Abstract
Background
Cardiovascular disease (CVD) is an important driver of mortality after kidney transplantation. Its broader impact on posttransplant health care utilization in US hospitals is unknown.
Methods
We used administrative claims data from the Nationwide Inpatient Sample and the American Hospital Association Annual Survey to identify hospitalizations for kidney transplant patients with a cardiovascular diagnosis from 2005 to 2011. CVD hospitalizations were stratified by transplant hospital status to characterize patterns in inpatient health care utilization and outcomes. Based on these analyses, the domestic burden of treatment for posttransplant CVD (myocardial infarction, stroke, congestive heart failure, dysrhythmia, cardiac arrest, malignant hypertension) was estimated.
Results
The total domestic burden of post-kidney transplant hospitalization between 2005 and 2011 is estimated at 389 138 of which 26.5% of episodes were related to CVD (n = 103 118). CVD was responsible for a growing proportion of post-transplant hospitalizations over time (24.4%-30.4%, P < 0.001). Compared with nontransplant hospitals, transplant hospitals had similar length of stay (median length of stay, 3.7 days), higher median costs per hospitalization (US $10 364 vs US $8606, overall US $9324), and lower adjusted mortality (3.2% vs 3.9%, overall 3.6%; P = 0.003).
Conclusions
Inpatient CVD care is increasing over time for kidney transplant patients, accounting for 30% of all post-transplant hospitalizations. Variation exists in the inpatient care, outcomes, and costs between by hospital type. Further studies are needed to better understand the mechanisms behind these phenomena.
Cardiovascular disease (CVD) is a leading cause of death after kidney transplantation.1,2 Strategies to address CVD after kidney transplantation have focused on risk factor modification, avoidance of transplant in patients with preexisting CVD, and prevention of events through the medical management of common co-morbidities including diabetes mellitus, hypertension, and hyperlipidemia.3,4 CVD treatment can be challenging—it demands significant health care resources, and even specialty care does not completely remove the risk of mortality. For kidney transplant patients, this challenge can be even greater due to the medical complexity of the patient.
Recent evidence suggests that the burden of CVD disease in kidney transplant recipients may be stabilizing or even declining in some contexts. Lam et al5 showed that the incidence of death, myocardial infarction (MI), coronary intervention, and ischemic stroke have remained stable around 8.5% to 9.9% from 1994 to 2009, without significant changes in 3-year risk-adjusted death-censored CV events at their center. Pilmore et al6 have suggested that mortality from CVD declined in the mid 2000s compared to older cohorts in Australia and New Zealand. These data are promising, but are contrary to other reports. Medicare data suggests post-transplant CVD incidence is actually increasing.7-9 The contradictory nature of these data represents a challenge for transplant providers and cardiovascular specialists designing care processes for post-transplant patients. Without appropriate data on current patterns of care for post-transplant CVD, efforts to design appropriate post-transplant care protocols, allocate resources, and plan future research may not be effective.
In this analysis, we characterized the patterns of care for CVD in the US post-kidney transplant population by describing in-hospital care using national-level administrative data. The goal of this analysis was to better define the scope of this problem and identify trends in care utilization that could inform future studies and improve outcomes.10-12
MATERIALS AND METHODS
Data Sources
For this analysis, we used 2005 to 2011 data from the Nationwide Inpatient Sample (NIS), which is a publicly available dataset supported by through Agency for Health Research and Quality’s Health Care Utilization Project (HCUP). The NIS is a 20% national administrative data sample of all US hospital discharges and contains demographic, diagnosis, and therapeutic information within a given hospitalization episode without patient identifiers. Diagnosis and therapeutic interventions are classified based on 9th International Classification of Disease codes. We merged hospitalization episode-based NIS data with hospital structural data from the American Hospital Association (AHA) Annual Survey of Hospitals using the Medicare provider identification number for the hospital. The AHA survey contains 1000 self-reported data elements on organizational structure, facilities and services, payer mix, and financial performance from 6,500 hospitals. We used these data to define “transplant hospitals”, which were defined as hospitals performing solid organ transplants in that year based on data self-reported to the AHA. In this context, we created a unique dataset to capture hospital admissions for kidney transplant patients admitted with CVD with hospital-specific resource data.
Defining Study Cohort
This study sample included hospitalizations of patients with kidney transplant status (V42.0) as any diagnosis. Cardiovascular hospitalizations were considered as a subset of all hospitalizations for kidney transplant recipients, and were defined as episodes with at least 1 primary or secondary cardiovascular diagnosis. Cardiovascular diagnoses included at least 1 of the following: MI (410.x), congestive heart failure (CHF) (428.x), dysrhythmia (427.x), cerebrovascular accident (CVA) (436. 437.1, 997.x), malignant hypertension (402.x), and cardiac arrest (427.5, 997.1). Cardiovascular procedures were based on International Classification of Disease-9 codes and included diagnostic cardiac catheterization, therapeutic cardiac catheterization (angioplasty, atherectomy, stenting), coronary artery bypass grafting, aortic valve surgery, mitral valve surgery, tricuspid valve surgery, aortic graft surgery, or other cardiac surgery. Outcomes of interest included length of hospital stay for each hospitalization episode, mortality, and total hospital costs. Hospital costs were calculated using Medicare cost-to-charge ratios for each hospital, and were adjusted for inflation to 2011 dollars by the Consumer Price Index.
Statistical Approach and Sample Weighting
The national discharge-level estimates were computed by incorporating the discharge weights within each sampling stratum.13 We compared the outcomes, demographic and clinical characteristics between hospitalizations in a transplant and non-transplant facility by using the χ2 test for the nominal data and t test for the continuous data. All analyses were conducted in SAS 9.4 (SAS Institute, Inc., Cary, NC). Statistical significance was considered at the P < 0.05 level. The study used publicly available deidentified hospital claims and hospital structural data was thus exempt from institutional review board approval.
RESULTS
Trends in Hospitalizations for CVD
From 2005 to 2011, annual domestic post-kidney transplant hospitalizations increased by 4.2% from 50080 to 52726 admissions. Figure 1 demonstrates the national estimates in trends in hospitalizations for CVD in the post-kidney transplant population. By 2011, 30.4% of all post-kidney transplantation hospitalizations were for CVD (n = 16,029), an increase from 24.4% in 2005 (not shown), but transplant and nontransplant hospitals had different trends. The growth in CVD hospitalizations as a function of all post-kidney transplant hospitalizations was observed primarily in non-transplant facilities (P = 0.01) (Figure 1). By 2011, 92.8% of these hospitalizations were in non-transplant hospitals (n = 568), as transplant hospital admissions for CVD declined to 7.2% in 2011.
FIGURE 1.
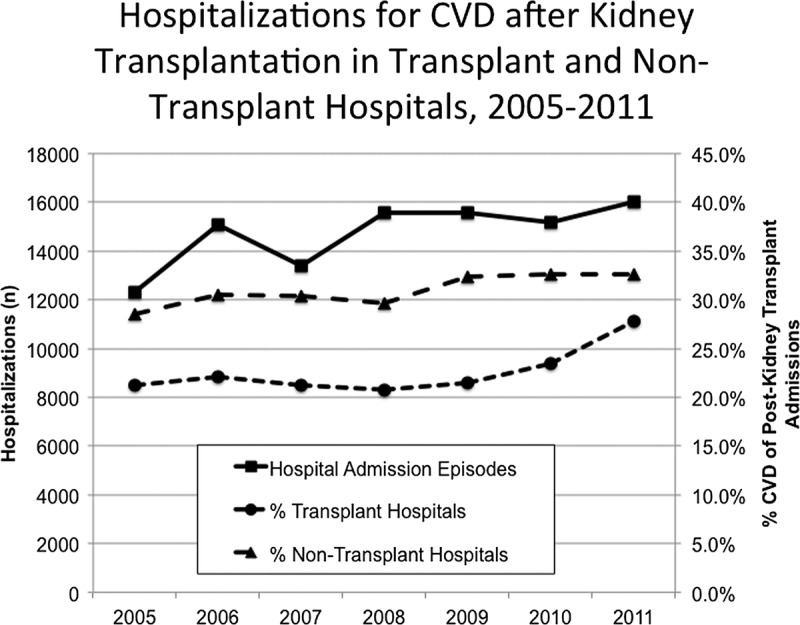
Hospitalizations for CVD after kidney transplantation in transplant and non-transplant hospitals, 2005 to 2011. Over the study period, there were 103118 hospitalizations in the United States that occurred after kidney transplantation. By 2011, more than 30% of these hospitalizations were attributable to CVD, totaling more than 16000 admissions (square solid line, left y-axis). Relative to all post-transplant admissions, non-transplant hospitals (triangle dash) had significantly higher proportions of CVD admissions compared to transplant hospitals (circle dash) (right y-axis). 58.3% of all post-kidney transplant CVD admissions in 2011 occurred in non-transplant facilities (17.7% of all post-transplant admissions) (not shown).
Over time, there were significant changes in the primary CVD diagnosis (Figure 2). Among all post-kidney transplant patients admitted with CVD, the proportion of MI admissions increased relatively by 32.2% over time, accounting for 2.6% of all hospitalizations and 8.5% of all CVD episodes by 2011. Stroke incidence relatively declined by 16.9% over time, accounting for 2.1% of all hospitalizations and 7.0% of the CVD episodes. CHF accounted for 16.4% of all post-transplant hospitalizations, growing by 24% from 2005. Dysrhythmias were very common in the post-kidney transplant population, accounting for 11.6% to 16.6% over the cohort, and demonstrating the most relative growth at 42.8% of all CVD diagnoses. Both cardiac arrest and malignant hypertension together accounted for a small percentage of all hospitalizations (1.2% of all post-transplant hospitalization and 4.1% of all CVD diagnosis in 2011), which declined even further with time.
FIGURE 2.
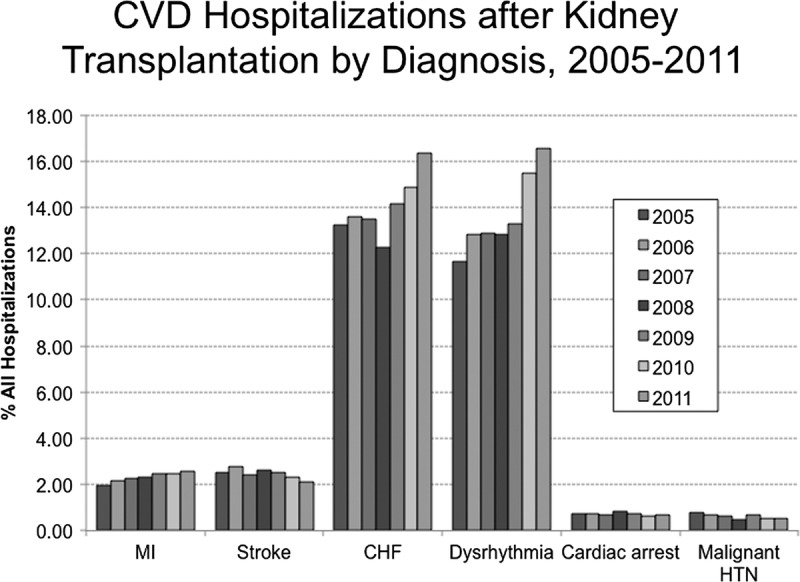
CVD Hospitalizations after Kidney Transplantation by Diagnosis, 2005-2011. This figure demonstrates diagnosis-specific trends in hospital admissions over the study period attributable to MI, stroke, CHF, Dysrhythmia, Cardiac Arrest, and malignant hypertension. Over the study period, there was a statistically significant increase in admissions for MI, accounting for 2.6% of all post-kidney transplant hospitalizations (P < 0.05). Stroke admissions declined slightly. The most significant increases were observed in more documented primary-diagnosis admissions for CHF and dysrhythmia (P = 0.01), accounting for 16% to 17% of all hospital admissions respectively. Cardiac arrest and malignant hypertension accounted for just over 1% of all post-kidney transplant hospital admissions across the study period.
Nationwide Estimates of Demographic and Clinical Differences in Patients Admitted to Transplant and Nontransplant Hospitals
Between 2005 and 2011, 103118 unique hospitalizations occurred for CVD in patients who had previously undergone kidney transplantation. Of these, 55.7% (n = 57449) occurred in non-transplant hospitals. Table 1 stratifies the study population based on hospitalization in a transplant or non-transplant facility. Compared with transplant hospitals, non-transplant hospitals admitted older patients, proportionally more females, and lower proportions of black and Hispanic patients. Nontransplant hospitals had a greater proportion of Medicare payer admissions, and transplant facilities had more Medicaid and private payer admissions.
TABLE 1.
Patient characteristics in hospitalizations for CVD after kidney transplantation, 2005-2011
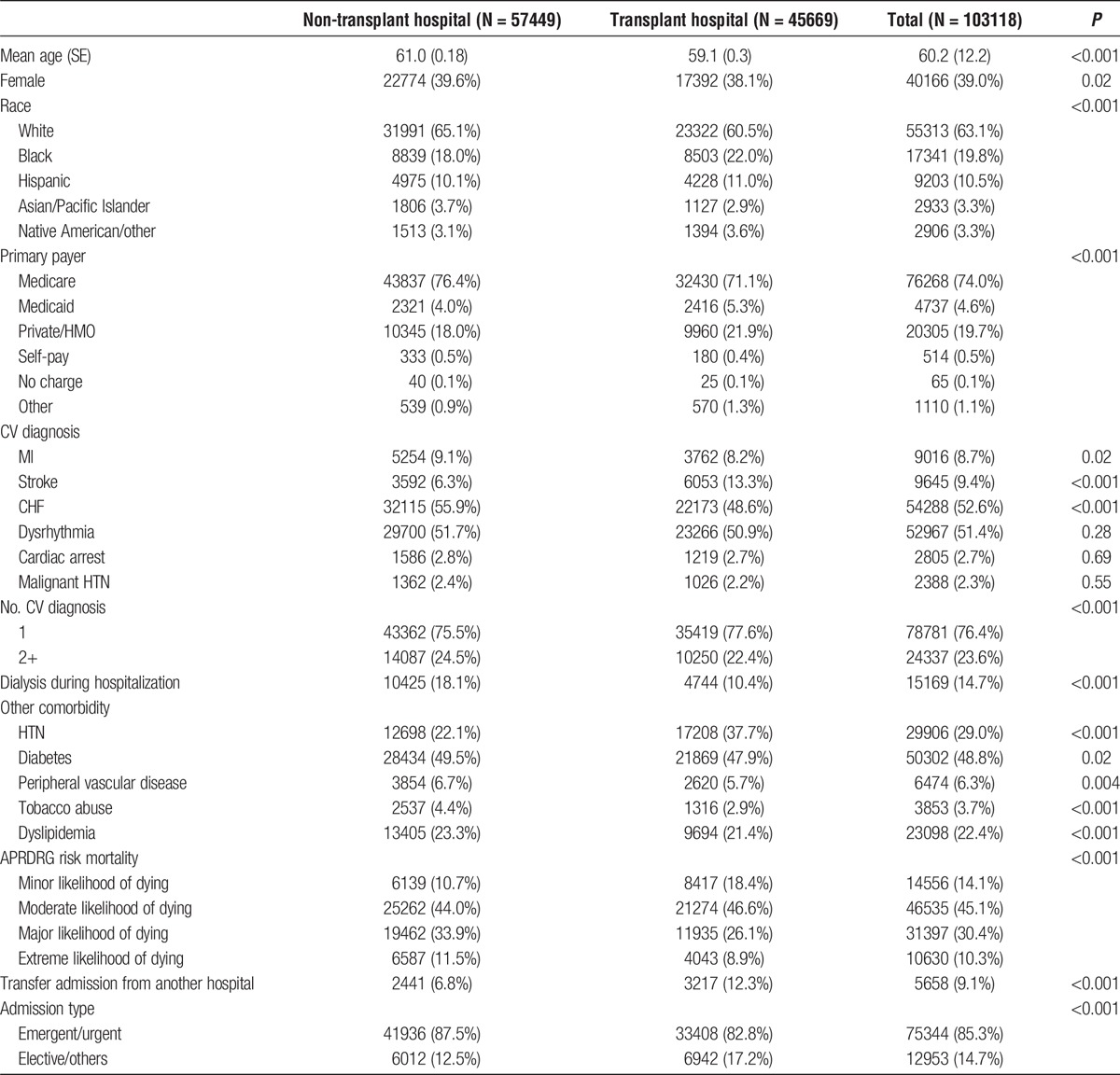
Differences in Admission Diagnoses
Non-transplant hospitals had significantly more admissions for MI and CHF, and less for stroke. Additionally, these hospitals had more patients with multiple CV diagnoses. With regard to comorbidity burden, non-transplant hospitals had significantly more patients with diabetes mellitus, peripheral vascular disease, tobacco abuse, dyslipidemia, and higher APR-DRG risk scores for mortality risk.
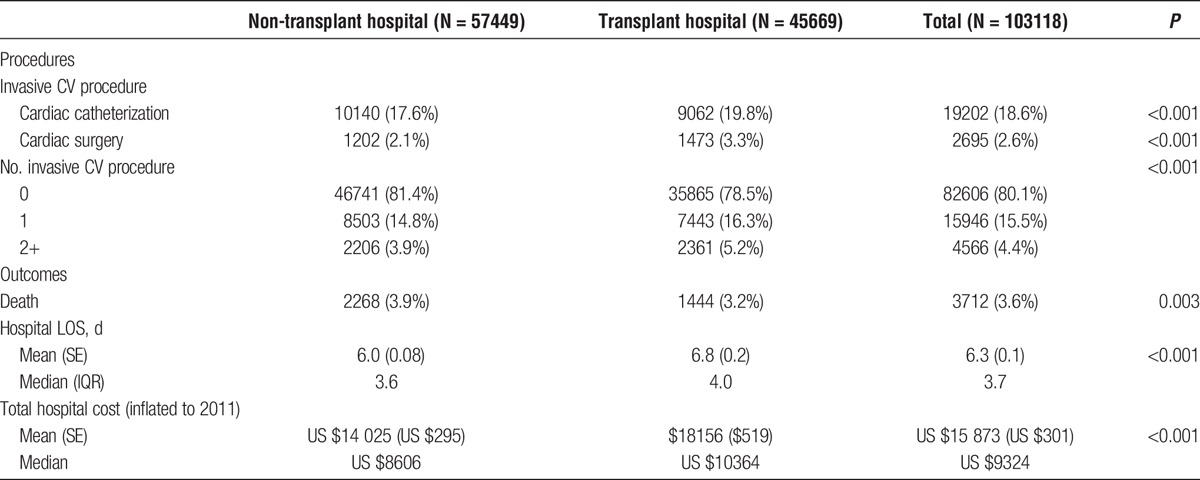
Differences in Care Utilization
In this cohort, dialysis utilization could represent acute graft dysfunction or a failed kidney allograft, and was present in 14.7% of all admissions, with significantly more in nontransplant hospitals (18.1% vs 10.4%, P < 0.001). Table 2 displays overall invasive CV procedure utilization, as well as clinical and financial outcomes of CVD hospitalizations in the postkidney transplant population. Across the entire cohort, nearly 20% of hospitalization episodes included invasive CV procedural utilization, which were more common in nontransplant hospitals. The most common procedures were diagnostic and therapeutic cardiac catheterization, which were observed in 18.6% hospitalizations. Cardiac surgical procedures occurred in 2.6% of CVD hospitalizations, and were significantly more common in transplant hospitals. Transplant hospitals had 1.3-fold more hospitalizations with multiple (≥2) CV procedures, concomitant with more elective admissions, yet received a higher proportion of inter-hospital transfers for CVD admission compared with nontransplant hospitals. Length of stay (LOS) and total inpatient cost per episode were rightward skewed, but median LOS was 3.6 and 4.0 days at non-transplant and transplant facilities, respectively. Admission episodes at transplant hospitals cost US $1758 more than at non-transplant hospitals.
TABLE 2.
Cardiovascular procedural utilization and clinical outcomes in post-kidney transplantation, 2005-2011
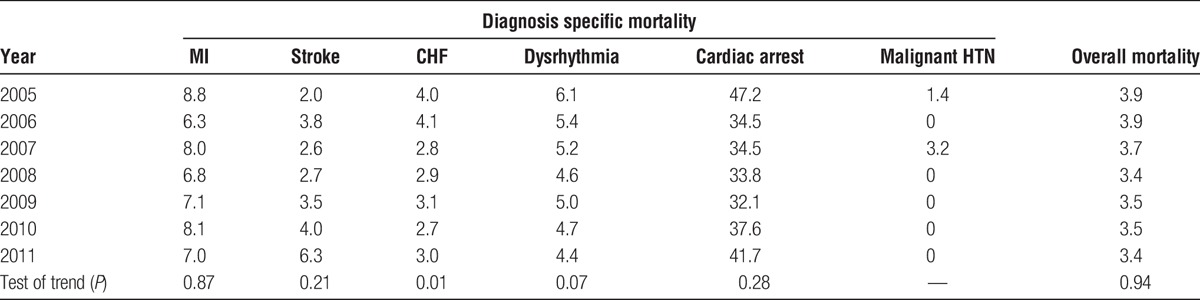
Trends in Unadjusted Mortality
Mortality in cardiovascular hospitalizations was 3.6% overall, with no significant trend over time (Table 3). By diagnosis, the absolute mortality for MI declined over the study period by 1.8%, but this was not statistically significant. Stroke mortality increased over the study period, but this did not reach statistical significance. CHF mortality declined significantly, by 1.0% over the study period (P < 0.01). Cardiac arrest had approximately 32% to 47% mortality in all years of the study, and mortality attributable to malignant hypertension was negligible.
TABLE 3.
Trends in in-hospital mortality (%) by cardiovascular diagnosis, 2005-2011
DISCUSSION
The clinical and economic burden of CVD in the postkidney transplant population is both significant and increasing. Using population-based data representing the United States between 2005 and 2011, we observed changes over time in inpatient health care utilization, differences by hospital type, and in clinical and financial outcomes. 30% of all post-transplant hospitalizations were linked to CVD in 2011. These data are important in the context of kidney disease population health, and sharpen hypotheses on determinants of clinical outcomes in CVD in this population.
Recent single center and large population data indicate that cardiovascular events after kidney transplantation are not growing in incidence.5,6 However, our data indicate that post-transplant patients have a notable burden of CVD events, and CVD hospitalizations as a proportion of all post-transplant hospitalizations are increasing. The difference between these studies may be related to differences in event rates within a single-center subgroup versus larger populations, definitions of what constitutes CVD, as well as differences in temporal ascertainment of CVD events after transplant between clinical and administrative data. Further studies, perhaps with linkages to pre-transplant data, would be helpful in framing future clinical interventions.
Several studies indicate that post-transplant CVD events are related to the exacerbation of pre-transplant risk factors.14 Before transplant, patients with CKD and ESRD are at significantly increased risk for CVD events and hospitalization.15-19 Careful selection of transplant candidates from this population would imply that the post-kidney transplant population would have low rates of CVD events.20 Certainly, early post-transplant events may be related to pretransplant risk factors, but later events may be more intrinsically related to decline in allograft function. Clinically, as kidney allograft function declines, post-transplant patients develop CKD, and are greater risk of mortality from CVD events as they approach ESRD.21,22 This is likely related to accelerated atherosclerosis, the occurrence of post-transplant diabetes, and other factors.23-25 Further analysis is needed to identify causative mechanisms behind these events, and prospective studies are warranted.
Several trends in this analysis allude to problems in posttransplant health care delivery as a potential mechanism for increases in health care utilization for post-transplant CVD, including treatment, outcome, and financial differences by hospital type. Post-transplant providers may not be addressing CVD event prevention, such as the low utilization of cardioprotective medication use, which requires further study.26,27 However, once CV events occur, hospital care drives outcomes. It is well-established that hospital characteristics are significant predictors of rescue from life-threatening complications in complex cardiovascular care and other conditions.28-30 Costs and health care utilization are known to vary across hospitals for episodes of kidney transplant care, so the findings related specifically to CVD are not altogether that surprising.31 Interestingly, while the most significant growth in cardiovascular hospitalizations was in non-transplant hospitals, transplant hospitals performed proportionally more procedures and had longer lengths of stay. This could be related to referral patterns for complex procedures, or selective referral of “risky” patients not accounted for in the data.32 The degree of variation between hospitals represents an important area for further research.
This analysis has limitations, particularly related to the data source used. These data are useful to understand an overview of post-transplant CVD. The timing of these events relative to transplant is unknowable as hospitalizations are not linked, and therefore predictors that may have a longitudinal effect on CVD events are not testable with these data. Another potential criticism is that administrative data may not capture all of the cardiovascular events that occurred due to problems with coding discharge diagnoses. Lentine et al33 have previously shown that administrative data on kidney transplant hospitalizations have sensitivity in detecting cardiovascular diagnoses, but these data do not capture the clinical detail required to determine severity of disease, intensity of cardiovascular care, and specifics of clinical outcomes. Similarly coded discharges could represent very different care trajectories for different patients. Further, we cannot ascertain how many unique patients represented this number of hospitalizations. We attempted to mitigate issues with data heterogeneity by selecting hospitalizations with a primary cardiovascular diagnosis. Finally, this study represents a deeper look at concerning trends for an important predictor of outcome in post-kidney transplant care, but does not explore the mechanisms responsible for these phenomena. Despite the limitations, this study brings concerning postkidney transplant population trends to the forefront, provides a glance at the extent of variation in CVD management in this population, and sets the stage for future studies aimed at identifying solutions.
Inpatient health care utilization for post-transplant CVD is a significant problem, and there are demonstrable differences in patterns of care. Future studies can be targeted toward several areas. Better risk factor management may have the potential to decrease CVD event rates, which could be evaluated with clinical interventions using prospective cohorts. Variation in care delivery and outcomes could be driven by differences in hospital structure and process. Future studies in this area should explore why health care utilization varies in these patients, which population subgroups have the greatest variation, and whether variation is attributable to structure of care delivery, processes of care, or both.34
In summary, CVD is a growing cause of post-transplant hospitalizations, and clinical outcomes for cardiovascular events vary between hospitals. This is a significant challenge in post-kidney transplant clinical management. It is incumbent on the transplant community to partner with clinical providers and researchers to optimize care delivery to this unique population.
Footnotes
Published online 16 January 2017.
The authors have no funding or conflicts of interest.
All authors contributed to conception and design of the study, acquisition of data, analysis and interpretation of data, drafting the article, and critically revising the article for intellectual content.
REFERENCES
- 1.Port FK, Wolfe RA, Mauger EA, et al. Comparison of survival probabilities for dialysis patients vs cadaveric renal transplant recipients. JAMA. 1993;270:1339–1343. [PubMed] [Google Scholar]
- 2.Wolfe RA, Ashby VB, Milford EL, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341:1725–1730. [DOI] [PubMed] [Google Scholar]
- 3.Stoumpos S, Jardine AG, Mark PB. Cardiovascular morbidity and mortality after kidney transplantation. Transpl Int. 2015;28:10–21. [DOI] [PubMed] [Google Scholar]
- 4.Liefeldt L, Budde K. Risk factors for cardiovascular disease in renal transplant recipients and strategies to minimize risk. Transpl Int. 2010;23:1191–1204. [DOI] [PubMed] [Google Scholar]
- 5.Lam NN, Kim SJ, Knoll GA, et al. The risk of cardiovascular disease is not increasing over time despite aging and higher comorbidity burden of kidney transplant recipients. Transplantation. 2016. [DOI] [PubMed] [Google Scholar]
- 6.Pilmore H, Dent H, Chang S, et al. Reduction in cardiovascular death after kidney transplantation. Transplantation. 2010;89:851–857. [DOI] [PubMed] [Google Scholar]
- 7.Valdés-Cañedo F, Pita-Fernández S, Seijo-Bestilleiro R, et al. Incidence of cardiovascular events in renal transplant recipients and clinical relevance of modifiable variables. Transplant Proc. 2007;39:2239–2241. [DOI] [PubMed] [Google Scholar]
- 8.Lentine KL, Schnitzler MA, Abbott KC, et al. Incidence, predictors, and associated outcomes of atrial fibrillation after kidney transplantation. Clin J Am Soc Nephrol. 2006;1:288–296. [DOI] [PubMed] [Google Scholar]
- 9.Lentine KL, Brennan DC, Schnitzler MA. Incidence and predictors of myocardial infarction after kidney transplantation. J Am Soc Nephrol. 2005;16:496–506. [DOI] [PubMed] [Google Scholar]
- 10.Ong SC, Gaston RS. Medical management of chronic kidney disease in the renal transplant recipient. Curr Opin Nephrol Hypertens. 2015;24:587–593. [DOI] [PubMed] [Google Scholar]
- 11.Akbari A, Hussain N, Karpinski J, et al. Chronic kidney disease management: comparison between renal transplant recipients and nontransplant patients with chronic kidney disease. Nephron Clin Pract. 2007;107:c7–c13. [DOI] [PubMed] [Google Scholar]
- 12.Rastogi A, Linden A, Nissenson AR. Disease management in chronic kidney disease. Adv Chronic Kidney Dis. 2008;15:19–28. [DOI] [PubMed] [Google Scholar]
- 13.Houchens R EA. Final Report on Calculating Nationwide Inpatient Sample (NIS) Variances for Data Years 2011 and Earlier. In. HCUP Methods Series Report 2003–02 2015.
- 14.Aalten J, Hoogeveen EK, Roodnat JI, et al. Associations between pre-kidney-transplant risk factors and post-transplant cardiovascular events and death. Transpl Int. 2008;21:985–991. [DOI] [PubMed] [Google Scholar]
- 15.Go AS, Chertow GM, Fan D, et al. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–1305. [DOI] [PubMed] [Google Scholar]
- 16.Tancredi M, Rosengren A, Olsson M, et al. The relationship between three eGFR formulas and hospitalization for heart failure in 54 486 individuals with type 2 diabetes. Diabetes Metab Res Rev. 2016;32:730–735. [DOI] [PubMed] [Google Scholar]
- 17.Yokoyama H, Araki S, Haneda M, et al. Chronic kidney disease categories and renal-cardiovascular outcomes in type 2 diabetes without prevalent cardiovascular disease: a prospective cohort study (JDDM25). Diabetologia. 2012;55:1911–1918. [DOI] [PubMed] [Google Scholar]
- 18.Nichols GA, Moler EJ. Cardiovascular disease, heart failure, chronic kidney disease and depression independently increase the risk of incident diabetes. Diabetologia. 2011;54:523–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rashidi A, Sehgal AR, Rahman M, et al. The case for chronic kidney disease, diabetes mellitus, and myocardial infarction being equivalent risk factors for cardiovascular mortality in patients older than 65 years. Am J Cardiol. 2008;102:1668–1673. [DOI] [PubMed] [Google Scholar]
- 20.Lentine KL, Hurst FP, Jindal RM, et al. Cardiovascular risk assessment among potential kidney transplant candidates: approaches and controversies. Am J Kidney Dis. 2010;55:152–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rao PS, Schaubel DE, Saran R. Impact of graft failure on patient survival on dialysis: a comparison of transplant-naive and post-graft failure mortality rates. Nephrol Dial Transplant. 2005;20:387–391. [DOI] [PubMed] [Google Scholar]
- 22.Fellström B, Jardine AG, Soveri I, et al. Renal dysfunction is a strong and independent risk factor for mortality and cardiovascular complications in renal transplantation. Am J Transplant. 2005;5:1986–1991. [DOI] [PubMed] [Google Scholar]
- 23.Shu KH, Tsai IC, Ho HC, et al. Coronary artery calcification in kidney transplant recipients with long-term follow-up. Transplant Proc. 2012;44:687–690. [DOI] [PubMed] [Google Scholar]
- 24.Maréchal C, Coche E, Goffin E, et al. Progression of coronary artery calcification and thoracic aorta calcification in kidney transplant recipients. Am J Kidney Dis. 2012;59:258–269. [DOI] [PubMed] [Google Scholar]
- 25.Santos RD. Coronary artery calcification progression and cardiovascular events in renal transplant recipients, bad inheritance from previous kidney disease: commentary on the study of Roe et al. Atherosclerosis. 2010;212:390–391. [DOI] [PubMed] [Google Scholar]
- 26.Lentine KL, Villines TC, Xiao H, et al. Cardioprotective medication use after acute myocardial infarction in kidney transplant recipients. Transplantation. 2011;91:1120–1126. [DOI] [PubMed] [Google Scholar]
- 27.Gaston RS, Kasiske BL, Fieberg AM, et al. Use of cardioprotective medications in kidney transplant recipients. Am J Transplant. 2009;9:1811–1815. [DOI] [PubMed] [Google Scholar]
- 28.Sheetz KH, Dimick JB, Ghaferi AA. Impact of hospital characteristics on failure to rescue following major surgery. Ann Surg. 2016;263:692–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ghaferi AA, Osborne NH, Birkmeyer JD, et al. Hospital characteristics associated with failure to rescue from complications after pancreatectomy. J Am Coll Surg. 2010;211:325–330. [DOI] [PubMed] [Google Scholar]
- 30.Gonzalez AA, Dimick JB, Birkmeyer JD, et al. Understanding the volume-outcome effect in cardiovascular surgery: the role of failure to rescue. JAMA Surg. 2014;149:119–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ellimoottil C, Ye Z, Chakrabarti AK, et al. Understanding inpatient cost variation in kidney transplantation: implications for payment reforms. Urology. 2016;87:88–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Etzioni DA, Wasif N, Mathur AK, et al. Impact of unaccounted risk factors on the interpretation of surgical outcomes. J Am Coll Surg. 2015;221:821–827. [DOI] [PubMed] [Google Scholar]
- 33.Lentine KL, Schnitzler MA, Abbott KC, et al. Sensitivity of billing claims for cardiovascular disease events among kidney transplant recipients. Clin J Am Soc Nephrol. 2009;4:1213–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Donabedian A. Evaluating the quality of medical care. Milbank Mem Fund Q. 1966;44:166–206. [PubMed] [Google Scholar]


