Abstract
A severely painful, dysfunctional, or destroyed distal radio-ulnar joint (DRUJ) can be reconstructed by fusion, interposition of soft tissue, or by arthroplasty using prostheses.
The objective of this study was to review the literature on implants and evaluate their effectiveness in terms of pain relief, range of motion and longevity.
A search was carried out using protocols and well-defined criteria in PubMed, the Cochrane Library and by screening reference lists. The review was conducted according to PRISMA guidelines.
Of the 27 publications reporting on nine different implants, we excluded reports with less than five cases and silastic replacements of the ulna head. Eighteen publications describing a total of five implants were selected for analysis. Nine of the publications were useful for the evaluation of implant longevity. Despite methodological shortcomings in many of the source documents, a summary estimate was possible.
It seems that DRUJ implants have good potential to improve function through pain reduction; an improvement was observed in 17 series, although it was significant in only seven series.
Instability is not uncommon with ulna head-only implants, but they cause fewer clinical problems and re-interventions than might be expected.
The risk of deep infection is small with the available implants.
Overall implant survival in papers with at least five years’ follow-up is 95%, with a slightly better longevity of 98% for the constrained implants.
Periprosthetic osteolysis/radiolucency is frequently reported. Its causes and consequences are not clarified.
Cite this article: Calcagni M, Giesen T. Distal radioulnar joint arthroplasty with implants: a systematic review. EFORT Open Rev 2016;1:191-196. DOI: 10.1302/2058-5241.1.160008.
Keywords: distal radioulnar joint, implants, arthroplasty
Introduction
A destroyed distal radioulnar joint (DRUJ) can be reconstructed by fusion, resection and/or interposition of soft tissue or arthroplasty. Fusion is not desirable, as prono-supination is second only to thumb opposition in the evolution of the upper limb and refinement in manipulation.
Resection arthroplasties have shown great limitations in producing pain relief and stability of the DRUJ. Studies by Hagert, and Lees and Scheker made it progressively obvious that both the Darrach and Sauvé-Kapandji operations (and any of their variants) were destabilising procedures in relation to the whole forearm.1,2
The DRUJ can also be reconstructed using artificial materials. Partial DRUJ arthroplasty was attempted in the 1970s by means of ulna head replacement with silastic implants. We define these implants as Type 1 implants, aimed at creating an interposition between the bone ends. Since the failed silicone arthroplasty was abandoned, until recently few reports could be found which described attempts at prosthetic replacement.
What we define as Type 2 implants are those that partially or completely replace the ulna head only, some of them presenting with features engineered to allow the reattachment of the ligamentous components in order to stabilise the DRUJ. Multi-component implants are, in our view, Type 3 implants, and they consist of a radial component replacing the sigmoid notch, and an ulna component fixed to the ulna shaft replacing the ulna head. These systems are constrained or semi-constrained. Type 3 implants are characterised by their attempt to mimic triangular fibro cartilage complex (TFCC) biomechanics whilst allowing radius proximal-distal shifting during prono-supination. They also seek to avoid direct contact between bone and artificial material at the joint interface surface.
The intent of this systematic review was to draw general conclusions regarding:
Clinical results, in terms of mobility and pain reduction;
Complications;
Implant longevity.
Methods
The review was conducted according to PRISMA guide-lines.3
Search strategy
We carried out a primary search through PubMed and the Cochrane Library. All studies on DRUJ arthroplasty and ulna head replacement written in English were included in a qualitative analysis, without time restriction. A continuous supplementary search, scanning the reference lists of the papers first included, was performed (2 December 2015). Cadaveric studies, biomechanical studies, studies not accessible in journals, books or online documents and reviews without primary data were excluded. Double publications and articles with an overlap of cases were relative exclusion criteria. Articles not written in English were judged on the basis of an English abstract, if available.
Quality assessment
We focussed on the number of cases, methodology and the observation period. Papers with fewer than ten cases were considered to be less useful and are therefore only mentioned very briefly. Implant longevity was primarily evaluated on the basis of papers with a cumulated implant survival of at least five years, and secondarily, on papers with a follow-up of a minimum of two years in each case. Function was evaluated using well-validated and relevant outcome measurement tools such as the Disabilities of Arm, Shoulder and Hand (DASH) score, the Patient-Rated Wrist Evaluation (PRWE) or the Mayo Wrist Score (MWS). Series with clinical data collected before surgery and similarly at follow-up were defined as prospective, even if there had been no mention of a pre-operative protocol. We attempted to clarify whether the authors were involved as inventors, developers or producers.
Results
A total of 27 papers were eligible. Screening for double publication and overlap of data, led to the exclusion of four papers.4,5,6,7 We also excluded three papers with fewer than five cases,8,9,10 and two reports on rubber ulna head replacement.11,12
Of the 18 articles remaining for final analysis, nine fulfilled the criteria for analysis of longevity.13-21 The eligible studies represent a maximum of 350 cases, but the precise number is likely somewhat smaller, due to an overlap between some of the series. Declared rheumatoid wrists constituted 5% of the total number of cases, and patients younger than 40 years of age totalled 13% of the 350 wrists. Two papers had fewer than ten cases, but more than five.22,23
Implants
We analysed a total of four different implants, including certain modifications (see Table 1 for a summary of the results). Of the analysed implants:
Table 1.
An analysis of four different implants
| Name and manufacturer | Implant type | No. of cases | Average follow-up (years) | Longevity | Most common complications | Patient satisfaction |
|---|---|---|---|---|---|---|
| UHP, Martin GMBH, Germany (Fig. 1) |
2 | 72 | 6.5 | 99% | Bone resorption at the ulna collar Sigmoid notch erosion |
95% |
| U-Head, Small Bone Innovation, USA. (Fig. 2) |
2 | 101 | 4 | 90% | Erosion at the sigmoid notch Pedestal in the ulna shaft |
96% |
| Aptis DRUJ Prostheses, Aptis Medical, USA. (Fig. 3) |
3 | 163 | 5 | 98% | ECU synovitis Progressive radiolucency of the ulna |
97% |
| Implant presented by Schuurman AH. Manufacturer not declared. (Fig. 4) |
3 | 19 | 4 | 64% (80% with late design) |
Not reported | 63% |
Two implants were ulna head-only replacements.
Two replaced the ulna head and sigmoid notch, and are semi-constrained.
Two resurfacing implants, two ulna head-only implants (Type 2 implants) and one Type 3 semi-constrained implant were not analysed, as fewer than five cases or no cases at all were reported.
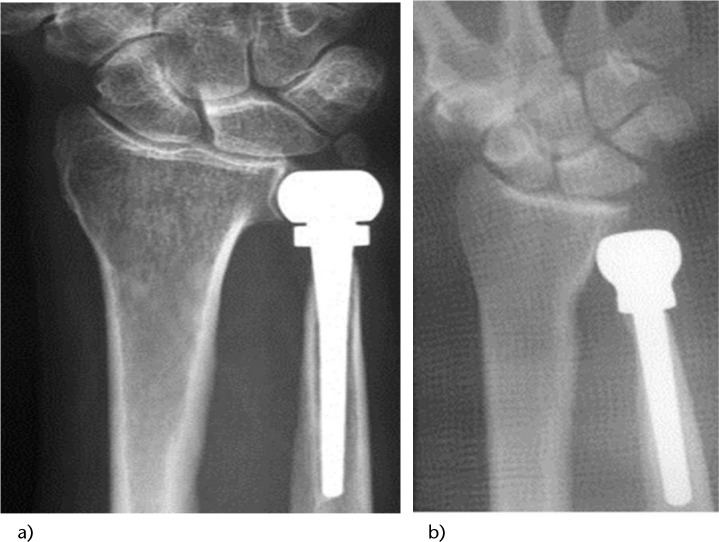
Of the analysed implants, one is titanium and ceramic, with the option of using a metal head for failed Sauve-Kapandji lesions (Fig. 1). Three implants are chromium-cobalt. The semi-constrained implants also have a component of polyethylene (Figs 2, 3, 4).
Fig. 1.

The Herbert Ulnar Head Prosthesis implant (KLS Martin Group, Jacksonville, FL) consists of a titanium stem with a ceramic head. A metallic head is optional for revision of failed Sauve-Kapandji.
Fig. 2.
The uHead implant (Small Bone Innovations, Inc, Morrisville, PA) has a similar design to the UHP implant. It is an implant in chromium-cobalt with a metallic head and a slot on the head for the re-fixation of the TFCC.
Fig. 3.
The Aptis DRUJ prostheses. It is formed by an ulnar and radial component. The interface is an ultra-high molecular polyethylene (UHMP) sphere that allows the proximal-distal migration of the radius during prono-supination.
Fig. 4.
The implant introduced by Shuurman. It is a chromium-cobalt implant with a radial and ulnar component. The radial component has a cruciform shape in order to assure stable osseo-integration in the radius. The interface is a polyethylene ring.
Clinical results
Three papers provided a pre- as well as post-operative range of prono-supination movement, demonstrating a statistical improvement in the range of motion, especially in supination.13,24,25 The other papers did not show any statistical improvement in the range of motion, or did not provide enough information to demonstrate such an improvement.
Ten papers (the majority) show a statistically-significant improvement in the Visual Analogue Scale (VAS) for pain.13-14,17-18,24,26-30 Two of these papers showed a statistical improvement in pain in 80% of cases.26,27 The other eight papers did show improvement in the VAS for pain, but it was either not statistically significant, or a statistical analysis was not performed.
Five reports of constrained implants with two components (Type 3 implants) reported the lifting capacity of the patients, and this appeared to be improved.14,20,26-27,30 One paper on Type 2 implants reported that lifting capacity was improved.13
Grip strength was not significantly improved or changed in most of the ten papers in which it was reported. In four papers, grip strength was significantly improved,14,18,29-30 whilst in another four papers, grip strength was not reported.
The DASH score was reported in 11 papers, and was significantly improved in four of them,14,22,26-27 all of which were Type 3 implants. The PRWE score was reported in seven papers and was significantly improved in three of them, which were all Type 3 implants.14,26-27 The Mayo Clinic score was reported in six papers and was significantly improved in four of them;14,17,26,29 two papers reported Type 2 implants and two papers Type 3 implants.
Thirteen papers reported patient satisfaction. The percentage of patient satisfaction was 95% for Type 2 implants with ulna head replacement only. For Type 3 implants, constrained and semi-constrained, the percentage of satisfied patients was 98% when we excluded the constrained implant presented by Schuurman et al. This implant alone showed a satisfaction rate of only 63%, and the percentage of satisfied patients with Type 3 implants drops to 80% if we include this series.
Implant loosening
Seventeen papers reported implant loosening. Nine of them had a follow-up equal to or greater than five years. Longevity was 95% for the Herbert and the Mayo implants (Type 2 implants), but with one independent review of 47 cases reporting a survival of 83% at six years.17 Longevity for the Scheker prostheses and the Mayo II implants (Type 3 implants) was 98%. Longevity for the implant presented by Schuurman (Type 3 implant) was 63% overall (80% for the latest design).
Complications
Late complications that required secondary surgery were quite common for the Scheker Implant (21%), with the most common complication being synovitis of the extensor carpi ulnaris (ECU) tendon. In one series this was reported to be as high as 44%.16 The second most common complication for this implant was irritation of the superficial radial nerve (RSN) and synovitis of the tendons of the first dorsal compartment, often due to excessive length of the radial screws.
In Type 2 implants (ulna head-only replacement) the most common complications were radiological, mainly DRUJ instability and sigmoid notch erosion (see below). It was impossible to extrapolate an overall percentage of the cases that required soft tissue stabilisation and/or interposition or any further procedure. Only in one study was the need of later soft tissue interposition reported, in 36% of cases.29 It is mentioned in several studies that the presence of a pedestal at the proximal tip of the stem of the ulna is correlated with a worse functional result.17 It is also mentioned that initial radiological changes at the ulna level and in the sigmoid notch have a tendency not to progress in the long-term.18 Finally, it is reported that only around half of the radiologically-unstable implants required further surgery. We found only two cases from over 350 reported procedures of deep post-operative infection (0.5%).
Radiology
Osteolysis or radiolucency at the ulna collar was assessed in varying ways. In ten of the 18 series, no useful information could be retrieved, whereas eight papers reported osteolysis without frank loosening of the implant components. This radiolucency or osteolysis at the distal ulna stump was reported to be 90%, and 100% of cases in Type 2 implants in two studies,24,30 and 30% for Type 3 implants, in four studies with a progressive tendency. In Type 2 implants radiological DRUJ instability was reported in three papers and observed in 21% of cases if we calculate all the cases reported (Fig. 3). For Type 2 implants (ulna head-only replacement), erosion of the sigmoid notch was observed in one-third of the cases with no apparent progression after five years.
Discussion
This report is limited by the poor quality of several articles and the lack of homogeneity in clinical evaluation. Only nine publications included data collected pre- as well as post-operatively. Of these nine papers, seven used a validated and widely-used outcome measurement system. In eight of the 18 papers, the inventor was among the authors (Fig. 4). This seemed not to have had an impact on the reported clinical or longevity results, but this factor represents an important bias.
Our analyses were limited to the calculation of mean or median values, whereas calculation of statistically-significant differences was not possible. Despite this, we found that some general conclusions were possible.
In terms of complications, it appears that the risk of deep infection is small, as we found only two cases (0.5%). Instability seems to be the main problem with Type 2 implants, followed by sigmoid notch erosion, but these two problems are not as preponderant as foreseen or suggested by the developers of constrained or semi-constrained implants with a radial component.
It has to be said that the only real measurement of optimal DRUJ function is the capacity to prono-supinate under-load and lifting capacity. This parameter is unfortunately reported in only two series reporting Type 3 implants. In general, mean values for motion at follow-up are similar for most implants, and generally an improved supination is reported, except in one series that reported an improved pronation with the Schuurman implant.28 The general tendency is for the mean level of function to increase, as evaluated with patient-rated outcome measures, and for pain to reduce. However, a general summary of the extent of pain reduction through the different reports is impossible. Satisfaction rates are generally reported as very high (95% Type 2, 98% Type 3). Only the implant reported by Schuurman showed large limitations in longevity with the latest design (80% survival at four years).
One of the main questions of this review was whether Type 3 implants produce better outcomes. The general impression is that Type 3 implants have slightly better results in terms of stability, function and longevity, but a higher rate of post-operative soft tissue complications that require surgery, principally synovitis of the extensor carpi radialis tendon.
In our study, a reasonable appreciation of the longevity of the implant was possible across 17 papers, although only nine provided information on cumulated implant survival. The most widely-accepted and commonly-used definition of failure in implant survival analysis is the removal of the implant. In some cases, the implant was removed as a result of increasing pain and discomfort. We excluded these cases from our longevity evaluation. We only considered cases with clinical pain and discomfort associated with radiological loosening of the implant itself to be implant failure. Periprosthetic osteolysis/radiolucency, with or without gross loosening, has been systematically investigated in only eleven series. The remaining studies report on the phenomenon but use no standardised definitions or methods. Osteolysis, which occurred frequently around the ulna shaft, seems to be a common problem for all types of implants.
Conclusions
It seems that constrained or semi-constrained implants have a strong potential for improvement of function, through pain reduction and preservation or improvement of mobility. These implants also seem to produce more post-operative complications, but do not have a higher rate of loosening. The risk of severe complications – deep infection and instability – is small with the available implants. An implant survival of 90%-100% at five years is reported in most series, and it has shown to be unsatisfactory only with the Type 3 implant introduced by Schuurman.
After considering the number of publications, and those not involving the inventor and the number of patients treated, the most popular implant seems to be the implant introduced by Scheker (Type 3).
The possible causes and consequences of frequently-reported complications among all types of implants such as radiolucency/osteolysis, sigmoid notch erosion and radiological instability need further investigation.
Footnotes
Conflict of Interest: Dr. Calcagni declares fees outside of the submitted work as a speaker for Swedish Orphan Biovitrum.
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Hagert CG. The distal radioulnar joint in relation to the whole forearm. Clin Orthop Relat Res 1992;275:56-64. PMID:1735234. [PubMed] [Google Scholar]
- 2. Lees VC, Scheker LR. The radiological demonstration of dynamic ulnar impingement. J Hand Surg [Br] 1997;22:448-50. [Google Scholar]
- 3. Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Open Med 2009;3:123-30. [PMC free article] [PubMed] [Google Scholar]
- 4. Schuurman AH, Teunis T. A new total distal radioulnar joint prosthesis: functional outcome. J Hand Surg [Am] 2010;35:1614-19. PMID:20843612. [DOI] [PubMed] [Google Scholar]
- 5. van Schoonhoven J, Herbert TH, Krimmer H. Neue Konzepte der Endoprothetik des distalen Radioulnargelenkes [New concepts for endoprostheses of the distal radio-ulnar joint]. Handchir Mikrochir Plast Chir 1998;30:387-392. PMID:9888011. [in German]. [PubMed] [Google Scholar]
- 6. van Schoonhoven J, Fernandez DL, Bowers WH, Herbert TJ. Salvage of failed resection arthroplasties of the distal radioulnar joint using a new ulnar head prosthesis. J Hand Surg [Am] 2000;25:438-46. PMID:10811747. [DOI] [PubMed] [Google Scholar]
- 7. V Schoonhoven J, Herbert TJ, Fernandez DL, Prommersberger KJ, Krimmer H. Ulnakopfprothese [Ulnar head prosthesis]. Orthopade 2003;32:809-15. PMID:14508648. [in German]. [DOI] [PubMed] [Google Scholar]
- 8. Ewald TJ, Skeete K, Moran SL. Preliminary experience with a new total distal radioulnar joint replacement. J Wrist Surg 2012;1:23-30. PMID:23904976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Garcia-Elias M. Eclypse: partial ulnar head replacement for the isolated distal radio-ulnar joint arthrosis. Tech Hand Up Extrem Surg 2007;11:121-8. PMID:17536535. [DOI] [PubMed] [Google Scholar]
- 10. Wehbé MA. Prosthetic arthroplasty of the distal radioulnar joint: historical perspective and 24-year follow-up. Hand Clin 2013;29:91-101. PMID:23168031. [DOI] [PubMed] [Google Scholar]
- 11. Sagerman SD, Seiler JG, Fleming LL, Lockerman E. Silicone rubber distal ulnar replacement arthroplasty. J Hand Surg [Br] 1992;17:689-93. PMID:1484256. [DOI] [PubMed] [Google Scholar]
- 12. Stanley D, Herbert TJ. The Swanson ulnar head prosthesis for post-traumatic disorders of the distal radio-ulnar joint. J Hand Surg [Br] 1992;17:682-8. PMID:1484255. [DOI] [PubMed] [Google Scholar]
- 13. Axelsson P, Sollerman C, Kärrholm J. Ulnar head replacement: 21 cases; mean follow-up, 7.5 years. J Hand Surg [Am] 2015;40:1731-8. PMID:26216078. [DOI] [PubMed] [Google Scholar]
- 14. Rampazzo A, Gharb BB, Brock G, Scheker LR. Functional outcomes of the aptis-scheker distal radioulnar joint replacement in patients under 40 years old. J Hand Surg [Am] 2015;40:1397-1403.e3. PMID:26095055. [DOI] [PubMed] [Google Scholar]
- 15. Bizimungu RS, Dodds SD. Objective outcomes following semi-constrained total distal radioulnar joint arthroplasty. J Wrist Surg 2013;2:319-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Savvidou C, Murphy E, Mailhot E, Jacob S, Scheker LR. Semiconstrained distal radioulnar joint prosthesis. J Wrist Surg 2013;2:41-8. PMID:24436788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kakar S, Swann RP, Perry KI, Wood-Wentz CM, Shin AY, Moran SL. Functional and radiographic outcomes following distal ulna implant arthroplasty. J Hand Surg [Am] 2012;37:1364-71. PMID:22721459. [DOI] [PubMed] [Google Scholar]
- 18. van Schoonhoven J, Mühldorfer-Fodor M, Fernandez DL, Herbert TJ. Salvage of failed resection arthroplasties of the distal radioulnar joint using an ulnar head prosthesis: long-term results. J Hand Surg [Am] 2012;37:1372-80. PMID:22652179. [DOI] [PubMed] [Google Scholar]
- 19. Yen Shipley N, Dion GR, Bowers WH. Ulnar head implant arthroplasty: an intermediate term review of 1 surgeon’s experience. Tech Hand Up Extrem Surg 2009;13:160-4. PMID:19730047. [DOI] [PubMed] [Google Scholar]
- 20. Laurentin-Pérez LA, Goodwin AN, Babb BA, Scheker LR. A study of functional outcomes following implantation of a total distal radioulnar joint prosthesis. J Hand Surg Eur Vol 2008;33:18-28. PMID:18332015. [DOI] [PubMed] [Google Scholar]
- 21. Kachooei AR, Chase SM, Jupiter JB. Outcome assessment after aptis distal radioulnar joint (druj) implant arthroplasty. Arch Bone Jt Surg 2014;2:180-4. PMID:25386579. [PMC free article] [PubMed] [Google Scholar]
- 22. Axelsson P, Sollerman C. Constrained implant arthroplasty as a secondary procedure at the distal radioulnar joint: early outcomes. J Hand Surg [Am] 2013;38:1111-8. PMID:23707011. [DOI] [PubMed] [Google Scholar]
- 23. Kaiser GL, Bodell LS, Berger RA. Functional outcomes after arthroplasty of the distal radioulnar joint and hand therapy: a case series. J Hand Ther 2008;21:398-409. PMID:19006766. [DOI] [PubMed] [Google Scholar]
- 24. Herzberg G. Periprosthetic bone resorption and sigmoid notch erosion around ulnar head implants: a concern? Hand Clin 2010;26:573-7. PMID:20951906. [DOI] [PubMed] [Google Scholar]
- 25. Fernandez DL, Joneschild ES, Abella DM. Treatment of failed Sauvé-Kapandji procedures with a spherical ulnar head prosthesis. Clin Orthop Relat Res 2006;445:100-7. PMID:16601411. [DOI] [PubMed] [Google Scholar]
- 26. Galvis EJ, Pessa J, Scheker LR. Total joint arthroplasty of the distal radioulnar joint for rheumatoid arthritis. J Hand Surg [Am]. 2014;39:1699-1704. PMID:24996676. [DOI] [PubMed] [Google Scholar]
- 27. Kakar S, Fox T, Wagner E, Berger R. Linked distal radioulnar joint arthroplasty: an analysis of the APTIS prosthesis. J Hand Surg Eur Vol 2014;39:739-44. PMID:24554688. [DOI] [PubMed] [Google Scholar]
- 28. Schuurman AH. A new distal radioulnar joint prosthesis. J Wrist Surg 2013;2:359-62. PMID:24436843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Willis AA, Berger RA, Cooney WP., III Arthroplasty of the distal radioulnar joint using a new ulnar head endoprosthesis: preliminary report. J Hand Surg [Am] 2007;32:177-89. PMID:17275592. [DOI] [PubMed] [Google Scholar]
- 30. Sauerbier M, Arsalan-Werner A, Enderle E, Vetter M, Vonier D. Ulnar head replacement and related biomechanics. J Wrist Surg 2013;2:27-32. PMID:24436786. [DOI] [PMC free article] [PubMed] [Google Scholar]