Abstract
Recent studies have challenged the long-held notion that neutral mechanical alignment after total knee arthroplasty leads to optimal function and survivorship.
The ideal alignment for function and survivorship may actually be different.
Kinematic alignment, where components are implanted to re-create the natural flexion/extension axis of the knee, may lead to improved functional results.
Residual varus alignment may not adversely impact survivorship provided the tibial component is implanted in neutral alignment.
Cite this article: Lording T, Lustig S, Neyret P. Coronal alignment after total knee arthroplasty. EFORT Open Rev 2016;1:12-17. doi: 10.1302/2058-5241.1.000002.
Keywords: knee, total arthroplasty, coronal alignment, mechanical alignment, kinematic alignment, functional results, survivorship
A long-held principle in total knee arthroplasty (TKA) is that long-term survival and optimal function are dependent on achieving a post-operative leg alignment within 3° of the neutral mechanical axis. To this end, computer navigation and now patient-specific instrumentation have been developed, to improve accuracy in implantation and maximise the number of arthroplasties falling within these limits. At the neuvièmes Journées Lyonnaises de Chirugie du Genou in 1999, Rivat and Neyret presented a view that residual varus of femoral origin was acceptable, but neutral mechanical alignment of the tibial component was mandatory.1 More recently, a number of authors have challenged this principle, suggesting “malalignment” of the mechanical axis may have little effect on the outcome of knee arthroplasty performed with modern prostheses.
The aim of this review is to assess the historical and contemporary evidence regarding the impact of coronal plane alignment in TKA on function and survivorship.
Anatomy and deformity
To describe the anatomy and coronal alignment of the leg, a number of descriptive terms are used.2 The anatomical axis of each bone refers to a line drawn along the centre of the intramedullary canal. The mechanical axis of the femur refers to a line drawn from the centre of the femoral head to the centre of the knee. For the tibia, the mechanical axis refers to a line between the centre of the knee and the centre of the ankle. The anatomical and mechanical axes of the femur form an angle of approximately 6°, while the two axes of the tibia are usually equivalent (Fig. 1).
Fig. 1.
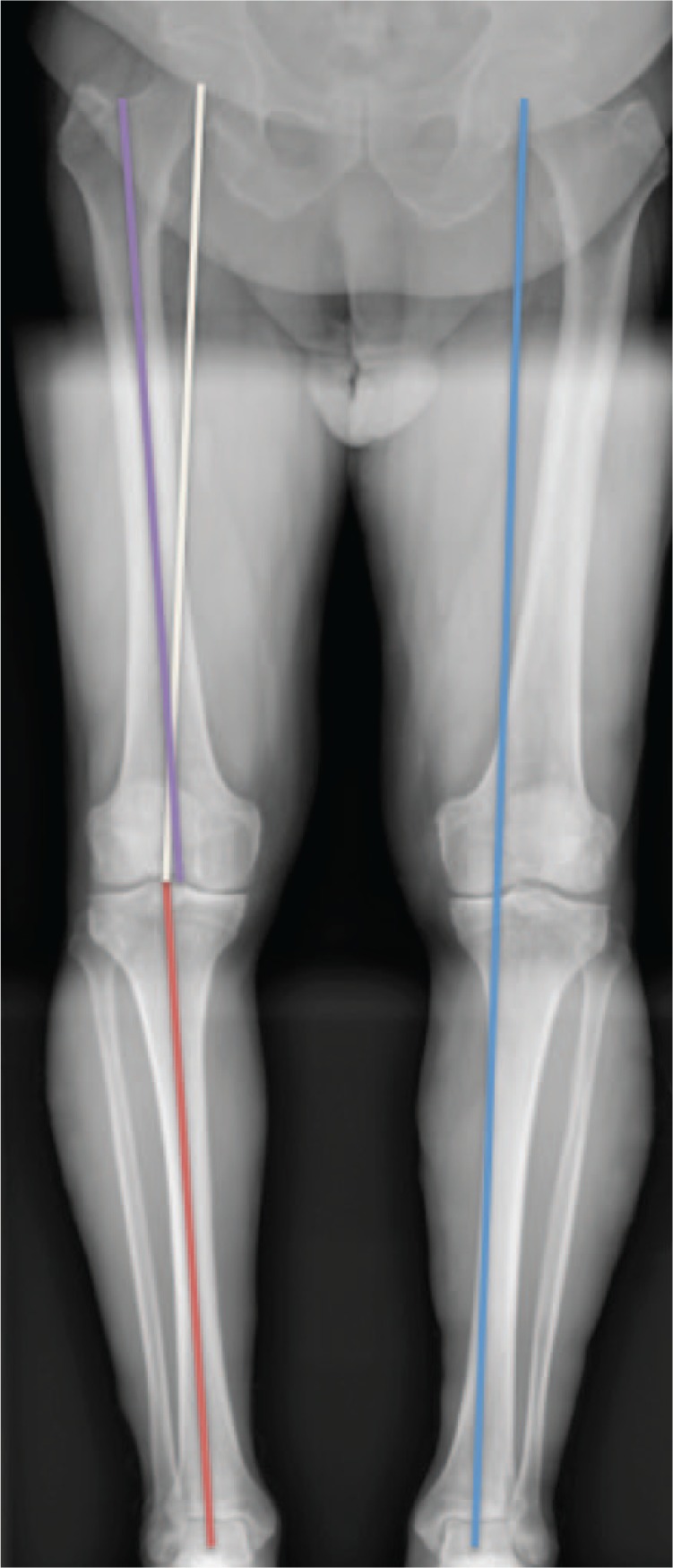
Long-leg radiograph. Right leg demonstrates mechanical axis (white line) and anatomical axis (purple line) of the femur. The anatomical and mechanical axes of the tibia are usually the same (red line). On the left leg, Maquet’s line passes through the medial compartment of the knee, indicating varus alignment.
The global mechanical axis, sometimes referred to as Maquet’s line, describes a line drawn from the centre of the femoral head to the centre of the talus3 (Fig. 1). Normally, this line passes through the centre of the knee. The anatomical femorotibial angle (aFTA) describes the angle between the anatomical axes of the femur and tibia, and is usually about 6° of valgus. The mechanical femorotibial angle (mFTA), formed by the mechanical axes of the two bones, is usually 0° or neutral, although variation exists in nature. This is sometimes referred to as the hip-knee-ankle angle (HKA).
Care must be taken when performing standardised radiographs for determination of coronal plane alignment. Variance in limb rotation and knee flexion may have significant impact on the observed angles.4,5 In a valgus knee model with a true aFTA of 18°, Swanson measured a change of almost 7° in the apparent aFTA with 20° of internal and external rotation.3 Hence, radiographs are generally taken with the patient standing and the feet together.
Deformity affecting leg alignment may occur at any level. In general, the closer an extra-articular deformity to the knee, the greater is its importance.6
Historical evidence supporting neutral alignment
In 1977, Lotke and Ecker first examined the correlation between implant positioning and functional outcome in 70 TKAs.7 Alignment and functional outcome were both evaluated using the author’s own 100-point scales. Long-leg films were not used and component rotation was not assessed. They noted a significant correlation between good clinical results and good alignment. In four of their five failures, the tibial component was positioned in varus. Denham and Bishop, in a 1978 study of biomechanics in relation to knee reconstruction, defined optimal positioning to be 7° ± 4° of anatomical valgus for the femoral component and 90° ± 4° to the anatomical axis for the tibia, to ensure the weight-bearing line passed through the centre of the joint.8 Hvid and Nielsen reported an increased incidence of radiolucent lines at two years surrounding tibial components implanted with > 4° tilt in any direction, with the interesting exception of varus angulation in osteoarthritic knees.9
In an important 1991 study, Jeffrey et al published the results of 115 early Denham knee arthroplasties, with a median follow-up of eight years.10 Using long-leg radiographs to assess coronal plane alignment, they found a significant difference in the rate of loosening between those aligned within ± 3° of the mechanical axis Maquet’s line (3% loosening), and those outside these limits (27% loosening; p = 0.001). This target range has subsequently been supported by numerous clinical and laboratory studies.11-18 These studies are summarised in Table I.
Table I.
Summary of early studies supporting neutral mechanical alignment
| Author | Year | Number | Prosthesis | Follow-up (yrs) | Outcome measures | Findings | Comments |
|---|---|---|---|---|---|---|---|
| Lotke7 | 1977 | 70 | Geometric | 1 to 3 | Own 100-point scales for clinical and radiographic outcomes | Significant correlation between clinical and radiographic scores | 4/5 failures had tibial component in varus |
| Hvid9 | 1984 | 138 | Insall/Berstein | 2 | Radiographic alignment, radiolucency, Insall score | Increased radiolucencies with global varus alignment, not significant for OA/Increased radiolucencies with any tibial tilt >4° | 3/3 failures had tibial component in varus |
| Jeffery10 | 1991 | 115 | Denham | 8 to 12 | Radiographic alignment, BASK score | 3% loosening when Maquet’s line within middle 1/3 of knee/24% loosening when Maquet’s line outside middle 1/3 | Study used long-leg radiographs |
Interestingly, not all studies from this period supported a neutral mechanical axis. Bargren et al reported a failure rate of 2.3% for the Freeman Swanson (ICLH) knee when aligned between 1° to 5° of anatomical valgus (1° to 5° varus mechanical alignment), against an overall failure rate of 27%.19
Recent evidence challenging neutral alignment
In the last few years, several reports have been highlighted challenging the superiority of neutral mechanical alignment. These studies are summarised in Table II.
Table II.
Summary of studies challenging the aim of neutral alignment
| Author | Year | Number | Prosthesis | Follow-up (yrs) | Outcome measures | Findings | Comments |
|---|---|---|---|---|---|---|---|
| Morgan20 | 2007 | 197 | Kinemax | 9 | Radiographic alignment, revision or intention to revise | No difference in revision rate for neutral (4° to 9° anatomical valgus), varus or valgus alignment | Retrospective study |
| Parratte21 | 2010 | 398 | Kinematic Condylar II | 15 | Radiographic alignment, Kaplan-Meier survival analysis | No difference in revision rate for mechanical axis 0° ± 3° compared with outliers | Retrospective study |
| PFC | |||||||
| Genesis | |||||||
| Bonner22 | 2011 | 501 | PFC | 15 (min 9) | Radiographic alignment, Kaplan-Meier survival analysis | Weak trend towards improved survivorship in aligned group (mechanical axis 0° ± 3°) (p = 0.47) | Retrospective study |
| Matziolis23 | 2010 | 218 | PFC Sigma | 5 to 10 | Radiographic alignment, KSS, WOMAC, SF-36 | No difference in revision rate or any outcome measure | Case control study comparing 30 most varus TKA to neutrally aligned, matched controls |
| Natural Knee II | |||||||
| Magnussen24 | 2011 | 553 | HLS I | 2 to 19 | Radiographic alignment, revision rate, KSS | No difference in revision rate or IKS for neutral or residual varus > 3°/Lower IKS scores with tibial component varus | Compared patients with pre-operative varus alignment based on neutral or varus post-operative alignment |
| HLS II | |||||||
| HLS Evolution | |||||||
| Noetos HLS | |||||||
| Vanlommel25 | 2013 | 143 | Profix | 7.2 | Radiographic alignment, KSS, WOMAC | Total KSS and function subscore, total WOMAC, stiffness and ADL subscores better in mild varus group (3-6° mechanical varus) compared to neutral and >6° varus groups | Compared patients with pre-operative varus alignment based on degree of post-operative varus |
Notes: KSS, Knee Society Score; WOMAC, Western Ontario and McMaster University Osteoarthritis Index; IKS, International Knee Society Score; SF-36, Short Form-36; ADL, activities of daily living.
Regarding survival, in 2007 Morgan et al reviewed the outcomes of 197 Kinemax™ TKAs at a mean of nine years post-operatively, and found no difference in revision rate between those in neutral, varus or valgus alignment.20 In a larger study, Parratte et al published a retrospective review of 398 cemented primary knee arthroplasties performed at the Mayo Clinic using three modern prostheses.21 Long-leg radiographs were performed for all patients pre- and post-operatively. The outlier group comprised 106 knees with post-operative mechanical alignment outside 0° ± 3°. They found no difference in survivorship at 15 years between the well-aligned and outlier groups, and concluded that describing alignment as a dichotomous variable was of little value for predicting durability. In a similar study of 501 TKAs using a single prosthesis, Bonner22 and co-workers found a weak trend towards a higher revision rate in those outside the 0° ± 3° range; however, this fell short of statistical significance (p = 0.47). They concluded that the relationship between mechanical alignment and survival for primary TKA is weaker than previously reported.
With regards to function, two medium-term studies have suggested that functional outcome is not adversely affected by residual post-operative varus alignment. From a series of 218 primary TKAs, Matziolis and colleagues compared the results of the 30 knees with the greatest post-operative varus alignment, to neutrally aligned, matched controls.23 The varus group had a mean post-operative mechanical axis deviation of 6.3° (3.9° to 10.7°). There was no difference in functional results using multiple validated measures, and no revisions in either group at a minimum five-year follow-up. Magnussen and colleagues, from the Centre Albert Trillat in Lyon, examined the results of 553 TKAs for varus osteoarthritis, comparing those with neutral post-operative mechanical alignment (0° ± 3°) and those with residual varus alignment > 3° at a mean follow-up of 4.7 years.24 They found no difference in Knee Society Score (KSS) or revision rate between the two groups, provided the residual varus was femoral in origin. Tibial component varus and femoral component valgus were both associated with inferior KSS results.
One recent study has found superior functional results for TKAs with mild residual varus. In a study of 143 consecutive TKAs for varus osteoarthritis, Vanlommel et al observed that the 46 knees with residual varus of 4° to 7° (FTMA 174° to 177°) demonstrated significantly better KSS and Western Ontario and McMaster University Osteoarthritis Index (WOMAC) scores than the neutral and significant varus groups at a mean of 7.2 years.25
Discussion
A number of criticisms have been made of early studies showing decreased survivorship with non-alignment of the mechanical axis. Most used only short-leg radiographs for assessment7,9,19 and involved early prosthesis designs no longer in use today.10 Polyethylene quality was inferior, and the sterilisation methods employed are now known to cause material property degradation.18
The literature regarding the impact of coronal alignment on functional outcomes is unclear. Most data comes from studies into navigation in TKA, examining short- to medium-term results. Some authors have reported improved knee function with more ideal alignment.26-28 Others have found no improvement and even poorer functional results using navigation.29-32 A systematic review in 2012 concluded that there was improved coronal plane alignment but no functional improvement with navigation;33 however, a recent meta-analysis did find improved function in the navigation group.34
Recently, Bellemans and co-workers have introduced the concept of constitutional varus, suggesting a neutral mechanical axis may be abnormal and even undesirable for many patients.35 In their study, 32% of men and 17% of women had a natural mechanical alignment ≥ 3° of varus. Similarly, others have explored the cylindrical axis of the knee36 and the concept of kinematic alignment.37
Kinematic alignment is based on the finding that the true axis about which knee flexion and extension occur is not perpendicular to the mechanical axis,38 and places the femoral and tibial components accordingly to recreate this anatomical axis. Howell and co-workers reported equivalent or slightly better WOMAC and Oxford knee scores (OKS) for varus and valgus outlier groups in 198 kinematically-aligned TKAs, although this did not reach significance. A more recent study of 219 consecutive, kinematically-aligned TKAs from the same author reported a comparable revision rate to registry data for the same prosthesis at six years, regardless of tibial component varus or overall limb alignment.39 There were three revisions reported, including one for tibial component loosening, with two further revisions pending for patellar component loosening. Dossett et al, in a randomised control trial, evaluated the short-term outcomes of 41 kinematically- and 41 mechanically-aligned TKAs.40 While the overall limb alignment was similar, the kinematic alignment group had 2.3° more tibial component varus and 2.4° more femoral component valgus. KSS, WOMAC and OKS were superior in the kinematically-aligned group. While there were no catastrophic early failures in these studies, the long-term survival of kinematically-aligned TKAs is unknown. Ishikawa et al, in a recent computer simulator and finite element analysis, found near-normal knee kinematics in kinematically-aligned TKAs; however, both patellofemoral and tibiofemoral peak contact stresses were increased by as much as 200% and 270% respectively in the kinematically-aligned model.41 Furthermore, the accuracy of the patient-specific instrumentation systems typically required to achieve kinematic alignment are still being investigated42,43 and may be inferior to traditional or navigated systems.44
Tibial component varus
Contrary to these results, a number of authors have reported inferior results associated with tibial component varus.7,16,24,45,46 Berend and colleagues, in a study of a cohort of 3152 knees with a mean five-year follow-up, found tibial component varus > 3° to significantly increase the odds of failure (hazard ratio 17.2, p < 0.0001).16 In a later study from the same centre on an expanded cohort of 6070 TKAs, Ritter et al found increased revision rates when the tibial component was implanted in varus, when the femoral component was implanted with > 8° of anatomical valgus, and when one component was implanted to “correct” for malalignment of the other component, despite resulting in neutral global limb alignment.45 There was no difference in survivorship between those with neutral tibial component and neutral overall alignment and those with neutral tibial alignment and overall varus limb alignment (< 2.5°), suggesting some residual varus global alignment in itself does not compromise results.
Residual valgus alignment after TKA is associated with inferior results. Karachalios et al found residual deformity to be much more common in valgus knees and associated with significantly inferior clinical results using the Bristol Knee Score.47 Fang et al reported a revision rate of 1.5% for those with post-operative valgus alignment compared with 0.5% for those in neutral alignment, noting that those with residual valgus tended to fail from ligament instability.48 Koskinen, in a study of 48 valgus knees implanted with cruciate-retaining prostheses, found residual valgus deformity to significantly increase the risk of revision with an odds ratio of 2 (95% confidence interval 1 to 3, p = 0.025).49 Eight of the 14 revisions were for progressive medial collateral ligament (MCL) instability. Consistent with these clinical reports, Bryant and coworkers, in a recent cadaveric study, found valgus loading of a TKA to significantly increase lateral tibio-femoral contact pressures and MCL strain.50
Conclusion
As noted by Tew and Waugh in 1985, while coronal alignment is certainly a factor in the outcome of TKA, it may not be the most important factor and may serve to compound failure from other causes.51 Other technical factors, such as sagittal and rotational alignment, joint line restoration, and soft-tissue balance all influence the final outcome. Recent work on kinematic alignment would suggest that the ideal alignments for patient function and prosthesis longevity may in fact be different. If so, advances in materials technology may allow for implant survival in a more functional but non-optimal mechanical environment. While mild residual global varus deformity may not negatively impact outcomes, survivorship may be negatively affected by varus of the tibial component.
Footnotes
Conflict of Interest: None declared.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1. Rivat P, Neyret P, Ait Si Selmi T. Influence de l’ordre des coupes, coupes dépendantes et indépendantes, rôle du tenseur. In: Chambat P, Neyret P, Deschamps G, eds. 9èmes Journées Lyonnaises De Genou, Chirurgie Prothétique Du Genou. Sauramps; 1999:1–36. http://www.decitre.fr/livres/chirurgie-prothetique-du-genou-9782840232087.html (date last accessed 7 October 2015).
- 2. Chao EY, Neluheni EV, Hsu RW, Paley D. Biomechanics of malalignment. Orthop Clin North Am 1994;25:379–386. [PubMed] [Google Scholar]
- 3. Maquet P. Biomechanics of gonarthrosis. Acta Orthop Belg 1972;38(suppl 1):33–54. (In French). [PubMed] [Google Scholar]
- 4. Swanson KE, Stocks GW, Warren PD, Hazel MR, Janssen HF. Does axial limb rotation affect the alignment measurements in deformed limbs? Clin Orthop Relat Res 2000;371:246–252. [DOI] [PubMed] [Google Scholar]
- 5. Brouwer RW, Jakma TSC, Brouwer KH, Verhaar JA. Pitfalls in determining knee alignment: a radiographic cadaver study. J Knee Surg 2007;20:210–215. [DOI] [PubMed] [Google Scholar]
- 6. Wolff AM, Hungerford DS, Pepe CL. The effect of extraarticular varus and valgus deformity on total knee arthroplasty. Clin Orthop Relat Res 1991;271:35–51. [PubMed] [Google Scholar]
- 7. Lotke PA, Ecker ML. Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg [Am] 1977;59-A:77–79. [PubMed] [Google Scholar]
- 8. Denham RA, Bishop RE. Mechanics of the knee and problems in reconstructive surgery. J Bone Joint Surg [Br] 1978;60-B:345–352. [DOI] [PubMed] [Google Scholar]
- 9. Hvid I, Nielsen S. Total condylar knee arthroplasty. Prosthetic component positioning and radiolucent lines. Acta Orthop Scand 1984;55:160–165. [DOI] [PubMed] [Google Scholar]
- 10. Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg [Br] 1991;73-B:709–714. [DOI] [PubMed] [Google Scholar]
- 11. Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res 1994;299:153–156. [PubMed] [Google Scholar]
- 12. D’Lima DD, Hermida JC, Chen PC, Colwell CW., Jr Polyethylene wear and variations in knee kinematics. Clin Orthop Relat Res 2001;392:124–130. [DOI] [PubMed] [Google Scholar]
- 13. D’Lima DD, Chen PC, Colwell CW., Jr Polyethylene contact stresses, articular congruity, and knee alignment. Clin Orthop Relat Res 2001;392:232–238. [DOI] [PubMed] [Google Scholar]
- 14. Liau J-J, Cheng C-K, Huang C-H, Lo W-H. The effect of malalignment on stresses in polyethylene component of total knee prostheses–a finite element analysis. Clin Biomech (Bristol, Avon) 2002;17:140–146. [DOI] [PubMed] [Google Scholar]
- 15. Green GV, Berend KR, Berend ME, Glisson RR, Vail TP. The effects of varus tibial alignment on proximal tibial surface strain in total knee arthroplasty: the posteromedial hot spot. J Arthroplasty 2002;17:1033–1039. [DOI] [PubMed] [Google Scholar]
- 16. Berend ME, Ritter MA, Meding JB, et al. Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res 2004;428:26–34. [DOI] [PubMed] [Google Scholar]
- 17. Werner FW, Ayers DC, Maletsky LP, Rullkoetter PJ. The effect of valgus/varus malalignment on load distribution in total knee replacements. J Biomech 2005;38:349–355. [DOI] [PubMed] [Google Scholar]
- 18. Collier MB, Engh CA, Jr, McAuley JP, Engh GA. Factors associated with the loss of thickness of polyethylene tibial bearings after knee arthroplasty. J Bone Joint Surg [Am] 2007;89–A:1306–1314. [DOI] [PubMed] [Google Scholar]
- 19. Bargren JH, Blaha JD, Freeman MA. Alignment in total knee arthroplasty. Correlated biomechanical and clinical observations. Clin Orthop Relat Res 1983;173:178–183. [PubMed] [Google Scholar]
- 20. Morgan SS, Bonshahi A, Pradhan, et al. The influence of postoperative coronal alignment on revision surgery in total knee arthroplasty. Int Orthop 2008;32:639–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg [Am] 2010;92-A:2143–2149. [DOI] [PubMed] [Google Scholar]
- 22. Bonner TJ, Eardley WGP, Patterson P, Gregg PJ. The effect of post-operative mechanical axis alignment on the survival of primary total knee replacements after a follow-up of 15 years. J Bone Joint Surg [Br] 2011;93-B:1217-1222. [DOI] [PubMed] [Google Scholar]
- 23. Matziolis G, Adam J, Perka C. Varus malalignment has no influence on clinical outcome in midterm follow-up after total knee replacement. Arch Orthop Trauma Surg 2010;130:1487–1491. [DOI] [PubMed] [Google Scholar]
- 24. Magnussen RA, Weppe F, Demey G, Servien E, Lustig S. Residual varus alignment does not compromise results of TKAs in patients with preoperative varus. Clin Orthop Relat Res 2011;469:3443–3450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Vanlommel L, Vanlommel J, Claes S, Bellemans J. Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc 2013;21:2325–2330. [DOI] [PubMed] [Google Scholar]
- 26. Choong PF, Dowsey MM, Stoney JD. Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty. J Arthroplasty 2009;24:560–569. [DOI] [PubMed] [Google Scholar]
- 27. Longstaff LM, Sloan K, Stamp N, Scaddan M, Beaver R. Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J Arthroplasty 2009;24:570–578. [DOI] [PubMed] [Google Scholar]
- 28. Blakeney WG, Khan RJK, Palmer JL. Functional outcomes following total knee arthroplasty: a randomised trial comparing computer-assisted surgery with conventional techniques. Knee 2014;21:364–368. [DOI] [PubMed] [Google Scholar]
- 29. Schmitt J, Hauk C, Kienapfel H, et al. Navigation of total knee arthroplasty: rotation of components and clinical results in a prospectively randomized study. BMC Musculoskelet Disord 2011;12:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Harvie P, Sloan K, Beaver RJ. Computer navigation vs conventional total knee arthroplasty: five-year functional results of a prospective randomized trial. J Arthroplasty 2012;27:667-672. [DOI] [PubMed] [Google Scholar]
- 31. Lad DG, Thilak J, Thadi M. Component alignment and functional outcome following computer assisted and jig based total knee arthroplasty. Indian J Orthop 2013;47:77-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lützner J, Dexel J, Kirschner S. No difference between computer-assisted and conventional total knee arthroplasty: five-year results of a prospective randomised study. Knee Surg Sports Traumatol Arthrosc 2013;21:2241-2247. [DOI] [PubMed] [Google Scholar]
- 33. Burnett RSJ, Barrack RL. Computer-assisted total knee arthroplasty is currently of no proven clinical benefit: a systematic review. Clin Orthop Relat Res 2013;471:264-276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Rebal BA, Babatunde OM, Lee JH, et al. Imageless computer navigation in total knee arthroplasty provides superior short term functional outcomes: a meta-analysis. J Arthroplasty 2014;29:938-944. [DOI] [PubMed] [Google Scholar]
- 35. Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 2012;470:45-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hancock CW, Winston MJ, Bach JM, Davidson BS, Eckhoff DG. Cylindrical axis, not epicondyles, approximates perpendicular to knee axes. Clin Orthop Relat Res 2013;471:2278-2283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML. Does A. Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res 2013;471:1000-1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hollister AM, Jatana S, Singh AK, Sullivan WW, Lupichuk AG. The axes of rotation of the knee. Clin Orthop Relat Res 1993;290:259-268. [PubMed] [Google Scholar]
- 39. Howell SM, Papadopoulos S, Kuznik K, Ghaly LR, Hull ML. Does varus alignment adversely affect implant survival and function six years after kinematically aligned total knee arthroplasty? Int Orthop 2015. (Epub ahead of print). [DOI] [PubMed] [Google Scholar]
- 40. Dossett HG, Swartz GJ, Estrada NA, LeFevre GW, Kwasman BG. Kinematically versus mechanically aligned total knee arthroplasty. Orthopedics 2012;35:e160-e169. [DOI] [PubMed] [Google Scholar]
- 41. Ishikawa M, Kuriyama S, Ito H, et al. Kinematic alignment produces near-normal knee motion but increases contact stress after total knee arthroplasty: A case study on a single implant design. Knee 2015;22:206-212. [DOI] [PubMed] [Google Scholar]
- 42. Lustig S, Scholes CJ, Oussedik SI, et al. Unsatisfactory accuracy as determined by computer navigation of VISIONAIRE patient-specific instrumentation for total knee arthroplasty. J Arthroplasty 2013;28:469-473. [DOI] [PubMed] [Google Scholar]
- 43. Parratte S, Blanc G, Boussemart T, et al. Rotation in total knee arthroplasty: no difference between patient-specific and conventional instrumentation. Knee Surg Sports Traumatol Arthrosc 2013;21:2213-2219. [DOI] [PubMed] [Google Scholar]
- 44. Ollivier M, Tribot-Laspiere Q, Amzallag J, et al. Abnormal rate of intraoperative and postoperative implant positioning outliers using “MRI-based patient-specific” compared to “computer assisted” instrumentation in total knee replacement. Knee Surg Sports Traumatol Arthrosc 2015. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 45. Ritter MA, Davis KE, Meding JB, et al. The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg [Am] 2011;93-A:1588-1596. [DOI] [PubMed] [Google Scholar]
- 46. Kim Y-H, Park J-W, Kim J-S, Park S-D. The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop 2014;38:379-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Karachalios T, Sarangi PP, Newman JH. Severe varus and valgus deformities treated by total knee arthroplasty. J Bone Joint Surg [Br] 1994;76-B:938-942. [PubMed] [Google Scholar]
- 48. Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty 2009;24(suppl):39-43. [DOI] [PubMed] [Google Scholar]
- 49. Koskinen E, Remes V, Paavolainen P, et al. Results of total knee replacement with a cruciate-retaining model for severe valgus deformity–a study of 48 patients followed for an average of 9 years. Knee 2011;18:145-150. [DOI] [PubMed] [Google Scholar]
- 50. Bryant BJ, Tilan JU, McGarry MH, et al. The biomechanical effect of increased valgus on total knee arthroplasty: a cadaveric study. J Arthroplasty 2014;29:722-726. [DOI] [PubMed] [Google Scholar]
- 51. Tew M, Waugh W. Tibiofemoral alignment and the results of knee replacement. J Bone Joint Surg [Br] 1985;67-B:551-556. [DOI] [PubMed] [Google Scholar]


