Abstract
Introduction
Stillbirth is a significant public health problem in low-to-middle-income countries and results in perinatal grief, often with negative psychosocial impact. In low-resource settings, such as Chhattisgarh, India, where needs are high, it is imperative to utilize low-cost, effective interventions. Mindfulness-based stress reduction (MBSR) is an empirically sound intervention that has been utilized for a broad range of physical and mental health problems, and is adaptable to specific populations. The main objective of this pilot study was to explore the feasibility and effectiveness of a shortened, culturally adapted mindfulness-based intervention to address complex grief after stillbirth.
Methods
We used an observational, pre-post-6-week post study design. The study instrument was made up of descriptive demographic questions and validated scales and was administered as a structured interview due to low literacy rates. We used a community participatory approach to culturally adapt the five-week mindfulness-based intervention and delivered it through two trained local nurses. Quantitative and qualitative data analyses explored study outcomes as well as acceptability and feasibility of the intervention.
Results
29 women with a history of stillbirth enrolled, completed the pretest and began the intervention; 26 completed the five-week intervention and post-test (89.7%), and 23 completed the six-week follow-up assessment (88.5%). Pretest results included elevated psychological symptoms and high levels of perinatal grief, including the active grief, difficulty coping, and despair subscales. General linear modeling repeated measures was used to explore posttest and six-week follow up changes from baseline, controlling for significantly correlated demographic variables. These longitudinal results included significant reduction in psychological symptoms; four of the five facets of mindfulness changed in the desired direction, two significantly; as well as significant reduction in overall perinatal grief and on each of the three subscales.
Discussion
The shortened, culturally adapted, mindfulness-based intervention pilot study was well received and had very low attrition. We also found significant reductions of perinatal grief and mental health symptoms over time, as well as a high degree of practice of mindfulness skills by participants. This study not only sheds light on the tremendous mental health needs among rural women of various castes who have experienced stillbirth in Chhattisgarh, it also points to a promising effective intervention with potential to be taken to scale for wider delivery.
Keywords: Perinatal grief, mental health, stillbirth, India, mindfulness-based intervention
Stillbirth rates are highest in low-resource settings, particularly in low to middle income countries, including India. In fact, 98% of the global stillbirth burden occurs in these countries, yet remains largely an unrecognized, preventable issue that has not been adequately addressed. In these settings, stillbirth most often occurs at the point of delivery (Bhutta & Black, 2013; McClure, Saleem, et al., 2015). It is a unique and particularly devastating grief when the anticipation of birth is met instead by crushing loss and death. It creates a unique grief that is long-lasting and complicated (Kelly, 2007; Lang et al., 2011; Mehta & Verma, 1990). It is therefore no surprise that the psychosocial sequela of stillbirth includes intense grief, anxiety and depression, and significant social impact (Boyle, Vance, Najman, & Thearle, 1996; Roberts, Anderson, Lee, & Montgomery, 2012; Sather, Fajon, Zaentz, & Rubens, 2010).
In developing countries, women’s roles are often defined by fertility and is tantamount to their worth (Fottrell et al., 2010; Pandalangat, 2006). Women in rural India are not exempt from this traditional, patriarchal view, and added to that, is ubiquitous son-preference (Roberts, Anderson, et al., 2012). Therefore, women who have a history of stillbirth not only suffer the inherent grief unique to that experience, they also suffer loss of social value (Fottrell et al., 2010; Inhorn, 2003). This combined grief and humiliation is borne in silence, as these women are strongly discouraged from talking about the experience (Roberts, Anderson, et al., 2012). Women, in the context of social norms including gender discrimination and the caste system (Bidner & Eswaran, 2015; Branisa, Klasen, Ziegler, Drechsler, & Jütting, 2014; Patel, Rodrigues, & DeSouza, 2002) may be particularly vulnerable. The caste system in India is a formal designation of social status of Hindu people groups (Mandal, 2005). The caste system includes high castes, scheduled castes and tribes, and other castes. Scheduled castes and tribes are considered low castes, oppressed people groups at great social disadvantage, who are marginalized and suffer even more significant health disparities than are present in a developing country (Balarajan, Selvaraj, & Subramanian, 2011; Thomas et al., 2015).
When resources are limited and needs are high, it is even more critical to utilize interventions that are not only culturally aligned, and low cost, but also based on evidence assuring a strong probability of the results that one intends to affect. Mindfulness-based stress reduction (MBSR) is an evidence-based intervention that has been utilized for a broad range of physical and psychological health problems (Davis & Hayes, 2011; Farb et al., 2010; Grossman, Niemann, Schmidt, & Walach, 2004; Ludwig & Kabat-Zinn, 2008). MBSR is a formal, manualized 8-week intervention which teaches the five facets of mindfulness: observing, describing, acting with awareness, a non-judging of inner experiences, and non-reacting to inner experiences. Mindfulness skills can be learned and cultivated to achieve mindfulness as a state of being—to be in the present moment and aware of one’s experience without judgment (Davis & Hayes, 2011). Recent research indicates the efficacy of brief MBSR and shortened mindfulness-based interventions (MBIs) (Bergen-Cico, Possemato, & Cheon, 2013; Call, Miron, & Orcutt, 2013). Carmody and Bear (2009) suggested that adaptations to shorten MBIs might be worthwhile for populations where extended time commitments are barriers to participation despite need for relief.
In our previous work in Chhattisgarh, a central Indian state, we indeed found significant mental health challenges among poor rural women with a history of stillbirth (Roberts, Montgomery, Lee, & Anderson, 2012) and subsequently studied the feasibility of a culturally adapted, mindfulness-based intervention aimed to improve coping. While the concept of the intervention was enthusiastically endorsed and a two-week pilot testing indicated promising efficacy, barriers to regular attendance were significant and clearly indicated that an eight-week intervention would not be feasible (Roberts & Montgomery, 2015). Despite this, results on MSSR outcomes were strong and women’s endorsement of the intervention extremely positive suggesting a good cultural fit, leading us to maintain our commitment to the MBSR delivery in this setting but modify its delivery to fewer but longer sessions. The purpose of this pilot study is to explore the feasibility and effectiveness of this shortened mindfulness-based intervention among poor women with a history of stillbirth in rural Chhattisgarh India.
Methods
Internal review board (IRB) approval was obtained from the research team’s university IRB and local approval was received from the municipal council’s district medical officer. After explanation of the study purpose, potential participants were given the opportunity to ask questions of research staff and consult with family members. Informed consent was obtained from each participant prior to beginning the study.
Sample
After obtaining permission from the Sarpanch (village chief), the Anganwadi, who is a village woman appointed as a maternal-child health worker (Park, 2009), was contacted and she referred women who had suffered stillbirth to us. Recruitment criteria included women with a history of stillbirth who spoke either Hindi or Chhattisgarhi, the local dialect. Initial participants also referred women they knew who had suffered stillbirth, thus purposive and snowball sampling technique were used (Tashakkori & Teddlie, 2003). Of note, women of all castes were recruited and participated, a somewhat unusual occurrence that was possible since women were recruited specifically for a life event that affects all women regardless of caste. Participants were recruited from two villages to obtain sufficient power.
Study design
This observational study utilized a pre-test, post-test (immediately after intervention completion), and 6-week follow-up assessment design. Surveys, completed as structured interviews due to low literacy rates, included demographics and validated surveys that have previously been pilot tested with this population after rigorous translation. Translation was completed by a bilingual committee. Independent forward and backward translation was completed and face validity checked for cultural and functional equivalence rather than literal translation (Jones, Lee, Phillips, Zhang, & Jaceldo, 2001; Pan & De La Puente, 2005).
Intervention
The five week mindfulness-based intervention was adapted from the Mindfulness Based Stress Reduction (MBSR) Curriculum Guide of the 8-week MBSR intervention developed by Dr. Jon Kabat-Zinn at the University of Massachusetts Medical Center (Blacker, Meleo-Meyer, Kabat-Zinn, & Santorelli, 2009; Kabat-Zinn, 2009). The intervention material and delivery method were culturally adapted based on our prior feasibility study and qualitative work using a community-based participatory approach (Roberts & Montgomery, 2015). After an initial training in the adapted MBSR and the research protocol, the same local nurses implemented the five weekly sessions in both villages. Weeks one and four were group sessions held in a central location within the village, while weeks two, three, and five were conducted in dyads and triads in participants’ homes. The sessions included didactic material covering the concept of mindfulness, mindfulness exercises, and discussions regarding how to use mindfulness skills in day-to-day life, as well as education regarding risk factors for stillbirth and preventive strategies. Between sessions, participants were encouraged to practice mindfulness exercises, keeping a simple daily log.
Measures
Hopkins Symptoms Check List – 10 (HSCL-10)
The HSCL-10 was translated into Urdu and performed well among a sample of poor, rural Pakistanis with low education levels (Syed, Zachrisson, Dalgard, Dalen, & Ahlberg, 2008); therefore, it was initially chosen for use among our population who share some similarities with the Syed et al. sample and performed well in our feasibility study (Roberts & Montgomery, 2015). The measure’s 10 items are rated on a Likert-type scale ranging from (1) not at all to (4) extremely, with higher scores representing more symptoms of anxiety and depression (Cronbach’s alpha = 0.76). A cut-off score of 1.65 was found by Syed et al. (2008) to indicate a high correlation between psychiatric symptoms and medical diagnosis with their study population, which is lower than the conventional 1.75 cut-off used in western populations.
Satisfaction With Life Scale (SWLS)
General satisfaction with life was measured using the 5-item SWLS with items rated on a Likert-type scale ranging from (1) strongly disagree to (7) strongly agree (Diener, Emmons, Larsen, & Griffin, 1985). The resulting summed scores range from five to 35 with higher scores representing greater satisfaction with life (Cronbach’s alpha = 0.70). The satisfaction with life scale is easily understood by respondents and is applicable in divergent life situations and countries (Diener, Inglehart, & Tay, 2013), including our study population (Roberts & Montgomery, 2015).
Short form of the Brief RCOPE
We used a 7-item version of the RCOPE scale with six items rated on a Likert-type scale ranging from (0) not at all to (3) a great deal to measure religious coping. Positive items are totaled separately from negative items, each subscale totaling 3 items (Feder et al., 2013). A higher score on each subscale represents greater use of positive or negative religious coping (Cronbach’s alphas = 0.59 and 0.68 respectively). Additionally, one item measures the extent that religion is used to understand or deal with stressful situations (John E. Fetzer Institute, 1999) and is rated on a scale of (0) not involved at all to (3) very involved.
Perinatal Grief Scale (PGS)
This is a 33-item questionnaire utilizing a Likert scale ranging from (1) strongly agree to (5) strongly disagree (Potvin, Lasker, & Toedter, 1989; Toedter, Lasker, & Janssen, 2001). Two reverse coded items were reversed before the items were summed for a possible index score of 33 to 165 with higher scores representing more severe grief (Cronbach’s alpha = 0.89). An index score greater than 91 indicates a high degree of grief (Toedter et al., 2001). Three subscales of 11 items each indicate active grief, difficulty coping, and despair (Potvin, Lasker, & Toedter, 1989).
Social Provisions Scale (SPS)
We used the 12-item version, which assesses social support received from others as perceived by the respondent (Mosley-Williams, Lumley, Gillis, Leisen, & Guice, 2002). A Likert-type scale ranging from (1) strongly disagree to (4) strongly agree is summed after reversing reverse-coded items for a possible index score of 12–48, and higher scores indicating more social support (Cronbach’s alpha =0.69).
Five Facet Questionnaire: Short Form (FFMQ-SF)
The FFMQ-SF includes 24 items utilizing a 5-point Likert scale ranging from (1) never or very rarely true to (5) very often or always true, to assess the five facets of mindfulness (Bohlmeijer, M, Fledderus, Veehof, & Baer, 2011). Each facet is scored independently after reversing all reverse-coded items (Cronbach’s alphas ranging from 0.60 for non-judging to 0.78 for observing). The five facets of mindfulness are distinct and therefore an index score for overall mindfulness cannot be given (Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006; Baer et al., 2008; Bohlmeijer et al., 2011).
Mindfulness exercise practice log
A pictorial practice log included body scan, awareness of breathing, yoga, pleasant moment, and attitude of gratitude reminders on a weekly calendar. Participants were instructed to mark each day that they practiced a particular skill. Practice logs were collected each week.
Program evaluation
Our end-of-program evaluation consisted of a 12-item questionnaire regarding perceived helpfulness of the intervention as well as logistical concerns. Each item was rated on a Likert-type scale ranging from (1) strongly disagree, to (5) strongly agree. Additionally, participants were asked for any other feedback or comments they wished to convey.
Follow-up evaluation
At six-weeks post intervention, participants were asked ten open-ended questions regarding the changes, if any, they had noted since completion of the program, their overall opinion of the program, which aspects were most/least beneficial to them, and what if any barriers they experienced which affected their participation.
Analysis
Quantitative pretest, post-test, and follow-up evaluation data were analyzed using SPSS. Analysis of these data included univariate (descriptive statistics), bivariate correlations of demographics with outcome variables, changes in outcome variables with t-tests and as appropriate chi-squares exploring significant changes over time, and general linear model repeated measures. Qualitative data (responses to open ended questions included in the program and follow-up evaluations) were analyzed using the content analysis method (Tashakkori & Teddlie, 2003).
Results
Study population
This study was completed across two sites, and while there were some demographic differences between the women of the two villages, there were no significant differences at baseline (pre-test) in the outcome variables, allowing us to combine the data. Thirty six women with a history of stillbirth were recruited from two villages, Pathariya (n = 19) and Daukapa (n = 17). The women were of reproductive age (approximately 18–35), which was estimated by discussion between the participant and research team because many participants did not know their age. The number of pregnancies per participant ranged from 1 to 6, and stillbirths suffered by each woman ranged from 1 to 3. Comparing the women by village revealed that the Daukapa participants included more women in the 26–35 years of age category, were more likely to have not had antenatal care, had a higher mean number of pregnancies (3.53 vs. 2.47), have more daughters, and a longer period of time since the most recent stillbirth (approximately 1.6 years vs. 0.76 years) than Pathariya participants. However, no significant differences were found on pretest variables of interest when comparing women from Pathariya and Daukapa (see Table 1 for details). The remainder of the results are reported for the combined sample. Participants included several castes, as self-reported by the women, and all were Hindu.
Table 1.
Demographics and variables by village
| Characteristic | Pathariya (n = 19) n (%) |
Daukapa (n = 17) n (%) |
|---|---|---|
| Age | ||
| 18–25 | 17 (89.5) | 9 (52.9)* |
| 26–35 | 2 (10.5) | 8 (47.1) |
| Gender of stillborn | ||
| Male | 12 (63.2) | 9 (52.9) |
| Female | 7 (36.8) | 8 (47.1) |
| Where stillbirth occurred | ||
| Home | 8 (42.1) | 7 (41.2) |
| Facility | 11 (57.9) | 10 (58.8) |
| Gestational age | ||
| 28–39 weeks | 5 (26.3) | 3 (17.6) |
| Full term | 14 (73.7) | 14 (82.4) |
| No antenatal care | 0 | 4 (23.5)* |
| Birth attendant | ||
| Relative | 4 (21.1) | 5 (29.4) |
| Dai | 2 (10.5) | 5 (29.4) |
| Nurse | 9 (47.4) | 2 (11.8) |
| Doctor | 4 (21.1) | 5 (29.4) |
| Education | ||
| None | 3 (15.8) | 7 (41.2) |
| Class 1–5 | 5 (26.3) | 6 (35.3) |
| Class 6–8 | 4 (21.1) | 3 (17.6) |
| Class 9+ | 7 (36.8) | 1 (5.9) |
| Health problems | ||
| None | 14 (73.7) | 10 (58.8) |
| Anemia | 4 (21.1) | 5 (29.4) |
| Malaria | 0 | 1 (5.9) |
| Other | 1 (5.3) | 1 (5.9) |
| Psychosocial problems | ||
| None | 14 (73.7) | 15 (88.2) |
| Anxiety | 1 (5.3) | 0 |
| Depression | 3 (15.8) | 1 (5.9) |
| Domestic violence | 1 (5.3) | 1 (5.9) |
| Autonomy | ||
| Cannot go to the market without permission | 15 (78.9) | 15 (88.2) |
| Visit natal kin—not allowed | 1 (5.3) | 1 (5.9) |
| — allowed but needs permission | 13 (68.4) | 12 (70.6) |
| — allowed without permission | 5 (26.3) | 4 (23.5) |
| M (SD) | M (SD) | |
|
|
||
| Total number of pregnancies | 2.47 (1.39) | 3.53 (1.38)* |
| Number of living sons | 0.63 (0.83) | 1.06 (1.44) |
| Number of living daughters | 0.42 (0.69) | 1.29 (1.36)* |
| Number of stillbirths | 1.42 (0.69) | 1.12 (0.33) |
| Days since stillbirth | 280.68 (443.31) | 589.76 (422.47)* |
| Health Symptoms | 2.19 (0.54) | 2.15 (0.55) |
| Satisfaction with life | 20.74 (7.48) | 25.06 (4.93) |
| Overall religiosity | 1.47 (0.61) | 1.35 (0.49) |
| Positive religious coping | 1.79 (0.57) | 1.67 (0.53) |
| Negative religious coping | 2.14 (0.79) | 2.18 (0.77) |
| Perinatal grief index | 111.42 (19.36) | 109.47 (17.74) |
| Social provision of support | 35.21 (5.34) | 33.47 (2.79) |
| Mindfulness—Describe | 15.89 (2.69) | 16.53 (2.10) |
| — Non-react | 15.95 (2.66) | 17.53 (3.56) |
| — Non-judge | 13.79 (4.04) | 12.53 (3.61) |
| — Observe | 14.16 (3.85) | 14.82 (4.22) |
| — Act with awareness | 17.00 (3.40) | 16.06 (3.88) |
Note:
= p < 0.05,
= p < 0.01,
p = < 0.001
Of the 36 women who completed the pretest, 29 began the intervention and 26 completed the intervention and posttest (89.7%); of those 23 (88.5%) completed the follow-up assessment. See Figure 1 for details of participant flow. Thus the attrition rate among participants who started the intervention was 10.3%.
Figure 1.
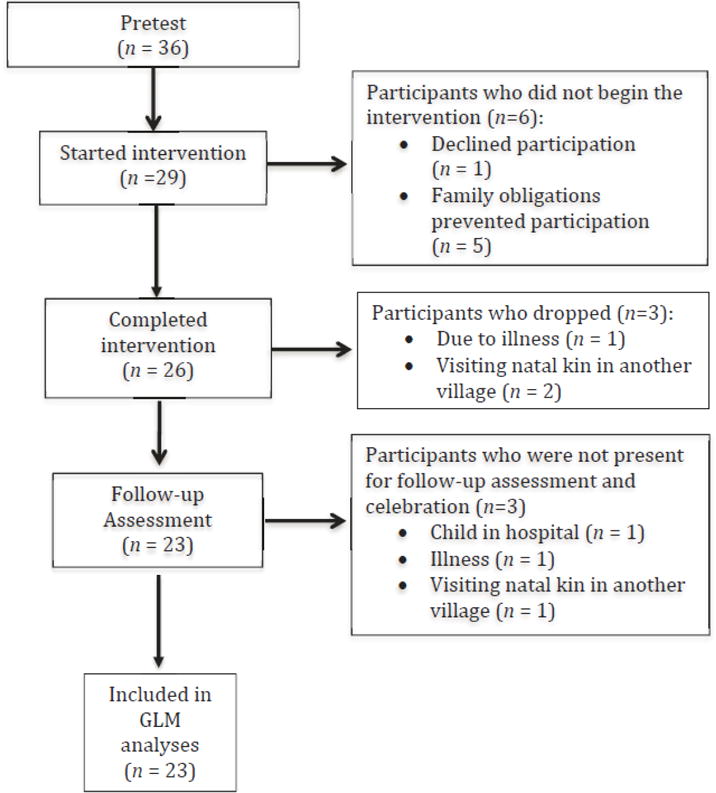
Flow of participants through each stage of study.
Univariate analysis at baseline (pre-test)
In the combined sample, 77.8% of the women reported that their pregnancy had been full term, that more of their stillborn babies were male than female (58.3% and 41.7% respectively), and mostly occurred in a facility rather than at home (58.3% vs. 41.7%). The number of pregnancies per woman ranged from 1 to 6, and the number of stillbirths experienced ranged from 1 to 3 (for women that had experienced more than one stillbirth, data was collected pertaining to the most recent stillbirth). The amount of time since the stillbirth occurred ranged from 20 days to four years. All of the women claimed the Hindu religion. Health problems were rarely self-identified: 66.7% reporting none, 25% reporting anemia, 2.8% malaria, and 5.6% other, which included heart and vision problems. Psychosocial problems were even more rarely self-identified: 80.6% reporting none, the remaining 19.4% included anxiety, depression, and domestic violence.
On average, the HSCL index was 2.20, elevated above both the 1.65 and 1.75 cut-offs, which are cut offs indicating a high correlation with psychiatric symptoms. Mean satisfaction with life was 22.71—within the 20–24 range—indicating average satisfaction with life. Negative religious coping was utilized more than positive religious coping (M = 2.10 and 1.73 respectively), with a mean of 1.52 for overall religious coping indicating that most participants chose the “somewhat involved” response option. The mean for social provision of support was 34.52, which is slightly above the mid-range possible index score of 30. Perinatal grief average was 110.04—above the cut-off score of 91—indicating high levels of grief. The three subscales of grief indicated active grief, then despair, and then difficulty coping as most prevalent (M = 42.09, 34.09, 33.87, respectively). Baseline scores for the five factors of mindfulness were as follows: describe (M = 15.62), non-react (M = 16.48), non-judge (M = 13.57), observe (M = 13.57), and act with awareness (M = 15.52).
Bivariate correlations
In preparation for outcome variable analysis, we explored demographics with each of the mindfulness components and mental health outcomes using bivariate correlation analysis, and ultimately controlled for those that were significant or trending when exploring program effects. A broad range of demographic variables were significantly associated with the outcome variables, several were significantly associated with more than one outcome variable (see Table 2 for details). Some demographics either trended (p < .10) or showed significant correlations (p < .05), including satisfaction with life, negative religious coping, social provision of support, the non-judge and observe components of mindfulness, perinatal grief and the active grief, difficulty coping, and despair subscales of the perinatal grief scale. There were no significant correlations between the demographic variables and overall religiosity.
Table 2.
Demographic bivariate correlations (2-tailed), N = 36
| Characteristic | r | Outcome variable |
|---|---|---|
| Psychosocial problems | .50** | Mental health symptoms (HSCL) |
|
| ||
| Gender of stillborn | .33+ | Satisfaction with life |
| Where stillbirth occurred | .40* | |
| Number of pregnancies | .50** | |
| Number of living sons | .35* | |
| Education | −.37* | |
|
| ||
| Number of pregnancies | −.36* | Positive religious coping |
| Education | .29+ | |
|
| ||
| Gender of stillborn | .32+ | Negative religious coping |
|
| ||
| Age | −.29+ | Social provision of support |
| Number of stillbirths | .38* | |
| Psychosocial problems | −.41** | |
| Visit natal kin | .35* | |
|
| ||
| Market permission | −.51** | Mindfulness—Non-react |
|
| ||
| Age | −.33+ | Mindfulness—Non-judge |
| Antenatal care | .35* | |
| Market permission | .51** | |
|
| ||
| Time since stillbirth occurred | .28+ | Mindfulness—Observe |
| Where stillbirth occurred | .42* | |
| Visit natal kin | −.46** | |
|
| ||
| Gender of stillborn | .41* | Mindfulness—Acting with awareness |
|
| ||
| Gender of stillborn | −.29+ | Perinatal grief scale (PGS) |
| Gestational age | −.33+ | |
| Number of living sons | −.37* | |
| Psychosocial problems | .32+ | |
| Market permission | −.35* | |
|
| ||
| Gestational age | −.32+ | PGS—Active grief |
| Number of pregnancies | −.30+ | |
| Number of living sons | −.45** | |
| Market permission | −.55** | |
|
| ||
| Gestational age | −.29+ | PGS—Difficulty coping |
| Number of living sons | −.28+ | |
|
| ||
| Gender of stillborn | −.33* | PGS—Despair |
| Psychosocial problems | .38* | |
| Market permission | −.33* | |
| Visit natal kin | −.30+ | |
Note:
p ≤ .10,
p < 0.05,
p < 0.01,
p < 0.001
Paired t-tests of Pre –Posttest changes (n = 26)
The HSCL index average significantly decreased from 2.21 to 1.75. The following changes in mean values were not statistically significant but changed in the desired direction: satisfaction with life increased to 24.81, positive religious coping increased to 1.71 while, overall use of religious coping increased to 1.65. Negative religious coping decreased to 1.97. Of the five facets of mindfulness, only one changed in the desired direction: observe, which increased (M = 14.88). All others non-significantly decreased.
Paired t-tests of Pre- 6 week changes (n = 23)
The HSCL index decreased significantly, averaging 1.92. While not significant, mean satisfaction with life increased to 24.65. The use of positive religious coping significantly decreased (M = 1.39), and though not statistically significant, negative religious coping decreased (M = 1.93), and overall use of religious coping increased (M = 1.87). The perceived social provision of support average increased (M = 35.78) but was not statistically significant. Changes in the facets of mindfulness occurred in the desired direction in four out of the five skills: acting with awareness significantly increased to 18.13, describe increased to 17.09 (p < .10), non-judge increased to 13.87, and observe decreased to 13.78. Non-react significantly decreased to 13.52. The average perinatal grief index score significantly decreased to 93.57, with significant decreases in each of the three subscales: active grief (M = 35.04), difficulty coping (M = 28.00), and despair (M = 30.52).
General linear modeling repeated measures longitudinal analyses results
To explore changes in posttest and 6 week follow up, scores from baseline scores we conducted within subjects repeated measures controlling for their respective significant demographic correlates determined through the bivariate analyses described in Table 2. Significant changes occurred in HSCL index scores, positive religious coping, and in two of the five mindfulness components; describe, and acting with awareness. While non-significant, two mindfulness components changed in the desired direction: non-judge and observe. Only one, mindfulness component, being nonreactive, changed significantly in the non-desired direction. The perinatal grief index scores with all subscales decreased (improved) significantly (see Table 3 for details).
Table 3.
GLM Repeated Measures with control of significant bivariate demographic correlates and Bonferroni correction. N = 23
| Variables | Pre M (SD) |
Post M (SD) |
Follow-up M (SD) |
p-value |
|---|---|---|---|---|
| Mental health symptoms (HSCL)a | 2.20 (0.58) | 1.79 (0.70) | 1.88 (0.58) | .042 |
| Satisfaction with lifeb | 22.71 (6.84) | 24.81 (5.78) | 25.43 (3.89) | .152 |
| Positive religious copingc | 1.73 (0.47) | 1.70 (0.72) | 1.34 (0.31) | .000 |
| Negative religious copingd | 2.10 (0.75) | 2.03 (0.97) | 1.85 (0.79) | .360 |
| Overall religiosity | 1.52 (0.60) | 1.67 (0.73) | 1.90 (0.77) | .329 |
| Social provision of supporte | 34.52 (4.96) | 32.76 (5.23) | 35.67 (4.21) | .252 |
| Mindfulness—Describe | 15.62 (1.43) | 16.33 (2.85) | 17.52 (3.46) | .043 |
| —Non-reactf | 16.48 (3.68) | 15.10 (4.84) | 13.67 (3.29) | .025 |
| —Non-judgeg | 13.57 (4.46) | 12.81 (4.69) | 13.90 (3.48) | .595 |
| —Observeh | 13.57 (4.19) | 15.24 (3.03) | 13.81 (2.70) | .224 |
| —Act with awarenessi | 15.52 (3.36) | 14.76 (5.18) | 17.90 (3.97) | .033 |
| Perinatal Griefj | 110.04 (21.29) | 93.57 (20.89) | .002 | |
| —Active Griefk | 42.09 (8.42) | 35.04 (8.76) | .005 | |
| —Difficulty Copingl | 33.87 (8.08) | 28.00 (6.40) | .004 | |
| —Despairm | 34.09 (7.78) | 30.52 (7.97) | .033 |
Controlled for psychosocial problems.
Controlled for gender of stillborn, where stillbirth occurred, gravida, number of living sons, education.
Controlled for gravida, education.
Controlled for gender of stillborn.
Controlled for age, number of stillbirths, psychosocial problems, visit with natal kin.
ontrolled for market permission.
Controlled for age, antenatal care, market permission.
Controlled for time since stillbirth occurred, where stillbirth occurred, visit with natal kin.
Controlled for gender of stillborn.
Controlled for gender of stillborn, gestational age, number of living sons, market permission.
Controlled for gestational age, number of pregnancies, number of living sons, market permission.
Controlled for gestational age, number of living sons.
Controlled for gender of stillborn, psychosocial problems, market permission, visit with natal kin.
Practice of mindfulness exercises
The 26 women who completed the intervention all kept track of their practice at home of the mindfulness exercises taught during the intervention. The three women who dropped out kept track for the weeks they participated, the rest of the women completed the practice log for each week of the intervention. Most women practiced each skill daily, for a total of 30 minutes on average.
End-of-program evaluations
All participants completed the end-of-program evaluation. On the Likert scale with 1 representing strongly disagree and 5 representing strongly agree, most participants (70.4%) strongly agreed with the format of the program, the remaining 29.6% chose agree. The women agreed or strongly agreed that they had learned a lot about stillbirth risk reduction, grief, and coping (51.9% and 48.1% respectively). Two participants were neutral about the shared group experience, while the rest either agreed (63.0%) or strongly agreed (29.6%) that it was helpful. All participants indicated that they would continue to use Mindfulness techniques. Most (77.8%) indicated that their families had noticed a difference in their ability to cope and 88.9% indicated that their families would allow them to return for future sessions given the opportunity.
Follow-up evaluation
When asked for their overall opinion of the program, all the participants had positive responses indicating that they thought it was useful and made them feel good. Some indicated that it was good for life in general; some noted that it was good for the body as well as the mind/emotions, and enjoyable.
“In this program I felt good and increased satisfaction in my life.”
“Good, very useful to deal with grief. It’s helpful for body also.”
In terms of any changes the women noticed in their thought patterns, responses to thoughts, mood, and ability to cope, most participants reported a “release of heaviness” and some expressed a new sense of peace. A few noted feeling happiness and increased interest in work or activities. All of the women expressed that the program had been beneficial but did not articulate specific aspects that were more beneficial than others. Barriers to participation included family illness and other family/household obligations, the schedule of sessions, and the time required to participate. One participant noted that initially, family members interfered when she practiced the mindfulness exercises, which caused her distress, but after a while they no longer disturbed her and it was “all okay.” All of the women indicated that they would recommend the program to others and repeat it themselves, given the opportunity.
Discussion
Our main objective for this pilot study was to explore the feasibility and effectiveness of our culturally adapted, shortened mindfulness-based intervention to address the complex grief experiences of rural women in Chhattisgarh, India. The intervention was very well received and over the five weeks had a very low attrition rate. Even six weeks later, nearly all participants completed the follow-up assessment.
All of our participants had experienced stillbirth in the third trimester, which mirrors previous research findings indicating that nearly 3 million third trimester stillbirths occur globally each year, 98% occurring in low to middle income countries. Although reductions in stillbirth rates are noted over the last decade in most of these countries, including India, most third trimester stillbirths are potentially preventable (McClure, Saleem, et al., 2015). Causes of stillbirth, maternal death and neonatal death are closely linked and well delineated in the literature (McClure, Bose, et al., 2015) and are important to progression of the effort to meet MDG 4 and 5 (Bhutta & Black, 2013). Scaling up of interventions to reduce stillbirth rates (primarily by ensuring basic and comprehensive emergency obstetric care, and facility births for all women, as well as women’s empowerment in general) will take time, training, and additional resources (Bhutta & Black, 2013; Mullan & Horton, 2011). Meanwhile, women who have experienced stillbirth suffer stigma, marginalization, and blame (Frøen et al., 2011), in addition to perinatal grief (Roberts, Anderson, et al., 2012; Roberts, Montgomery, et al., 2012). Our study aligns with the call to increase visibility of stillbirths and invest in stillbirth-related research (Goldenberg et al., 2011).
Our participants had high levels of perinatal grief and indications of anxiety and depression. Umphrey and Cacciatore (2014) note that losing a child is one of the most painful, traumatic, and challenging experiences among humanity, to which grieving is a natural response, placing parents—especially mothers, at risk for mental health issues after perinatal loss (Bennett, Litz, Lee, & Maguen, 2005).
Health care providers and family often minimize or are dismissive of the loss compounding the negative overall impact of this traumatic experience, creating physical and emotional sequela (Lang et al., 2011). The International Stillbirth Alliance (ISA) stresses the importance of bereavement support, which begins with recognition of stillbirth as a tragic loss (Heazell et al., 2013). The Lancet’s Stillbirths Series also highlights the need for bereavement support (Frøen et al., 2011). In the context of tremendous mental health needs and complex grief, this study not only sheds light on the mental health burden for women who have experienced stillbirth in rural Chhattisgarh, India, but also points to a potential way to begin to more systematically address the problem and in the long term, encourage higher levels of social provision of support.
Our GLM results indicate changes over the pre-post-post (follow-up) interval, which included significant changes in the mental health (health symptoms checklist index scores); positive religious coping; the describe, non-react, and acting with awareness components of mindfulness; and, most importantly, significantly decreased the overall levels of perinatal grief, and each of the grief subscales—active grief, difficulty coping, and despair. These quantitative changes over time were confirmed by the qualitative data indicating that participants practiced the mindfulness exercises and self-reported changes in their ability to cope. While mindfulness-based interventions are not expected to eliminate grief, they can help alleviate some of the resultant distress (Thieleman, Cacciatore, & Hill, 2014). Moreover, we wish to point to the finding that several results actually continued to improve over time as the women implemented their daily practices of mindfulness.
While these findings are encouraging, several limitations must be considered in the interpretation of these results. Limitations include the small sample size, which of course is part of any pilot study, as is the purposive sampling (participants were all poor, Hindu women with a history of stillbirth in rural Chhattisgarh), which limits generalizability, and the study design that while longitudinal, had no control group. Additionally, conceptual translation of the FFMQ proved challenging, particularly concerning non-react and non-judge, where even bilingual nurses had difficulty understanding double-negatives. This likely explains lack of changes in the desired direction for non-react dimensions of the mindfulness skills. Indeed, when we followed up this issue with local Hindu speaking colleagues, we were told that these questions were difficult to comprehend or were “confusing” as stated. We will need to resolve this instrumentation and also our power issue going forward when we will rigorously explore the intervention with a larger sample and a control group design.
Strengths to be noted include the use of an evidence-based well-published intervention, and participatory methods in adapting it culturally to the context of the women living in this low resource settings that does not provide them tools to help them with their grief. Furthermore, part of the pilot test was the use of a fiscally more realistic use of a train-the-trainer model, utilizing and training nurses from a local hospital, allowing for local capacity building as well as increasing the chances of further diffusion of the intervention. Finally, receptivity across castes is important in addition to the promises of feasibility and effectiveness that this intervention offers, as it indicates unique scale-ability.
Conclusion
In our overall evaluation of this pilot study, we feel that the cultural adaptation, delivery method, and intervention dose were appropriate for the setting as indicated by the high rate of participation and positive program results, with results increasing in the desired direction over time, a strong measure of success. Our approach was to culturally adapt an evidence-based intervention in collaboration with the local community and deliver it using a locally available team of nurses. The overall positive outcomes and local “ownership” provide a strong argument that it is possible to deliver such an intervention by building local capacity. While this is highly encouraging, further rigorous research, with a larger sample size and a control group is needed to explore if our results, including the changes in the desired direction, will hold over longer periods of time. At this point we feel, however, that our early pilot study results point to the viability of this shortened, adapted mindfulness-based intervention as an intervention that holds great promise for being taken to scale in this high need environment.
Acknowledgments
We want to thank Dr. Anil Henry, director of Christian Hospital Mungeli (CHM) in Chhattisgarh, India for facilitating contacts and providing local support. We also want to thank Sweta Titus and Namita Titus, CHM nurses, and additional CHM staff. A special thanks to the women who shared their lives, including stillbirth experiences, and enthusiastically engaged in the intervention. Funding: Loma Linda University School of Nursing seed grant
Contributor Information
Lisa Roberts, Loma Linda University.
Susanne Montgomery, Loma Linda University.
References
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, Williams JMG. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15(3):329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Balarajan Y, Selvaraj S, Subramanian S. Health care and equity in India. The Lancet. 2011;377(9764):505–515. doi: 10.1016/S0140-6736(10)61894-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett SM, Litz BT, Lee BS, Maguen S. The Scope and Impact of Perinatal Loss: Current Status and Future Directions. Professional Psychology: Research and Practice. 2005;36(2):180–187. doi: 10.1037/0735-7028.36.2.180. [DOI] [Google Scholar]
- Bergen-Cico D, Possemato K, Cheon S. Examining the Efficacy of a Brief Mindfulness-Based Stress Reduction (Brief MBSR) Program on Psychological Health. Journal of American College Health. 2013;61(6):348–360. doi: 10.1080/07448481.2013.813853. [DOI] [PubMed] [Google Scholar]
- Bhutta ZA, Black RE. Global maternal, newborn, and child health—so near and yet so far. New England Journal of Medicine. 2013;369(23):2226–2235. doi: 10.1056/NEJMra1111853. [DOI] [PubMed] [Google Scholar]
- Bidner C, Eswaran M. A gender-based theory of the origin of the caste system of India. Journal of Development Economics. 2015;114:142–158. [Google Scholar]
- Blacker M, Meleo-Meyer F, Kabat-Zinn J, Santorelli S. Stress Reduction Clinic Mindfulness-Based Stress Reduction (MBSR) Curriculum Guide. Center for Mindfulness in Medicine, Health Care, and Society: University of Massachusets Medical School; 2009. p. 20. [Google Scholar]
- Bohlmeijer EM, Fledderus M, Veehof M, Baer R. Psychometric Properties of the Five Facet Mindfulness Questionnaire in Depressed Adults and Development of a Short Form. Assessment. 2011;18(3):308–320. doi: 10.1177/1073191111408231. [DOI] [PubMed] [Google Scholar]
- Boyle FM, Vance JC, Najman JM, Thearle MJ. The mental health impact of stillbirth, neonatal death or sids: Prevalence and patterns of distress among mothers. Social Science & Medicine. 1996;43(8):1273–1282. doi: 10.1016/0277-9536(96)00039-1. [DOI] [PubMed] [Google Scholar]
- Branisa B, Klasen S, Ziegler M, Drechsler D, Jütting J. The institutional basis of gender inequality: The Social Institutions and Gender Index (SIGI) Feminist economics. 2014;20(2):29–64. [Google Scholar]
- Call D, Miron L, Orcutt H. Effectiveness of brief mindfulness techniques in reducing symptoms of anxiety and stress. Mindfulness. 2013 doi: 10.1007/s12671-013-0218-6. [DOI] [Google Scholar]
- Carmody J, Baer RA. How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. Journal of Clinical Psychology. 2009;65(6):627–638. doi: 10.1002/jclp.2055. [DOI] [PubMed] [Google Scholar]
- Davis D, Hayes JA. What are the benefits of mindfulness? A practice review of psychotherapy-related research. Psychotherapy. 2011;48(2):198–208. doi: 10.1037/a0022062. [DOI] [PubMed] [Google Scholar]
- Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life Scale. Journal of Personality Assessment. 1985;49(1):71. doi: 10.1207/s15327752jpa4901_13. Retrieved from http://0-search.ebscohost.com.catalog.llu.edu/login.aspx?direct=true&db=aph&AN=6385463&site=ehost-live&scope=site. [DOI] [PubMed] [Google Scholar]
- Diener E, Inglehart R, Tay L. Theory and Validity of Life Satisfaction Scales. Social Indicators Research. 2013;112(3):497–527. doi: 10.1007/s11205-012-0076-y. [DOI] [Google Scholar]
- Farb NAS, Anderson AK, Mayberg H, Bean J, McKeon D, Segal ZV. Minding one’s emotions: Mindfulness training alters the neural expression of sadness. Emotion. 2010;10(1):25. doi: 10.1037/a0017151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feder A, Ahmad S, Lee EJ, Morgan JE, Singh R, Smith BW, Charney DS. Coping and PTSD symptoms in Pakistani earthquake survivors: Purpose in life, religious coping and social support. Journal of Affective Disorders. 2013;147(1–3):156–163. doi: 10.1016/j.jad.2012.10.027. [DOI] [PubMed] [Google Scholar]
- Fottrell E, Kanhonou L, Goufodji S, Behague D, Marshall T, Patel V, Filippi V. Risk of psychological distress following severe obstetric complications in Benin: the role of economics, physical health and spousal abuse. The British Journal of Psychiatry. 2010;196(1):18. doi: 10.1192/bjp.bp.108.062489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frøen JF, Cacciatore J, McClure EM, Kuti O, Jokhio AH, Islam M, Shiffman J. Stillbirths: why they matter. The Lancet. 2011;377(9774):1353–1366. doi: 10.1016/S0140-6736(10)62232-5. [DOI] [PubMed] [Google Scholar]
- Goldenberg RL, McClure EM, Bhutta ZA, Belizán JM, Reddy UM, Rubens CE, Darmstadt GL. Stillbirths: the vision for 2020. Lancet. 2011;377(9779):1798–1805. doi: 10.1016/S0140-6736(10)62235-0. [DOI] [PubMed] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of psychosomatic research. 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Heazell AEP, Leisher S, Cregan M, Flenady V, Frøen JF, Gravensteen IK, Erwich JJHM. Sharing experiences to improve bereavement support and clinical care after stillbirth: report of the 7th annual meeting of the international stillbirth alliance. Acta Obstetricia et Gynecologica Scandinavica. 2013;92(3):352–361. doi: 10.1111/aogs.12042. [DOI] [PubMed] [Google Scholar]
- Inhorn MC. Global infertility and the globalization of new reproductive technologies: illustrations from Egypt. Social Science & Medicine. 2003;56(9):1837. doi: 10.1016/s0277-9536(02)00208-3. [DOI] [PubMed] [Google Scholar]
- John E. Fetzer Institute. Multidimensional Measurement of Religousness/Spirituality for Use in Health Research. Kalamazoo, MI: John E. Fetzer Institute; 1999. p. 96. [Google Scholar]
- Jones P, Lee J, Phillips L, Zhang X, Jaceldo K. An adaptation of Brislin’s translation model for cross-cultural research. Nursing research. 2001;50(5):300–304. doi: 10.1097/00006199-200109000-00008. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Delta; 2009. [Google Scholar]
- Kelly ER. Marking short lives: Constructing and sharing rituals following pregnancy loss. New York, NY US: Peter Lang Publishing; 2007. [Google Scholar]
- Lang A, Fleiszer AR, Duhamel F, Sword W, Gilbert KR, Corsini-Munt S. Perinatal loss and parental grief: The challenge of ambiguity and disenfranchised grief. OMEGA-Journal of Death and Dying. 2011;63(2):183–196. doi: 10.2190/OM.63.2.e. [DOI] [PubMed] [Google Scholar]
- Ludwig DS, Kabat-Zinn J. Mindfulness in medicine. JAMA: the journal of the American Medical Association. 2008;300(11):1350–1352. doi: 10.1001/jama.300.11.1350. [DOI] [PubMed] [Google Scholar]
- Mandal H. India, an illustrated atlas of scheduled castes. Anthropological Survey of India; 2005. [Google Scholar]
- McClure EM, Bose CL, Garces A, Esamai F, Goudar SS, Patel A, Kodkany BS. Global network for women’s and children’s health research: a system for low-resource areas to determine probable causes of stillbirth, neonatal, and maternal death. Maternal Health, Neonatology and Perinatology. 2015;1(1):11. doi: 10.1186/s40748-015-0012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClure EM, Saleem S, Goudar SS, Moore JL, Garces A, Esamai F, Pasha O. Stillbirth rates in low-middle income countries 2010–2013: a population-based, multi-country study from the Global Network. Reproductive health. 2015;12(Suppl 2):S7. doi: 10.1186/1742-4755-12-S2-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta L, Verma I. Helping parents to face perinatal loss. Indian journal of pediatrics. 1990;57(5):607–609. doi: 10.1007/BF02728696. [DOI] [PubMed] [Google Scholar]
- Mosley-Williams A, Lumley MA, Gillis M, Leisen J, Guice D. Barriers to treatment adherence among African American and white women with systemic lupus erythematosus. Arthritis & Rheumatism: Arthritis Care & Research. 2002;47(6):630–638. doi: 10.1002/art.10790. Retrieved from http://0-search.ebscohost.com.catalog.llu.edu/login.aspx?direct=true&db=rzh&AN=2004191507&site=ehost-live&scope=site. [DOI] [PubMed] [Google Scholar]
- Mullan Z, Horton R. Bringing stillbirths out of the shadows. The Lancet. 2011;377(9774):1291–1292. doi: 10.1016/S0140-6736(11)60098-6. [DOI] [PubMed] [Google Scholar]
- Pan Y, De La Puente M. Census Bureau guideline for the translation of data collection instruments and supporting materials: Documentation on how the guideline was developed. Survey Methodology. 2005;06 [Google Scholar]
- Pandalangat N. Mental Health Services for Women in Third World Countries and Immigrant Women. In: Romans S, Seeman M, editors. Women’s mental health: a life-cycle approach. Lippincott Williams & Wilkins; 2006. [Google Scholar]
- Park K. Park’s Textbook of Preventive and Social Medicine. 20th. Jabalpur, India: Banarsidas Bhanot; 2009. [Google Scholar]
- Patel V, Rodrigues M, DeSouza N. Gender, Poverty, and Postnatal Depression: A Study of Mother in Goa, India. American Journal of Psychiatry. 2002;159(1):43. doi: 10.1176/appi.ajp.159.1.43. Retrieved from http://0-search.ebscohost.com.catalog.llu.edu/login.aspx?direct=true&db=aph&AN=6039493&site=ehost-live. [DOI] [PubMed] [Google Scholar]
- Potvin L, Lasker J, Toedter L. Measuring grief: A short version of the Perinatal Grief Scale. Journal of Psychopathology and Behavioral Assessment. 1989;11(1):29–45. doi: 10.1007/bf00962697. [DOI] [Google Scholar]
- Roberts LR, Anderson BA, Lee JW, Montgomery S. Grief and Women: Stillbirth in the Social Context of India. International Journal of Childbirth. 2012;2(3):12. doi: 10.1891/2156-5287.2.3.187. doi: http://dx.doi.org/10.1891/2156-5287.2.3.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts LR, Montgomery S. Mindfulness-based Intervention for Perinatal Grief after Stillbirth in Rural India. Issues in Mental Health Nursing. 2015;36:222–230. doi: 10.3109/01612840.2014.962676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts LR, Montgomery S, Lee JW, Anderson BA. Social and Cultural Factors Associated with Perinatal Grief in Chhattisgarh, India. Journal of Community Health. 2012;37(3):572–582. doi: 10.1007/s10900-011-9485-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sather M, Fajon A, Zaentz R, Rubens C. Global report on preterm birth and stillbirth (5 of 7): advocacy barriers and opportunities. BMC Pregnancy and Childbirth. 2010;10(Suppl 1):S5. doi: 10.1186/1471-2393-10-S1-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syed HR, Zachrisson HD, Dalgard OS, Dalen I, Ahlberg N. Concordance between Hopkins Symptom Checklist (HSCL-10) and Pakistan Anxiety and Depression Questionnaire (PADQ), in a rural self-motivated population in Pakistan. BMC Psychiatry. 2008;8:1–12. doi: 10.1186/1471-244X-8-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tashakkori A, Teddlie C. Handbook of mixed methods in social & behavioral research. Thousand Oaks, CA: Sage Publications, Inc; 2003. [Google Scholar]
- Thieleman K, Cacciatore J, Hill PW. Traumatic bereavement and mindfulness: A preliminary study of mental health outcomes using the ATTEND model. Clinical Social Work Journal. 2014;42(3):260–268. [Google Scholar]
- Thomas D, Sarangi BL, Garg A, Ahuja A, Meherda P, Karthikeyan SR, Druvasula R. Closing the health and nutrition gap in Odisha, India: A case study of how transforming the health system is achieving greater equity. Social Science & Medicine. 2015 doi: 10.1016/j.socscimed.2015.06.010. [DOI] [PubMed] [Google Scholar]
- Toedter LJ, Lasker JN, Janssen HM. International comparison of studies using the Perinatal Grief Scale: A decade of research on pregnancy loss. Death Studies. 2001;25(3):205–228. doi: 10.1080/074811801750073251. [DOI] [PubMed] [Google Scholar]
- Umphrey LR, Cacciatore J. Love and Death: Relational Metaphors Following the Death of a Child. Journal of Relationships Research. 2014;5:e4. [Google Scholar]


