Abstract
Chronic posterolateral rotatory instability (PLRI) is the most common form of chronic elbow instability.
PLRI usually occurs from a fall on the outstretched hand. On impact, the radial head and ulna rotate externally coupled with valgus displacement of the forearm. This leads to posterior displacement of the radial head relative to the capitellum, thus causing disruption of some or all of the lateral-sided stabilisers.
PLRI is mainly a clinical diagnosis with a history of instability, clicking and lateral-sided pain, with a positive clinical examination including the pivot-shift test, push-up, chair and tabletop test.
MRI can often help guide diagnosis but more commonly assists in surgical planning.
Surgery is indicated in patients with persistent, symptomatic instability of the elbow causing pain or functional deficit. There are several surgical techniques to treat PLRI, often leading to good to excellent results.
An open or arthroscopic technique has been successfully used in patients with symptomatic PLRI following one or more episodes of dislocation or subluxation. At the pre-operative examination under general anaesthesia, all of our patients had a positive pivot-shift test but not a frank dislocation. We prefer to perform a lateral collateral ligament (LCL) reconstruction with an allograft tendon.
The outcomes after repair are good to excellent in the majority of patients. Results of acute repair are generally better compared with reconstruction. This is due to the fact that predictive factors for a poor outcome include the number of previous surgeries and the prevalence of degenerative changes at the elbow.
Recurrent instability is not uncommon following repair or reconstruction and has been reported in up to 25% of patients after medium- to longer-term follow-up.
Cite this article: EFORT Open Rev 2016;1:461-468. DOI: 10.1302/2058-5241.160033
Keywords: elbow reconstruction, instability, PLRI, ligament
Introduction
Posterolateral rotatory instability (PLRI) was first described by O’Driscoll et al,1 and while it is relatively uncommon, it is the most common form of chronic elbow instability. The lateral collateral ligament (LCL) complex is the main component for lateral-sided stability and comprises the radial collateral ligament (RCL), the lateral ulnar collateral ligament (LUCL), the annular ligament and the accessory LCL.2 Other stabilisers include osseous structures, such as the radial head and coronoid process,3 and dynamic muscular constraints such as wrist and finger extensors.4 Any and all of these stabilisers can be involved in chronic PLRI. It is important to note, however, that the proximal radioulnar articulation is not involved since it moves as a unit.1 Chronic instability typically occurs from a traumatic event that commonly involves an elbow dislocation that remains unstable as the lateral collateral ligament complex fails to heal.5 While some patients have a history of elbow dislocation(s), others may have a documented injury involving the lateral side of the elbow, multiple cortisone injections, cubitus varus or even a history of lateral-sided surgery, e.g. debridement of lateral epicondylitis with iatrogenic damage to the LCL.1,5-7
PLRI usually occurs from a fall on the outstretched hand. On impact, the radial head and ulna rotate externally together with valgus displacement of the forearm. This leads to posterior displacement of the radial head relative to the capitellum, thus causing disruption of some or all of the lateral-sided stabilisers.8
Patients complain of lateral-sided elbow pain and mechanical symptoms such as clicking or instability. Treatment options range from LCL imbrication and repair to reconstruction with allograft or autograft.8
Anatomy
The elbow comprises the radius, ulna and humerus. These three bones articulate to form three joints: the radiohumeral, ulnohumeral and proximal radioulnar joints. The articulation and its surrounding soft tissues, including capsule, ligaments and muscles, determine the stability of the elbow and are position-dependent.8 The LCL complex includes the RCL, the LUCL, the annular ligament and the accessory lateral collateral ligament. The RCL and LUCL share their origin on the lateral epicondyle and are not individually identifiable at this level.4 The LUCL arches over the annular ligament and inserts on the tubercle of the supinator crest. The insertion has been described as bi-lobed.9
The LUCL resists external rotation stresses to the elbow but sectioning of the LUCL alone does not produce PLRI.1 For PLRI to occur, both the RCL and LUCL need to be disrupted.2,10,11 The annular ligament may or may not be intact.12 In addition, fracture of bony stabilisers such as the radial head or coronoid process can increase the degree of PLRI.3
Wrist and finger extensors, originating on the lateral epicondyle of the humerus, are dynamic stabilisers of the lateral elbow. Contraction of these muscles has been shown to decrease laxity in LCL-deficient elbows.4,13 Other studies have confirmed that the musculature is directly involved in elbow stability, and sectioning the muscles decreases stability.10
Physical examination
Chronic PLRI is a clinical diagnosis that includes a history of instability, clicking and lateral-sided pain with a positive clinical examination. Mechanical symptoms, such as clicking, along with tenderness on lateral-sided palpation, may be present. Varus laxity, while sometimes subtle, can be present with disrupted lateral-sided structures. The pivot-shift test is performed on a supine patient, the forearm is hypersupinated and a valgus stress along with axial load are applied to the elbow while moving from extension to flexion. The pivot-shift test on a conscious patient is considered positive with apprehension. Under general anaesthesia, the pivot-shift test is considered positive with subluxation or dislocation of the elbow which generally happens between 30° and 45° of flexion (Fig. 1a) and then reduces with further flexion (Fig. 1b).4 This test is highly specific but has low sensitivity in the awake patient.4 The posterolateral rotatory drawer test is considered positive when the radial head can be appreciated to translate posterior in relationship to the humerus with external pressure on the radial head.
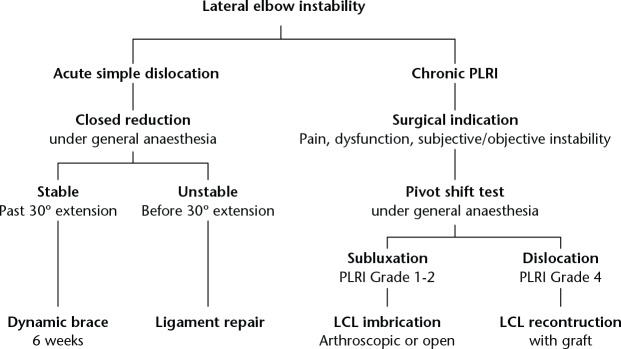
Fig. 1.
a) A positive pivot-shift test results in a (sub)luxation of the forearm relative to the humerus. Posterior translation of the radius can be seen as a dimple in the skin. This usually occurs with the elbow at around 30° of flexion. b) With further flexion, the forearm will reduce and the elbow will regain its normal contour (Courtesy of MoRe Foundation).
The push-up, chair and tabletop tests are more active tests that use patient participation. Patients, if able, may perform push-ups with the forearm in supination; this stresses the unstable lateral side, causing an inability to fully extend the arm along with pain when positive.14 The tabletop test requires patient participation with the patient’s hand supporting their weight on the table while flexing the elbow and keeping the forearm in supination. A positive tabletop test includes pain and apprehension at around 40° of elbow flexion. A positive tabletop re-location test is when the same test is repeated except with the examiner supporting the radial head and the pain and apprehension are alleviated.14
Imaging
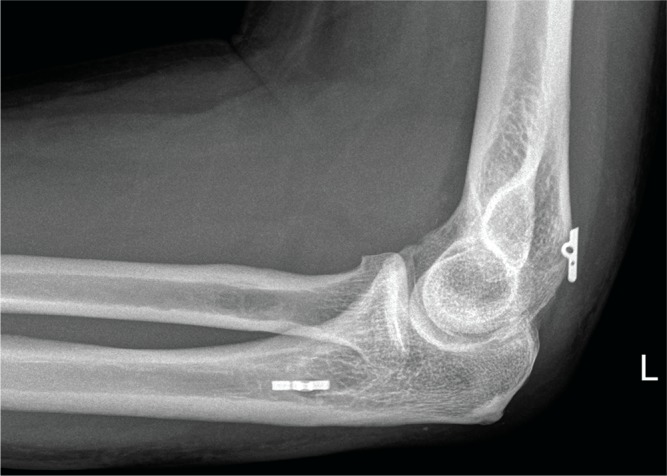
As previously noted, PLRI is a clinical diagnosis. However, further imaging may be helpful to confirm the diagnosis. Radiographs and CT scans may show indirect signs of ligamentous injury such as calcification of the lateral ligament, subluxation of the joint or fracture of the capitellum, coronoid or radial head (Fig. 2). An impaction defect in the posterolateral capitellum (‘Hill-Sachs’ lesion of the elbow) (Fig. 3) may also be identified. MRI will identify a ruptured LCL, scar tissue (Fig. 4), and cartilage damage that can negatively impact outcome, along with common extensor avulsion injury. The MRI can often help guide diagnosis but more commonly assists in surgical planning.
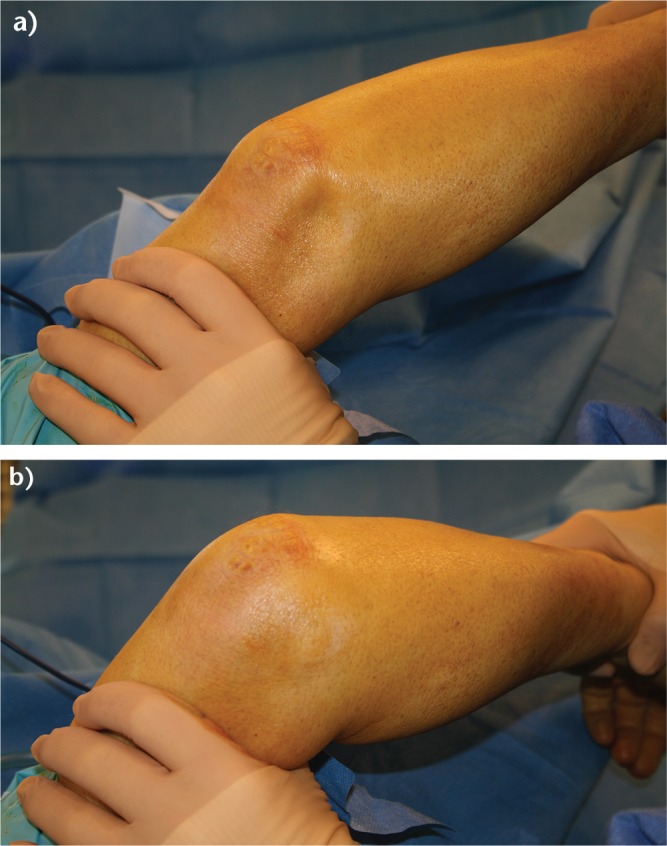
Fig. 2.
a) Lateral radiographic view, showing a subluxation of the elbow, indicating a posterolateral rotatory instability mechanism. b) Anteroposterior view of the elbow of a patient with chronic posterolateral rotatory instability. The calcification in the lateral collateral ligament (LCL) complex indicates failed healing of an LCL avulsion (Courtesy of MoRe Foundation).
Fig. 3.

CT image of an elbow showing a non-displaced radial head fracture and a concomitant fracture of the posterior aspect of the capitellum. This is the elbow’s equivalent to a ‘Hill-Sachs’ lesion of the humeral head (Courtesy of MoRe Foundation).
Fig. 4.

MRI showing a complete, chronic insufficiency of the stabilising structures of the lateral elbow (Courtesy of MoRe Foundation).
Surgical management
Non-operative management of PLRI is ineffective. Bracing, dynamic stabiliser strengthening and activity modification can be attempted. However, in general, surgical treatment is required to stabilise the joint.
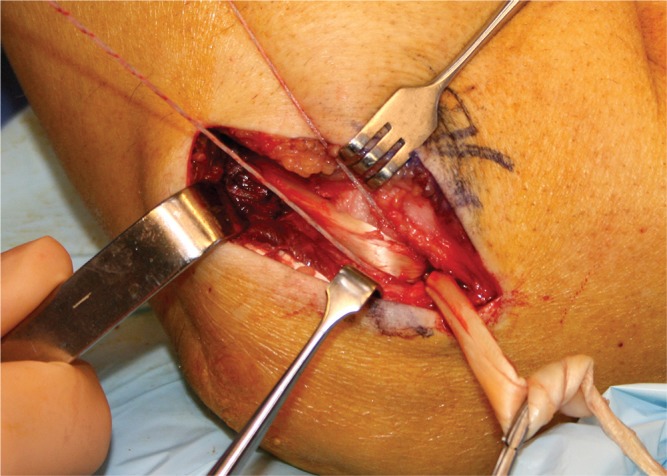
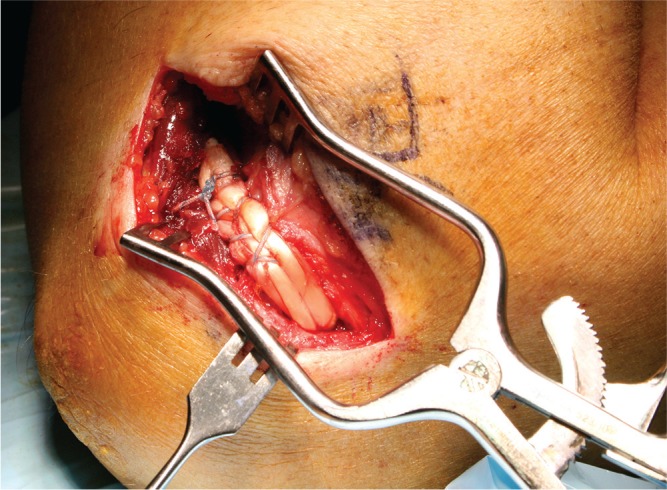
Surgery is indicated in patients with persistent, symptomatic instability of the elbow causing pain or functional deficit. There are several surgical techniques to treat PLRI, often leading to good or excellent results.9 Based on the available literature and our personal experience, we have developed an algorithm (Fig. 5). Primary repair of the chronically ruptured LCL complex depends on the integrity and quality of the remaining tissue. It is typically performed with the patient in a supine position and the arm on an armtable. Both loco-regional anaesthesia and general anaesthesia can be used, depending on the patient’s preference. A small (3 cm to 4 cm) lateral incision is made. The extensor tendon insertion may be avulsed together with the LCL complex. An extensor tendon split is used to gain access to the joint if the common extensor is intact (Fig. 6). Any haemarthrosis is evacuated and the joint is rinsed with saline. Capitellar and radial head cartilage are inspected and any flaps may be debrided or stabilised. The LCL is re-inserted into the lateral condyle (Fig. 7). We prefer to use a small bone anchor but bone tunnels may also be used. The extensor tendon split is closed strongly as this fortifies the LCL repair. Savoie et al have described an arthroscopic technique for the acute repair of a ruptured LCL complex.15
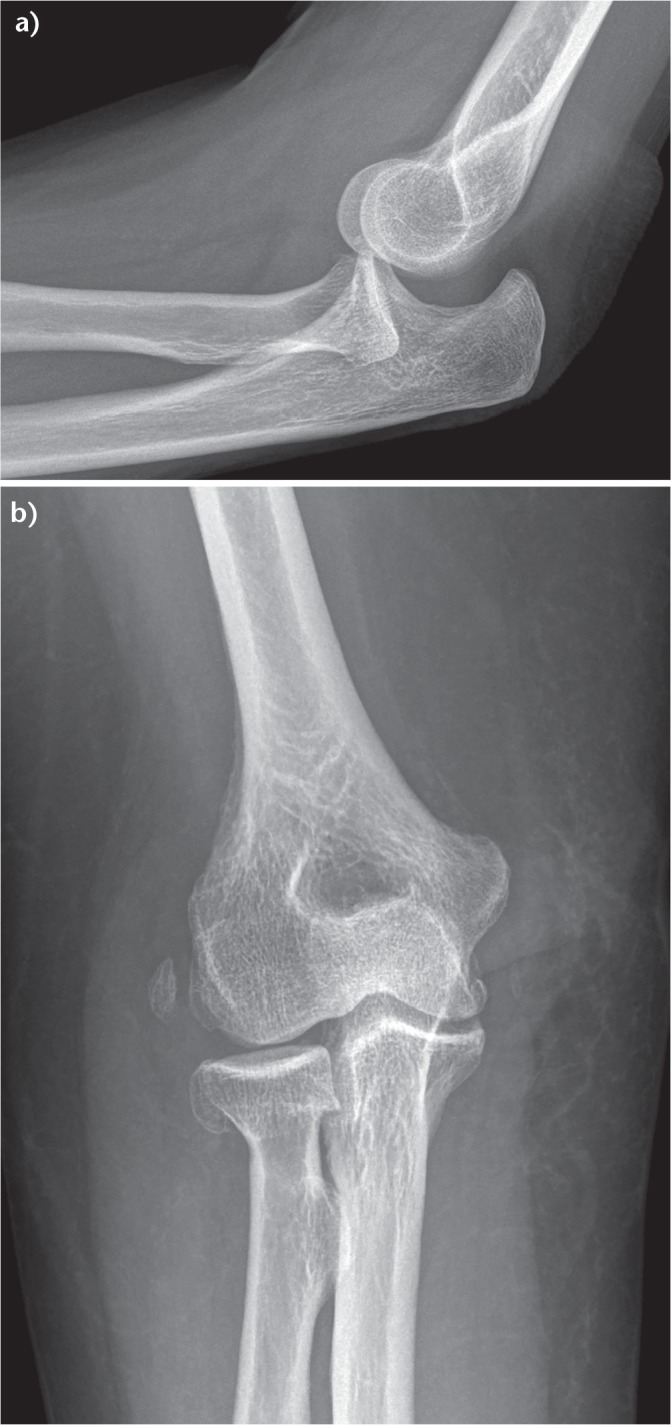
Fig. 5.
Algorithm for the treatment of patients with lateral-sided elbow instability (Courtesy of MoRe Foundation).
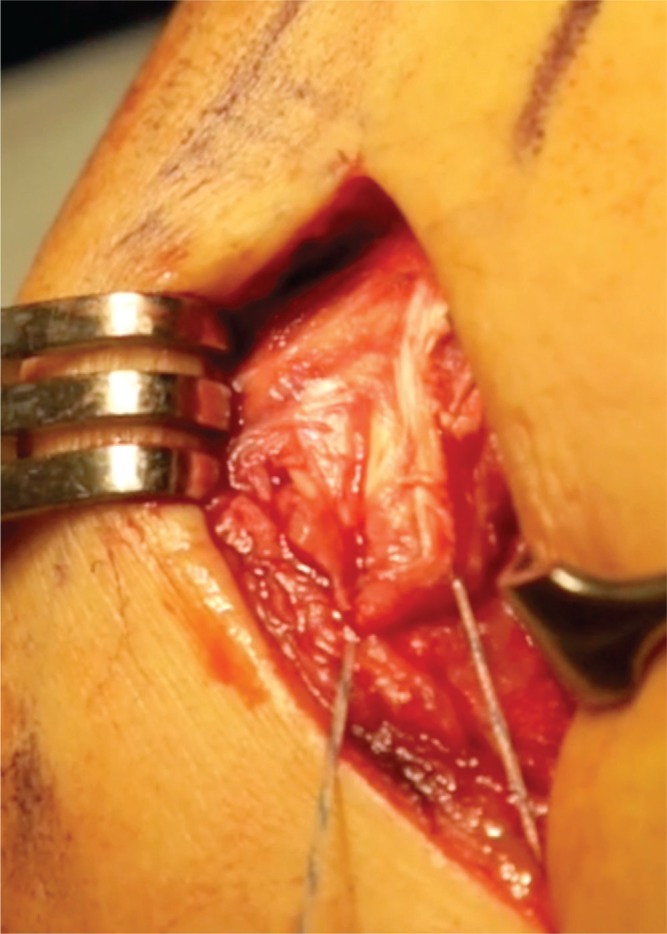
Fig. 6.
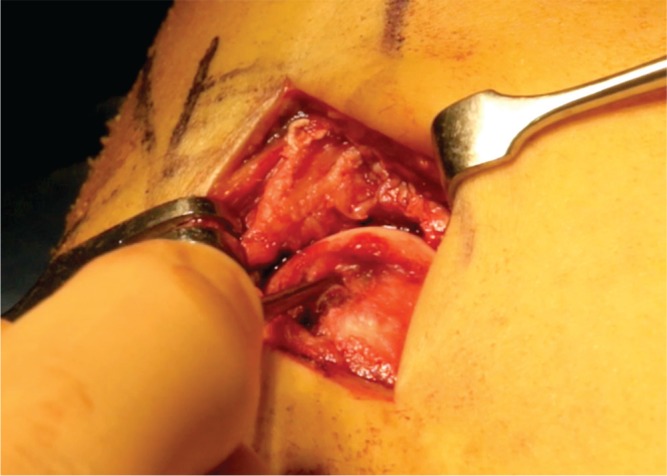
Lateral intra-operative view showing a complete avulsion of the lateral collateral ligament (LCL) complex. The LCL stump is held by the forceps (Courtesy of MoRe Foundation).
Fig. 7.
The lateral collateral ligament complex is re-inserted with the use of a bone anchor (Courtesy of MoRe Foundation).
Open and arthroscopic techniques are both options in chronically unstable elbows. An arthroscopic technique was first described by Savoie et al15 and was adapted by the senior author (RvR). The technique we use consists of imbrication of the LCL utilising a #2 PDS suture intra-articular from the lateral epicondyle to the supinator crest (Fig. 8). The suture is then doubled (Fig. 9) and the tails are passed subcutaneously back to the soft spot portal and tied, creating a double-sutured repair, imbricating the LCL complex, lateral capsule and the anconeus in one layer. Pre- and peri-operative screening of patients is essential if an arthroscopic technique is contemplated. No comparative data are available on when to imbricate the LCL, when to repair or when to reconstruct. There is some weak evidence suggesting that reconstruction may be better than repair in a large group of patients with mixed pathology.16
Fig. 8.
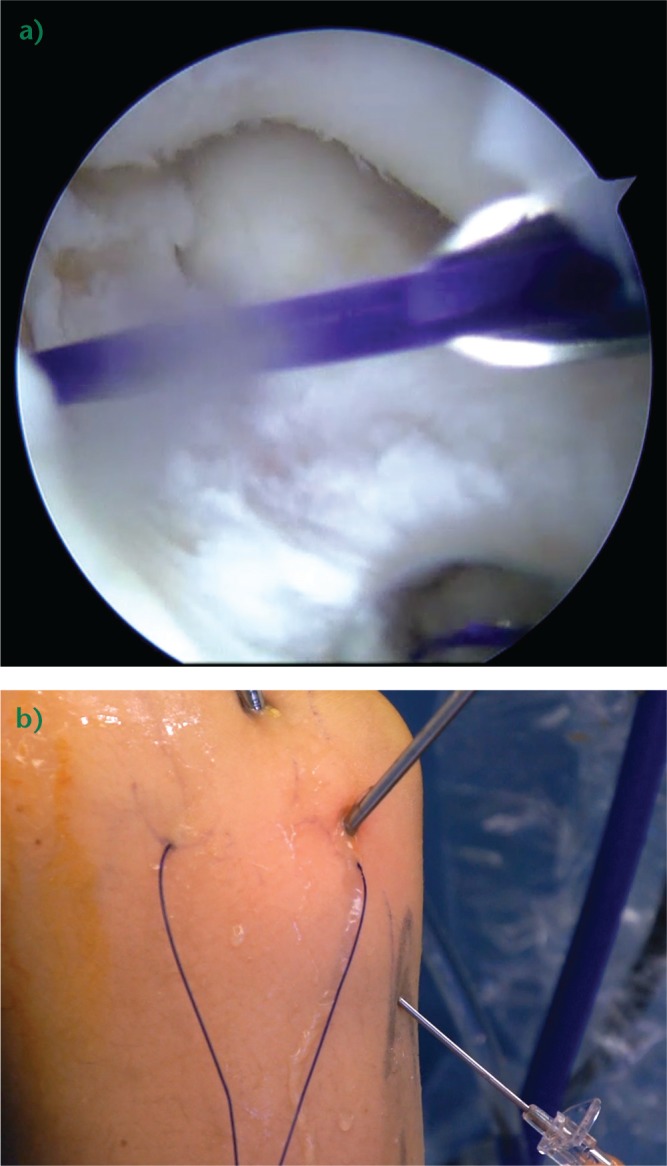
a) Arthroscopic view. A needle is used to shuttle a PDS suture from the insertion of the lateral ulnar collateral ligament (LUCL) on the lateral epicondyle (Courtesy of MoRe Foundation). b) A second suture is shuttled into the joint from the origin of the LUCL on the ulna (Courtesy of MoRe Foundation).
Fig. 9.
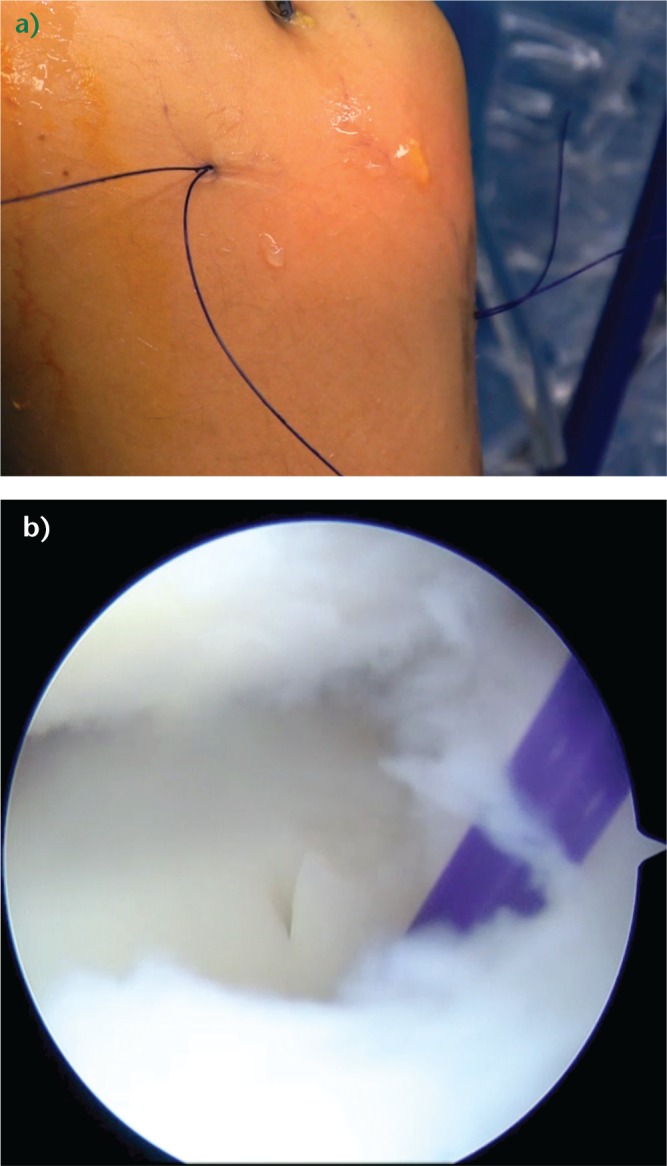
a) External and b) intra-articular view of the double PDS suture used to imbricate the lateral collateral ligament complex (Courtesy of MoRe Foundation).
Thus far, our arthroscopic technique has been successfully used in patients with symptomatic PLRI following one or more episodes of dislocation or subluxation. At the pre-operative examination under general anaesthesia, all patients had a positive pivot-shift test but not a frank dislocation. We prefer to perform a LCL reconstruction with an allograft tendon.
There are a variety of surgical techniques available for LUCL reconstruction. Distal graft fixation options include a two-tunnel technique, a single-tunnel technique fixed with an interference screw or cortical button, or suture anchors. Proximal fixation has utilised three tunnels or a single-tunnel docking technique. A variety of graft choices are available including allograft or autograft and a variety of tendons including palmaris longus, plantaris, Achilles, triceps, semitendinosus or gracilis. All are of sufficient strength to reconstruct the LCL complex.17 The open technique of lateral ligament reconstruction uses an incision centred over the lateral epicondyle using Kocher’s interval between the anconeus and the extensor carpi ulnaris (ECU) (Fig. 10). The supinator crest on the ulna is palpated and followed proximally. A small tubercle can often be palpated on the most proximal part of the crest just distal to the radial head and is the insertion of the LUCL. The common extensor tendon is released from posterior to anterior. The senior author (RvR) prefers allograft extensor hallucis longus. A cortical bone button fixation device on both the ulna (4.5 mm intramedullary) and the humerus (6.0 mm, posterior cortex 4.5 mm) (Fig. 11) is used. The native capsule is closed deep to the reconstruction to avoid friction between the graft and the lateral elbow joint (Fig. 11). The graft is tightly fixed on the ulna and both limbs are pulled through the loop of the second cortical device in the humerus. The forearm is held in pronation and the graft is tightened (Fig. 12). The graft is then doubled on itself and sutured. Although the LCL is isometric, the LUCL has been shown to be lax in extension and tighten in flexion, therefore the graft is tensioned in approximately 30° of flexion (Fig. 13), allowing the reconstruction to tighten further when the elbow is flexed (Fig. 14).18
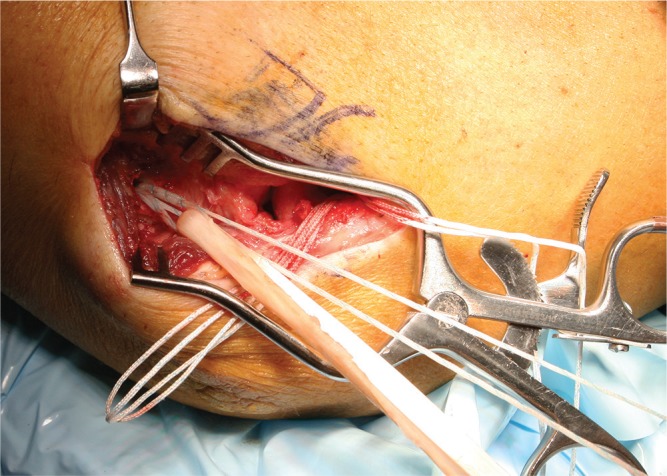
Fig. 10.

Lateral intra-operative view of the elbow. The skin incision is made posterior to the lateral ulnar collateral ligament. Kocher’s interval is developed between the anconeus and extensor carpi ulnaris muscles (Courtesy of MoRe Foundation).
Fig. 11.
The graft is placed through the loop of the ulnar cortical device. A second cortical button was placed in the humerus (Courtesy of MoRe Foundation).
Fig. 12.
Post-operative lateral radiograph showing correct positioning of both cortical buttons (Courtesy of MoRe Foundation).
Fig. 13.
The graft is tensioned and pulled into the humeral canal (Courtesy of MoRe Foundation).
Fig. 14.
The lateral ulnar collateral ligament is strongly reconstructed once all graft limbs are sutured (Courtesy of MoRe Foundation).
Results
Outcomes after acute repair are good to excellent in the majority of patients.11,16
Results of acute repair are generally better compared with reconstruction. This is due to the fact that predictive factors for a poor outcome include the number of previous surgeries and the prevalence of degenerative changes at the elbow.15,16
Results of arthroscopic repair or reconstruction are sparse but seem to be promising with good to excellent results in most reports, without an increase in complications relating to the surgery.15
Overall, results after reconstruction for PLRI are good to excellent in about 85% of patients. Several authors have reported results after reconstruction with a majority of patients remaining stable with worse outcomes in patients who have degenerative arthritis, pain only without symptoms of instability, and prior surgery.6,19
Jones et al reported on eight patients at a mean of seven years post-operatively after LUCL reconstruction using a palmaris longus autograft utilising a two-distal ulnar tunnel and a proximal docking technique.19 The authors reported complete resolution of instability in six patients and recurrence in two of eight patients (25%). Despite recurrence, all patients were reported to be satisfied at final follow-up. Nestor et al evaluated 11 patients (three repairs and eight reconstructions) who underwent surgery for PLRI.20 The reconstructions were performed using a five-tunnel technique (three in the humerus and two in the ulna) and a palmaris longus autograft. They noted three patients with fair outcomes and one with a poor outcome, according to their classification. The patients who underwent repair had good results, however, they had less severe disease than the patients who underwent reconstruction. Prior surgery and the presence of radiocapitellar arthritis were noted to be risk factors for poor outcomes. They suggest that all patients are counselled regarding these risks and that the quality of the joint is assessed pre-operatively and during surgery. Sanchez-Sotelo et al reported their outcomes in 45 patients (12 repairs and 33 reconstructions) who underwent surgery for PLRI. Five patients (11%) noted further instability and 27% of patients described fair or poor results.16 Better results were noted in patients with a post-traumatic aetiology or subjective instability, and in those patients where a graft was utilised. Most recently, Baghdadi et al reported on 11 patients who had a revision LUCL reconstruction for a failed prior reconstruction utilising an allograft tendon.21 The revision reconstructions were performed at a mean of three years after the initial LUCL reconstruction. Osseous deficiency was identified at some level in eight of 11 patients. At an average of five years post-revision reconstruction, eight of 11 elbows remained stable. All patients that remained stable had a good or excellent result whereas all patients that had persistent instability were noted to have some degree of bone loss. The authors concluded that revision LUCL reconstruction is an option for persistent instability although it must be recognised that almost half of patients either had persistent instability after revision or a fair or poor outcome.
Complications
Recurrent instability is not uncommon following repair or reconstruction and has been published in up to 25% of patients after medium- to longer-term follow-up.19
In our experience a common complication after arthroscopic repair is self-limiting lateral elbow pain due to a prominent suture knot. If this is not resolved spontaneously, the knot can be removed. We are not aware of any papers reporting bone tunnel breakage after lateral or medial ligament reconstruction, however, we have personally experienced one patient with a fracture of the distal humerus one year after the reconstruction, seemingly initiated through the bone tunnel.
Conclusion
Chronic PLRI is a relatively uncommon problem that can involve both soft-tissue and osseous structures. Conservative treatment is often disappointing. Surgical repair or reconstruction of the LCL generally leads to good to excellent outcomes but recurrence can be seen in up to 25% of patients. Degenerative changes and the number of prior surgeries are predictors for less favourable outcome.
Footnotes
Conflict of Interest: None declared.
Funding
The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article. In addition, benefits have been or will be directed to a research fund, foundation, educational institution, or other non-profit organisation with which one or more of the authors are associated.
References
- 1. O’Driscoll SW, Bell DF, Morrey BF. Posterolateral rotatory instability of the elbow. J Bone Joint Surg [Am] 1991;73-A:440-446. [PubMed] [Google Scholar]
- 2. Dunning CE, Zarzour ZD, Patterson SD, Johnson JA, King GJ. Ligamentous stabilizers against posterolateral rotatory instability of the elbow. J Bone Joint Surg [Am] 2001;83-A:1823-1828. [DOI] [PubMed] [Google Scholar]
- 3. Schneeberger AG, Sadowski MM, Jacob HA. Coronoid process and radial head as posterolateral rotatory stabilizers of the elbow. J Bone Joint Surg [Am] 2004;86-A:975-982. [DOI] [PubMed] [Google Scholar]
- 4. Dunning CE, Zarzour ZD, Patterson SD, Johnson JA, King GJ. Muscle forces and pronation stabilize the lateral ligament deficient elbow. Clin Orthop Relat Res 2001;388:118-124. [DOI] [PubMed] [Google Scholar]
- 5. Steinmann SP. Elbow instability. Curr Orthop 2002;16:341-348. [Google Scholar]
- 6. O’Driscoll SW, Spinner RJ, McKee MD, et al. Tardy posterolateral rotatory instability of the elbow due to cubitus varus. J Bone Joint Surg [Am] 2001;83-A:1358-1369. [DOI] [PubMed] [Google Scholar]
- 7. Kalainov DM, Cohen MS. Posterolateral rotatory instability of the elbow in association with lateral epicondylitis. A report of three cases. J Bone Joint Surg [Am] 2005;87-A:1120-1125. [DOI] [PubMed] [Google Scholar]
- 8. Mehta JA, Bain GI. Posterolateral rotatory instability of the elbow. J Am Acad Orthop Surg 2004;12:405-415. [DOI] [PubMed] [Google Scholar]
- 9. Cohen MS, Hastings H., II Rotatory instability of the elbow. The anatomy and role of the lateral stabilizers. J Bone Joint Surg [Am] 1997;79-A:225-233. [PubMed] [Google Scholar]
- 10. McAdams TR, Masters GW, Srivastava S. The effect of arthroscopic sectioning of the lateral ligament complex of the elbow on posterolateral rotatory stability. J Shoulder Elbow Surg 2005;14:298-301. [DOI] [PubMed] [Google Scholar]
- 11. Olsen BS, Søjbjerg JO, Nielsen KK, et al. Posterolateral elbow joint instability: the basic kinematics. J Shoulder Elbow Surg 1998;7:19-29. [DOI] [PubMed] [Google Scholar]
- 12. King GJ, Dunning CE, Zarzour ZD, Patterson SD, Johnson JA. Single-strand reconstruction of the lateral ulnar collateral ligament restores varus and posterolateral rotatory stability of the elbow. J Shoulder Elbow Surgery 2002;11:60-64. [DOI] [PubMed] [Google Scholar]
- 13. O’Driscoll SW. Classification and evaluation of recurrent instability of the elbow. Clin Orthop Relat Res 2000;370:34-43. [DOI] [PubMed] [Google Scholar]
- 14. Regan W, Lapner PC. Prospective evaluation of two diagnostic apprehension signs for posterolateral instability of the elbow. J Shoulder Elbow Surg 2006;15:344-346. [DOI] [PubMed] [Google Scholar]
- 15. Savoie FH, III, O’Brien MJ, Field LD, Gurley DJ. Arthroscopic and open radial ulnohumeral ligament reconstruction for posterolateral rotatory instability of the elbow. Clin Sports Med 2010;29:611-618. [DOI] [PubMed] [Google Scholar]
- 16. Sanchez-Sotelo J, Morrey BF, O’Driscoll SW. Ligamentous repair and reconstruction for posterolateral rotatory instability of the elbow. J Bone Joint Surg [Br] 2005;87-B:54-61. [PubMed] [Google Scholar]
- 17. Baumfeld JA, van Riet RP, Zobitz ME, et al. Triceps tendon properties and its potential as an autograft. J Shoulder Elbow Surg 2010;19:697-699. [DOI] [PubMed] [Google Scholar]
- 18. Moritomo H, Murase T, Arimitsu S, et al. The in vivo isometric point of the lateral ligament of the elbow. J Bone Joint Surg [Am] 2007;89-A:2011-2017. [DOI] [PubMed] [Google Scholar]
- 19. Jones KJ, Dodson CC, Osbahr DC, et al. The docking technique for lateral ulnar collateral ligament reconstruction: surgical technique and clinical outcomes. J Shoulder Elbow Surgery 2012;21:389-395. [DOI] [PubMed] [Google Scholar]
- 20. Nestor BJ, O’Driscoll SW, Morrey BF. Ligamentous reconstruction for posterolateral rotatory instability of the elbow. J Bone Joint Surg [Am] 1992;74-A:1235-1241. [PubMed] [Google Scholar]
- 21. Baghdadi YM, Morrey BF, O’Driscoll SW, Steinmann SP, Sanchez-Sotelo J. Revision allograft reconstruction of the lateral collateral ligament complex in elbows with previous failed reconstruction and persistent posterolateral rotatory instability. Clin Orthop Relat Res 2014;472:2061-2067. [DOI] [PMC free article] [PubMed] [Google Scholar]