprain. Sports Med 2000;29:361-371. [DOI] [PubMed] [Google Scholar]
- 47. Konradsen L, Ravn JB. Ankle instability caused by prolonged peroneal reaction time. Acta Orthop Scand 1990;61:388-390. [DOI] [PubMed] [Google Scholar]
- 48. Bullock-Saxton JE. Local sensation changes and altered hip muscle function following severe ankle sprain. Phys Ther 1994;74:17-28; discussion 28-31. [DOI] [PubMed] [Google Scholar]
- 49. Nitz AJ, Dobner JJ, Kersey D. Nerve injury and grades II and III ankle sprains. Am J Sports Med 1985;13:177-182. [DOI] [PubMed] [Google Scholar]
- 50. Konradsen L, Olesen S, Hansen HM. Ankle sensorimotor control and eversion strength after acute ankle inversion injuries. Am J Sports Med 1998;26:72-77. [DOI] [PubMed] [Google Scholar]
- 51. Wilkerson GB, Pinerola JJ, Caturano RW. Invertor vs. evertor peak torque and power deficiencies associated with lateral ankle ligament injury. J Orthop Sports Phys Ther 1997;26:78-86. [DOI] [PubMed] [Google Scholar]
- 52. Wilson RW, Gieck JH, Gansneder BM, et al. Reliability and responsiveness of disablement measures following acute ankle sprains among athletes. J Orthop Sports Phys Ther 1998;27:348-355. [DOI] [PubMed] [Google Scholar]
- 53. Bonnin M, Tavernier T, Bouysset M. Split lesions of the peroneus brevis tendon in chronic ankle laxity. Am J Sports Med 1997;25:699-703. [DOI] [PubMed] [Google Scholar]
- 54. Brown KW, Morrison WB, Schweitzer ME, Parellada JA, Nothnagel H. MRI findings associated with distal tibiofibular syndesmosis injury. AJR Am J Roentgenol 2004;182:131-136. [DOI] [PubMed] [Google Scholar]
- 55. Roemer FW, Jomaah N, Niu J, et al. Ligamentous injuries and the risk of associated tissue damage in acute ankle sprains in athletes: a cross-sectional MRI study. Am J Sports Med 2014;42:1549-1557. [DOI] [PubMed] [Google Scholar]
- 56. Griffith JF, Lau DT, Yeung DK, Wong MW. High-resolution MR imaging of talar osteochondral lesions with new classification. Skeletal Radiol 2012;41:387-399. [DOI] [PubMed] [Google Scholar]
- 57. Takao M, Ochi M, Uchio Y, et al. Osteochondral lesions of the talar dome associated with trauma. Arthroscopy 2003;19:1061-1067. [DOI] [PubMed] [Google Scholar]
- 58. Ward NJ, Wilde GP, Jackson WF, Walker N. Compartment syndrome following ankle sprain. J Bone Joint Surg [Br] 2007;89-B:953-955. [DOI] [PubMed] [Google Scholar]
- 59. Arciero RA, Shishido NS, Parr TJ. Acute anterolateral compartment syndrome secondary to rupture of the peroneus longus muscle. Am J Sports Med 1984;12:366-367. [DOI] [PubMed] [Google Scholar]
- 60. Knight KL. Initial care of acute injuries: the RICES technique. In: Cryotherapy in sport injury management. Champaign, Ill: Human Kinetics; 1995:209-215. [Google Scholar]
- 61. Wolfe MW, Uhl TL, Mattacola CG, McCluskey LC. Management of ankle sprains. Am Fam Physician 2001;63:93-104. [PubMed] [Google Scholar]
- 62. Bleakley C, McDonough S, MacAuley D. The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med 2004;32:251-261. [DOI] [PubMed] [Google Scholar]
- 63. Seah R, Mani-Babu S. Managing ankle sprains in primary care: what is best practice? A systematic review of the last 10 years of evidence. Br Med Bull 2011;97:105-135. [DOI] [PubMed] [Google Scholar]
- 64. Wexler RK. The injured ankle. Am Fam Physician 1998;57:474-480. [PubMed] [Google Scholar]
- 65. Refshauge KM, Raymond J, Kilbreath SL, Pengel L, Heijnen I. The effect of ankle taping on detection of inversion-eversion movements in participants with recurrent ankle sprain. Am J Sports Med 2009;37:371-375. [DOI] [PubMed] [Google Scholar]
- 66. Kerkhoffs GM, Handoll HH, de Bie R, Rowe BH, Struijs PA. Surgical versus conservative treatment for acute injuries of the lateral ligament complex of the ankle in adults. Cochrane Database Syst Rev 2002;3:CD000380. [DOI] [PubMed] [Google Scholar]
- 67. Kannus P, Renström P. Treatment for acute tears of the lateral ligaments of the ankle. Operation, cast, or early controlled mobilization. J Bone Joint Surg [Am] 1991;73-A:305-312. [PubMed] [Google Scholar]
- 68. Shrier I. Treatment of lateral collateral ligament sprains of the ankle: a critical appraisal of the literature. Clin J Sport Med 1995;5:187-195. [DOI] [PubMed] [Google Scholar]
- 69. Chaudhry H, Simunovic N, Petrisor B. Cochrane in CORR ®: surgical versus conservative treatment for acute injuries of the lateral ligament complex of the ankle in adults (review). Clin Orthop Relat Res 2015;473:17-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Polzer H, Kanz KG, Prall WC, et al. Diagnosis and treatment of acute ankle injuries: development of an evidence-based algorithm. Orthop Rev (Pavia) 2012;4:e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Docherty CL, Moore JH, Arnold BL. Effects of strength training on strength development and joint position sense in functionally unstable ankles. J Athl Train 1998;33:310-314. [PMC free article] [PubMed] [Google Scholar]
- 72. Hockenbury RT, Sammarco GJ. Evaluation and treatment of ankle sprains: clinical recommendations for a positive outcome. Phys Sportsmed 2001;29:57-64. [DOI] [PubMed] [Google Scholar]
- 73. Willems T, Witvrouw E, Verstuyft J, Vaes P, De Clercq D. Proprioception and Muscle Strength in Subjects With a History of Ankle Sprains and Chronic Instability. J Athl Train 2002;37:487-493. [PMC free article] [PubMed] [Google Scholar]