Abstract
The incidence and severity of ankle fractures in elderly patients is increasing steadily. These injuries are challenging to treat and prone to complications.
Individual fracture treatment is tailored depending on bone quality, skin conditions, comorbidities, and functional demand of the patient. This article provides a review of current techniques to obtain stable fixation despite poor bone quality. To avoid complications, it is imperative to consider and treat comorbidities such as diabetes and osteoporosis.
In the absence of severe systemic comorbidities, the results after open reduction and internal fixation of malleolar fractures in patients above and below 60 years of age are nearly identical, while nonoperative treatment of unstable fractures leads to significantly inferior outcomes. Therefore, the general indications for surgery in elderly patients should not differ from those in younger patients.
However, it is essential to detect severe conditions such as Charcot neuro-osteoarthropathy because these require a completely different treatment regime, and standard internal fixation will invariably fail in these patients.
Cite this article: Rammelt S. Management of ankle fractures in the elderly. EFORT Open Rev 2016;1:239-246. DOI: 10.1302/2058-5241.1.000023.
Keywords: osteoporosis, diabetes, complications, posterior tibia, dislocation, syndesmosis, Charcot neuroarthropathy
Both the incidence and severity of ankle fractures in elderly patients with considerable comorbidity is rising steadily in most European countries.1 The patients are predominately women with considerable comorbidities including cardiovascular diseases, obesity, chronic pulmonary diseases and complicated diabetes. Poor bone quality in osteoporotic and diabetic patients may lead to more complicated fracture patterns and problems with fixation.2 The soft tissue envelope may be compromised through chronic vascular disease, prolonged steroid medication, and diminished skin turgor leading to open injuries even in low energy fractures.3 Mobilisation of the patients after surgery will be complicated by sarcopaenia, decreased strength, co-ordination and compliance.4
Despite the inherent higher risks in elderly patients, a therapeutic nihilism is unwarranted. An increasing number of elderly people retain an active lifestyle with high functional demands. Cast immobilisation for highly unstable ankle fractures (especially the inherently unstable pronation-abduction fractures that are frequently seen in the elderly) leads to malunion or nonunion rates between 48% and 73%.5-7 Numerous comparative studies5,6,8 including one prospective-randomised study in patients above 55 years of age8 found significantly better results after open reduction and internal fixation than after non-operative treatment for displaced malleolar fractures in the elderly. Therefore, in the absence of severe systemic comorbidities, the principal indications for surgery should not differ from those in younger patients.9 If relevant comorbidities are present, the treatment regimen has to be adapted accordingly.
This article will discuss current treatment approaches to ankle fractures in elderly patients with specific reference to frequent and relevant comorbidities such as diabetes and osteoporosis.
Diabetes mellitus
Diabetes affects wound and fracture healing on multiple levels. Clinical and experimental studies have demonstrated a diminished healing capacity of both bone and soft tissues including ligaments in patients with diabetes.10-11 In type I diabetes the missing anabolic effect of insulin and amylin in early stages, and vascular changes in later stages lead to a manifest osteoporosis with increased fracture risk.12 Chronic hyperglycaemia negatively affects the function of immunocompetent cells like fibroblasts and leukocytes leading to significantly increased rates of infection and other complications as compared to non-diabetics.11 The combination of these pathological conditions results in a significant delay in bone healing in diabetic patients, with reported union times of 163% to 187% when compared with non-diabetic patients.10 As a result of these changes in bone metabolism, patients with manifest diabetes have a higher chance of sustaining a more severe ankle fracture along with increased mortality rates.8,13
The risk of complications and the chances of diabetic comorbidities increase dramatically with poor control of the blood glucose level as reflected by a high HbA1C value.11,14 The presence of neuropathy increases the chance of a complication by a factor of 4 in diabetics.11 In addition, more than 40% of diabetic patients also present with peripheral arterial disease.15 Obesity has been identified as an independent risk factor for complications and poorer outcomes in both diabetics and non-diabetics.16
Care has to be taken to identify patients with diabetic, hereditary or idiopathic Charcot neuro-osteoarthropathy (CN) at the ankle.17 In particular, in patients with neurogenic osteoarthropathy who are non-diabetic and do not have a hereditary disorder, this condition (‘charcoid’) may be overlooked and standard treatment may lead to catastrophic results.2 These patients will need a completely different treatment regime.
Osteoporosis
Osteoporosis results from a disruption of the homeostasis between osteoclasts and osteoblasts. Due to its high metabolic turnover rate, trabecular bone is affected first, followed by cortical thinning.18 This condition affects more than 200 million patients worldwide, 6.3 million alone in Germany in 2009.19 The incidence is 885 000 patients/year with a prevalence of 24% in women and 6% in men. The condition is frequently not recognised, as only an estimated 5% of patients with osteoporosis receive drug treatment.19 Therefore, an acute fracture is often the first symptom of the disease with a lifetime fracture risk of about 40%.18 Ankle fractures make up about 10% of osteoporotic fractures. Osteporosis is defined as a T-score of less than -2.5, which means that the bone mineral density (BMD) is 2.5 standard deviations below the young adult average BMD obtained by dual-energy x-ray absorptiometry scan (DEXA), or by the presence of a fragility fracture. The ten-year probability of sustaining an osteoporotic fracture (FRAX) can be calculated using BMD and other risk factors including age, sex, body-mass index (BMI), fracture history, smoking, and other comorbidities. A FRAX > 30% requires specific therapy.18
Orthopaedic surgeons in Europe are facing a steadily increasing number of ankle fractures in patients with osteoporosis, and it is estimated that the number of low-energy ankle fractures will increase threefold by 2030.1 In patients with a history of osteoporotic fractures, inadequate trauma and/or highly unstable pronation-abduction (PA) ankle fracture-dislocations, osteoporosis has to be suspected. In a recent CT study of 194 ankles, elderly patients showed more complex fracture patterns and significantly higher bone attenuation than the younger age group, suggestive of osteoporosis.20 Routine osteodensitometry and adequate medication after confirming the diagnosis of osteoporosis are mandatory in the management of these patients.
Evaluation of elderly patients with ankle fractures
A careful history of the accident may already raise the suspicion of an osteoporotic or pathological ankle fracture if there has been no significant trauma. Clinical examination focusses on acute deformities, open wounds, the overall soft tissue condition and the neurovascular status of the injured limb (Fig. 1).
Fig. 1.

Fracture-dislocation with impeding skin necrosis produced by a prominent medial fragment of the distal tibia. Immediate reduction is warranted.
In addition, the limb should be checked for pathological disorders unrelated to the fracture that may indicate a neurological disorder, like dry, scalding skin, claw toes, subtle cavus and, above all, loss of protective sensation in the sole of the foot. In case of doubt, sensation is tested at four plantar sites with a standard 5.07 (10-g) Semmes-Weinstein monofilament. If a chronic vascular disease is suspected, the transcutaneous oxygen pressure (TcPO2) of the skin may be measured. Pressures above 30 mm Hg are needed to heal surgical wounds.16
Serum levels of glucose and haemoglobin A1C (HbA1C), as a marker for the long-term control of hyperglycaemia, should be obtained in diabetic patients in order to guide further treatment. In patients over 65 years of age with an acute ankle fracture, a routine osteodensitometry should be performed.
The diagnosis of an ankle fracture is confirmed with standard radiographs (Fig. 2). Because elderly patients will frequently present with more complex fracture patterns, a generous use of CT scanning is indicated for planning the operative approach (Fig. 4). This is especially true in the presence of a posterior tibial fragment or with suspected impaction of the tibial plafond, which cannot be assessed reliably with standard radiographs.21, 22 In the case of fracture-dislocations, CT scanning is performed after gross reduction of the fracture and external fixation.23
Fig. 2 a, b.

Trimalleolar fracture (pronation abduction stage 3) in a 79-year-old woman with severe osteoporosis.
Fig. 4 (a, b).
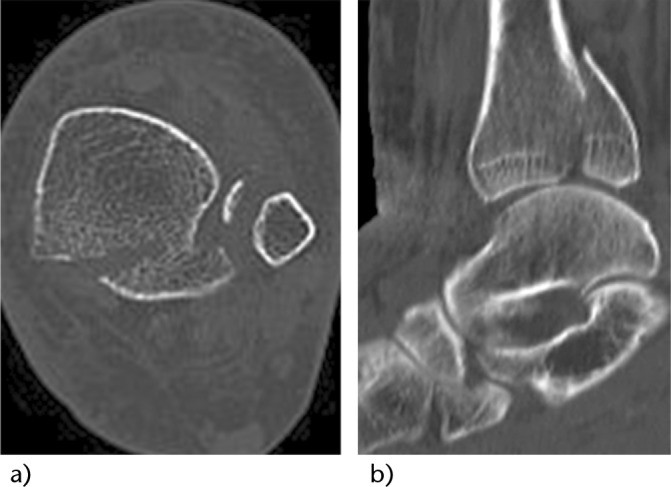
CT scanning reveals a large posterior fragment with marginal impaction of the tibial plafond (same patient as Figs 2 and 3). Note the displacement of the posterior fragment that follows the distal fibular fragment held by the posteior syndesmosis.
Non-operative treatment
Closed, stable and non-displaced fractures may be treated non-operatively. These include isolated fibular fractures without additional syndesmotic or medial ligament ruptures and isolated medial malleolar fractures without syndesmotic or lateral instability. Relevant injury to the tibio-fibular syndesmosis and/or deltoid ligament has to be ruled out by either stress or standing radiographs.23,24 Likewise, with any medial malleolar fracture, a ligamentous syndesmosis injury and a high fibular fracture (Maisonneuve type) have to be ruled out.
Manual stress testing, gravity stress testing and weight-bearing radiographs have all been suggested to detect ankle instability in acute malleolar fractures. It appears that there is a structural stability reserve in the ankle with axial loading, and therefore more patients have positive manual or gravity stress radiographs than signs of instability in weight-bearing radiographs.2,24 Therefore, the latter may be more reliable because they reflect the physiological conditions. On the other hand, it might be difficult to obtain standing radiographs in elderly patients with an acute ankle fracture who are frail or have comorbidities. Fractures that are stable under stress radiographs or axial loading can be treated with a stable orthosis or a special walker/boot that puts the foot in neutral and limits supination under full weight-bearing. A cast may be needed initially for three to five days in cases of severe soft tissue swelling. The orthosis is worn for six weeks until fracture healing. Control radiographs are obtained at one week after the injury to rule out secondary dislocation.
With poor bone quality, cast immobilisation with off-loading until radiographic evidence of bone healing is recommended. In patients with manifest Charcot neuro-osteo-arthropathy, prolonged immobilisation and complete off-loading in a well-padded total-contact cast is the first line of treatment.2,17
Emergency treatment
Grossly displaced fracture-dislocations should be reduced as soon as possible, ideally under sufficient analgesia at the site of injury, to avoid further damage to the soft tissues. If definite internal fixation is not feasible on the day of injury, highly unstable fractures should be treated initially with external fixation (Fig. 3) until definite internal fixation becomes feasible, because they tend to re-dislocate with cast immobilisation, thus being at risk for severe soft tissue complications.2,22
Fig. 3.

Tibiometatarsal transfixation is employed in cases of unstable fractures and fracture-dislocations, if a primary internal fixation is not feasible for various reasons (same patient as Fig. 2).
Open fractures and closed fractures with subcutaneous stripping, compartment syndrome, soft tissue incarceration, and impeding skin necrosis from displaced fragments all represent an emergency indication for surgery. If wound closure is impossible after debridement, fracture reduction and fixation, collagen-based skin substitutes or vacuum-assisted wound closure is employed temporarily. For optimal immobilisation and soft tissue monitoring, a tibio-metatarsal external fixator is applied in addition to any internal fixation.23 Definitive wound closure is achieved during planned revisions either by direct suture, skin graft, local or free flaps.
Techniques of fixation
Standard internal fixation22 can be considered for patients presenting with non-osteoporotic bone, palpable pulses, diabetic patients with an HbA1C of less than 7.0 indicating good control of the blood glucose levels, a BMI less than 25, and who are able to sense a 5.07 or smaller Semmes-Weinstein monofilament without manifestations of autonomic dysfunction.
In the following, several options for internal fixation of osteoporotic ankle fractures will be discussed. With extremely soft bone, a combination of these measures may be warranted.
Locking plates
Locking plates create a fixed-angle product with less risk of loosening for individual screws (Fig. 5). In a cadaveric fibula model, locking plates provided higher biomechanical stability than non-locking plates.25 Current interlocking plate designs are pre-contoured and have a low profile in order to contain smaller fragments, provide more locking options, and avoid skin irritation (Fig. 6). Fixation strength of a pre-contoured interlocking plate is independent of BMD, whereas fixation strength of non-locking screws is dependent on BMD.26 However, locking plates can fail in osteoporotic bone with either serial cut-out or serial breakage of the locking screws distal to the fracture because they usually have a smaller diameter than non-locking screws. A combination of locking and non-locking screws may be beneficial to compress the plate down to the bone and produce friction between the plate and bone, thus increasing stability.27 To enhance stability of the whole construct, longer and multiple plates may be used.
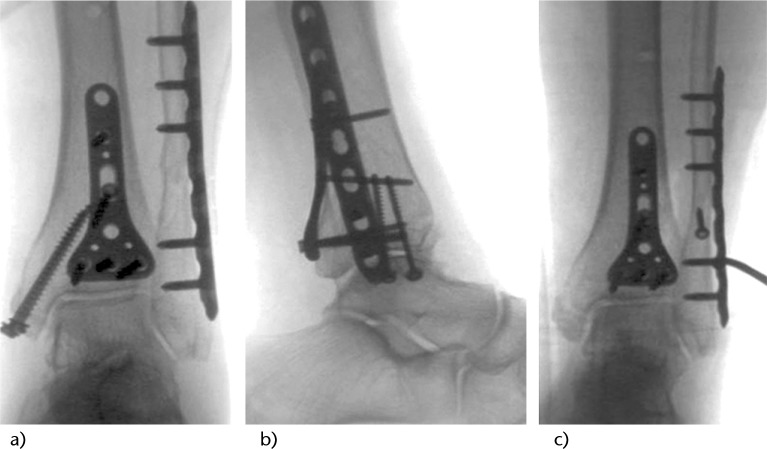
Fig. 5 a, b.
Internal fixation is achieved with a posterior and lateral interlocking plate, and screw fixation of the medial malleolus. c) Fixation of the posterior fragment stabilises the tibiofibular syndesmosis as demonstrated with the intra-operative hook test (same patient as Figs 2-4).
Fig. 6.
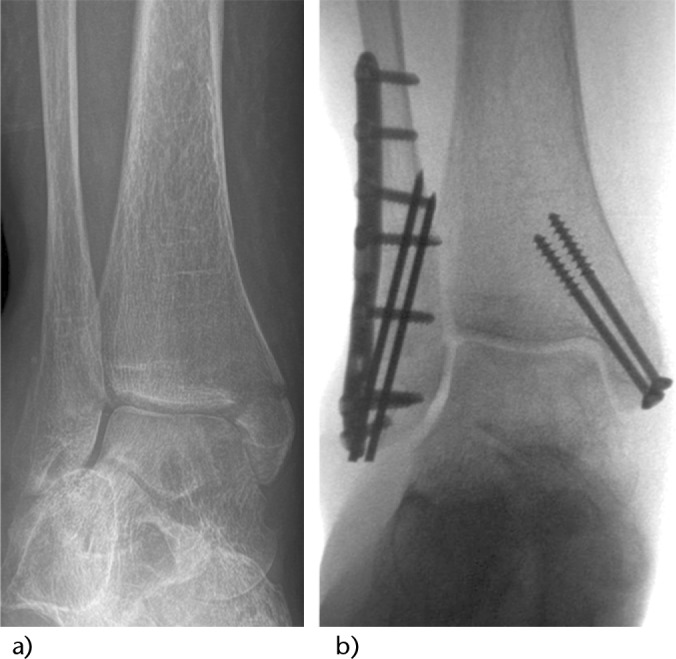
a) Bimalleolar fracture (pronation abduction stage 3) in a 57-year-old woman with osteoporosis. b) Interlocking, contoured fibular plating is supplemented by two intramedullary K-wires that engage the medial cortex.
Posterior plating of the fibula
The use of a posterior anti-glide plate on the distal fibular plate provides more biomechanical stability than a conventional or locking lateral plate.28,29 In oblique fractures, an additional interfragmentary compression screw may be placed through the plate. Care has to be taken not to position the plate within 1 cm of the tip of the fibula in order to avoid irritation of the peroneal tendons.30 In addition, a posterolateral approach to the fibula provides a better soft tissue protection for the plate than a lateral approach, which is of particular advantage in elderly patients with frail skin.
Direct fixation of the posterior tibial fragment
Recently, the role of direct stabilisation of the posterior tibial fragment has gained increased attention.21-23 Because the strong posterior tibiofibular ligament inserts at the lateral posterior tibial margin, fixation of the posterior fragment will re-establish the integrity and physiological tension of the tibiofibular syndesmosis.31 Furthermore, the exact position of this fragment is important for the anatomical position of the fibula within the tibial incisura.32 Anatomical reduction and fixation of the posterior fragment results in a stabilisation effect comparable to that of a syndesmotic screw and is associated with a lower incidence of malpositioning in post-operative CT scans.33 Direct lag screw fixation of the posterior fragment is more reliable than indirect fixation from anterior. In osteoporotic bone, a dorsal anti-glide plate (Fig. 5) will provide even more stability.23
Trans-syndesmotic fixation
In patients with osteoporotic bone, a pathological external rotation force to the ankle will produce bone avulsions of the distal tibiofibular syndesmosis rather than a purely ligamentous injury. Therefore, direct fixation of the posterior tibial rim as described above and anterior syndesmotic avulsions at the distal tibia or fibula will most likely restore syndesmotic stability.23,31-33 However, trans-syndesmotic screw fixation will enhance stability of the ankle mortise even in the absence of a syndesmotic instability, because it uses the tibia for additional stabilisation of the fibular fixation and doubles the number of cortices purchased by the screws (‘tibia pro fibula’). This technique is therefore of particular use in osteoporotic and/or diabetic patients and can be combined with the use of a locking plate on the distal fibula (Fig. 7).34
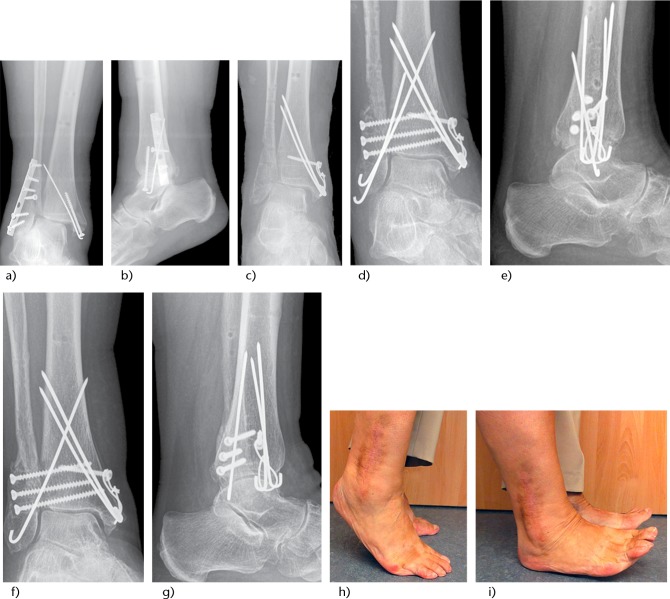
Fig. 7.
a, b Failure of standard internal fixation in a 77-year-old diabetic patient with poor bone quality but without neuropathy. c) The lateral plate had to be removed because of wound dehiscence and wound edge necrosis to avoid deep infection. d, e) The ankle mortise was restored using three syndesmotic screws (tibia pro fibula) and intramedullary pinning of the lateral and medial malleolus because of the poor soft tissue conditions. f, g) At one year after revision surgery the fractures have healed with a stable and congruent mortise. h, i) The wounds have healed uneventfully with a broad lateral scar and ankle range of motion is almost completely restored. Note the missing fifth toe after a diabetic gangrene four years earlier.
Intramedullary fixation of the distal fibula
In highly osteoporotic bone, an additional intramedullary fixation may enhance fixation with a lateral fibular plate. The use of two additional K-wires (see Fig. 6) increases the stability by 81% and torsional stability by 200% as compared to a one-third tubular plate alone.35 In patients with vulnerable skin conditions, an intramedullary fibular nail may be used to minimise soft tissue compromise.36 Another simple option to enhance fixation of the distal fibula is the use of a hook plate.2,37
Cement augmentation
Bone cements may be used to augment fixation in severely osteoporotic bone. Polymethylmethacrylate (PMMA) cement is biomechanically stable and has been widely used to enhance pull-out strength with screw fixation. Screws are inserted into the cement prior to hardening and tightened after the cement has been allowed to set. Alternatively, the hardened cement may be drilled. PMMA cement can by loaded with antibiotics in order to prevent or treat infection. In critical situations PMMA can be used as a temporary void filler, which creates a periosteum-like membrane for secondary bone grafting.39 On the other hand, PMMA is highly exothermic and non-resorbable. The use of resorbable calcium phosphate cement may be an alternative with gradual replacement by bone remodelling. In vitro studies showed comparable biomechanical properties to PMMA, but evidence from clinical studies is rare.40
Tibiotalocalcaneal fusion
Tibiotalocalcaneal fusion with a retrograde nail provides high stability, but it also results in a completely stiff ankle and hindfoot in patients who are not easy to mobilise. Therefore, it should only be an option in bedridden patients.41 Hindfoot fusion with specially designed, curved nails is an excellent treatment option for patients with Charcot neurogenic osteoarthropathy of the ankle/hindfoot type (Sanders IV), because standard techniques of internal fixation will invariably fail in these patients.17 Alternatively, a small wire external fixator may be used.42
Post-operative treatment and accompanying measures
Post-operatively, patients are protected with a lower leg cast for six to eight weeks with partial weight-bearing of 15–20 kg representing the weight of the leg touching the ground. Frequently, elderly patients will not be able to partially off-load their leg and should therefore rather be subjected to off-loading until bony union. The increased time to bone healing in patients with diabetic or idiopathic neuropathy should be considered. In patients with Charcot neuro-osteoarthropathy, a total contact cast should be applied until bony consolidation and then changed to a specific walker.
For every 1% reduction in HbA1C, there is an estimated 25% to 30% reduction in the rate of diabetic complications;43 therefore, adequate control of blood glucose levels is an integral part of the management of diabetic patients with an acute fracture. Routine osteodensitometry and adequate medication are mandatory after osteoporotic fractures. Treatment for manifest osteoporosis includes life style modifications (smoking and alcohol cessation, physical activity), vitamin D and calcium supplementation, and anti-resorptive drugs (bisphosphonates, raloxifene, denosumab). Promising new treatment options investigated in clinical trials are anabolic drugs (Calcilytic MK-5442) and antibodies against Sclerostin and Dickkopf-1.18
Results and complications
A wealth of clinical studies has shown higher complication rates after operative treatment of ankle fracture in patients with diabetes.8,10,11,13,14,16,44 Further risk factors that may coincide with diabetes are obesity, peripheral vascular disease and smoking.15,16 Low-energy open fractures are particularly prone to complications, with reported wound complications in up to 64% of patients, infection rates of up to 36%, subsequent below-knee amputation in up to 42% and a two-month mortality of 27%.45 Although the studies available have low patient numbers, the impact of skin ageing in open fractures is well-recognised.3 These fractures should therefore be regarded as limb-threatening injuries.
In the absence of severe systemic comorbidities, the results after open reduction and internal fixation of malleolar fractures in patients above and below 60 years of age are nearly identical,9 while non-operative treatment leads to significantly inferior outcomes.5-8 Therefore, the general indications for surgery in elederly patients should not differ from those in younger patients. If relevant comorbidities are present, the treatment regimen has to be adapted accordingly as outlined above.
Footnotes
Conflict of Interest: The author is a member of the AOTrauma Foot & Ankle Expert Group and the AOTrauma Foot & Ankle Education Task Force. As such he is involved in implant development for Trauma Surgery and receives travel support from AOTrauma for Meetings and Courses. The author receives research grants for investigations on biomaterials and bone healing from the Deutsche Forschungsgemeinschaft (German Research Association, DFG).
Funding
Although none of the authors has received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article, benefits have been or will be received but will be directed solely to a research fund, foundation, educational institution, or other non-profit organization with which one or more of the authors are associated.
References
- 1. Kannus P, Palvanen M, Niemi S, Parkkari J, Jarvinen M. Increasing number and incidence of low-trauma ankle fractures in elderly people: Finnish statistics during 1970-2000 and projections for the future. Bone 2002;31:430-3. [DOI] [PubMed] [Google Scholar]
- 2. Rammelt S, Heim D, Hofbauer LC, Grass R, Zwipp H. Problems and controversies in the treatment of ankle fractures. Unfallchirurg 2011;114:847-60. [DOI] [PubMed] [Google Scholar]
- 3. Court-Brown CM, Biant LC, Clement ND, Bugler KE, Duckworth AD, McQueen MM. Open fractures in the elderly. The importance of skin ageing. Injury 2015;46:189-94. [DOI] [PubMed] [Google Scholar]
- 4. Hong W, Cheng Q, Zhu X, et al. Prevalence of sarcopenia and its relationship with sites of fragility fractures in elderly Chinese men and women. PLoS One 2015;14;10:e0138102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ali MS, McLaren CA, Rouholamin E, O’Connor BT. Ankle fractures in the elderly: nonoperative or operative treatment. J Orthop Trauma 1987;1:275-80. [DOI] [PubMed] [Google Scholar]
- 6. Anand N, Klenerman L. Ankle fractures in the elderly: MUA versus ORIF. Injury 1993;24:116-20. [DOI] [PubMed] [Google Scholar]
- 7. Buckingham R, Hepple S, Winson I. Outcome of ankle fractures in the elderly. Foot Ankle Surg 2000;6:175-8. [Google Scholar]
- 8. Makwana NK, Bhowal B, Harper WM, Hui AW. Conservative versus operative treatment for displaced ankle fractures in patients over 55 years of age. A prospective, randomised study. J Bone Joint Surg [Br] 2001;83:525-9. [DOI] [PubMed] [Google Scholar]
- 9. Davidovitch RI, Walsh M, Spitzer A, Egol KA. Functional outcome after operatively treated ankle fractures in the elderly. Foot Ankle Int 2009;30:728-33. [DOI] [PubMed] [Google Scholar]
- 10. Loder RT. The influence of diabetes mellitus on the healing of closed fractures. Clin Orthop Relat Res 1988;232:210-6. [PubMed] [Google Scholar]
- 11. Wukich DK, Crim BE, Frykberg RG, Rosario BL. Neuropathy and poorly controlled diabetes increase the rate of surgical site infection after foot and ankle surgery. J Bone Joint Surg [Am] 2014;96:832-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hofbauer LC, Brueck CC, Singh SK, Dobnig H. Osteoporosis in patients with diabetes mellitus. J Bone Miner Res 2007;22:1317-28. [DOI] [PubMed] [Google Scholar]
- 13. Ganesh SP, Pietrobon R, Cecilio WA, Pan D, Lightdale N, Nunley JA. The impact of diabetes on patient outcomes after ankle fracture. J Bone Joint Surg [Am] 2005;87:1712-8. [DOI] [PubMed] [Google Scholar]
- 14. Liu J, Ludwig T, Ebraheim NA. Effect of the blood HbA1c level on surgical treatment outcomes of diabetics with ankle fractures. Orthop Surg 2013;5:203-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Novo S. Classification, epidemiology, risk factors, and natural history of peripheral arterial disease. Diabet Obes Metabol 2002;4 Suppl 2:S1-6. [DOI] [PubMed] [Google Scholar]
- 16. Cavo MJ, Fox JP, Markert R, Laughlin RT. Association between diabetes, obesity, and short-term outcomes among patients surgically treated for ankle fracture. J Bone Joint Surg [Am] 2015;97:987-94. [DOI] [PubMed] [Google Scholar]
- 17. Rammelt S, Zwipp H, Schneiders W. Treatment strategies for Charcot osteoarthropathy. Osteologie 2014;23:107-16. [Google Scholar]
- 18. Rachner TD, Khosla S, Hofbauer LC. Osteoporosis: now and the future. Lancet 2011;377(9773):1276-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hadji P, Klein S, Gothe H, et al. The epidemiology of osteoporosis - Bone Evaluation Study (BEST): an analysis of routine health insurance data. Dt Arztebl Int 2013;110:52-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lee KM, Chung CY, Kwon SS, Won SH, Lee SY, Chung MK, et al. Ankle fractures have features of an osteoporotic fracture. Osteoporosis Int 2013;24:2819-25. [DOI] [PubMed] [Google Scholar]
- 21. Bartonicek J, Rammelt S, Kostlivy K, Vanecek V, Klika D, Tresl I. Anatomy and classification of the posterior tibial fragment in ankle fractures. Arch Orthop Trauma Surg 2015;135:505-16. [DOI] [PubMed] [Google Scholar]
- 22. Rammelt S, Zwipp H. Ankle fractures. In: Bentley G, editor. European Instructional Course Lectures 12. New York: Springer; 2012:205-19. [Google Scholar]
- 23. Rammelt S, Zwipp H, Mittlmeier T. Operative treatment of pronation fracture-dislocations of the ankle. Operat Orthop Traumatol 2013;25:273-91. [DOI] [PubMed] [Google Scholar]
- 24. Weber M, Burmeister H, Flueckiger G, Krause FG. The use of weightbearing radiographs to assess the stability of supination-external rotation fractures of the ankle. Arch Orthop Trauma Surg 2010;130:693-8. [DOI] [PubMed] [Google Scholar]
- 25. Kim T, Ayturk UM, Haskell A, Miclau T, Puttlitz CM. Fixation of osteoporotic distal fibula fractures: A biomechanical comparison of locking versus conventional plates. J Foot Ankle Surg 2007;46:2-6. [DOI] [PubMed] [Google Scholar]
- 26. Zahn RK, Frey S, Jakubietz RG, et al. A contoured locking plate for distal fibular fractures in osteoporotic bone: a biomechanical cadaver study. Injury 2012;43:718-25. [DOI] [PubMed] [Google Scholar]
- 27. Illert T, Rammelt S, Drewes T, Grass R, Zwipp H. Stability of locking and non-locking plates in an osteoporotic calcaneal fracture model. Foot Ankle Int 2011;32:307-13. [DOI] [PubMed] [Google Scholar]
- 28. Schaffer JJ, Manoli A., 2nd The antiglide plate for distal fibular fixation. A biomechanical comparison with fixation with a lateral plate. J Bone Joint Surg [Am] 1987;69:596-604. [PubMed] [Google Scholar]
- 29. Minihane KP, Lee C, Ahn C, Zhang LQ, Merk BR. Comparison of lateral locking plate and antiglide plate for fixation of distal fibular fractures in osteoporotic bone: a biomechanical study. J Orthop Trauma 2006;20:562-6. [DOI] [PubMed] [Google Scholar]
- 30. Weber M, Krause F. Peroneal tendon lesions caused by antiglide plates used for fixation of lateral malleolar fractures: the effect of plate and screw position. Foot Ankle Int 2005;26:281-5. [DOI] [PubMed] [Google Scholar]
- 31. Gardner MJ, Brodsky A, Briggs SM, Nielson JH, Lorich DG. Fixation of posterior malleolar fractures provides greater syndesmotic stability. Clin Orthop Relat Res 2006;447:165-71. [DOI] [PubMed] [Google Scholar]
- 32. Rammelt S, Obruba P. An update on the diagnosis and treatment of syndemosis injuries. Eur J Trauma Emerg Surg 2015;41:601-14. [DOI] [PubMed] [Google Scholar]
- 33. Miller AN, Carroll EA, Parker RJ, Helfet DL, Lorich DG. Posterior malleolar stabilization of syndesmotic injuries is equivalent to screw fixation. Clin Orthop Relat Res 2010;468:1129-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Jani MM, Ricci WM, Borrelli J, Jr, Barrett SE, Johnson JE. A protocol for treatment of unstable ankle fractures using transarticular fixation in patients with diabetes mellitus and loss of protective sensibility. Foot Ankle Int 2003;24:838-44. [DOI] [PubMed] [Google Scholar]
- 35. Koval KJ, Petraco DM, Kummer FJ, Bharam S. A new technique for complex fibula fracture fixation in the elderly: a clinical and biomechanical evaluation. J Orthop Trauma 1997;11:28-33. [DOI] [PubMed] [Google Scholar]
- 36. Rajeev A, Senevirathna S, Radha S, Kashayap NS. Functional outcomes after fibula locking nail for fragility fractures of the ankle. J Foot Ankle Surg 2011;50:547-50. [DOI] [PubMed] [Google Scholar]
- 37. Heim D, Niederhauser K. One-third tubular hook plate. Operat Orthop Traumatol 2007;3:305-9. [DOI] [PubMed] [Google Scholar]
- 38. Panchbhavi VK, Mody MG, Mason WT. Combination of hook plate and tibial pro-fibular screw fixation of osteoporotic fractures: a clinical evaluation of operative strategy. Foot Ankle Int 2005;26:510-5. [DOI] [PubMed] [Google Scholar]
- 39. Biewener A, Meyer J, Rentsch C, et al. Internal fixation of meta- and diaphyseal intercalary bone defects after tumour resection with intramedullary nailing and porous polymethylmetacrylate (PMMA) spacer. Orthopäde 2007;36:152-8, 60-3. [DOI] [PubMed] [Google Scholar]
- 40. Collinge C, Merk B, Lautenschlager EP. Mechanical evaluation of fracture fixation augmented with tricalcium phosphate bone cement in a porous osteoporotic cancellous bone model. J Orthop Trauma 2007;21:124-8. [DOI] [PubMed] [Google Scholar]
- 41. Al-Nammari SS, Dawson-Bowling S, Amin A, Nielsen D. Fragility fractures of the ankle in the frail elderly patient: treatment with a long calcaneotalotibial nail. Bone Joint J 2014;96-B:817-22. [DOI] [PubMed] [Google Scholar]
- 42. Pinzur MS. The role of ring external fixation in Charcot foot arthropathy. Foot Ankle Clin 2006;11:837-47. [DOI] [PubMed] [Google Scholar]
- 43. Hoogwerf BJ, Sferra J, Donley BG. Diabetes mellitus-overview. Foot Ankle Clin 2006;11:703-15. [DOI] [PubMed] [Google Scholar]
- 44. Bibbo C, Lin SS, Beam HA, Behrens FF. Complications of ankle fractures in diabetic patients. Orthop Clin North Am 2001;32:113-33. [DOI] [PubMed] [Google Scholar]
- 45. Toole WP, Elliott M, Hankins D, Rosenbaum C, Harris A, Perkins C. Are low-energy open ankle fractures in the elderly the new geriatric hip fracture? J Foot Ankle Surg 2015;54:203-6. [DOI] [PubMed] [Google Scholar]