Abstract
Patients with unstable, malaligned knees often present a challenging management scenario, and careful attention must be paid to the clinical history and examination to determine the priorities of treatment.
Isolated knee instability treated with ligament reconstruction and isolated knee malalignment treated with periarticular osteotomy have both been well studied in the past. More recently, the effects of high tibial osteotomy on knee instability have been studied.
Lateral closing-wedge high tibial osteotomy tends to reduce the posterior tibial slope, which has a stabilising effect on anterior tibial instability that occurs with ACL deficiency.
Medial opening-wedge high tibial osteotomy tends to increase the posterior tibia slope, which has a stabilising effect in posterior tibial instability that occurs with PCL deficiency.
Overall results from recent studies indicate that there is a role for combined ligament reconstruction and periarticular knee osteotomy.
The use of high tibial osteotomy has been able to extend the indication for ligament reconstruction which, when combined, may ultimately halt the evolution of arthritis and preserve their natural knee joint for a longer period of time.
Cite this article: Robin JG, Neyret P. High tibial osteotomy in knee laxities: Concepts review and results. EFORT Open Rev 2016;1:3-11. doi: 10.1302/2058-5241.1.000001.
Keywords: Knee instability, malalignment, ACL, PCL, high tibial osteotomy, ligament reconstruction
The use of high tibial osteotomy (HTO) in Orthopaedic surgery has been well documented in the literature for many years. In general, this procedure has been performed in the setting of symptomatic unicompartmental arthrosis associated with coronal plane malalignment and in a stable knee.1 The aim is to off-load the symptomatic affected compartment by correcting the coronal deformity present in the tibia and thereby reducing pain and improving function.
HTO techniques for varus malalignment have changed over time. Historically, lateral closing-wedge techniques were mostly performed; however, recently medial opening-wedge osteotomies have become popular.2 Both techniques aim to off-load the affected medial compartment and both have been shown to have satisfactory short- and long-term clinical results.3-13
In contrast with the past where a varus thrust and instability were contra-indications to HTO owing to reported inferior results,14,15 more recently attention has been directed at treating coronal malalignment and associated knee instabilities with HTO with and without ligament reconstruction. Further, there has been more interest shown in sagittal plane deformity of the proximal tibia. In particular the posterior tibial slope (PTS) has received more attention with regard to its importance in sagittal balance of the unstable knee.2
Isolated HTO has been reported in the treatment of acute and chronic anterior cruciate ligament (ACL) instability as well as posterior cruciate ligament (PCL) and posterolateral corner (PLCnr) laxities.15-19 More literature is available regarding the combination of HTO and ligament reconstruction in these clinical scenarios. The short- and medium-term results of these techniques documented in the literature are encouraging and further results are needed on the long-term results when they become available.20-29
There are two categories of patients who may be appropriate for HTO in the setting of knee instability, and it is critical when assessing these patients that a thorough focussed history be undertaken.21 The first clinical scenario is that of a patient with arthritic symptoms in the setting of chronic ligament deficiency and coronal or sagittal deformity. In these patients, the overwhelming history is that of pain, swelling and reduced function. They may also have some giving way or other feature of ligament instability. In these patients, HTO alone is often recommended, nevertheless the results of ligament reconstruction in this group are often disappointing.21 The second patient group mainly has symptoms because of ligament deficiency, together with a proximal tibial deformity, and only slight signs of osteoarthritis (OA) on their radiographs and mild pain. Noyes has described these patients as being some of the most difficult to treat as the patient population consists of young, high-demand individuals. Performing a HTO in these patients extends the indication for ligament reconstruction and joint stabilisation. Hopefully, this might lead to a better long-term outcome but this is yet to be proven.22
Anatomical contributions to knee imbalance
The knee is stabilised by multiple soft-tissue and bony structures. When considering these, it is important to recognise that the knee is stabilised in the frontal (coronal) and sagittal plane by primary and secondary mechanisms. Following ACL rupture, chronic imbalance in these planes is considered a significant contributing factor in the arthritic process.23-24 Plain radiographs are crucial for analysing the pattern and extent of imbalance.
Frontal imbalance
Imbalance in the frontal plane is assessed on bilateral comparative monopodal-stance anteroposterior radiographs. Three patterns of joint space alteration may be observed which relate to the anatomical factors involved in the imbalance: isolated medial tibio-femoral compartment narrowing, asymmetric lateral compartment opening and combined medial narrowing with lateral compartment opening.
Four main factors in frontal imbalance contribute to altered transmission of forces across the knee:
ACL rupture: following ACL rupture, there is increased medial rotation of the tibia, which leads to displacement of the instantaneous centre of rotation of the knee toward the medial compartment.
Medial meniscus injury: the role of the medial meniscus in preventing OA is well documented. Medial meniscectomy alone or in combination with ACL deficiency has been shown to have degenerative changes in 77% of knees at long-term follow-up.30 At the time of ACL reconstruction, if there was an associated partial meniscectomy, the risk of OA reaches 30%. When there has been a total meniscectomy, the risk of OA reaches 60%.30
PLCnr: PLCnr lesions occur at the time of initial knee injury, rather than occurring as a chronic “stretching out” phenomenon.24 These structures, of which the lateral collateral ligament is the most important, are crucial in controlling frontal balance. In particular, they prevent excessive tibio-femoral external rotation and varus opening at the tibio-femoral joint. Combined ACL and PLCnr injury leads to asymmetrical lateral compartment opening seen on radiographs. This is present in 5% of cases.24
Constitutional varus deformity: there is an increase in medial compartment forces seen when there is a constitutionally varus knee. Most commonly this results from proximal tibia vara; however, this deformity may also arise from the femur or even from both. This deformity acts as a potential factor in the arthritic process, and favours the development of OA in an ACL-deficient knee when the bony deformity is > 6° to 8°.
Sagittal imbalance
Three factors contribute to sagittal imbalance, and they are assessed on comparative bilateral monopodal-stance lateral radiographs performed at 30° of flexion. These factors are:
ACL: the ACL is key to limiting anterior tibial translation (ATT). After ACL rupture, significant increase in ATT only occurs after loading the knee. In the absence of external forces, the kinematics of a knee with and without ACL deficiency are similar.24 In the presence of ACL deficiency and passive or active external forces, an ATT of 2 mm or more is considered pathological.30
Medial meniscus injury: the medial meniscus, in particular the posterior horn, acts as a brake to control ATT. Secondary medial meniscal injuries are common following ACL rupture. It has been shown that in 70% of cases there will be either a medial meniscus tear or a posteromedial corner disruption when (using the described radiographic technique) there is a differential ATT of 6 mm or more. When the differential is > 10 mm, these abnormalities are seen in > 90% of cases.31
Posterior tibial slope: the association of coronal plane deformity and ligament insufficiency is well described in the literature and deformity in the sagittal plane has recently been given more significance.2,24
The PTS has been defined in multiple different ways because of inconsistency of the anatomical landmarks being used. The most common measurement is taken from plain radiographs as the angle subtended by a line parallel to the mid-diaphysis of the tibia and a line parallel to the posterior inclination of the tibial plateau. This angle refers to the osseous PTS. Medially, this value is between 9° to 11° and laterally 6° to 8° with a large amount of variation.2 It has been considered excessive when the PTS is > 13°.24 The soft-tissue PTS depends on the integrity of the menisci and chondral surfaces. When these are intact the posterior slope is relatively reduced owing to the posterior horn of the menisci being higher than the anterior horn.32
The effects of exaggerated deformity of the posterior slope have been associated with knee instability in multiple ways. It has been shown radiographically that with an increase in PTS, there is an increase in ATT both in the setting of ACL deficiency and ACL-intact knees.33 This relationship has been shown to be linear. That is, with an increase in posterior tibial slope, there is a linear increase in anterior tibial translation in monopodal stance.34
Various authors have also confirmed this to be the case in cadaveric studies. In these reports, an anterior tibial osteotomy was performed to exaggerate the PTS and the knees were then subjected to axial forces to study tibial translation, joint kinematics, and forces applied to the cruciate ligaments.
In a series of studies, Giffin et al have demonstrated that small degrees of increase in PTS in ligamentously-intact knees increase the anterior tibial resting position, which is further accentuated under compressive loads. The change in slope did not affect the anteroposterior translation or the in situ forces on the cruciate ligaments.2 When the PCL was sacrificed, a posterior tibial sag was produced. Following a 5 mm anterior opening-wedge tibial osteotomy to the increase in tibial slope, the sag reduced significantly throughout the range of movement. Load applied to the knee exaggerated the ATT further. This led the authors to conclude that increasing the posterior tibial slope may be able to stabilise the knee in PCL deficiency.2 Other cadaveric studies have confirmed Giffin’s findings; however, there is controversy as to whether changing the PTS has an effect on tension on the cruciate ligaments and the surrounding secondary stabilisers.35
Voos et al performed a cadaveric study and examined ATT, the Lachman test and pivot-shift test after sectioning the ACL and altering the tibial slope. The main finding was that following ACL sectioning and increasing the tibial slope with a medial opening-wedge HTO, there was no difference in ATT and Lachman test; however, there was a significant increase in the pivot-shift test.36 Similar results have also been reported in a clinical study where patients who were ACL deficient had significantly greater pivot-shift grades when they had a greater tibial slope.37
Due to the triangular three-dimensional shape of the proximal tibia, HTOs addressing coronal deformities also have a predictable effect in the sagittal plane.38 Medial opening-wedge HTO has the tendency to increase the PTS. Attention to detail must be observed during this operation to ensure that the sagittal alignment will be maintained and the slope will not be increased. As small a change in the gap heights of 1 mm has the ability to change the posterior slope by 2°.38 Adherence to surgical technique and correct placement of fixation devices ensures that significant sagittal plane alterations do not occur unnecessarily. Purposefully increasing the posterior slope with a medial opening-wedge HTO may be beneficial in the setting of PCL deficiency. Conversely, lateral closing-wedge HTOs have the effect of reducing the posterior slope. This may be beneficial in the setting of an ACL-deficient knee.
Significance of knee instability and imbalance
Instability in the sagittal plane, particularly with ACL insufficiency, significantly alters the knee biomechanics. An alteration in sagittal plane kinematics leads to abnormal loading of the posteromedial aspect of the tibial articular cartilage. In chronic ACL deficiency with anterior tibial subluxation a cupula is often formed posteromedially. Further, damage to the posterior horn of the medial meniscus is more likely to occur, losing its stabilising effect and relatively increasing the mechanical PTS. This in turn worsens the ATT and the cycle continues until there is advanced secondary OA of the medial compartment.
Clinical assessment
The most critical feature of assessing patients with malalignment and instability is to understand their primary complaint. This may be difficult as the symptoms of acute or chronic instability include pain, swelling, giving way and actual mechanical instability. The age of the patient, their degree of activity and the degree and type of instability all play an important role in decision-making. What is of utmost importance is the significance the instability plays in that patient’s life. For instance, some patients find that their knee is unstable with regular activities of daily living or walking on uneven ground. Others will only report instability while performing high intensity pivoting sports. The type of instability is also vital to understand. The patient may relate their instability symptoms to a frontal (coronal) plane thrust when walking or a “back-knee” type gait. It may also be the pivoting type symptom in the setting of cruciate ligament deficiency or even a combination of these problems. Above all, the clinician must be able to decide from the history whether pain relating to arthritis is the predominant problem for the patient, as the treatment may well be different in this setting.
The clinical presentation of a patient with ligament deficiency and malalignment often falls into two main clinical groups. These two different groups have been identified as their treatment differs. The first group mainly present with pain and a small element of instability. They usually are around 40 years old and have chronic ACL deficiency, varus malalignment and advanced medial compartment arthritis.21 The focus for these patients is to alleviate pain relating to the arthritis and a HTO alone often produces satisfactory results.20,21 The second group present with instability as the overwhelming complaint and may or may not have a small amount of medial knee pain. These patients are usually younger and have acute or chronic ACL deficiency and medial unicompartmental pre-OA detected on radiographs. In these patients, by performing a valgus HTO, the indication for ACL reconstruction can be extended.22-23 In these patients it is also critical to clinically assess and analyse radiographs carefully to detect concomitant lateral or posterolateral corner injury. When there is medial compartment narrowing combined with lateral opening visualised on radiographs (in 5% of cases), lateral reconstruction plus ACL reconstruction must be combined to ensure an excessive HTO correction is not undertaken.
A thorough clinical examination is essential. Particular attention must be given to coronal and sagittal standing alignment and signs of varus/valgus or recurvatum thrusts during gait. The presence of an effusion may relate to arthrosis, chondral or meniscal injury. Localised joint line pain on palpation may relate to arthritis or a meniscal tear. An accurate assessment of range of movement may indicate whether there is genu recurvatum and any fixed deformities may indicate the stage of arthritis. Identifying crepitus may be a sign of early chondral damage in a particular compartment. Careful examination of knee stability will be able to identify which ligament or combination of ligaments (especially the lateral collateral and posterolateral corner) has been injured. Further, the degree and correctibility of tibiofemoral subluxation must be sought. Both knees should be examined together to check for symmetry.
Investigation with a full set of radiographs will aid diagnosis and planning of surgery. Comparative bilateral monopodal-stance radiographs are essential to detect the factors contributing to the knee imbalance and therefore which factors can be addressed surgically. Standard anteroposterior, lateral and Schuss views should also be obtained. Full-length alignment x-rays will enable an assessment of malalignment to be made in comparison with the contralateral limb. Stress radiographs in the coronal and sagittal plane document the degree of tibiofemoral subluxation and reducibility (Fig 1).
Fig. 1.
Stress views for posterior instability; a) photograph showing patient set-up and b) radiograph performed according to the John Bartlett Method.
Surgical treatment
In deciding on a surgical plan for patients with knee instability and malalignment, two major principles must be kept in mind:
Correcting alignment is critical and often the first step in management.
Soft-tissue reconstruction alone in the setting of malalignment is likely to fail over time.2
A tailored algorithm must be created for the individual patient based on their assessment; however, the two broad treatment categories are performing a HTO alone, or in combination with concomitant or delayed ligament reconstruction.
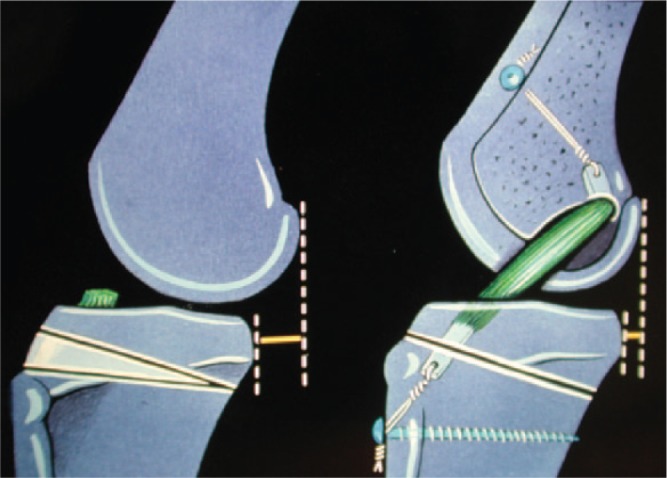
The decision to perform a HTO alone or in combination with ligament reconstruction is guided by a combination of symptoms, patient demographics and which ligaments are involved. In the setting of a patient with medial unicompartmental pain related to arthritis, varus malalignment and chronic ACL deficiency, a biplanar medial opening- (or lateral closing-) wedge HTO alone may be enough to improve pain and stability. A correction of the posterior slope to neutral may be able to reduce any ATT and reduce the instability symptoms related to the ACL deficiency. Where instability is the overriding symptom in the setting of varus malalignment or pre-OA, an ACL reconstruction in combination of HTO may be performed to protect the ACL graft and slow the progression of any arthritis (Fig. 2). Where there is clinical and radiographic evidence of concomitant PLCnr deficiency, it is critical to address this as well as the ACL reconstruction in order to reduce the degree of correction required from the HTO. A combined HTO and lateral ligament or PLCnr reconstruction may also be necessary to improve symptoms (Fig. 3).26
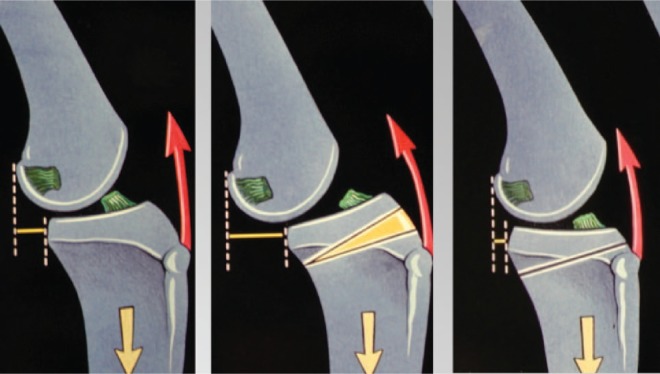
Fig. 2.
Schematic diagram illustrating a combined lateral closing-wedge HTO plus ACL reconstruction. The arrows and line represent the weight-bearing mechanical axis being transferred from the medial to lateral compartment following osteotomy.
Fig. 3.

Schematic diagram illustrating a combined medial opening-wedge HTO, ACL reconstruction and lateral collateral ligament reconstruction. The arrows represent lateral collateral ligament insufficiency.
In the setting of bicruciate ligament injury, the posterior tibial slope may also need to be addressed in combination with ACL and PCL reconstruction. In order to protect both ACL and PCL grafts, it is ideal to maintain neutrality of the posterior tibial slope and correct any coronal plane deformity.
Results in the literature
Isolated HTO for the unstable knee
The literature is scarce on studies regarding osteotomy alone to treat symptomatic ACL deficiency in the setting of varus malalignment. Currently, isolated HTO (including isolated slope-reducing extension osteotomy) for the treatment of pure ACL instability is not an established therapeutic option19 (Fig. 4). Three studies have reported generally good outcomes in small patient cohorts who all had an element of pain owing to degenerative change. In all of these studies, HTO alone was performed primarily because of arthritic pain in the setting of ACL deficiency.
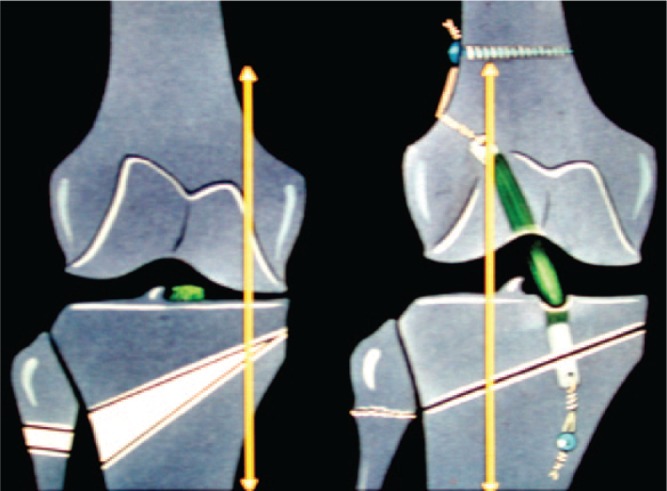
Fig. 4.
Schematic diagram illustrating an anterior closing-wedge HTO to reduce the posterior tibial slope in the setting of ACL deficiency. The red arrows represent the function of the extensor mechanism of the knee in the setting of ACL deficiency. When the tibial slope is increased there is an exaggeration of the effect of ACL deficiency. When the slope is reduced with an osteotomy this effect is also reduced.
Fowler reported on short-term follow-up of seven patients who underwent lateral closing-wedge HTO alone. All seven patients recorded improvements in three subjective areas (pain change, instability and overall function) using a ten-point Likert scale. He concluded that the procedure was successful to treat patients with chronic ACL deficiency and medial joint degeneration who complain of pain and instability on day-to-day activities.16 Lattermann and Jacob reported on three groups of patients, one of which had a lateral closing-wedge HTO for pain on light daily activities with infrequent instability. Ten out of 11 patients reported great improvement in pain relief and no progression of instability. Only three out of 11 patients had a side-to-side difference of > 5 mm on Lachman testing.21 Noyes also reported on three groups of patients who underwent lateral closing-wedge HTO alone or in combination with extra-articular tenodesis or ACL reconstruction for varus malalignment and chronic ACL deficiency.20 The HTO alone group recorded overall patient rating scores equivalent to those of the HTO plus ACL reconstruction group.
Historically, posterior instability in the setting of mechanical malalignment treated with ligament reconstruction alone yielded poor results.2 In contrast to ACL related instability however, isolated HTO is now an accepted therapeutic option for posterior and posterolateral instability combined with genu recurvatum and/or varus deformity19 (Fig. 5). Naudie reported on 16 patients who had either isolated PCL injury, combined PCL and PLCnr injury or posterior capsular injury with an opening-wedge HTO.15 The PTS was increased to a mean of 8° and the mechanical leg alignment was changed to a mean of 6° valgus. All patients reported that knee stability had improved post-operatively and all were satisfied, except one. It must be recognised, however, that five patients subsequently had delayed PCL reconstruction to further improve stability. Arthur studied isolated PLCnr injuries in 21 patients who underwent an initial opening-wedge HTO and were assessed prospectively for a mean of 37 months.18 In eight of the 21 patients (38%), HTO alone was sufficient to control instability and avoid the need for a PLCnr reconstruction. Importantly, most of those who subsequently did require a ligament reconstruction had a history of high velocity knee injury or multi-ligament knee injury. In total 67% of patients with an isolated PLCnr injury did not require ligament reconstruction. In a smaller sized study, Badhe and Forster reported on 14 patients who had a HTO alone or in combination for ligamentous knee injuries. Only three underwent an isolated HTO for PLCnr injuries with two having good results and one a fair result.17
Fig. 5.
Schematic diagram illustrating an anterior opening-wedge HTO to increase the posterior tibial slope in the setting of genu recurvatum relating to a reverse posterior tibial slope. The arrow (left side) represents the reverse slope on the tibia. The arrow (right side) symbolises the creation of an opening-wedge osteotomy.
HTO plus ligament reconstruction for the unstable knee
In the last decade, relatively more has been reported in the literature regarding HTO combined with ligament reconstruction for both ACL and PCL deficiency compared with HTO as a solitary procedure. Multiple techniques for HTO and ligament reconstruction have been described and the timing of the procedures differs between studies. Nevertheless, most of these reports generally have positive outcomes.
Noyes et al analysed the gait in patients with ACL-deficient, varus angulated knees and suggested that in order to reduce the likely ongoing medial compartment degeneration, HTO should be the first treatment in these patients, followed by ACL reconstruction.20 In a two-to-seven year follow-up study, they reported the results of 41 patients who had a varus malaligment and chronic ACL deficiency. A total of 14 of these patients had concomitant extra-articular lateral tenodesis with lateral closing-wedge HTO, while 16 had either a simultaneous or delayed ACL reconstruction following the same type of HTO. Those patients having a HTO and ACL reconstruction showed better overall rating scores and objective stability testing than those with the tenodesis and HTO. Following ACL reconstruction and HTO fewer patients returned to sporting activities, however these results were not statistically tested. They stressed the importance of preserving the proximal tibiofibular joint during HTO, to prevent proximal fibular migration and exaggerating the posterolateral laxity.
Dejour et al reported on short-term results of lateral closing-wedge HTO combined with ACL reconstruction in the ACL-deficient varus knee23 (Fig. 2). The same cohort was examined for longer-term results at a mean of 12 years post-surgery22. Initially, 44 knees were followed up for a mean of 3.5 years. The combined operation was shown to improve clinical symptoms, and clinical and functional stability. Pre-operatively, 31 patients did not play sport despite being very active before ACL injury. Post-operatively, only one patient could play competitive sport; however, another 26 could engage in leisure sports. There was no progression of arthritis radiographically and 91% of patients were satisfied or very satisfied with their result. At a mean follow-up of 12 years, 30 knees were available for assessment. In all, 47% of patients returned to intensive sports and 37% played moderate sports. Five knees (17%) had progressed only one arthritis grade radiographically. The authors concluded that this procedure controls anterior laxity, allowed return to sports, does not lead to rapid arthritic progression and had low morbidity.
In a separate study, Neyret et al described a combined ACL reconstruction and extension HTO to treat patients with symptomatic ACL deficiency and pre-OA who had an increased PTS24 (Fig. 6). The reduction in slope was thought to protect the ACL graft. The preliminary results of this procedure were reported in another study,27 and found that the combination of ACL reconstruction and extension HTO was better than extension HTO alone. The same authors also perform the converse operation for PCL deficiency with reduced tibial slope. In this operation a flexion osteotomy is combined with PCL reconstruction.
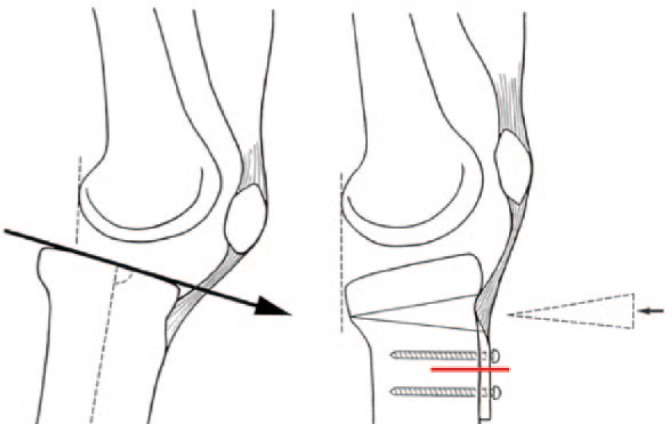
Fig. 6.
Schematic diagram illustrating a combined anterior closing-wedge HTO plus ACL reconstruction.
In total, 41 young patients with ACL deficiency and varus lower-limb alignment were studied prospectively by Noyes et al.26 A total of 34 of these patients had a HTO followed by ACL reconstruction (mean eight months later). Follow-up at a mean of 4.5 years showed that symptomatic giving way was eliminated in 85%, 71% had a reduction in pain, and 66% were able to resume light recreational activities. Although the radiographic analysis showed the majority of the knees to be well aligned, no mention was made of any degenerative change.
Medium-term results of 32 patients who had combined “over the top” ACL reconstruction, extra-articular lateral-plasty and closing-wedge HTO were reported by Zaffagnini et al at a mean of 6.5 years post-surgery.28 Improvements were seen in global objective IKDC scores with 88% of patients graded as IKDC A or B compared with 3% pre-operatively. KT-1000 testing showed a reduction in anterior tibial displacement with a mean side-to-side difference of 2.2 mm. Despite these improvements, there was progression of medial arthritis in 22% of patients. The authors believe this may be due to the older age group of their study population with a pre-operative mean age of 40 years.28
Another study of very similar design looked at 29 patients with a mean age of 43 years who had early medial arthritis, ACL deficiency and varus malalignment.29 They were followed up at a mean of six years following medial opening-wedge HTO in combination with ACL reconstruction (hamstring autograft in 17 and bone-patella tendon-bone autograft in 12). They were at a mean of 14 years post-initial injury. In total 79% of patients had returned to sport, with 45% engaging in competitive sports. In all, 97% were free of instability and 72% were free of pain. Similar IKDC objective scores to that of Zaffagnini et al were recorded with 70% recording A or B global objective IKDC scores, however there was no evidence of radiographic progression of arthritis according to IKDC grade.
Combined HTO, PCL and PLCnr procedures for posterior instability and varus malalignment have also been studied. One study has shown that good results are achievable when performing a combined HTO and PLCnr/PCL reconstruction.17 Though the study population was small (six patients out of a cohort of 14), improved Cincinnati knee scores (CKS) were recorded compared with their pre-operative state. The best scores were found when medial opening-wedge HTO was performed in combination with ligament reconstruction as compared with lateral closing-wedge HTO and ligament reconstruction.
Another study showed that in patients with a lower energy injury, a combined HTO and ligament procedure may be unnecessary.18 In patients who had a higher energy injury (motor vehicle accident or multi-ligament injury), improved CKS were not seen with HTO alone and they subsequently required delayed ligament reconstruction. Disappointingly, these patients were not followed up to determine whether their results improved post-ligament reconstruction. Despite this, other authors have subsequently agreed that an initial isolated HTO followed by a period of observation may be the best option in patients with chronic posterolateral ligament deficiency.35
Reported surgical complications
The overall reported incidence of complications during combined HTO and ligament reconstruction is low. One study did report a higher than expected incidence of complications, especially when compared with performing HTO in isolation.21
The commonly-recorded complications tend to be those general complications observed from Orthopaedic lower-limb procedures such as deep venous thrombosis, superficial wound infection and haematoma. The complications relating specifically to this type of surgery were relatively uncommon. There are few reports in the literature of non-union requiring repeat osteotomy and bone grafting, common peroneal nerve palsy, knee stiffness, patella baja and intra-articular fracture. The most common reported specific complication was that of over or under correction of the osteotomy requiring revision surgery. Overall, HTO in isolation and when combined with ligament reconstruction (either simultaneous or delayed) was shown to have low morbidity.22
Conclusions
In conclusion, patients with unstable malaligned knees prove to be some of the most challenging patients for Orthopaedic surgeons. It is well reported in the literature that managing isolated knee instability with ligament reconstruction and isolated malaligned knees with HTO provides good medium- to long-term results. In the last two decades, however, advances have been made into studying the effects of HTO on knee stability, especially the effect on the posterior tibial slope on sagittal stability. Biomechanically, a lateral closing-wedge HTO has the propensity to decrease the PTS, which has a stabilising effect on anterior instability. This effect may be useful in combined ACL reconstruction and HTO for a varus, ACL-deficient knee. When using a medial opening-wedge HTO technique for the same clinical problem, careful attention must be paid such that the tibial slope is not increased. Conversely a medial opening-wedge HTO tends to increase the posterior tibial slope and may be more useful in stabilising a varus PCL-deficient knee. Historically, owing to the relatively uncommon presentation of the unstable malaligned knee, most studies reported in the literature have small cohorts of varying demographics and injuries. This makes comparison of results difficult to interpret. However, it is evident from the increasing number of studies in the literature that this presentation is either becoming more problematic in the community or that it is being recognised as such. Currently, isolated HTO for ACL related instability is not supported in the literature. Conversely, ligament reconstruction in combination with HTO has provided very satisfactory results in most studies. High tibial osteotomy has been able to potentially avoid difficult posterolateral soft-tissue reconstruction in certain cohorts, whereas this is not the case in others where a combined ACL and PLCnr reconstruction may be necessary to avoid extreme HTO corrections. HTO has also been able to extend the indication for ACL reconstruction which, when combined, may ultimately halt the evolution of arthritis and preserve their natural knee joint for a longer period of time.
Footnotes
Conflict of Interest: None declared.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1. Lustig S, Scholes CJ, Costa AJ, Coolican MJ, Parker DA. Different changes in slope between the medial and lateral tibial plateau after open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 2013;21:32-38. [DOI] [PubMed] [Google Scholar]
- 2. Giffin JR, Shannon FJ. The role of the high tibial osteotomy in the unstable knee. Sports Med Arthrosc 2007;15:23-31. [DOI] [PubMed] [Google Scholar]
- 3. Coventry MB. Osteotomy about the knee for degenerative and rheumatoid arthritis. J Bone Joint Surg [Am] 1973;55-A:23-48. [PubMed] [Google Scholar]
- 4. Coventry MB. Upper tibial osteotomy for gonarthrosis. The evolution of the operation in the last 18 years and long term results. Orthop Clin North Am 1979;10:191-210. [PubMed] [Google Scholar]
- 5. Fujisawa Y, Masuhara K, Shiomi S. The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am 1979;10:585-608. [PubMed] [Google Scholar]
- 6. Naudie D, Bourne RB, Rorabeck CH, Bourne TJ. The Install Award. Survivorship of the high tibial valgus osteotomy. A 10- to -22-year followup study. Clin Orthop Relat Res 1999;367:18-27. [PubMed] [Google Scholar]
- 7. Aglietti P, Rinonapoli E, Stringa G, Taviani A. Tibial osteotomy for the varus osteoarthritic knee. Clin Orthop Relat Res 1983;176:239-251. [PubMed] [Google Scholar]
- 8. Bauer GC, Insall J, Koshino T. Tibial osteotomy in gonarthrosis (osteo-arthritis of the knee). J Bone Joint Surg [Am] 1969;51-A:1545-1563. [PubMed] [Google Scholar]
- 9. Broughton NS, Newman JH, Baily RA. Unicompartmental replacement and high tibial osteotomy for osteoarthritis of the knee. A comparative study after 5-10 years’ follow-up. J Bone Joint Surg [Br] 1986;68-B:447-452. [DOI] [PubMed] [Google Scholar]
- 10. Cass JR, Bryan RS. High tibial osteotomy. Clin Orthop Relat Res 1988;230:196-199. [PubMed] [Google Scholar]
- 11. Insall J, Shoji H, Mayer V. High tibial osteotomy. A five-year evaluation. J Bone Joint Surg [Am] 1974;56-A:1397-1405. [PubMed] [Google Scholar]
- 12. Insall JN, Joseph DM, Msika C. High tibial osteotomy for varus gonarthrosis. A long-term follow-up study. J Bone Joint Surg [Am] 1984;66-A:1040-1048. [PubMed] [Google Scholar]
- 13. Ivarsson I, Myrnerts R, Gillquist J. High tibial osteotomy for me- dial arthritis of the knee. A 5 to 7 and an 11 to 13 year follow-up. J Bone Joint Surg [Br] 1990;72-B:238-244. [DOI] [PubMed] [Google Scholar]
- 14. Coventry MB. Osteotomy of the upper portion of the tibia for degenerative arthritis of the knee. A preliminary report. J Bone Joint Surg [Am] 1965;47-A:984-990. [PubMed] [Google Scholar]
- 15. Naudie DD, Amendola A, Fowler PJ. Opening wedge high tibial osteotomy for symptomatic hyperextension-varus thrust. Am J Sports Med 2004;32:60-70. [DOI] [PubMed] [Google Scholar]
- 16. Fowler PJ, Kirkley A, Roe J. Osteotomy of the proximal tibia in the treatment of chronic anterior cruciate ligament insufficiency. J Bone Joint Surg [Br] 2002;84-B(SUPP III):353. [Google Scholar]
- 17. Badhe NP, Forster IW. High tibial osteotomy in knee instability: the rationale of treatment and early results. Knee Surg Sports Traumatol Arthrosc 2002;10:38-43. [DOI] [PubMed] [Google Scholar]
- 18. Arthur A, LaPrade RF, Agel J. Proximal tibial opening wedge osteotomy as the initial treatment for chronic posterolateral corner deficiency in the varus knee. A prospective clinical study. Am J Sports Med 2007;35:1844-1850. [DOI] [PubMed] [Google Scholar]
- 19. Feucht MJ, Mauro CS, Brucker PU, Imhoff AB, Hinterwimmer S. The role of the tibial slope in sustaining and treating anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc 2013;21:134-145. [DOI] [PubMed] [Google Scholar]
- 20. Noyes FR, Barber SD, Simon R. High tibial osteotomy and ligament reconstruction in varus angulated, anterior cruciate ligament-deficient knees. A two- to seven-year follow-up study. Am J Sports Med 1993;21:2-12. [DOI] [PubMed] [Google Scholar]
- 21. Lattermann C, Jakob RP. High tibial osteotomy alone or combined with ligament reconstruction in anterior cruciate ligament-deficient knees. Knee Surg Sports Traumatol Arthrosc 1996;4:32-38. [DOI] [PubMed] [Google Scholar]
- 22. Bonin N, Ait Si, Selmi T, Donell ST, Dejour H, Neyret P. Anterior cruciate reconstruction combined with valgus upper tibial osteotomy: 12 years follow-up. Knee 2004;11:431-437. [DOI] [PubMed] [Google Scholar]
- 23. Dejour H, Neyret P, Bonnin M. Instability and osteoarthritis. In: Fu FH, Harner CD, Vince KG, eds. Knee Surgery. Baltimore, Maryland: Lippincott Williams & Wilkins, 1994:859-875. [Google Scholar]
- 24. Neyret P, Zuppi G, Ait Si, Selmi T. Tibial deflexion osteotomy. Oper Tech Sports Med 2000;8:61-66. [Google Scholar]
- 25. Lipke JM, Janekic J, Nelson CI, et al. The role of incompetence of the anterior cruciate and lateral ligaments in antero-lateral instability. J Bone Joint Surg [Am] 1981;63-A:954-960. [PubMed] [Google Scholar]
- 26. Noyes FR, Barber-Westin SD, Hewett TE. High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med 2000;28:282-296. [DOI] [PubMed] [Google Scholar]
- 27. Dejour D, Khun A, Dejour H. Osteotomie tibiale de déflexion et laxité chronique antérieure à propos de 22 cas. Rev Chir Orthop Repar Appar Mot 1998;84:28-29. [Google Scholar]
- 28. Zaffagnini S, Bonanzinga T, Grassi A, et al. Combined ACL reconstruction and closing-wedge HTO for varus angulated ACL-deficient knees. Knee Surg Sports Traumatol Arthrosc 2013;21:934-941. [DOI] [PubMed] [Google Scholar]
- 29. Trojani C, Elhor H, Carles M, Boileau P. Anterior cruciate ligament reconstruction combined with valgus high tibial osteotomy allows return to sports. Orthop Traumatol Surg Res 2014;100:209-212. [DOI] [PubMed] [Google Scholar]
- 30. Neyret P, Donell S, Dejour D, DeJour H. Partial meniscectomy and anterior cruciate ligament rupture in soccer players. Am J Sports Med 1993;21:455-460. [DOI] [PubMed] [Google Scholar]
- 31. Neyret P, Ait Si Selmi T, Pires LG. Arthrose et laxité. Paris, France: Conférence d’Enseignement, Société Française d’Arthoscopie, 1998. [Google Scholar]
- 32. Agneskirchner JD, Hurschler C, Stukenborg-Colsman Imhoff AB, Lobenhoffer P. Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a biomechanical study in human cadaveric knees. Winner of the AGA-DonJoy Award 2004. Arch Orthop Trauma Surg 2004;124:575-584. [DOI] [PubMed] [Google Scholar]
- 33. Bonnin M. La Subluxation Tibiale Anterieure en Appui Mono- podal. In: Les Ruptures du Ligament Croise Anteriieur: Etude Clinique et Biomechanique. Lyon, France: Universite Claude Bernard, 1990.[[bibmisc]] [Google Scholar]
- 34. Dejour D, Bonin N, Locatelli E. Tibial anticurvatum osteotomies. Oper Tech Sports Med 2000;8:67-70. [Google Scholar]
- 35. Savarese E, Bisicchia S, Romeo R, Amendola A. Role of high tibial osteotomy in chronic injuries of posterior cruciate ligament and posterolateral corner. J Orthop Traumatol 2011;12:1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Voos JE, Suero EM, Citak M, et al. Effect of tibial slope on the stability of the anterior cruciate ligament-deficient knee. Knee Surg Sports Traumatol Arthrosc 2012;20:1626-1631. [DOI] [PubMed] [Google Scholar]
- 37. Brandon ML, Haynes PT, Bonamo JR, et al. The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy 2006;22:894-899. [DOI] [PubMed] [Google Scholar]
- 38. Noyes FR, Goebel SX, West J. Opening wedge tibial osteotomy: the 3-triangle method to correct axial alignment and tibial slope. Am J Sports Med 2005;33:378-387. [DOI] [PubMed] [Google Scholar]