Abstract
The pathogenesis of hallux valgus deformity is multifactorial. Conservative treatment can alleviate pain but is unable to correct the deformity. Surgical treatment must be adapted to the type and severity of the deformity. Success of surgical treatment ranges from 80% to 95%, and complication rates range from 10% to 30%.
Ankle osteoarthrosis most commonly occurs as a consequence of trauma. Ankle arthrodesis and total ankle replacement are the most common surgical treatments of end stage ankle osteoarthrosis. Both types of surgery result in similar clinical improvement at midterm; however, gait analysis has demonstrated the superiority of total ankle replacement over arthrodesis. More recently, conservative surgery (extraarticular alignment osteotomies) around the ankle has gained popularity in treating early- to mid-stage ankle osteoarthrosis.
Adult acquired flatfoot deformity is a consequence of posterior tibial tendon dysfunction in 80% of cases. Classification is based upon the function of the tibialis posterior tendon, the reducibility of the deformity, and the condition of the ankle joint. Conservative treatment includes orthotics and eccentric muscle training. Functional surgery is indicated for treatment in the early stages. In case of fixed deformity, corrective and stabilising surgery is performed.
Cite this article: Crevoisier X, Assal M, Stanekova K. Hallux valgus, ankle osteoarthrosis and adult acquired flatfoot deformity: a review of three common foot and ankle pathologies and their treatments. EFORT Open Rev 2016;1:58–64. DOI: 10.1302/2058-5241.1.000015.
Keywords: hallux valgus, ankle osteoarthritis, acquired flatfoot deformity, diagnosis, conservative and surgical management
Hallux valgus
Hallux valgus deformity is the most common reason to visit a foot and ankle surgeon in Europe. The deformity occurs more commonly in females than males (8:1). Although a familiar predisposition has been identified, the aetiology and pathogenesis of hallux valgus still remain unclear and are thought to be multifactorial. The usually accepted radiological definition of hallux valgus on weight-bearing radiographs includes increased intermetatarsal (IM > 10°) and metatarso-phalangeal (MTP > 10°) angles. However, the analysis of hallux valgus deformity is much more subtle than a simple radiographic angular evaluation. Clinically, it should include the mobility of the first MTP joint, its reducibility, the extent of intra-articular pain, the presence of transfer metatarsalgia and the presence of associated deformities including clawtoes, dislocation of the lesser MTP joints, flatfoot, etc. Radiological attention should be focussed on the congruence or incongruence of the first MTP joint, orientation of the distal metatarsal articular angle (DMAA), degenerative changes of the joint, indirect manifestations of the insufficiency of the first ray, typically including hypertrophy of the second metatarsal, fatigue fracture of the second metatarsal, osteoarthrosis of the second tarso-metatarsal joint (TMT2) and dislocation of the lesser MTP joints (Fig. 1). This careful analysis is mandatory for the choice of the most efficient treatment. Conservative treatment includes the adaptation of footwear and the design and fitting of insoles. It can bring pain alleviation but no conservative treatment has the faculty to correct the deformity.
Fig. 1.
Indirect signs of first ray insufficiency include: a) osteoarthritis of the second tarso-metatarsal joint, and b) fatigue fracture of the second metatarsal. Other indirect signs are hypertrophy of the second metatarsal and dislocation of the lesser MTP joints.
Surgical treatment includes the combination of bony and soft tissue procedures. Approaches can be open, minimally invasive or percutaneous. Percutaneous approaches to the hallux are becoming increasingly popular and constant improvements are reported.1,2 Nevertheless, to date, no strong evidence exists regarding their superiority over open techniques.3,4 In most cases, and in our experience, success rather depends upon the correct evaluation of the pathology and upon the mastering of a given technique by the surgeon. Without entering into details, mild to moderate deformities (i.e. IM angle < 18° to 20°, with absence of degenerative changes, absence of significant indirect signs of insufficiency of the first ray) can be managed by a distal first metatarsal osteotomy (e.g. chevron or scarf osteotomy), associated or not with a proximal phalanx medial closing-wedge osteotomy (Akin) and a distal soft tissue procedure (Fig. 2). Severe deformities require a proximal first metatarsal osteotomy or a TMT1 fusion (Lapidus) associated with a distal soft tissue procedure (Fig. 3). In some cases (rheumatoid arthritis, osteo-arthritic MTP1, elderly patient, etc.), a MTP1 fusion may be the best choice. The juvenile hallux valgus, which includes a congruent first MTP and a pathological DMAA (Fig. 4), requires not only the correction of the IM angle but also correction of the DMAA in order to prevent recurrence. Overall results following hallux valgus surgery are good or excellent in 80% to 90% of cases. The complication rate is in the range of 10% to 30% and includes recurrence, overcorrection, residual pain, nonunion and chronic regional pain syndrome (CRPS).5,6
Fig. 2.

Mild to moderate deformities can be managed by a distal first metatarsal osteotomy and a distal soft tissue procedure.
Fig. 3.

Severe deformities require a proximal first metatarsal osteotomy or a TMT1 fusion (Lapidus as shown here) associated with a distal soft tissue reefing procedure.
Fig. 4.
On these AP views of a juvenile hallux valgus we can appreciate on both a) and c) the congruent joint and the pathologic distal metatarsal articular angle. The correction has been performed by b) a de-rotating chevron osteotomy in the mild case and by d) a modified Lapidus procedure plus a de-rotating chevron osteotomy in the more severe case.
Ankle osteoarthrosis
Ankle osteoarthrosis most commonly occurs as a consequence of trauma.7 The prevalence of ankle osteoarthritis is difficult to determine, nevertheless it is known that the prevalence of symptomatic ankle osteoarthritis is nine times less frequent than that of the knee and the hip. Ankle osteoarthrosis is associated with pain and gait alteration.7,8 Conservative treatment includes medication and orthotics. Ankle arthrodesis and total ankle arthroplasty (TAA) are the most commonly used surgical treatments and have been shown to be associated with equivalent mid-term clinical results.9,10 Recently, conservative surgery around the ankle, including corrective osteotomies and soft tissues balancing, has gained popularity in treating early- to mid-stage ankle osteoarthritis.11
Ankle arthrodesis (AA) was described by Albert in 1879, and for almost a century it was considered the gold standard for surgical treatment of end-stage ankle osteoarthritis. Relative contraindications include advanced osteoarthritis of the neighbouring joints, rheumatoid arthritis, arteriopathy and poor soft tissues conditions. In the first two cases a TAA should be discussed and in the two latter cases a pluri-disciplinary approach involving vascular and plastic surgeons is required.
Several techniques have been described, including closed, open and arthroscopic procedures. Open procedures can be performed through lateral, anterior or posterior approaches. Having the choice between these different approaches is useful in cases involving fragile soft tissue conditions. Many fixation techniques also exist, including casting alone, external fixation and internal fixation with screws, plates and/or staples (Fig. 5). Positioning of the fused ankle is very important and should include a slight valgus of the hind foot (5° to 10°), a slight external rotation (10°), and a neutral position in the sagittal plane. Respecting these positions allows the hind foot complex to optimise compensatory motion, resulting in a more physiological gait pattern.7,8,12 Ankle arthrodesis has been demonstrated to result in significant pain alleviation and good functional results.9,10,13,14 In recent years there has been a trend towards arthroscopic ankle arthrodesis because it has been shown to result in shorter hospital stay, lower initial complication rate and better early outcome.15 Performing arthroscopic ankle arthrodesis in cases of severe deformity, however, may be challenging, or impossible. Major drawbacks associated with ankle arthrodesis, as described in the literature over the last 40 years, are the 10% to 60% rate of occurrence of osteoarthritis in the neighbouring joints in the long-term,16 a nonunion rate of 10% to 20%, which has now dropped to 5% to 10% thanks to modern fixation techniques, and an historical infection rate of 3% to 25%, which is much closer to 2% to 5% today.
Fig. 5.
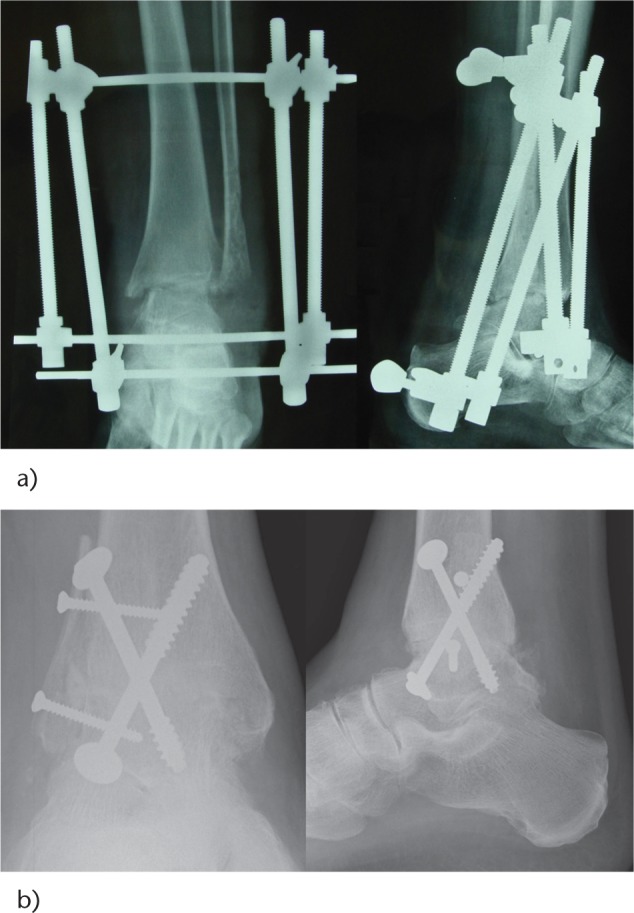
Many fixation techniques exist for ankle arthrodesis: a) AP and lateral views of an arthrodesis of the left ankle with external fixation using the Charnley frame; b) AP and lateral views of an arthrodesis of the right ankle with crossed screws internal fixation.
Total ankle arthroplasty (TAA) was first performed in the early 1970s and consisted of the implantation in some cases of an inverted femoral hip prosthesis into the tibia and a cemented acetabular cup into the calcaneus. After a difficult start due to a high complication rate, mostly associated with inadequate implant designs and fixation, ankle arthroplasty has strongly evolved during the past 20 years and is now challenging ankle arthrodesis as an alternative treatment for end-stage ankle osteoarthritis.17 Careful patient selection is more important for the success of TAA than the technical features. Indications for TAA include end-stage osteoarthrosis, rheumatoid arthritis, low to moderate functional demand, sufficient bone quality, healthy soft tissue envelope and well-aligned ankle and hind foot. Relative contraindications are high functional demand, diabetes, previous septic ankle arthritis and being overweight. Absolute contraindications include active or recent septic ankle arthritis, talar or distal tibial necrosis, unstable soft tissue envelope, neuroarthropathy and morbid arteriopathy. Today, the concept which includes anatomical design, minimal bone resection, non-cemented fixation, three components and semi-constrained mechanics is generally accepted regarding implant design (Fig. 6). The advantages of fixed-bearing versus mobile-bearing implants are not yet established. However, since the US market is the largest and since there is no FDA approval for mobile bearing ankle prostheses yet in the USA, there is a natural trend towards the use of fixed-bearing implants. Furthermore, even if not definitively proven, fixed-bearing implants are thought to reduce peri-prosthetic cyst formation and, thus, to possibly increase implant survival rates. Pre-operative assessment requires careful clinical examination of the foot and ankle as well as of the lower limbs, weight-bearing radiographs of the ankle and CT scans. Implantation planning can be performed on radiographs or on a CT scan using two-dimensional drawing templates or computer-assisted three-dimensional (3D) reconstruction. An anterior approach is usually performed, i.e. between the extensor hallucis longus and the tibialis anterior tendons. Few prostheses are designed to be implanted through a lateral, trans-malleolar approach. Post-operative care usually includes the application of a below-knee walking cast for six weeks associated with immediate weight bearing as tolerated, followed by a physiotherapy programme to optimise ankle motion, strength and proprioception. In terms of function and pain alleviation, mid-term results after TAA are equivalent to those following ankle arthrodesis.9,10,14 In terms of biomechanics, neither the arthrodesis nor the TAA is able to restore normal gait. Nevertheless, TAA is associated with a more physiological gait pattern than arthrodesis.8,18 The main drawbacks associated with TAA include, at first, and based upon several national registers, the low implant survival rate when compared with prosthetic replacement of other weight-bearing joints. In fact, the average survival rate is 80% at ten years, and up to 90% in the best cases. Additionally, the revision rate is particularly high: 10% to 20% at five years and 20% to 40% at ten years.19,20 Most frequent complications include primary or secondary malleolar fractures (0% to 10%), loosening (5% to 20%) and infections (2% to 4%). Peri-prosthetic cyst formation (Fig. 7) has been recognised as a major problem in recent years; they are encountered in up to 60% of cases21 and their origin is still not clearly established although polyethylene and metallic particles seem to play a leading role. Based upon the low survival rate and the shortcomings of TAA, optimising implant design and also exploring the concept of revision implants have now become important fields of research.
Fig. 6.
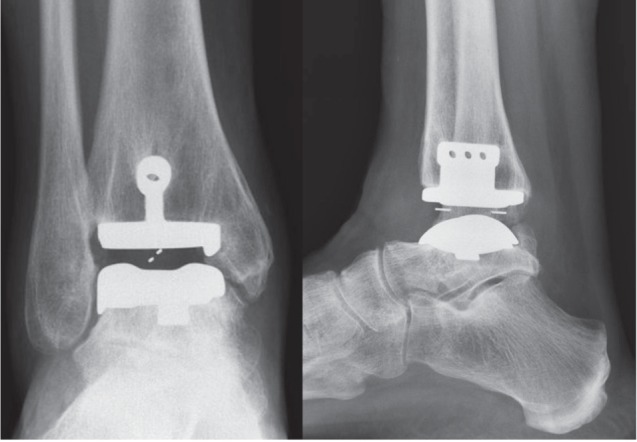
AP and lateral views of a three-component, semi-constrained, cementless, mobile-bearing ankle prosthesis of the left ankle.
Fig. 7.
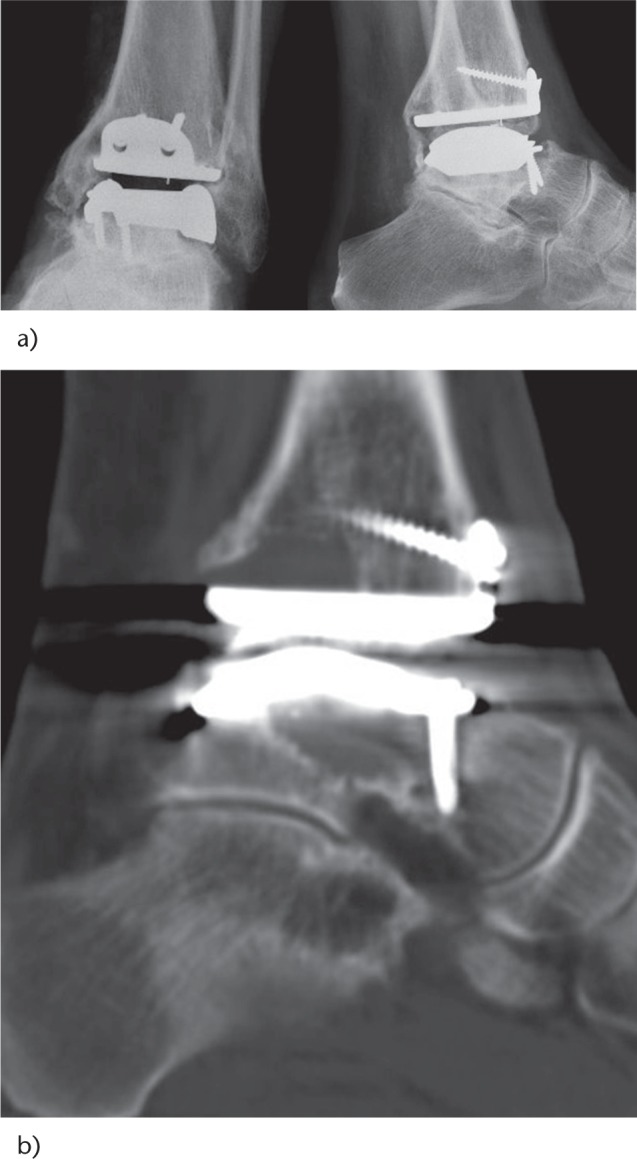
Peri-prosthetic cyst formation has become a major concern in total ankle arthroplasty (TAA). They cannot always be recognised on a) conventional radiographs and require b) a CT scan to be quantified.
Shortcomings regarding mid- and long-term results after either ankle arthrodesis or TAA have led to the search for alternative surgical solutions. Conservative surgery around the ankle belongs to these potential solutions. Techniques for supramalleolar corrective osteotomies had already been described almost 40 years ago.22 In the early 2000s, a small series demonstrated their efficiency, especially in the case of varus osteoarthritis of the ankle.23,24 Today, conservative surgery has evolved towards a more refined approach including assessment of the type of deformity, the stage of ankle osteoarthritis, the main location of the deformity, and the combination of osseous and soft tissue procedures for morphologic and functional correction.11 To date, only a few clinical reports are available but their results appear to be promising and, above all, they stimulate research in this field.
Adult acquired flatfoot deformity
Adult acquired flatfoot deformity (AAFD) is a 3D deformity including valgus of the hind foot, flattening of the longitudinal arch and abduction of the forefoot (Fig. 8) and, in most cases, the talo-navicular joint is the apex of the deformity and the key joint for its correction. Conditions like rheumatoid arthritis (RA), trauma or neurological disorders may result in an acquired flatfoot deformity. The most frequent cause of AAFD, however, is the posterior tibial tendon dysfunction in 80% of cases. The pathology ranges from a flexible flatfoot with painful but functional posterior tibial tendon to a rigid deformity including osteoarthritis of the ankle. The most commonly-used classification of AAFD was established by Johnson and Strom in 198925 and completed by Myerson in 1996:26 It is based on the severity of the deformity, its reducibility and the articular alterations. The pathology is not limited to the posterior tibial tendon but also includes ligamentous structures, especially the deltoid spring ligaments, and the joints of the hind foot complex and the ankle joint. Symptoms associated with AAFD include pain and swelling along the posterior tibial tendon, pain at the lateral aspect of the hind foot (sinus Tarsi, fibulo-calcaneal impingement) and at the ankle in the late stages. Clinical signs include swelling and tenderness along the tibialis posterior tendon in the early stages, then increased valgus of the hind foot, flattening of the longitudinal arch and abduction of the forefoot. Assessment of the function of the tibialis posterior tendon (single heel rise test) (Fig. 9), of the reducibility of the hind foot and of the midfoot deformities, and of the length of the gastrocnemii (Silfverskiöld test) are the most important aspects of the functional clinical examination. Radiographic examination usually includes anteroposterior (AP)/lateral weight-bearing radiographs of the foot and AP weight-bearing radiographs of the ankle.
Fig. 8.

Acquired adult flatfoot deformity is a 3D deformity including valgus of the hind foot, flattening of the longitudinal arch (planus) and abduction of the forefoot.
Fig. 9.

The single heel rise test is an important aspect in the assessment of adult acquired flatfoot deformity. In this patient, presenting with a flexible flatfoot deformity of the left foot, the absence of correction of the hind foot into varus during single heel rise is pathognomonic for a tibialis posterior tendon dysfunction.
In the early stages (stages I and II), conservative treatment should be attempted since specific eccentric programmes associated with the prescription of orthoses have been shown to result in symptomatic and functional improvements,27 however without changes in tendon morphology or neovascularisation. In the later stages (stages III and IV), where the deformity is already fixed, conservative treatment will have poor corrective capability. However, in cases of inoperability of the patient, custom-made shoes and orthoses can bring pain alleviation and functional improvement. Depending upon the success or otherwise of the conservative treatment, surgery can be performed at all stages. In stage I, a tibialis posterior tendon synovectomy can bring pain alleviation. In stage II, functional surgery will usually be indicated and includes a soft tissue procedure (i.e. replacement of the diseased posterior tibial tendon by a flexor tendon, flexor hallucis longus or flexor digitorum longus, frequently associated with gastrocnemius lengthening and, in some cases, with the spring ligament reconstruction) and a protective bony procedure (i.e. medial displacement osteotomy of the greater tuberosity of the calcaneus or lengthening of the lateral column) (Figs 10 and 11). The above-mentioned procedures are the most frequently described techniques in the literature. For neither the soft tissues nor the bony procedures has one technique been proven to be superior to the other. Furthermore, even if gastrocemius lengthening is performed in the majority of cases, its absolute necessity has not been established. In stage III, stabilising surgery includes double or triple corrective arthrodesis of the hind foot. In stage IV, an additional procedure often has to be performed at the ankle (i.e. TAA or arthrodesis). Results of functional surgery go along with pain alleviation and functional improvement. Mid-term biomechanical evaluation has even demonstrated normalisation of gait in some cases. Corrective stabilising surgery also reduces pain and improves function but without full normalisation of gait.28 The overall complication rate after flatfoot surgery is in the range of 10% to 30%.29
Fig. 10.
Functional surgery for flexible flatfoot deformity usually includes soft tissues and bony procedures. a) The harvest of the flexor digitorum longus tendon (FDL) at the node of Henry and its transfer into the navicular as replacement of the diseased posterior tibial tendon. b) Medial displacement calcaneal osteotomy realigns the hind foot and neutralises the valgus traction of the triceps surae; it protects the transferred FDL.
Fig. 11.
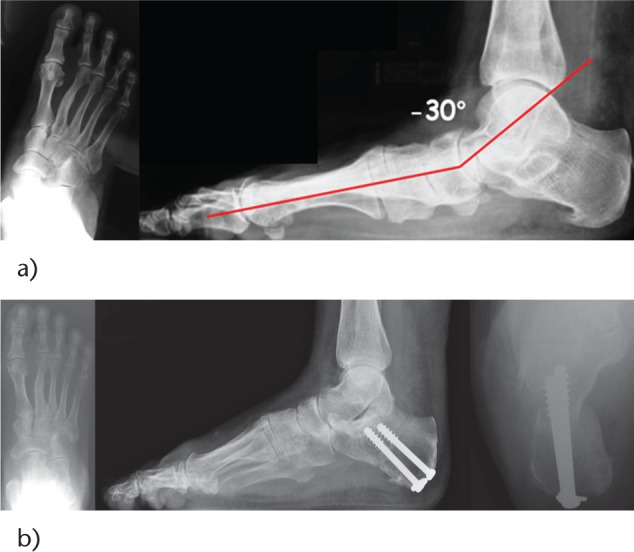
Radiographic appearance of a stage II flexible acquired flatfoot deformity a) before and b) after functional surgical correction including lengthening of the gastrocnemii, medial displacement osteotomy of the calcaneus and flexor digitorum longus transfer to the distal stump of the tibialis posterior tendon.
Footnotes
Conflict of Interest: None declared.
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Redfern D, Vernois J, Legré BP. Percutaneous surgery of the forefoot. Clin Podiatr Med Surg 2015;32:291-332. [DOI] [PubMed] [Google Scholar]
- 2. Magnan B, Bortolazzi R, Samaila E, Pezzè L, Rossi N, Bartolozzi P. Percutaneous distal metatarsal osteotomy for correction of hallux valgus. Surgical technique. J Bone Joint Surg [Am] 2006;88(suppl 1 Pt 1):135-148. [DOI] [PubMed] [Google Scholar]
- 3. Leemrijse T, Valtin B, Besse JL. [Hallux valgus surgery in 2005. Conventional, mini-invasive or percutaneous surgery? Uni- or bilateral? Hospitalisation or one-day surgery?]. Rev Chir Orthop Repar Appar Mot 2008;94:111-127. [Article in French] [DOI] [PubMed] [Google Scholar]
- 4. Trnka HJ, Krenn S, Schuh R. Minimally invasive hallux valgus surgery: a critical review of the evidence. Int Orthop 2013;37:1731-1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Easley ME, Trnka HJ. Current concepts review: hallux valgus part II: operative treatment. Foot Ankle Int 2007;28:748-758. [DOI] [PubMed] [Google Scholar]
- 6. Easley ME, Trnka HJ. Current concepts review: hallux valgus part 1: pathomechanics, clinical assessment, and nonoperative management. Foot Ankle Int 2007;28:654-659. [DOI] [PubMed] [Google Scholar]
- 7. Thomas RH, Daniels TR. Ankle arthritis. J Bone Joint Surg [Am] 2003;85-A(5):923-936. [DOI] [PubMed] [Google Scholar]
- 8. Chopra S, Rouhani H, Assal M, Aminian K, Crevoisier X. Outcome of unilateral ankle arthrodesis and total ankle replacement in terms of bilateral gait mechanics. J Orthop Res 2014;32:377-384. [DOI] [PubMed] [Google Scholar]
- 9. Haddad SL, Coetzee JC, Estok R, Fahrbach K, Banel D, Nalysnyk L. Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis. A systematic review of the literature. J Bone Joint Surg [Am] 2007;89:1899-1905. [DOI] [PubMed] [Google Scholar]
- 10. Daniels TR, Younger AS, Penner M, et al. Intermediate-term results of total ankle replacement and ankle arthrodesis: a COFAS multicenter study. J Bone Joint Surg [Am] 2014;96:135-142. [DOI] [PubMed] [Google Scholar]
- 11. Knupp M, Hintermann B. Treatment of asymmetric arthritis of the ankle joint with supramalleolar osteotomies. Foot Ankle Int 2012;33:250-252. [DOI] [PubMed] [Google Scholar]
- 12. Buck P, Morrey BF, Chao EY. The optimum position of arthrodesis of the ankle. A gait study of the knee and ankle. J Bone Joint Surg [Am] 1987;69:1052-1062. [PubMed] [Google Scholar]
- 13. Thomas R, Daniels TR, Parker K. Gait analysis and functional outcomes following ankle arthrodesis for isolated ankle arthritis. J Bone Joint Surg [Am] 2006;88:526-535. [DOI] [PubMed] [Google Scholar]
- 14. Jordan RW, Chahal GS, Chapman A. Is end-stage ankle arthrosis best managed with total ankle replacement or arthrodesis? A systematic review. Adv Orthop 2014;986285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Townshend D, Di Silvestro M, Krause F, et al. Arthroscopic versus open ankle arthrodesis: a multicenter comparative case series. J Bone Joint Surg [Am] 2013;95:98-102. [DOI] [PubMed] [Google Scholar]
- 16. Coester LM, Saltzman CL, Leupold J, Pontarelli W. Long-term results following ankle arthrodesis for post-traumatic arthritis. J Bone Joint Surg [Am] 2001;83-A:219-228. [DOI] [PubMed] [Google Scholar]
- 17. Henne TD, Anderson JG. Total ankle arthroplasty: a historical perspective. Foot Ankle Clin 2002;7:695-702. [DOI] [PubMed] [Google Scholar]
- 18. Piriou P, Culpan P, Mullins M, Cardon JN, Pozzi D, Judet T. Ankle replacement versus arthrodesis: a comparative gait analysis study. Foot Ankle Int 2008;29:3-9. [DOI] [PubMed] [Google Scholar]
- 19. Labek G, Klaus H, Schlichtherle R, Williams A, Agreiter M. Revision rates after total ankle arthroplasty in sample-based clinical studies and national registries. Foot Ankle Int 2011;32:740-745. [DOI] [PubMed] [Google Scholar]
- 20. Henricson A, Nilsson JA, Carlsson A. 10-year survival of total ankle arthroplasties: a report on 780 cases from the Swedish Ankle Register. Acta Orthop 2011;82:655-659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Besse JL, Brito N, Lienhart C. Clinical evaluation and radiographic assessment of bone lysis of the AES total ankle replacement. Foot Ankle Int 2009;30:964-975. [DOI] [PubMed] [Google Scholar]
- 22. Weber BG. Zur Operationstechnik der supramalleolaren valgisierenden Osteotomie beim Erwachsenen. [Operative techniques for supramalleolar valgus osteotomy in adults (author’s transl)]. Unfallheilkunde 1977;80:191-193. [Article in German] [PubMed] [Google Scholar]
- 23. Takakura Y, Takaoka T, Tanaka Y, Yajima H, Tamai S. Results of opening-wedge osteotomy for the treatment of a post-traumatic varus deformity of the ankle. J Bone Joint Surg [Am] 1998;80:213-218. [DOI] [PubMed] [Google Scholar]
- 24. Harstall R, Lehmann O, Krause F, Weber M. Supramalleolar lateral closing wedge osteotomy for the treatment of varus ankle arthrosis. Foot Ankle Int 2007;28:542-548. [DOI] [PubMed] [Google Scholar]
- 25. Johnson KA, Strom DE. Tibialis posterior tendon dysfunction. Clin Orthop Relat Res 1989;196-206. [PubMed] [Google Scholar]
- 26. Myerson MS, Corrigan J. Treatment of posterior tibial tendon dysfunction with flexor digitorum longus tendon transfer and calcaneal osteotomy. Orthopedics 1996;19:383-388. [DOI] [PubMed] [Google Scholar]
- 27. Kulig K, Lederhaus ES, Reischl S, Arya S, Bashford G. Effect of eccentric exercise program for early tibialis posterior tendinopathy. Foot Ankle Int 2009;30:877-885. [DOI] [PubMed] [Google Scholar]
- 28. Arangio GA, Salathe EP. A biomechanical analysis of posterior tibial tendon dysfunction, medial displacement calcaneal osteotomy and flexor digitorum longus transfer in adult acquired flat foot. Clin Biomech (Bristol, Avon) 2009;24:385-390. [DOI] [PubMed] [Google Scholar]
- 29. Pinney SJ, Lin SS. Current concept review: acquired adult flatfoot deformity. Foot Ankle Int 2006;27:66-75. [DOI] [PubMed] [Google Scholar]





