Abstract
High-energy pilon fractures are challenging injuries. Multiple options are described for the definitive surgical management of these fractures, but there is no level I evidence for optimal management. The current management and recommendations for treatment will be reviewed in this article.
Anatomical reduction of the fracture, restoration of joint congruence and reconstruction of the posterior column with a correct limb axis minimising the soft-tissue insult are the key points to a good outcome when treating pilon fractures.
Even when these goals are achieved, there is no guarantee that results will be acceptable in the mid-term due to the frequent progression to post-traumatic arthritis.
In high-energy fractures with soft-tissue compromise, a staged treatment is generally accepted as the best way to take care of these devastating fractures and is considered a local ‘damage control’ strategy.
The axial cuts from the CT scan images are essential in order to define the location of the main fracture line, the fracture pattern (sagittal or coronal) and the number of fragments. All of this information is crucial for pre-operative planning, incision placement and articular surface reduction.
No single method of fixation is ideal for all pilon fractures, or suitable for all patients. Definitive decision making is mostly dependent on the fracture pattern, condition of the soft-tissues, the patient’s profile and surgical expertise.
Cite this article: Tomás-Hernández J. High-energy pilon fractures management: state of the art. EFORT Open Rev 2016;1:354-361. DOI: 10.1302/2058-5241.1.000016.
Keywords: pilon fracture, high-energy, open reduction and internal fixation, ORIF, distal tibia, tibial plafond, staged treatment
Introduction
Pilon fractures are distal tibia end fractures affecting the weight-bearing articular surface. They represent around 1% of all lower extremity fractures, and are more common in males between 35 and 40 years of age.1 Such injuries may be caused by high- or low-energy mechanisms.
Axial compression injuries where the talus impacts on the distal articular surface, causing implosion of the tibial plafond are caused by high-energy mechanisms with key characterisitcs including severe soft-tissue injuries, comminution and multiple displaced articular fragments. Conversely, rotational injuries are typically low-energy fractures with less soft-tissue injury and, usually, a distal tibial spiral fracture pattern. In this review, we will focus on the management of high-energy, axial compression injuries.
Initial management
The surgical management of pilon fractures is technically demanding and requires accurate pre-operative planning. The pre-operative plan should include a complete clinical and radiographic evaluation. It is mandatory to evaluate the neurovascular function and the status of the soft-tissue envelope of the injured extremity, as open wounds, lacerations, oedema, deep skin contusions and blisters are common findings with pilon fractures (Fig. 1).
Fig. 1.

Soft-tissue status after a high-energy pilon fracture.
A systematic physical examination should be performed in order to identify any associated injuries involving the ipsilateral foot, knee or other locations in cases of polytrauma.2 In addition, it is useful to identify the patient comorbidities associated with risks of soft-tissue complications such as malnutrition, alcoholism, diabetes, neuropathy, tobacco use, peripheral vascular disease and osteoporosis.3 Radiographic evaluation starts with standard ankle radiographs and full-length images of the tibia and fibula in order to determine the displacement of the talus (proximal or medial/lateral dislocation), the proximal extension of the fracture into the shaft, the association of fibular fractures and the metaphyseal comminution.
The initial management of this fracture differs depending on the type of injury. If we are dealing with a low-energy rotational injury without soft-tissue compromise, it is usually safe to immobilise the extremity in a cast and plan for an early primary open reduction and internal fixation (ORIF) following the classical principles described in 1979 by Rüedi and Allgöwer.4 On the other hand, early primary ORIF of high-energy pilon fractures is usually associated with soft-tissue complications and, in the case of an open fracture, the incidence of deep wound infection or dehiscence which requires surgical debridement, reported to be necessary in up to 19% of cases.5,6
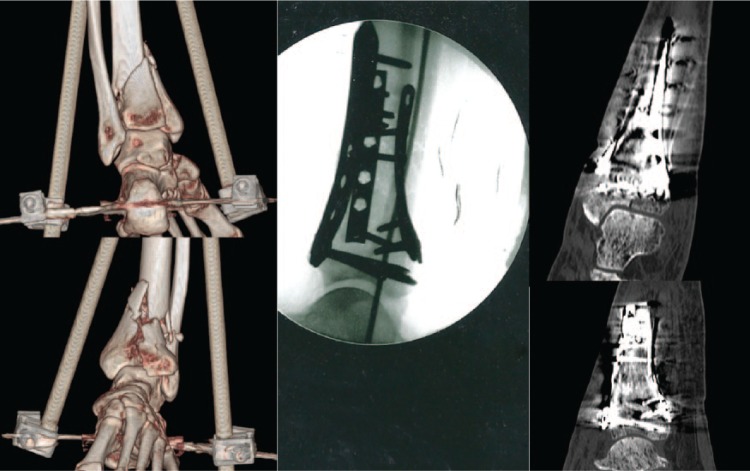
For that reason, in high-energy fractures with soft-tissue compromise a staged treatment like those described in two 1999 articles7,8 is generally accepted as the best way to take care of this devastating fracture and is considered a local ‘damage control’ strategy.9 The protocol consists of initial ankle-spanning external fixation (delta or rectangular frame) with or without fibular fixation and delayed definitive ORIF until soft-tissues are restored. The timing of fibular fixation is controversial10 as an acute inappropriate incision placement for fibular fixation can compromise future approaches. We rarely fix the fibula at the same time as we perform the spanning external fixation, because we plan the definitive surgical approaches after viewing the CT scan images post-external stabilisation. This facilitates the fracture interpretation under traction.11 Temporary stabilisation should be performed as soon as possible with the goal of restoring the alignment rather than obtaining a perfect reduction, while bearing in mind the need to avoid pins crossing possible future surgical fields. An extension of the fixator onto the first metatarsal is helpful to avoid an equinus contracture in cases where it is expected to be necessary to mantain the spanning situation for a long period due to the initial soft-tissue status (Fig. 2).
Fig. 2.

Spanning external fixation as part of a staged treatment.
Diagnostics
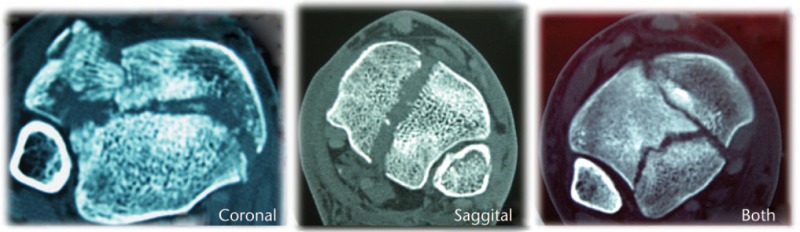
As already mentioned, the most useful method of determining the ‘personality’ and morphology of a is the CT scan after spanning the fracture. The axial cuts from the CT scan are mandatory images in order to define the location of the main fracture line, the fracture pattern (sagittal or coronal) and the number of fragments12 (Fig. 3).
Fig. 3.
Fracture patterns: coronal, saggital and both.
All of this information is crucial for pre-operative planning, incision placement and articular reduction. CT has been shown to provide additional beneficial information for 82% of cases, resulting in a change to the surgical plan in 64% of cases operations.13
Topliss, Jackson and Atkins12 used the CT scan on 126 consecutive pilon fractures. Their study offered a CT-based classification of fracture pattern variability. They classified fracture patterns as either ‘sagittal’ or ‘coronal’, based on the main fracture line from the axial CT cuts at the plafond level. They correlated this information with patient and deformity characteristics, finding that sagittal patterns were more frequently related to high-energy injuries in young patients and tended to present with varus deformity, while coronal patterns tended to be related to low-energy fractures in elderly patients and often presented with valgus deformity.
Fracture pattern will be different depending on the position of the foot and the force direction of the impact. If the foot is dorsiflexed, the anterior part of the pilon will be more comminuted, while if the foot is neutral or plantar flexed, the central and posterior part will be more affected respectively. Usually there are three constant articular fragments that can vary in size and comminution: anterolateral, posterolateral and medial. From a surgical point of view, it is helpful to divide the distal tibia and plafond into three basic columns: lateral, medial and posterior.14 Generally, posterior fragments are less comminuted than those in the anterior or central areas.
Classifications
The most used radiograph classifications for pilon fractures are those of Rüedi and Allgöwer,4 and the AO Foundation and Orthopaedic Trauma Association classifications (AO/OTA).15
Rüedi and Allgöwer classified pilon fractures into three groups:
Type I: Non-displaced fractures;
Type II: Displaced fractures with loss of articular congruency;
Type III: Displaced and severely comminuted fractures with impaction.
The AO/OTA classification divided pilon fractures into three main groups — 43-A: extra-articular fractures; 43-B: partial articular fractures; 43-C: complete articular fractures.
The Rüedi and Allgöwer classification has been widely used over the years, but has low inter-rater reliability, especially between types II and III. The AO/OTA classification was proven to have superior inter-rater agreement,16 and its usage has gradually gained traction, becoming more used and accepted.
Definitive management
Controversy still exists regarding how best to treat these injuries, but most clinicians advocate surgical intervention, unless contraindicated, with some combination of ORIF or external fixation with or without limited ORIF.
Treatment goals include anatomical reduction of the articular surface, restoration of the extremity length, rotation and axial alignment with respect to the soft-tissue envelope with a stable construct that allows early motion of the ankle to achieve a stable, reduced and healed ankle which will allow ambulation. Multiple options are described for the definitive surgical management of pilon fractures, but there is no level I evidence for optimal management.17 Actual treatments are described below.
Open reduction internal fixation (ORIF)
Once the soft-tissues have recovered from injury and the ‘personality’ of the fracture has been assessed from CT scans, it is time to plan the surgical technique. The tendency is to design the approach closer to the main fracture line in the axial cuts of the CT scan, to minimise the soft-tissue damage and surgical stripping.
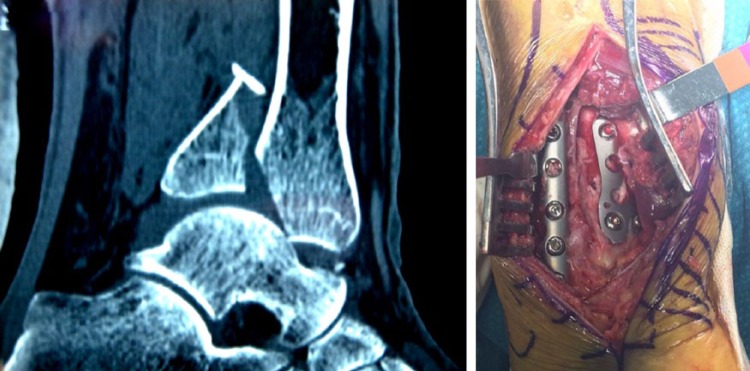
The restoration of the articular surface normally starts by opening the more anterior articular fragments to visualise the central and posterior fragments (Fig. 4).
Fig. 4.
Opening the more anterior fragments allows access to the central and posterior comminution.
The individual articular fragments are then reduced from posterior to anterior, using the posterolateral articular fragment as a template. The provisional reduction of each fragment should be performed with Kirschner (K-)wires, and definitive fixation can be accomplished with two or three screws. Sometimes there are smaller osteochondral fragments that can be fixed with mini-fragment screws, bioresorbable pins, or even flush-cut and buried wires.18 When the articular reduction is achieved, multiple anatomical low profile locking or non-locking plates are available to connect the articular fragment to the tibia.19
Generally, fracture patterns that end with valgus failure and lateral compression (coronal patterns) have main fracture lines that exit laterally in the tibia, and are better supported with anterolateral plating techniques through anterolateral approaches. On the other hand, fracture patterns that end with varus angulation of the tibia with lateral tension failure and compression of the medial side (sagittal patterns) are better supported with medial buttress plates; most of them can be managed with good outcomes through minimally invasive techniques with percutaneous medial approaches (Fig. 5).20-22
Fig. 5.

Pilon fracture treated with a minimally invasive, percutaneous medial technique.
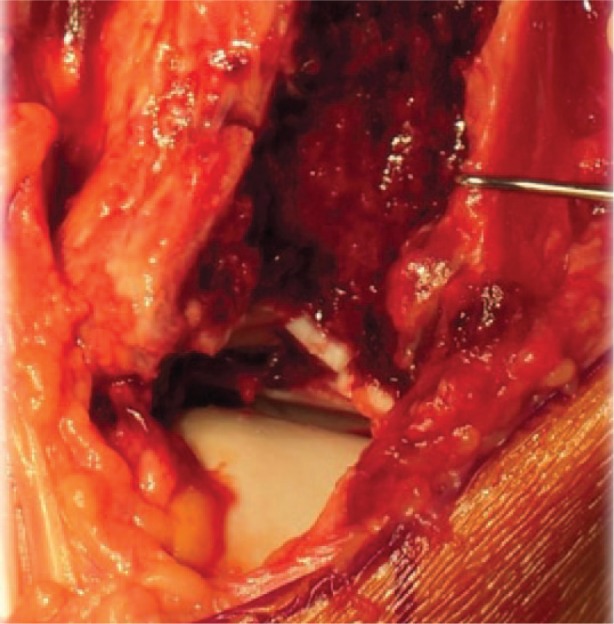
More complex fractures with complete articular injuries in the medial, lateral and central areas usually need mid-line, anteromedial or anterior extensile approaches23,24 that allow visualisation of the entire plafond to reduce the joint. These complex fractures may require a combination of anterolateral and medial plates for their fixation (Fig. 6).25
Fig. 6.
Complex fractures may require a combination of different plates and approaches for fixation.
In the majority of pilon fracture cases, posterior fragments can be addressed directly or indirectly from anterior approaches, but there are some situations where the posterior fracture aspect is better approached directly from a posterolateral approach, in the interval between the peroneal tendons and the flexor hallucis longus,26 such as pilon fractures with extensive comminution of the metaphyseal—diaphyseal aspect of the posterior column with shortening and malalignment, or cases where there are incarcerated fragments posteriorly that are not accessible from the anterior. In those scenarios, the posterior column must be reduced and then fixed with a one-third tubular plate or a pre-contoured anatomical implant acting as a buttress plate. This approach must be used with caution because of its possible skin complications.27 After posterior reduction is achieved, the posterior column acts as a template to reduce the anterior pilon. An advantage of the posterolateral approach is that the fibula can be addressed if needed from the same incision by mobilising the peroneal tendons medially (Fig. 7).28
Fig. 7.
An advantage of the posterolateral approach is that the fibula can be addressed if needed from the same incision, by mobilising the peroneal tendons medially.
Controversy remains regarding when and how to perform the fibular fixation that is associated with pilon fractures in 90% of cases.29 Classically, the surgical sequence described by Rüedi and Allgöwer begins with the fibular reduction.4 The benefits of beginning by fixing the fibula include the restoration of the length of the lateral column and the indirect reduction by ligamentotaxis that can be achieved of the anterolateral Chaput fragment, and the posterolateral Volkman fragments that remain in continuity with the lateral malleolus.30 However there are some concerns about fixing the fibula as the first surgical step:
In cases of severe fibular comminution, it can be difficult to obtain a perfect anatomical reduction in terms of length and rotation. The lack of anatomical reduction of the fibula may prevent anatomical reduction of the tibia. In that situation, it can be more helpful to start the surgical sequence by reducing the tibia.
In those cases where an anterolateral tibial approach is planned, the addition of a close incision for the fibula may contribute to wound complications and it is not recommended. If we combine approaches, we have to bear in mind the need to leave a skin bridge of at least 6 cm between them, in order to avoid such complications.31 In such a scenario, the stabilisation of the fibular fracture with a rod or titanium elastic nail may be an alternative, although Lee et al32 found a lower rate of malunion and ankle arthrosis when the fibula was fixed by plating.
In complex C3-type fractures with bone loss and comminution in the metaphyseal area, ignoring the fibula fracture allows the option of tibial shortening to improve bone contact and management of the bone defect.
A one-third tubular plate is usually chosen when anatomical reduction can be achieved in fracture patterns with minimal comminution. However, in the presence of severe comminution a more rigid implant is preferred such as a 3.5 mm reconstruction plate or a low-contact dynamic compression plate acting as a bridge plate.
Generally, the post-operative protocol following ORIF includes a posterior splint for two weeks to prevent ankle equinus and to allow for soft-tissue healing, followed by a removable boot and non-weight-bearing for ten to 12 weeks. Free ankle range of motion exercises are permitted once the skin has healed. At ten to 12 weeks post-operatively, progressive weight-bearing is allowed, depending on radiograph results.
External fixation with or without limited ORIF
As a result of the unacceptable complication rates classically linked to early ORIF of pilon fractures in the 1980s,6 alternative management strategies were developed. External fixation was a rational strategy to minimise wound complications and deep infections in selected cases, but C-type fractures with impacted fragments are difficult to reduce by ligamentotaxis alone. The articular incongruence and malunion in those cases led to a compromised outcome due to the development of early post-traumatic arthritis.33 In order to improve the articular reduction that can be obtained with external fixation, it is useful in many cases to perform a limited articular ORIF as an adjunct.34,35 Generally, fractures with metaphyseal comminution and large articular fragments reducible by ligamentotaxis, open fractures with soft-tissue injury that compromises standard approaches and severely contaminated open fractures or patients with comorbidities are scenarios where treatment with an external fixation with or without limited ORIF can be a good option.
Hybrid external fixators are attached to the distal tibial epiphysis through a partial ring with tensioned wires. Proximally, the hybrid fixator is constructed from conventional external fixator components attached to the diaphysis with Schanz screws. The proximal frame attaches to the distal ring with appropriate connecting clamps. A variety of frame configurations have been proposed. Early hybrid fixators for the distal tibia were as simple as a partial ring with two tensioned wires for the epiphyseal region connected to a single rod attached to two diaphyseal Schanz screws. Experienced surgeons now recommend at least two or three pins proximal to the fracture, inserted from different directions with a cross-braced frame, and at least two or three tensioned 2 mm wires in the articular portion. To reduce the risk of joint infection, intra-articular placement of the wires is to be avoided, if possible. Pins that are inserted less than 20 mm proximal to the tibiotalar joint may enter the joint capsule (Fig. 8).
Fig. 8.

Hybrid external fixator.
Several authors (Leung et al35 and Bone et al,36 for example) have reported results using external fixation with limited ORIF that are comparable with previous studies using ORIF alone. A recent meta-analysis by Wang et al37, reaches the same conclusion. Nine studies investigating ORIF and limited internal fixation combined with an external fixator (LIFEF) for the treatment of tibial plafond fractures were included in this meta-analysis. The purpose of the analysis was to determine whether LIFEF yielded fewer post-operative complications when compared with ORIF. The meta-analysis found that rates of nonunion, malunion and delayed union, bone healing, deep and superficial infection, arthritis symptoms and chronic osteomyelitis were comparable between groups.
There is not a single method of fixation ideal for all pilon fractures or suitable for all patients. Definitive decision-making is mostly dependent on the fracture pattern, the condition of the soft-tissues, the patient’s profile and surgical expertise.
Outcomes
Outcomes following high-energy pilon fractures are usually poor when compared with functional outcome scores of the uninjured population. Pollak et al38 studied the mid-term outcomes of pilon fractures managed with either ORIF or external fixation, with or without limited ORIF. Patient scores in the SF-36 General Health Questionnaire were significantly lower than age-matched controls. They demonstrated that 43% of previously working patients were unemployed after suffering the injury and 68% of individuals attributed their situation to sequelae of their fractures. Sands et al39 reported similar outcomes using the same SF-36 score. Another very important finding is that clinical results usually deteriorate with time, and the incidence of post-traumatic arthritis significantly increases over time.40
Conclusions
Anatomical reduction of the fracture, restoration of joint congruency and reconstruction of the posterior column with a correct limb axis and thus minimising soft-tissue insult are the key factors of a positive outcome when treating pilon fractures. Even when these goals are achieved, there is no guarantee that results will be acceptable in the mid-term due to the frequent progression to post-traumatic arthritis.40 No method of treatment has shown clear superiority regarding rates of nonunion, malunion, delayed union, bone healing, deep and superficial infection, arthritis symptoms or chronic osteomyelitis, therefore we can conclude (as Sirkin and Sanders41 proposed) that surgeons should treat these complex fractures with the method with which they are most comfortable. Surgeons who feel comfortable with techniques of internal fixation are best qualified to perform open reductions, while surgeons who have experience with percutaneous fixation and hybrid external fixator application should use this method.
Footnotes
Conflict of Interest: None declared.
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Mandi DM, Belin RP, Banks J, Barrett B. Pilon fractures. Clin Podiatr Med Surg 2012;29:243-278, viii. [DOI] [PubMed] [Google Scholar]
- 2. Crist BD, Khazzam M, Murtha YM, Della Rocca GJ. Pilon fractures: advances in surgical management. J Am Acad Orthop Surg 2011;19:612-622. [DOI] [PubMed] [Google Scholar]
- 3. Teeny SM, Wiss DA. Open reduction and internal fixation of tibial plafond fractures. Variables contributing to poor results and complications. Clin Orthop Relat Res 1993;292:108-117. [PubMed] [Google Scholar]
- 4. Rüedi TP, Allgöwer M. The operative treatment of intra-articular fractures of the lower end of the tibia. Clin Orthop Relat Res 1979;138:105-110. [PubMed] [Google Scholar]
- 5. White TO, Guy P, Cooke CJ, et al. The results of early primary open reduction and internal fixation for treatment of OTA 43.C-type tibial pilon fractures: a cohort study. J Orthop Trauma 2010;24:757-763. [DOI] [PubMed] [Google Scholar]
- 6. McFerran MA, Smith SW, Boulas HJ, Schwartz HS. Complications encountered in the treatment of pilon fractures. J Orthop Trauma 1992;6:195-200. [DOI] [PubMed] [Google Scholar]
- 7. Sirkin M, Sanders R, DiPasquale T, Herscovici D., Jr A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma 1999;13:78-84. [DOI] [PubMed] [Google Scholar]
- 8. Patterson MJ, Cole JD. Two-staged delayed open reduction and internal fixation of severe pilon fractures. J Orthop Trauma 1999;13:85-91. [DOI] [PubMed] [Google Scholar]
- 9. Blauth M, Bastian L, Krettek C, Knop C, Evans S. Surgical options for the treatment of severe tibial pilon fractures: a study of three techniques. J Orthop Trauma 2001;15:153-160. [DOI] [PubMed] [Google Scholar]
- 10. Williams TM, Marsh JL, Nepola JV, et al. External fixation of tibial plafond fractures: is routine plating of the fibula necessary? J Orthop Trauma 1998;12:16-20. [DOI] [PubMed] [Google Scholar]
- 11. Teixidor-Serra J, Alvarez-Ferre S, Tomás-Hernández J, et al. Tibial plafond fractures: retrospective review. J Bone Joint Surg [Br] 2011;93-B(suppl II):217. [Google Scholar]
- 12. Topliss CJ, Jackson M, Atkins RM. Anatomy of pilon fractures of the distal tibia. J Bone Joint Surg [Br] 2005;87-B:692-697. [DOI] [PubMed] [Google Scholar]
- 13. Tornetta P, III, Gorup J. Axial computed tomography of pilon fractures. Clin Orthop Relat Res 1996;323:273-276. [DOI] [PubMed] [Google Scholar]
- 14. Cole PA, Mehrle RK, Bhandari M, Zlowodzki M. The pilon map: fracture lines and comminution zones in OTA/AO type 43C3 pilon fractures. J Orthop Trauma 2013;27:e152-e156. [DOI] [PubMed] [Google Scholar]
- 15. Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma 2007;21(suppl):S1-S133. [DOI] [PubMed] [Google Scholar]
- 16. Swiontkowski MF, Sands AK, Agel J, et al. Interobserver variation in the AO/OTA fracture classification system for pilon fractures: is there a problem? J Orthop Trauma 1997;11:467-470. [DOI] [PubMed] [Google Scholar]
- 17. Calori GM, Tagliabue L, Mazza E, et al. Tibial pilon fractures: which method of treatment? Injury 2010;41:1183-1190. [DOI] [PubMed] [Google Scholar]
- 18. Tarkin IS, Clare MP, Marcantonio A, Pape HC. An update on the management of high-energy pilon fractures. Injury 2008;39:142-154. [DOI] [PubMed] [Google Scholar]
- 19. Stapleton JJ, Zgonis T. Surgical treatment of tibial plafond fractures. Clin Podiatr Med Surg 2014;31:547-564. [DOI] [PubMed] [Google Scholar]
- 20. Borens O, Kloen P, Richmond J, et al. Minimally invasive treatment of pilon fractures with a low profile plate: preliminary results in 17 cases. Arch Orthop Trauma Surg 2009;129:649-659. [DOI] [PubMed] [Google Scholar]
- 21. Borg T, Larsson S, Lindsjö U. Percutaneous plating of distal tibial fractures. Preliminary results in 21 patients. Injury 2004;35:608-614. [DOI] [PubMed] [Google Scholar]
- 22. Collinge C, Kuper M, Larson K, Protzman R. Minimally invasive plating of high-energy metaphyseal distal tibia fractures. J Orthop Trauma 2007;21:355-361. [DOI] [PubMed] [Google Scholar]
- 23. Assal M, Ray A, Stern R. Strategies for surgical approaches in open reduction internal fixation of pilon fractures. J Orthop Trauma 2015;29:69-79. [DOI] [PubMed] [Google Scholar]
- 24. Assal M, Ray A, Stern R. The extensile approach for the operative treatment of high-energy pilon fractures: surgical technique and soft-tissue healing. J Orthop Trauma 2007;21:198-206. [DOI] [PubMed] [Google Scholar]
- 25. Jacob N, Amin A, Giotakis N, et al. Management of high-energy tibial pilon fractures. Strategies Trauma Limb Reconstr 2015;10:137-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Konrath GA, Hopkins G., II Posterolateral approach for tibial pilon fractures: a report of two cases. J Orthop Trauma 1999;13:586-589. [DOI] [PubMed] [Google Scholar]
- 27. Bhattacharyya T, Crichlow R, Gobezie R, Kim E, Vrahas MS. Complications associated with the posterolateral approach for pilon fractures. J Orthop Trauma 2006;20:104-107. [DOI] [PubMed] [Google Scholar]
- 28. Ketz J, Sanders R. Staged posterior tibial plating for the treatment of Orthopaedic Trauma Association 43C2 and 43C3 tibial pilon fractures. J Orthop Trauma 2012;26:341-347. [DOI] [PubMed] [Google Scholar]
- 29. Barei DP, Nork SE, Bellabarba C, Sangeorzan BJ. Is the absence of an ipsilateral fibular fracture predictive of increased radiographic tibial pilon fracture severity? J Orthop Trauma 2006;20:6-10. [DOI] [PubMed] [Google Scholar]
- 30. Rouhani A, Elmi A, Akbari Aghdam H, et al. The role of fibular fixation in the treatment of tibia diaphysis distal third fractures. Orthop Traumatol Surg Res 2012;98:868-872. [DOI] [PubMed] [Google Scholar]
- 31. Howard JL, Agel J, Barei DP, Benirschke SK, Nork SE. A prospective study evaluating incision placement and wound healing for tibial plafond fractures. J Orthop Trauma 2008;22:299-305. [DOI] [PubMed] [Google Scholar]
- 32. Lee Y-S, Chen S-W, Chen S-H, et al. Stabilisation of the fractured fibula plays an important role in the treatment of pilon fractures: a retrospective comparison of fibular fixation methods. Int Orthop 2009;33:695-699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Borrelli J, Jr, Ricci WM. Acute effects of cartilage impact. Clin Orthop Relat Res 2004;423:33-39. [DOI] [PubMed] [Google Scholar]
- 34. Papadokostakis G, Kontakis G, Giannoudis P, Hadjipavlou A. External fixation devices in the treatment of fractures of the tibial plafond: a systematic review of the literature. J Bone Joint Surg [Br] 2008;90-B:1-6. [DOI] [PubMed] [Google Scholar]
- 35. Leung F, Kwok HY, Pun TS, Chow SP. Limited open reduction and Ilizarov external fixation in the treatment of distal tibial fractures. Injury 2004;35:278-283. [DOI] [PubMed] [Google Scholar]
- 36. Bone L, Stegemann P, McNamara K, Seibel R. External fixation of severely comminuted and open tibial pilon fractures. Clin Orthop Relat Res 1993;292:101-107. [PubMed] [Google Scholar]
- 37. Wang D, Xiang J-P, Chen X-H, Zhu Q-T. A meta-analysis for postoperative complications in tibial plafond fracture: open reduction and internal fixation versus limited internal fixation combined with external fixator. J Foot Ankle Surg 2015;54:646-651. [DOI] [PubMed] [Google Scholar]
- 38. Pollak AN, McCarthy ML, Bess RS, Agel J, Swiontkowski MF. Outcomes after treatment of high-energy tibial plafond fractures. J Bone Joint Surg [Am] 2003;85-A:1893-1900. [DOI] [PubMed] [Google Scholar]
- 39. Sands A, Grujic L, Byck DC, et al. Clinical and functional outcomes of internal fixation of displaced pilon fractures. Clin Orthop Relat Res 1998;347:131-137. [PubMed] [Google Scholar]
- 40. Chen SH, Wu PH, Lee YS. Long-term results of pilon fractures. Arch Orthop Trauma Surg 2007;127:55-60. [DOI] [PubMed] [Google Scholar]
- 41. Sirkin M, Sanders R. The treatment of pilon fractures. Orthop Clin North Am 2001;32:91-102. [DOI] [PubMed] [Google Scholar]