Abstract
Background
It is vitally important to seek input from key stakeholders to increase the quality and relevance of health-related research and accelerate its adoption into practice. Patients and caregivers have rarely been involved in setting research priorities in the transplantation and donation field. The objectives of this explorative study are: (i) to discuss research priorities within the Canadian National Transplant Research Program during a priority-setting exercise with patients, caregivers, organ donors and researchers and (ii) to compare the identified priorities with research published in 2 prestigious transplantation journals.
Methods
A pilot workshop attended by 10 patients and caregivers and 5 researchers was held in Montréal (Quebec, Canada) in August 2014 to identify research priorities. Priorities were identified using a thematic analysis of the workshop transcription conducted by multiple coders. These priorities were compared with the topics of research articles published in 2 major transplantation journals between 2012 and 2014.
Results
The themes of the 10 research priorities identified by study participants were related to different research domains: social, cultural, and environmental health factors (4); biomedical or clinical (4); and research about health systems and services (2). 26.7% of the research articles published were related to the identified priorities. Thirteen percent looked at ways to improve graft survival and 8.5% looked at the development of tolerance, 2 priorities identified by participants. Fewer than 5% examined the other 8 research priorities identified as important by workshop participants.
Conclusions
This is the first study reporting patients' and researchers' priorities in the field of transplantation and donation in Canada. There is a discrepancy between topics that key stakeholders find important and research published in 2 major transplantation journals. The research priorities identified during our initial workshop will be validated through a national survey and workshop.
Transplantation of solid organs and hematopoietic cells is the preferred treatment for patients with end-stage organ failure and certain malignancies. However, transplantation is associated with many physical and medical challenges, including organ shortage, complications associated with immunosuppressive drugs, acute rejection, chronic allograft dysfunction and graft loss, graft-versus-host disease, as well as psychological and social challenges such as quality of life, return to work and sexual activity. Patients, family members, and health care professionals have different views on these challenges. It is important to understand the viewpoints of different stakeholders to consider the concerns of those who may benefit from the research. Patients and caregivers have rarely been involved in setting research priorities in the field of transplantation and donation.
The Strategy for Patient-Oriented Research (SPOR), spearheaded by the Canadian Institutes of Health Research (CIHR) as part of its Patient Engagement Framework, defines patient engagement as a “meaningful and active collaboration in governance, priority setting, conducting research and knowledge translation.”1 The term patient is “an overarching term inclusive of individuals with personal experience of a health issue and informal caregivers, including family and friends.”1 Patient engagement in research can take 3 forms: consultation, collaboration and partnership, and patient-led research.2 There are several reasons why patient engagement is vitally important: (i) patients and their caregivers have an experiential expertise in their diseases and illnesses3,4; (ii) taking patients' views into account increases the quality and relevance of research, facilitates the recruitment of study participants and the dissemination of results, and accelerates the implementation of recommendations5,6; (iii) it provides new insights that could lead to innovative discoveries7; and (iv) it enhances public trust in medical research by making it more accountable and transparent.7 Studies have shown that patients may benefit from being engaged in the research process because they feel valued and important; they have the opportunity to give back to the medical community; and they are better informed about medical research, their disease and its management.8 Researchers may benefit from patients' input by gaining a deeper understanding of their needs and experiences.8 The emerging importance of patient engagement in research is evident in the recent development of several institutes and initiatives, including the Patient-Centered Outcomes Research Institute in the United States,9 the James Lind Alliance10 in the United Kingdom, and the CIHR-led SPOR in Canada.1 In Canada, researchers in the field of chronic kidney disease used the James Lind Alliance strategy to determine research priorities with patients on or nearing dialysis.11 The results were used to build a research network, funded by the SPOR-CIHR, grouping together researchers, patients and caregivers—the CAN-Solve CKD Network.12
There have been many initiatives to engage patients in priority-setting in research.11,13-16 Review of the literature identifies no other publications regarding a strategy that aims to determine the priorities of patients, caregivers and clinicians in the field of transplantation (solid organs and stem cells) and donation. The Canadian National Transplant Research Program (CNTRP) is a national research initiative designed to increase organ and tissue donation in Canada, improve graft survival, and enhance the quality of life of Canadians who receive transplants.17 The program brings together over 300 Canadian researchers in the field of donation and transplantation of solid organs and hematopoietic cells. The CNTRP aims to increase patient partnerships in research. This exercise and consultation in research agenda setting is the first step in the development of a patient partnership strategy within the CNTRP.
This article reports the results of a research prioritization exercise within the CNTRP involving transplant patients, caregivers, organ donors and researchers, and compares the priorities identified during this exercise with the topics of research articles published between 2012 and 2014 in 2 major transplantation journals: the American Journal of Transplantation (AJT) and Transplantation.
MATERIALS AND METHODS
Workshop
On August 21, 2014, a pilot workshop was held in Montréal, Quebec, Canada. The objectives of the workshop were to: (i) present theoretical perspectives on patient engagement, including examples of successful patient integration in research; and (ii) brainstorm around the main areas of uncertainty in the field of organ donation and transplantation, to identify research priorities. A purposive and snowball sample methodology was used: the sample had to be small to allow discussion (15 participants) and diverse (recipients of different organs, organ donors, patients awaiting an organ, caregivers and researchers from different fields of expertise).18 Recruitment was made either through treating physicians, the Collaboration and Patient Partnership Unit of the Université de Montréal (a patient partnership-focused organization) or a list of patients who had previously expressed their interest in participating in research projects. Patients invited had to be fluent in French. Thirteen patients and caregivers were invited: 3 heart transplant patients; 1 kidney-pancreas transplant patient; 1 liver-lung transplant patient; 1 lung transplant patient; 2 stem cell transplant patients; 1 kidney transplant patient; 1 patient waiting for a kidney transplant; 1 kidney donor; 1 kidney transplant patient’s caregiver and 1 parent of a lung transplant patient and cornea donor. Recruitment of the researchers was done through the researchers’ professional network. Ten researchers were invited: 3 in the field of stem cell transplantation, 2 in heart transplantation (1 in pediatric and 1 in adult), 2 in organ donation, 1 in bioethics, 1 in kidney transplantation, 1 in pancreatic islet transplantation. Refusals to participate were all due to unavailability at the workshop date. One stem cell transplant patient had agreed to participate but was sick on the day of the workshop. The workshop had a total of 15 participants: 10 of the 13 patients and caregivers approached, and 5 of the 10 researchers. All participants signed a participant information and consent form. The discussion was facilitated by the co-director of the Collaboration and Patient Partnership Unit of the Université de Montréal (VD), who is also a patient with a chronic disease, and who has experience in implementing patient engagement strategies and facilitating group discussions. The discussion was exploratory. Participants were asked to recall their experience related to transplantation and/or donation and to express the challenges they have faced that research should address. Each participant had time to speak before a plenary discussion with researchers. The workshop was conducted in French. It was digitally recorded and transcripts of the discussion were studied using inductive content and thematic analysis.19 NVivo (version 9) (QSR International) computer software was used. A researcher (C.D.) coded all the data obtained from the interviews, whereas an independent researcher (J.A.) coded 15% of all the transcripts to ensure validity of results.19 The rate of coding agreement was 90.8%. The workshop participants were invited to complete evaluation forms in which they could include any additional comments or insights that might not have occurred to them during the workshop discussion. The results of the analysis were sent to participants for validation. Institutional ethics approval was obtained from the Centre hospitalier de l'Université de Montréal.
Analysis of Published Research Topics Protocol
To review published research topics, the table of contents of all issues of 2 major transplantation journals—AJT and Transplantation—published between January 1, 2012, and December 31, 2014, were examined. These 2 journals were chosen because they are the most-cited journals on general transplantation. Their impact factors are ranked second and fourth in the transplantation category; the journals ranked first and third are restricted to specific organs and therefore cannot represent trends in general transplantation.20 We retrieved all research articles from the table of contents and obtained 1,658 citations with the corresponding abstract. Articles published in sections such as letters to the editor, forums and literature reviews were excluded, as most of these are not research reports per se. A total of 715 articles published in both the Original Articles and Brief Communications sections of the AJT and 943 articles published in the Rapid Communications, Basic and Experimental research, and Clinical and Translational research sections of Transplantation were collected. The titles of all references were imported into the NVivo (version 9) (QSR International) computer software.
Each reference was coded according to the 4 pillars of research defined by CIHR: (i) biomedical; (ii) clinical; (iii) research about health systems and services; and (iv) the social, cultural, and environmental factors that affect the health of populations. Biomedical and clinical themes were combined, as they are closely related and it was not relevant for the purposes of this study to distinguish between them. Each reference was also coded according to organ/tissue type, if applicable (kidney, heart, liver, lungs, pancreas, pancreatic islet, intestine, composite tissue allograft, stem cells, and corneas). Our coding scheme also included the 10 priorities identified after the workshop. If the research topic of the study was not obvious from the title, the abstract was read to ascertain the theme. A researcher (JA) coded all publication titles, whereas an independent researcher (C.D.) coded 15% of all the articles to validate the analysis. The rate of coding agreement was 99.24%. This high coding agreement can be explained by the fact that the organ category and research domain were easily coded. Descriptive statistics were performed.
RESULTS
Participant Characteristics
Patients and caregivers had diverse experiences with regard to donation and transplantation: 3 participants were heart transplant patients, 1 was a kidney-pancreas transplant patient, 1 was a liver-lung transplant patient, 1 was a lung transplant patient, 1 was a stem cell transplant patient, 1 was a patient waiting for a kidney transplant, 1 was a kidney donor, and 1 was the parent of a lung transplant patient and cornea donor. There were 4 women and 6 men in the patient/caregiver group.
The researchers (3 men and 2 women) worked in 5 different areas of transplantation and donation: intensive care and donation, translational medicine in kidney transplantation, pancreatic islet transplantation, heart transplantation, and ethics.
Research Priorities
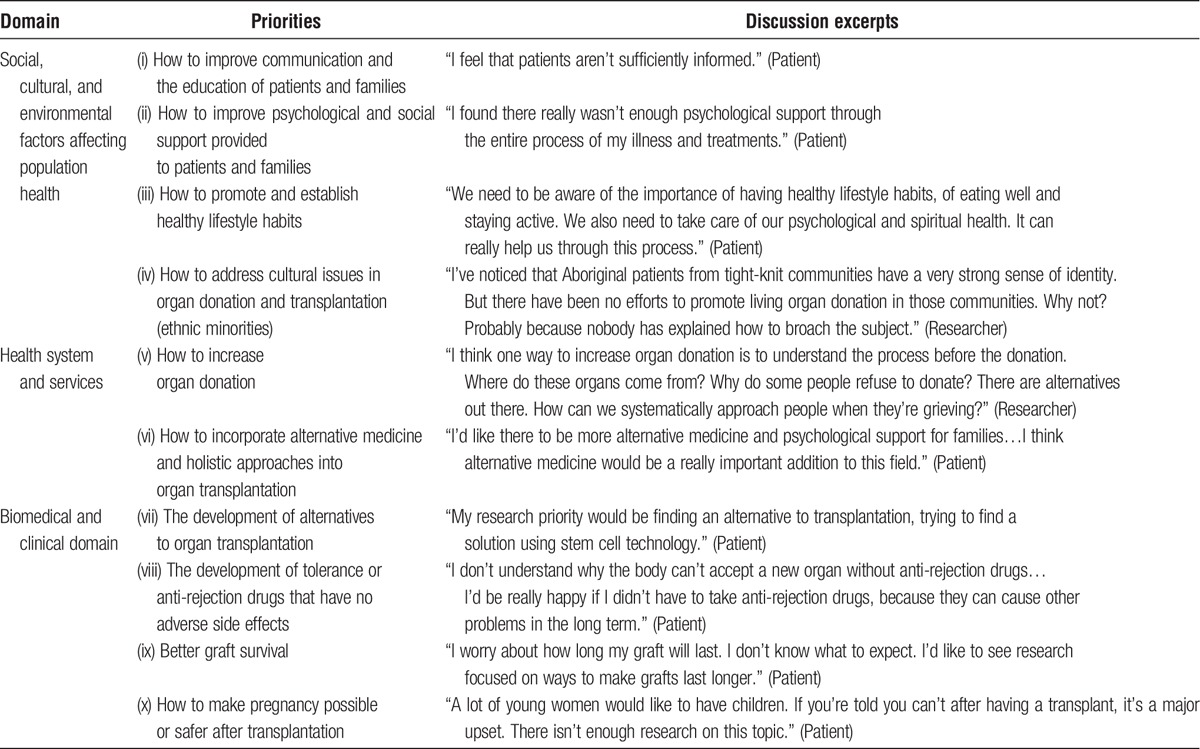
The participants identified 10 research priorities. Table 1 summarizes these findings and provides translated excerpts from the discussion. Eight priorities were primarily identified by patients and caregivers: (i) how to improve communication with patients and families and promote health literacy; (ii) how to improve psychological and social support provided to patients and families; (iii) how to promote and establish healthy lifestyle habits; (iv) how to incorporate alternative medicine and holistic approaches into organ transplantation; (v) the development of alternatives to organ transplantation, such as xenotransplantation, artificial organs, and 3-dimensional printing; (vi) the development of tolerance or antirejection drugs that have no adverse side effects; (vii) how to improve graft survival; and (viii) how to make pregnancy possible or safer after transplantation. The researchers added to this list the issues of (ix) how to address cultural issues (x) and how to increase organ donation.
TABLE 1.
Top 10 priorities in research identified by patients, caregivers and researchers
In addition to identifying research priorities, all participants in the workshop expressed concerns about how to improve knowledge translation and dissemination, and how to engage patients in research. Two excerpts from the discussion on knowledge translation and patient engagement in research are illustrative:
“I’d like us to be even more involved in research. I’d like there to be roundtable discussions, opportunities for us to get informed. It’s all very well to do tests, but we don’t know enough about the results. How was all that information used? I’d like to know. If I participate in something, I want to learn and understand why I’m participating.” (Patient) [translation]
“I never realized before today that our research is not only on patients but also for patients. From now on, this understanding is going to inform my work; how the patients on whom I’m doing research can be included in the process.” (Researcher) [translation]
Characteristics of Articles
The characteristics of the articles are summarized in Table 2. The majority of articles addressed issues related to kidney and liver transplantation. Articles were categorized as biomedical or clinical, related to the health system and services, or focused on the social, cultural and environmental factors affecting population health. Some articles were placed in more than 1 category. Around 90% of the articles were classified as biomedical or clinical, which included research in basic science, pharmacology, clinical trials and translational science. Topics covered by these articles included surgical procedures, histocompatibility, immunosuppressive drugs, causes of rejection, and postoperative complications. Only 12.9% of all the articles from AJT and Transplantation examined topics related to the health system and services or the social, cultural and environmental factors that affect population health. Research on the health system included topics such as organ allocation, kidney paired donation, the evaluation of program performance, and the effects of different policies on donor and recipient selection. Articles in the social, cultural, and environmental determinants of population health explored topics such as the impact of socioeconomic status on organ transplantation, the influence of sex or ethnicity on access to transplantation, and attitudes toward organ/tissue donation. Figure 1 shows a distribution of the articles published in each research domain for the different organs. Articles on general transplantation (not specific to an organ) and articles on kidney or liver transplantation have a higher proportion of articles in social, cultural, and environmental determinants of population health and research on the health system domains.
TABLE 2.
Article characteristics
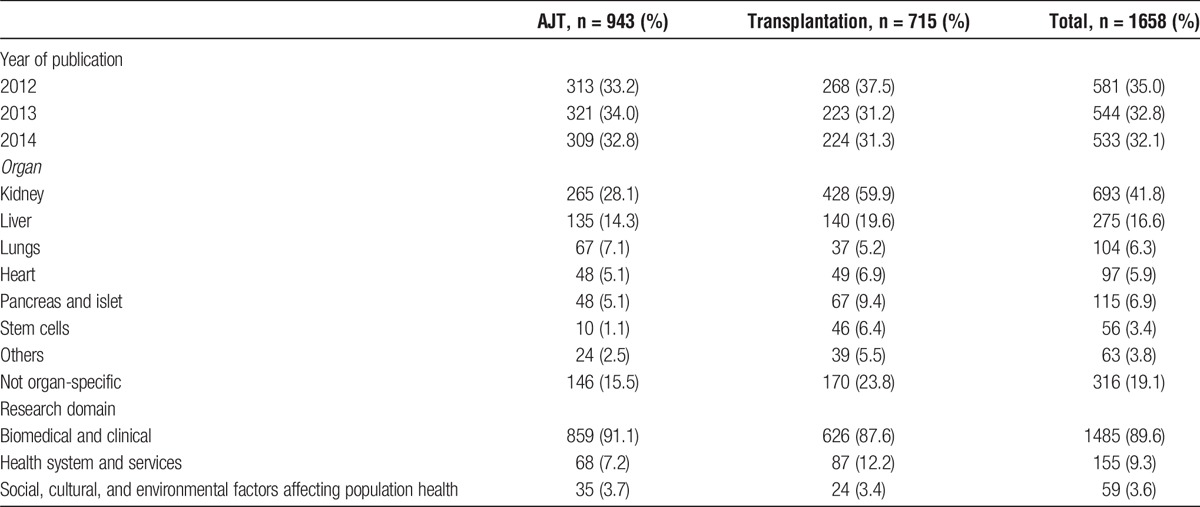
FIGURE 1.
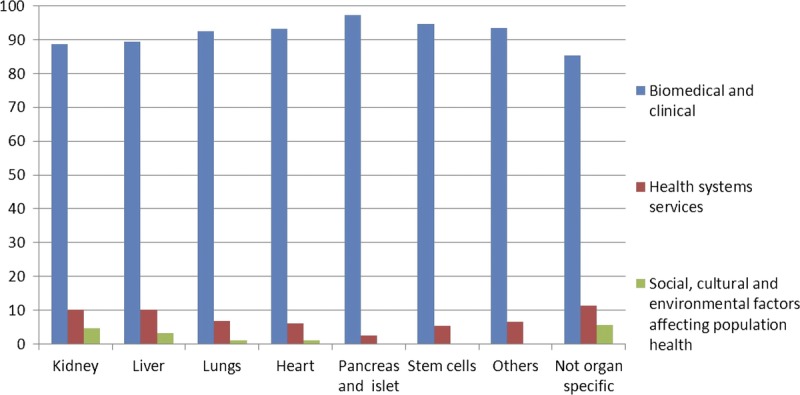
Distribution of articles published in each domain by organ.
Comparison of Priorities Identified by Patients, Caregivers, and Researchers
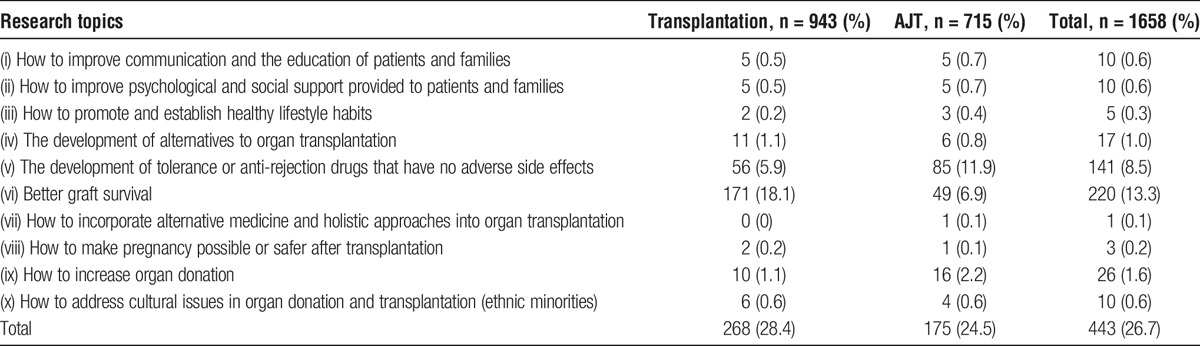
Around one quarter of the articles in each journal addresses the priorities identified by patients, caregivers and researchers during the workshop: 28.4% in Transplantation and 24.5% in AJT. Table 3 summarizes the distribution of articles according to research priorities. The 2 research priorities most covered in the publications were the development of tolerance (8.5%) and how to improve graft survival (13.3%), accounting for 82% of the articles in line with the 10 patient-identified priorities. 1.6% of articles were related to means of increasing organ donation. The 7 other patient-identified priorities were each covered by 1% or less of the articles.
TABLE 3.
Number of published articles related to patient-identified research priorities
DISCUSSION
During this pilot workshop, 10 research priorities important to transplantation patients, their caregivers, and researchers were identified. Review of the literature identifies no other publications looking at the research priorities of patients, caregivers, and researchers in the field of transplantation and donation. A recent Australian study reports on a priority-setting workshop focused on chronic kidney disease, attended by kidney transplant patients.21 Among the top 5 priorities identified, 3 were related to kidney transplantation—namely, how to improve family consent to deceased donation (taking cultural factors into account), how to improve long-term posttransplant outcomes, and how to improve and individualize drug therapy to minimize side effects.21 The priorities identified in Australia are similar to those identified during our workshop.
The priorities identified during our workshop indicate a strong interest in psychosocial research—for instance, on how to improve patient-physician communication and how to educate patients and their families, and improve psychological and social support. Clinical priorities identified by patients are directly related to their daily life, for instance, how to reduce the side effects of immunosuppressive drugs, how to improve healthy lifestyle habits, and how to make pregnancy safer after transplantation. The researchers in the workshop and the waitlisted patient identified strategies to increase organ donation as a priority. Patients who had already received an organ did not spontaneously identify organ donation as a priority, although they agreed that this was of major importance. For them, posttransplant issues, related more closely to their daily life, were of more important concern.
The workshop results show that there is a need for increased dialogue among patients, the general public, and researchers. The experiences of patients and researchers are both different and complementary. Patients draw attention to aspects of their daily life that may have been overlooked by clinicians and researchers. In contrast, researchers have a big-picture perspective that provides them with insights into research topics that affect patients' daily lives. Engaging patients in setting research priorities results in a broader range of relevant research themes.11,13 During the workshop, patients and caregivers expressed the desire to know the results of research related to their diseases and in which they sometimes participate. Knowledge translation to clinicians is known to be important for increasing the probability that research results will change bedside practice.22 However, our results suggest that patients and caregivers would like to be considered as knowledge users and should be targets of knowledge translation.
Consistent with what has been observed in other fields,23-25 our comparison of research priorities identified by patients and caregivers with research published in Transplantation and the AJT shows a significant discrepancy. 26.7% of the research published in these journals was consistent with the 10 priorities identified by the patients, caregivers and researchers in our study. Current research is mainly biomedical and clinical. The 2 priorities that are mainly biomedical—improving immunosuppressive drugs and graft survival—account for most of the studies that aligned with the priorities identified by the workshop participants in our study. The other 8 priorities combined were covered by less than 5% of the published research examined. The patients and caregivers in our workshop group also expressed a strong interest in psychosocial research, which does not receive much attention in these 2 transplantation journals.
This pilot study has limitations. First, the research priorities were identified by a small group of French-speaking patients, caregivers and clinicians mostly from the province of Quebec. The results therefore cannot be generalized. Another limitation was the fact that the group did not include family members of deceased organ donors. The researchers in the group do not represent all fields of donation and transplantation research. However, the workshop was only the first step in a process aimed at developing a Canadian patient-oriented research partnership in transplantation and donation within the CNTRP. These results are preliminary and will be validated through a national survey and workshop.
Another limitation is the scope of our analysis of published research. Our analysis was limited to 2 major transplantation journals. Had social science journals been included in our analysis, the results may have been very different. However, we believe that the main journals in transplantation should reflect the research that is generally being carried out in this field. They are also the journals of transplant organizations: the American Society of Transplantation, the American Society of Transplant Surgeons, the Transplantation Society, and the International Liver Transplantation Society. Both journals claim to be leading and influential in their field on their websites.26 The AJT website states that the journal covers all major subject areas, including ethical and social issues.26,27 Our study shows that these subjects may be underrepresented compared to clinical and biomedical issues, even though they are of major importance for end-users. These journals are the ones reaching clinicians and researchers, it is important for their readers to know that their contents may not be in line with—or may not entirely reflect—what patients and caregivers really want. Themes of major importance for patients and caregivers may have been overlooked by the research community.
CONCLUSIONS
The research priorities identified through this pilot study indicated that patients and caregivers are most interested in the psychosocial aspects of research. The analysis of research published in 2 major transplantation journals shows a discrepancy between the research that patients, caregivers and clinicians would like to see and the research that is actually published. These preliminary results will help guide future efforts to engage patients in the research process within the CNTRP. Also, the identified research priorities should influence research funding in the field of organ transplantation and donation in Canada. Our workshop is a first step toward starting a dialogue and partnership between patients, caregivers, and researchers within the CNTRP, and will be followed by a national survey and workshop with patients, caregivers, and researchers.
Footnotes
Published online 17 January, 2017.
This research project was funded by a research grant from the Canadian Institutes of Health Research.
The authors declare no conflicts of interest.
J.A. participated in the research, data analysis and writing of the article. C.D. participated in the research, data analysis and writing of the article. S.A. participated in the research design and review of the article. V.D. participated in the research design, research and review of the article. D.H. participated in the research design, research and review of the article. M.-J.H. participated in the research design and review of the article. L.W. participated in the research design and review of the article. L.W. participated in the research design, research and review of the article. M.-C.F. designed the workshop and participated in the research, data analysis and writing of the article.
REFERENCES
- 1.Canadian Institutes of Health Research. Strategy for Patient-Oriented Research—Patient Engagement Framework. 2014; http://www.cihr-irsc.gc.ca/e/48413.html. Accessed August 15, 2014.
- 2.Forsythe LP, Ellis LE, Edmundson L, et al. Patient and stakeholder engagement in the PCORI pilot projects: description and lessons learned. J Gen Intern Med. 2016;31:13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Caron-Flinterman JF, Broerse JE, Bunder JF. The experiential knowledge of patients: a new resource for biomedical research? Soc Sci Med. 2005;60:2575–2584. [DOI] [PubMed] [Google Scholar]
- 4.Kennedy I. Patients are experts in their own field. BMJ. 2003;326:1276–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schipper K, Abma TA. Coping, family and mastery: top priorities for social science research by patients with chronic kidney disease. Nephrol Dial Transplant. 2011;26:3189–3195. [DOI] [PubMed] [Google Scholar]
- 6.Forsythe LP, Szydlowski V, Murad MH, et al. A systematic review of approaches for engaging patients for research on rare diseases. J Gen Intern Med. 2014;29(Suppl 3):S788–S800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nass P, Levine S, Yancy C. Methods for Involving Patients in Topic Generation for Patient-Centered Comparative Effectiveness Research—An International Perspective. Washington DC: Patient-Centered Outcomes Research Institute; 2012. [Google Scholar]
- 8.Brett J, Staniszewska S, Mockford C, et al. A systematic review of the impact of patient and public involvement on service users, researchers and communities. Patient. 2014;7:387–395. [DOI] [PubMed] [Google Scholar]
- 9.Patient-Centered Outcomes Research Institute. Research we support. 2014; http://www.pcori.org/research-we-support/landing/. Accessed August 11, 2014.
- 10.The James Lind Alliance. Tackling treatment uncertainties together. http://www.lindalliance.org/index.asp. Accessed August 11, 2014. [DOI] [PubMed]
- 11.Manns B, Hemmelgarn B, Lillie E, et al. Setting research priorities for patients on or nearing dialysis. Clin J Am Soc Nephrol. 2014;9:1813–1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.CAN Solve CKD Network. 2016; http://www.bcrenalagency.ca/research/research-focus/can-solve-ckd-network. Accessed August 18, 2016.
- 13.Abma TA. Patients as partners in a health research agenda setting: the feasibility of a participatory methodology. Eval Health Prof. 2006;29:424–439. [DOI] [PubMed] [Google Scholar]
- 14.Barnieh L, Jun M, Laupacis A, et al. Determining research priorities through partnership with patients: an overview. Semin Dial. 2015;28:141–146. [DOI] [PubMed] [Google Scholar]
- 15.Schipper K, Dauwerse L, Hendrikx A, et al. Living with Parkinson's disease: priorities for research suggested by patients. Parkinsonism Relat Disord. 2014;20:862–866. [DOI] [PubMed] [Google Scholar]
- 16.Tong A, Chando S, Crowe S, et al. Research priority setting in kidney disease: a systematic review. Am J Kidney Dis. 2015;65:674–683. [DOI] [PubMed] [Google Scholar]
- 17.Canadian National Transplant Research Program. Transforming transplant research in Canada. 2013; http://www.cntrp.ca/#!about/c4nz. Accessed August 15, 2014.
- 18.Poses RM, Isen AM. Qualitative research in medicine and health care: questions and controversy. J Gen Intern Med. 1998;13:32–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miles MB, Huberman MA. Qualitative data analysis: A source book of new methods. Première ed Newbury Park, CA: SAGE publications; 1984. [Google Scholar]
- 20.Thomson Reuteurs. InCites Journal Citation Reports. 2014; https://jcr.incites.thomsonreuters.com/JCRJournalHomeAction.action. Accessed february 19, 2016.
- 21.Tong A, Crowe S, Chando S, et al. Research Priorities in CKD: Report of a National Workshop Conducted in Australia. J Am Soc Nephrol. 2015;66:212–222. [DOI] [PubMed] [Google Scholar]
- 22.Canadian Institutes of Health Research. Guide to Knowledge Translation Planning at CIHR: Integrated and End-of-Grant Approaches. 2015; http://www.cihr-irsc.gc.ca/e/documents/kt_lm_ktplan-en.pdf. Accessed November 16, 2015.
- 23.Jun M, Manns B, Laupacis A, et al. Assessing the extent to which current clinical research is consistent with patient priorities: a scoping review using a case study in patients on or nearing dialysis. Can J Kidney Health Dis. 2015;2:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tallon D, Chard J, Dieppe P. Relation between agendas of the research community and the research consumer. Lancet. 2000;355:2037–2040. [DOI] [PubMed] [Google Scholar]
- 25.Crowe S, Fenton M, Hall M, et al. Patients’, clinicians’ and the research communities’ priorities for treatment research: there is an important mismatch. Res Involvem Engagem. 2015;1:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.American Journal of Transplantation. http://onlinelibrary.wiley.com/journal/10.1111/(ISSN)1600-6143/homepage/ProductInformation.html. Accessed August 22, 2016.
- 27.Transplantation. http://journals.lww.com/transplantjournal/pages/aboutthejournal.aspx. Accessed August 22, 2016.


