Abstract
Cisplatin (cis-diaminedichloroplatinum II; CDDP) is an effective anticancer drug, but it has limitations because of its nephrotoxicity. This study investigates the protective effect of N-acetylcysteine (NAC) and taurine (TAU), both individually and in combination, against CDDP nephrotoxicity in rats. For this purpose, 48 male rats were assigned into eight groups (n=6) as follows: 1) control group, 2) NAC group, 3) TAU group, 4) NAC–TAU group, 5) CDDP group, 6) CDDP–NAC group, 7) CDDP–TAU group, and 8) CDDP–NAC–TAU group. Cisplatin was administered as a single intraperitoneal injection at a concentration of 6 mg/kg. Three days after CDDP administration, NAC (50 mg/kg) and/or TAU (50 mg/kg) were administered three times weekly for four consecutive weeks. Kidney function markers in serum, urinary glucose and protein, as well as oxidant and antioxidant parameters in renal tissue were assessed. Administration of CDDP significantly elevated urinary glucose and protein, as well as serum creatinine, urea, and uric acid. Moreover, CDDP enhanced lipid peroxidation and suppressed the major enzymatic antioxidants in the kidney tissue. Treatment with NAC or TAU protected against the alterations in the serum, urine, and renal tissue when used individually along with CDDP. Furthermore, a combined therapy of both was more effective in ameliorating CDDP-induced nephrotoxicity, which points out to their synergistic effect.
Keywords: cisplatin, nephrotoxicity, oxidative stress, N-acetylcysteine, taurine
Introduction
Platinum-based chemotherapeutic agents, including cisplatin (cis-diaminedichloroplat-inum II; CDDP), are widely used for the treatment of a broad spectrum of cancers.1 However, the clinical use of CDDP is limited because of its high incidence of toxicity, mainly nephrotoxicity.2 More than 25% of patients receiving CDDP develop signs of nephrotoxicity due to its high tendency to accumulate within epithelial cells of the renal proximal tubules.3 Different mechanisms have been proposed for CDDP toxicity, including direct damage of cellular DNA, mitochondrial dysfunction, and activation of apoptotic pathway.4 Generation of reactive oxygen species (ROS) and/or suppression of the antioxidant defense system are also determinant steps in CDDP nephrotoxicity.5 The clinical use of CDDP can be enhanced by using an adjunct therapy that counteracts its adverse side effects. Several studies have demonstrated a prophylactic effect of compounds that interfere with the generation of ROS.6–8 N-acetylcysteine (NAC) is a sulfhydryl donor with multiple therapeutic properties. It has been documented to act as a free radical scavenger, mitochondrial protectant, and inhibitor of lipid peroxidation (LPO) and cellular necrosis.9 NAC also promotes liver detoxification by inhibiting xenobiotic biotransformation.10 It enhances many cellular defense mechanisms and enriches the cellular glutathione (GSH) level by acting as a precursor in the GSH synthesis pathway.11 Furthermore, NAC is capable of restoring impaired prooxidant/antioxidant balance and has been widely used as an effective antioxidant against oxidative stress both in vivo and in vitro.12,13 Taurine (2-aminoethanesulfonic acid; TAU) is the most abundant free intracellular sulfur-containing amino acid in cells and tissues. Mammals have limited ability to synthesize TAU and therefore depend primarily on their diets to replenish their body levels of this amino acid. It is essential for the development and survival of mammalian cells, especially cells of the cerebellum and kidney.14 TAU is a cytoprotective agent that has multiple physiological actions such as detoxification, osmoregulation, cell membrane stabilization, and calcium flux regulation.14 It is also an effective scavenger for hydroxyl radicals and may play a key role against oxidative stress.15 Furthermore, TAU has been reported to attenuate nephrotoxicity induced by anticancer drugs and to protect renal tubular cells from atrophy and apoptosis.16,17
In the current study, we investigated CDDP-induced alterations in serum and urinary biochemical parameters related to kidney function as well as the changes in the renal oxidant/antioxidant status of male rats. Our main interest has been focused on elucidating the possible protective effect of NAC and TAU, both individually and in combination, against CDDP-induced nephrotoxicity and oxidative stress.
Materials and methods
Chemicals and drugs
Cisplatin, NAC, and TAU were purchased from Sigma Chemicals (St Louis, MO, USA). All other chemicals and reagents used in this study were of analytical grade.
Animals
Adult male albino rats (initially weighing 180±20 g) were used in the experiments. They were obtained from the High Institute of Public Health, Alexandria University, Egypt. Animals were maintained under standard conditions (temperature: 23°C±3°C, humidity: 40%–50%, and a 12:12-h light:dark cycle) and had free access to standard rat chow and drinking water. The experimental protocol and animal handling methods of this study followed the National Institutes of Health (NIH) guidelines and were approved by the local research ethics committee at Alexandria University.
Experimental protocol
After an acclimatization period of 1 week, rats were randomly assigned to one of the following eight groups (n=6). The first group (control group) received 0.5 mL saline. Rats of the second group (NAC group) received 50 mg/kg NAC. The third group (TAU group) received 50 mg/kg TAU. The fourth group (NAC–TAU group) received the previous doses of both NAC and TAU (50 mg/kg NAC and 50 mg/kg TAU). The fifth group (CDDP group) was given a single injection of CDDP at a dose of 6 mg/kg. The sixth group (CDDP–NAC group) received the previous doses of both CDDP and NAC (6 mg/kg CDDP and 50 mg/kg NAC). The seventh group (CDDP–TAU group) received the previous doses of both CDDP and TAU (6 mg/kg CDDP and 50 mg/kg TAU). The eighth group (CDDP–NAC–TAU group) received the previous doses of CDDP, NAC, and TAU (6 mg/kg CDDP, 50 mg/kg NAC, and 50 mg/kg TAU). Doses of CDDP, NAC, and TAU were selected based on previous studies.18–20 All drugs were dissolved in physiological saline and administered intraperitoneally (ip). NAC and/or TAU were administered three times weekly for four consecutive weeks starting 3 days following CDDP administration.
Serum and urine collection and preparation of kidney homogenate
Twenty-four hours after the last dose of the treatment protocol, rats were sacrificed by fast decapitation under light ether anesthesia. Blood samples were collected from all groups. The collected blood was left to clot at room temperature and centrifuged at 3,000 rpm for 15 min at 4°C to separate the serum, which was stored at −20°C for biochemical analysis. For urine collection, the urinary bladder of rats was emptied by gentle compression of the pelvic area and pulling of the rats’ tails. The urine samples were then centrifuged, and the supernatants were collected for measuring glucose and protein concentrations. Kidneys were immediately excised, trimmed of fatty tissues, washed with physiological saline solution, and blotted between filter papers. For preparation of renal tissue homogenate, 1 g of tissue was homogenized in 10 mL potassium phosphate buffer containing 0.1 mM ethylenediaminetetraacetic acid (EDTA) and centrifuged at 3,000 rpm for 15 min. The supernatant was collected and stored at -20°C for analysis.
Body weight and kidney ratio
Body weight of each rat was recorded on the first and the last days of the experimental period for calculation of change in body weight. Moreover, kidneys were excised and weighed immediately for calculation of kidney ratio using the following formula: kidney ratio (%) = kidney weight (g) ×100/body weight (g).
Kidney function biomarkers
Levels of creatinine, urea, and uric acid were assayed spec-trophotometrically using commercially available diagnostic kits (Biodiagnostic, Cairo, Egypt) according to the manufacturer’s instructions.
Urinary protein and glucose
Urinary protein level was determined according to Lowry’s method.21 Glucose level was detected in urine using commercially available strips (Teco Diagnostics, Anaheim, CA, USA).
Determination of redox status in kidney homogenate
LPO in kidney tissue (measured as malondialdehyde [MDA]) was determined by monitoring the reaction of thiobarbituric acid (TBA) with MDA to form a colored complex that absorbs at 532 nm.22 The total antioxidant capacity (TAC) in serum was determined according to the method of Miller and Rice-Evans.23 Antioxidants in the sample inhibit the oxidation of 2,2′-azino-bis(3-ethylbenzthiazoline-6-sulfonic acid) (ABTS) to ABTS+. The amount of ABTS+ was measured at 405 nm. The activity of glutathione peroxidase (GPx) was determined as described by Paglia and Valentine.24 GPx catalyzes the oxidation of GSH to form oxidized GSH, which is converted in the presence of GSH reductase (GR) and reduced nicotinamide adenine dinucleotide phosphate (NADPH) to the reduced form and NADP+. The decrease in absorbance (A340) is directly proportional to the GPx activity. GR activity was determined by measuring the amount of NADPH consumed during the conversion of oxidized GSH to reduced GSH.25 Catalase (CAT) activity was assayed depending on the reaction of the enzyme with a known quantity of H2O2.26 In the presence of peroxidase, the remaining H2O2 reacts with 3,5-dichloro-2-hydroxybenzene sulfonic acid (DHBS) and 4-aminophenazone (AAP) to form a chromophore whose color intensity is inversely proportional to the amount of CAT in the sample. The activity of superoxide dismutase (SOD) in renal tissue was determined as described by Kakkar et al27 using nitro blue tetrazolium dye and phenazine methosulfate.
Statistical analysis
Data obtained in the current study are presented as mean ± standard error for each experimental group (n=6). These data were analyzed using analysis of variance followed by post hoc comparisons between mean values of different groups. Statistical significance was acceptable at a level of P≤0.05.
Results
Changes in body weight and kidney ratio
Administration of CDDP (6 mg/kg) significantly (P≤0.05) decreased the body weight (8.5%) (Figure 1A) and increased the kidney ratio (77.8%) (Figure 1B) compared to the control group. Administration of NAC and/or TAU to normal rats did not alter the body weight or the kidney ratio compared with the control group. Treatment of CDDP-intoxicated rats with NAC and/or TAU significantly ameliorated the reduction in body weight compared to the results in the CDDP group. Furthermore, administration of NAC and/or TAU along with CDDP significantly reduced the kidney ratio (27.7%, 22.3%, and 37.5% in CDDP–NAC, CDDP–TAU, and CDDP–NAC–TAU groups, respectively) compared to the CDDP group.
Figure 1.
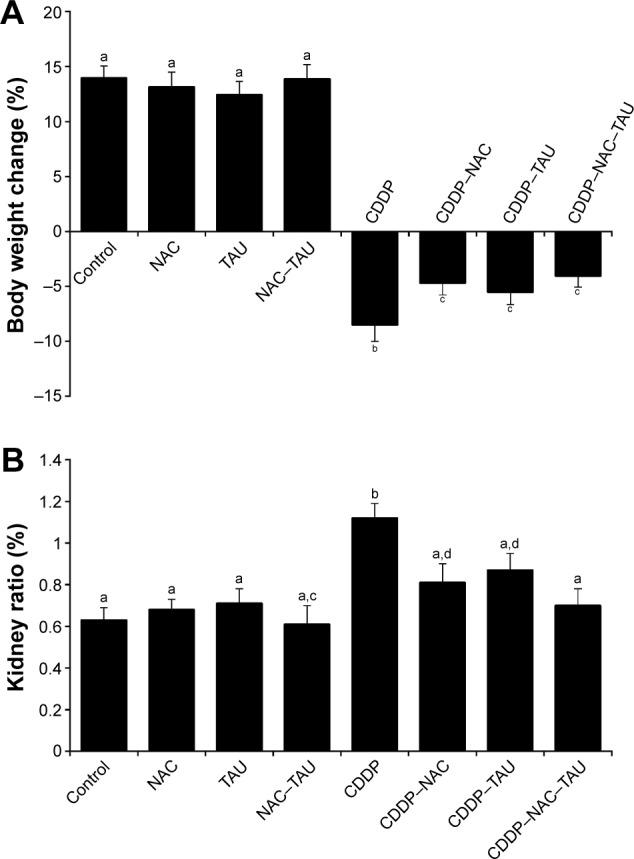
Effect of CDDP, NAC, and TAU both individually and in combination on (A) body weight change (%) and (B) kidney ratio (%) in male rats.
Notes: Data are expressed as mean ± standard error (n=6). Bars not sharing common superscript letters (a–d) are significantly different (P≤0.05).
Abbreviations: CDDP, cisplatin; NAC, N-acetylcysteine; TAU, taurine.
Changes in serum biochemical indices related to kidney function
Data presented in Table 1 reveal a significant (P≤0.05) elevation in serum biomarkers related to kidney function in rats treated with CDDP. Administration of CDDP resulted in 197.6% increase in the level of creatinine, 100.4% increase in the level of urea, and 467.6% increase in the level of uric acid compared to the control group. Administration of NAC or TAU individually to the CDDP-intoxicated rats improved the level of these kidney markers although their values remained statistically significant compared with the control group. Regarding the CDDP–NAC–TAU group, administration of NAC and TAU in combination to the CDDP-intoxicated rats significantly (P≤0.05) reduced these kidney parameters (59.2%, 46.2%, and 79.5%, respectively) compared with the CDDP group (Table 1).
Table 1.
Changes in level of creatinine, urea, and uric acid in the serum after treatment with CDDP, NAC, and TAU both individually and in combination
| Groups | Creatinine, mg/dL | Urea, mg/dL | Uric acid, mg/dL |
|---|---|---|---|
| Control | 0.84a±0.06 | 34.13a±3.39 | 0.37a±0.05 |
| NAC | 0.78a±0.08 | 30.33a±2.29 | 0.38a±0.06 |
| TAU | 0.91a±0.08 | 36.41a±2.08 | 0.54a,b±0.07 |
| NAC–TAU | 0.80a±0.05 | 33.50a±2.09 | 0.41a±0.06 |
| CDDP | 2.50c±0.18 | 68.40c±6.43 | 2.10c±0.12 |
| CDDP–NAC | 1.23b±0.07 | 40.86a,d±3.25 | 0.96b±0.04 |
| CDDP–TAU | 1.66d±0.32 | 47.20d±3.74 | 1.19d±0.13 |
| CDDP–NAC–TAU | 1.02a±0.21 | 36.80a±2.80 | 0.43a±0.06 |
Notes: Each value represents the mean ± standard error for each experimental group (n=6). Mean values within the same column not sharing a common superscript (a–d) are significantly different (P≤0.05).
Abbreviations: CDDP, cisplatin; NAC, N-acetylcysteine; TAU, taurine.
Changes in urinary excretion of glucose and protein
The effect of CDDP intoxication in addition to the role of NAC and/or TAU in urinary excretion of glucose and protein are shown in Table 2. Administration of 6 mg/kg of CDDP induced a marked and significant (P≤0.05) increase of 557.3% and 660% in urinary glucose and protein levels, respectively, compared to the control group. Supplementation with NAC (50 mg/kg) significantly reduced the levels of these markers by 57.9% and 61.2%, respectively, compared to the CDDP group. Similarly, TAU supplementation at a dose of 50 mg/kg significantly reduced these biomarkers by 44% and 54.4%, respectively, compared with the control group. Furthermore, combined supplementation with both NAC and TAU showed a more pronounced protective effect than monotherapy with each individually. Together, they reduced the urinary glucose and protein levels (76.1% and 81.9%, respectively) compared to the CDDP group (Table 2).
Table 2.
Changes in the level of urinary glucose and protein after treatment with CDDP, NAC, and TAU both individually and in combination
| Groups | Urinary glucose, mg/dL | Urinary protein, mg/dL |
|---|---|---|
| Control | 7.12a±0.43 | 0.75a±0.06 |
| NAC | 6.50a±0.60 | 0.91a±0.04 |
| TAU | 7.33a±0.54 | 1.02a±0.05 |
| NAC–TAU | 6.71a±0.66 | 0.90a±0.05 |
| CDDP | 46.80c±3.93 | 5.70c±0.26 |
| CDDP–NAC | 19.71b±1.23 | 2.21b±0.18 |
| CDDP–TAU | 26.20d±2.59 | 2.60b±0.15 |
| CDDP–NAC–TAU | 11.20a,b±0.97 | 1.03a±0.08 |
Notes: Each value represents the mean ± standard error for each experimental group (n=6). Mean values within the same column not sharing a common superscript (a–d) are significantly different (P≤0.05).
Abbreviations: CDDP, cisplatin; NAC, N-acetylcysteine; TAU, taurine.
Changes in redox status in renal tissue
As shown in Figure 2A, administration of CDDP significantly (P≤0.05) increased the level of LPO (measured as MDA) in renal tissue by 193.3% compared to the control. Treatment with either NAC or TAU individually significantly (P≤0.05) reduced the elevated LPO level in CDDP-administered rats (43.4% and 30.4%, respectively) compared with the CDDP group. Values in these groups (CDDP–NAC and CDDP–TAU) remained statistically significant compared to the control group. Furthermore, administration of both NAC and TAU in combination to the CDDP-intoxicated rats was more effective in reducing the renal LPO level (58.2%) compared to the CDDP group. Administration of CDDP significantly decreased the serum TAC (78%). Monotherapy with NAC or TAU after CDDP administration significantly increased the serum TAC compared to the CDDP group (221% and 189.5%, respectively). Furthermore, combined therapy using both NAC and TAU was more powerful in restoring the TAC compared with each monotherapy alone. Together, they increased the TAC by 336.8% compared to the CDDP group. No statistically significant difference in TAC in normal rats treated only with NAC and/or TAU was observed compared with the control group (Figure 2B).
Figure 2.
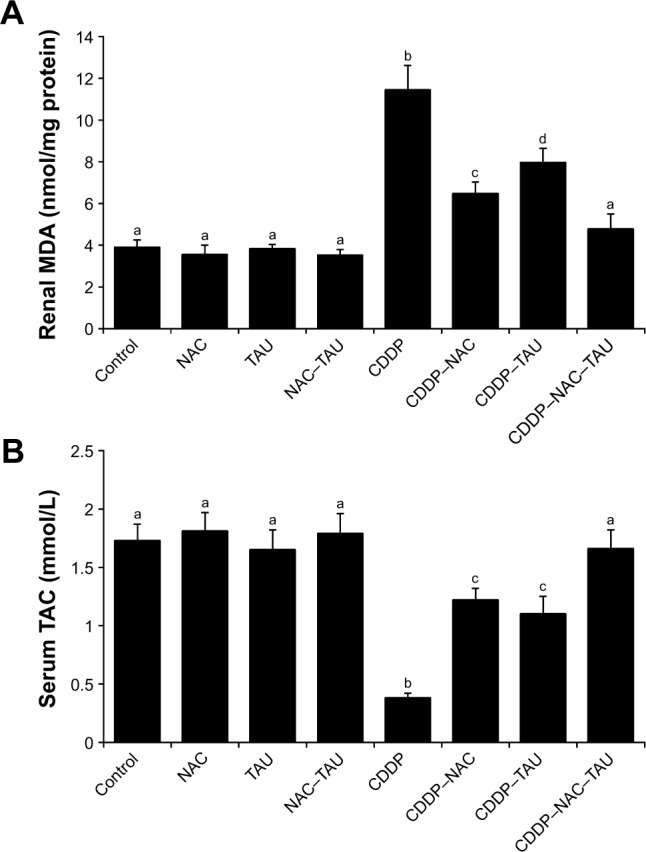
Effect of CDDP, NAC, and TAU both individually and in combination on (A) level of renal MDA (nmol/mg protein) and (B) serum TAC (mmol/L) in male rats.
Notes: Data are expressed as mean ± standard error (n=6). Bars not sharing common superscript letters (a–d) are significantly different (P≤0.05).
Abbreviations: CDDP, cisplatin; NAC, N-acetylcysteine; TAU, taurine; MDA, malondialdeyde; TAC, total antioxidant capacity.
According to Table 3, administration of CDDP suppressed the enzymatic antioxidant status of the kidney. It significantly (P≤0.05) decreased the activity of the enzymatic antioxidants GPx (76.3%), GR (61.9%), CAT (58.2%), and SOD (63.9%) in the renal tissue. Supplementation with 50 mg/kg NAC to CDDP-intoxicated rats resulted in a significant (P≤0.05) increase of 265.6%, 122.9%, 105.2%, and 143.9% in the activity of GPx, GR, CAT, and SOD, respectively, compared with the CDDP group. Moreover, supplementation with TAU individually to CDDP-administered rats significantly ameliorated the enzymatic antioxidant status, as shown by an increase in the activity of GPx, GR, CAT, and SOD by 217.2%, 99.4%, 70.3%, and 108.5%, respectively, compared with the CDDP group. Treatment of the CDDP-intoxicated rats with both NAC and TAU (CDDP–NAC–TAU group) provided maximum protection and resulted in complete recovery of the activity of the enzymatic antioxidants compared to both monotherapy groups (CDDP–NAC and CDDP–TAU groups).
Table 3.
Changes in the activity of GPx, GR, CAT, and SOD in kidney tissue after treatment with CDDP, NAC, and TAU both individually and in combination
| Groups | GPx, U/mg protein | GR, µmol/mg protein | CAT, U/mg protein | SOD, U/mg protein |
|---|---|---|---|---|
| Control | 78.33a±4.30 | 36.83a±2.79 | 56.50a±2.72 | 58.67a±3.22 |
| NAC | 79.33a±4.36 | 37.17a±2.46 | 59.83a±3.24 | 58.00a±2.61 |
| TAU | 77.33a±3.52 | 36.33a±2.39 | 58.67a±5.38 | 59.33a±5.30 |
| NAC–TAU | 78.50a±5.58 | 34.33a±1.61 | 57.17a±3.29 | 60.17a±2.98 |
| CDDP | 18.60b±1.21 | 14.04b±2.42 | 23.60b±2.11 | 21.20b±1.59 |
| CDDP–NAC | 68.0a,c±2.15 | 31.29a,c±1.66 | 48.43a,c±2.94 | 51.71a,c±3.15 |
| CDDP–TAU | 59.0c±1.58 | 28.0c±2.24 | 40.20c±3.46 | 44.20c±3.46 |
| CDDP–NAC–TAU | 77.4a±2.93 | 37.8a±2.63 | 57.40a±2.44 | 56.40a±3.93 |
Notes: Each value represents the mean ± standard error for each experimental group (n=6). Mean values within the same column not sharing a common superscript (a–c) are significantly different (P≤0.05).
Abbreviations: CDDP, cisplatin; NAC, N-acetylcysteine; TAU, taurine; GPx, glutathione peroxidase; GR, glutathione reductase; CAT, catalase; SOD, superoxide dismutase.
Discussion
Most cancer patients suffer from the adverse effects of their therapeutic drugs. CDDP is a frontline chemotherapeutic drug usually used to treat several cancers. Despite its beneficial effects, nephrotoxicity is still a major detrimental side effect of CDDP. The exact mechanism for this nephrotoxicity is not well defined, although several studies have been carried out in this regard. Previous studies have established that the generation of free radicals and induction of oxidative stress are strongly implicated in the nephrotoxicity of CDDP.28 The use of an antioxidant therapy may be effective in preventing or at least reducing the deleterious side effects of CDDP. Results of our study have demonstrated that administration of a single injection of CDDP induced signs of renal injury as manifested by the elevation of serum creatinine, urea, and uric acid, in addition to increased urinary excretion of glucose and protein. Furthermore, CDDP significantly enhanced the LPO level and suppressed the activity of the major enzymatic antioxidants in renal tissue, which further support the hypothesis that oxidative damage is one of the major factors leading to tissue damage after CDDP treatment. In an attempt to modulate CDDP-induced nephrotoxicity, NAC and TAU were administered both individually and in combination. Results illustrated a protective effect for both NAC and TAU when used individually. Furthermore, a combination of both was more efficient in attenuating CDDP-induced nephrotoxicity, which points to their synergistic protective effect.
Changes in body and organ weights are considered to be major indicators in toxicological studies. Our results revealed a significant reduction in body weight and a significant increase in kidney ratio in response to CDDP administration compared to the control. Similar results were recorded in previous studies.29,30 The observed reduction in body weight may be associated with loss of water from the body. Administration of CDDP resulted in renal tubular injury and loss of the tubular cells that reabsorb water, which subsequently increases urine volume.2,31 The observed increase in kidney ratio might be due to edema of renal parenchyma because CDDP is known to induce renal inflammation.29,32
Changes in serum biomarkers related to kidney function are important indicators for renal dysfunction. Proteinuria and glycosuria are also considered to be signs of development of nephropathy.33 In our study, CDDP induced renal injury as manifested by an increase in the serum level of creatinine, urea, and uric acid. These results are in agreement with previous studies.34,35 Furthermore, CDDP-administered rats had an increased excretion of glucose and protein in urine, which is in accordance with previous studies.36,37 Elevation in these markers may be a result of progressive injury in the renal vasculature as a secondary event following CDDP-induced increase in ROS. Injury in the renal vasculature causes contraction of mesangial cells and alters the filtration surface area, leading to a decline in the glomerular filtration rate.38 Furthermore, CDDP can reduce the renal blood flow and increase the renal vascular resistance.39
ROS generated by toxicants and many drugs play a key role in cellular injury and in the pathogenesis of several diseases. Our study confirms that the administration of CDDP increases the level of LPO in renal tissue (measured as MDA), making the kidney more vulnerable to damage by oxygen radicals. These results are in line with those of previous reports.34,40 CDDP has the ability to induce highly reactive free radicals such as H2O2, superoxide anions, and hydroxyl radicals. These radicals can directly interact with many subcellular components, including DNA, proteins, lipids, and other macromolecules and eventually trigger cell death.8 When ROS are produced extensively, cells activate their different antioxidant defense mechanisms to counteract these reactive species. Reduction in the activity of one or more component of the antioxidant system due to toxicants or drugs results in oxidative stress. In the current study, a marked suppression in the activity of the major antioxidant enzymes (GPx, GR, SOD, and CAT) was detected in the renal tissue following CDDP administration. These results support the hypothesis that CDDP toxicity is associated with depletion of the antioxidant defense system. A similar decline in the activity of the enzymatic antioxidants was reported in several studies.6,41,42 The decline in the enzymatic antioxidants, along with the increase in LPO, indicates that the enzymes are being consumed in combating the increased free radical production in renal tissue. The change in oxidant/antioxidant balance following CDDP administration points out to a state of oxidative stress in the kidney, which may be responsible for the observed perturbations in the biochemical markers.
NAC is a sulfur-containing amino acid that mimics the effect of naturally occurring antioxidants. In this study, administration of NAC attenuated CDDP-induced nephro-toxicity and restored proper kidney functioning. This was evidenced by the restoration of serum creatinine, urea, uric acid, as well as the urinary glucose and protein values to levels near the control value. Furthermore, renal MDA level was significantly reduced and the activity of the major enzymatic antioxidants was markedly enhanced in renal tissue compared to the CDDP treated group. These results are in agreement with previous studies that illustrated a protective effect of NAC against CDDP-induced nephrotoxicity in rats.43,44 The beneficial effects of NAC are related to its activity as a powerful free radical scavenger. Its free sulfhydryl group can react directly with electrophilic compounds such as free radicals.45 It also enhances the synthesis of cellular GSH and hence potentiates the endogenous antioxidant mechanism.11 This may explain the ability of NAC to restore the activity of antioxidant enzymes in the kidney in our study. NAC was found to be able to modulate the disturbed renal blood flow caused by inferior vena cava occlusion by the scavenging of free radicals.46 It also ameliorated the reduced renal vascular resistance caused by CDDP.47 The effect of NAC on the renal blood flow and vascular resistance in CDDP-intoxicated rats may explain the observed improvement in the renal function. The protective effect of NAC may also be related to its ability to reduce the concentration of platinum in the kidney by increasing its renal excretion and/or preventing its accumulation in the renal tissue.43
TAU supplementation in our study significantly mitigated CDDP-induced nephrotoxicity and oxidative stress. The protective effect of TAU was evidenced by the apparent improvement in the biochemical variables determining nephrotoxicity in serum and urine. Furthermore, TAU inhibited LPO and enhanced the activity of GPx, GR, SOD, and CAT in the renal tissue. Consistent with our results, TAU has been documented to protect against nephrotoxicity and oxidative damage induced by various drugs and free radical-generating compounds.16,17,48 TAU has multiple actions and therefore can attenuate oxidative injury and its subsequent alterations in biochemical parameters. It can bind directly to free radicals to form less-reactive molecules.49 TAU has been proposed to be a membrane stabilizer that maintains membrane permeability and prevents ion leakage associated with oxidative injury.50 CDDP administration can disturb calcium homeostasis because it damages renal tubular cells that reabsorb calcium.51 TAU may protect against CDDP toxicity by regulating calcium fluxes.14 Furthermore, the protective effect of TAU against CDDP-induced renal injury may be related to its ability to enhance the activity of the endogenous antioxidants.17,52 One or more of these actions may be responsible for the protective effect of TAU against CDDP-induced nephrotoxicity.
Conclusion
CDDP impaired proper kidney functioning and disturbed the renal oxidant/antioxidant status. Administration of NAC individually significantly protected against CDDP-induced renal failure. Furthermore, the detrimental effects of CDDP were reversed by treatment with TAU. The use of a combined therapy of both NAC and TAU was more effective than each monotherapy, which clearly points out to their synergistic protective effect. The therapeutic effects of NAC and TAU are largely attributed to their unique cytoprotective actions and their ability to restore the activity of enzymatic antioxidants in renal tissue. Further studies are needed to explore the exact molecular mechanism responsible for the nephroprotective effect of NAC and TAU to establish their feasible application as a prophylactic adjunct during CDDP therapy.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Zhang J, Wang L, Xing Z, et al. Status of bi- and multi-nuclear platinum anticancer drug development. Anticancer Agents Med Chem. 2010;10(4):272–282. doi: 10.2174/187152010791162270. [DOI] [PubMed] [Google Scholar]
- 2.Ali BH, Al-Moundhri MS. Agents ameliorating or augmenting the nephrotoxicity of cisplatin and other platinum compounds. Food Chem Toxicol. 2006;44(8):1173–1183. doi: 10.1016/j.fct.2006.01.013. [DOI] [PubMed] [Google Scholar]
- 3.Humanes B, Lazaro A, Camano S, et al. Cilastatin protects against cisplatin-induced nephrotoxicity without compromising its anticancer efficiency in rats. Kidney Int. 2012;82(6):652–663. doi: 10.1038/ki.2012.199. [DOI] [PubMed] [Google Scholar]
- 4.Siddik ZH. Cisplatin: mode of cytotoxic action and molecular basis of resistance. Oncogene. 2003;22(47):7265–7279. doi: 10.1038/sj.onc.1206933. [DOI] [PubMed] [Google Scholar]
- 5.Hagar H, El-Medany A, Salam R, El-Medany G, Nayal O. Betaine supplementation mitigates cisplatin induced nephrotoxicity by abrogation of oxidative/nitrosative stress and suppression of inflammation and apoptosis in rats. Exp Toxicol Pathol. 2015;67(2):133–141. doi: 10.1016/j.etp.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 6.Abouzeinab NS. Antioxidant effect of silymarin on cisplatin-induced renal oxidative stress in rats. J Pharmacol Toxicol. 2015;10(1):1–19. [Google Scholar]
- 7.Saad AA, Youssef MI, El-Shennawy LK. Cisplatin induced damage in kidney genomic DNA and nephrotoxicity in male rats: the protective effect of grape seed proanthocyanidin extract. Food Chem Toxicol. 2009;47(7):1499–1506. doi: 10.1016/j.fct.2009.03.043. [DOI] [PubMed] [Google Scholar]
- 8.Satoh M, Kashihara N, Fujimoto S, et al. A novel free radical scavenger, edarabone, protects against cisplatin-induced acute renal damage in vitro and in vivo. J Pharmacol Exp Ther. 2003;305(3):1183–1190. doi: 10.1124/jpet.102.047522. [DOI] [PubMed] [Google Scholar]
- 9.Samuni Y, Goldstein S, Dean O, Berk M. The chemistry and biological activities of N-acetylcysteine. Biochim Biophys Acta. 2013;1830(8):4117–4129. doi: 10.1016/j.bbagen.2013.04.016. [DOI] [PubMed] [Google Scholar]
- 10.De Vries N, De Flora S. N-acetylcysteine. J Cell Biochem. 1993;17F:S270–S277. [Google Scholar]
- 11.Yalcin S, Bilgili A, Onbasilar I, Eraslan G, Ozdemir M. Synergistic action of sodium selenite and N-acetylcysteine in acetaminophen induced liver damage. Hum Exp Toxicol. 2008;27(5):425–429. doi: 10.1177/0960327108094612. [DOI] [PubMed] [Google Scholar]
- 12.Campos R, Shimizu MH, Volpini RA, et al. N-acetylcysteine prevents pulmonary edema and acute kidney injury in rats with sepsis submitted to mechanical ventilation. Am J Physiol Lung Cell Mol Physiol. 2012;302(7):L640–L650. doi: 10.1152/ajplung.00097.2011. [DOI] [PubMed] [Google Scholar]
- 13.Srivastava RK, Rahman Q, Kashyap MP, Lohani M, Pant AB. Ameliorative effects of dimetylthiourea and N-acetylcysteine on nanoparticles induced cytogenotoxicity in human lung cancer cells-A549. PLoS One. 2011;6(9):e25767. doi: 10.1371/journal.pone.0025767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huxtable RJ. Physiological actions of taurine. Physiol Rev. 1992;72(1):101–163. doi: 10.1152/physrev.1992.72.1.101. [DOI] [PubMed] [Google Scholar]
- 15.Oliveira M, Minotto J, De Oliveira M, et al. Scavenging and antioxidant potential of physiological taurine concentrations against different reactive oxygen/nitrogen species. Pharmacol Rep. 2010;62(1):185–193. doi: 10.1016/s1734-1140(10)70256-5. [DOI] [PubMed] [Google Scholar]
- 16.Saad SY, Al-Rikabi AC. Protection effects of taurine supplementation against cisplatin-induced nephrotoxicity in rats. Chemotherapy. 2002;48(1):42–48. doi: 10.1159/000048587. [DOI] [PubMed] [Google Scholar]
- 17.Tabassum H, Parvez S, Rehman H, Banerjee BD, Siemen D, Raisuddin S. Nephrotoxicity and its prevention by taurine in tamoxifen induced oxidative stress in mice. Hum Exp Toxicol. 2007;26(6):509–518. doi: 10.1177/0960327107072392. [DOI] [PubMed] [Google Scholar]
- 18.Ali BH, Al-Moundhri MS, Tageldin M, et al. Ontogenic aspects of cisplatin-induced nephrotoxicity in rats. Food Chem Toxicol. 2008;46(11):3355–3359. doi: 10.1016/j.fct.2008.07.030. [DOI] [PubMed] [Google Scholar]
- 19.Shalby A, Assaf N, Ahmed H. Possible mechanisms for N-acetylcysteine and taurine in ameliorating acute renal failure induced by cisplatin in rats. Toxicol Mech Methods. 2011;21(7):538–546. doi: 10.3109/15376516.2011.568985. [DOI] [PubMed] [Google Scholar]
- 20.Sener G, Sehirli O, Ipçi Y, et al. Protective effects of taurine against nicotine-induced oxidative damage of rat urinary bladder and kidney. Pharmacology. 2005;74(1):37–44. doi: 10.1159/000083245. [DOI] [PubMed] [Google Scholar]
- 21.Lowry OH, Rosebrough NJ, Farr AL, Randall RJ. Protein measurement with the Folin phenol reagent. J Biol Chem. 1951;193(1):265–275. [PubMed] [Google Scholar]
- 22.Ohkawa H, Ohishi N, Yagi K. Assay for lipid peroxidation in animal tissues by thiobarbituric acid reaction. Ann Biochem. 1979;95(2):351–358. doi: 10.1016/0003-2697(79)90738-3. [DOI] [PubMed] [Google Scholar]
- 23.Miller N, Rice-Evans C. Spectrophotometric determination of antioxidant activity. Redox Rep. 1996;2(3):161–171. doi: 10.1080/13510002.1996.11747044. [DOI] [PubMed] [Google Scholar]
- 24.Paglia DE, Valentine WN. Studies on quantitative and qualitative characterization of erythrocyte glutathione peroxidase. J Lab Clin Med. 1967;70(1):158–169. [PubMed] [Google Scholar]
- 25.Carlberg I, Mannervik B. Glutathione reductase. Methods Enzymol. 1985;113:484–490. doi: 10.1016/s0076-6879(85)13062-4. [DOI] [PubMed] [Google Scholar]
- 26.Aebi H. Catalase in vitro. Methods Enzymol. 1984;105:121–126. doi: 10.1016/s0076-6879(84)05016-3. [DOI] [PubMed] [Google Scholar]
- 27.Kakkar P, Das B, Viswanathan PN. A modified spectrophotometric assay of superoxide dismutase. Indian J Biochem Biophys. 1984;21(2):130–132. [PubMed] [Google Scholar]
- 28.Peres LA, da Cunha AD. Acute nephrotoxicity of cisplatin: molecular mechanisms. J Bras Nefrol. 2013;35(4):332–340. doi: 10.5935/0101-2800.20130052. [DOI] [PubMed] [Google Scholar]
- 29.Anusuya N, Durgadevi P, Dhinek A, Mythily S. Nephroprotective effect of ethanolic extract of garlic (Allium sativum) on cisplatin induced nephrotoxicity in male Wistar rats. Asian J Pharm Clin Res. 2013;6:97–100. [Google Scholar]
- 30.Shimeda Y, Hirotani Y, Akimoto Y, et al. Protective effects of capsaicin against cisplatin-induced nephrotoxicity in rats. Biol Pharm Bull. 2005;28(9):1635–1638. doi: 10.1248/bpb.28.1635. [DOI] [PubMed] [Google Scholar]
- 31.Muthuraman A, Singla SK, Peters A. Exploring the potential of flunarizine for cisplatin-induced painful uremic neuropathy in rats. Int Neurourol J. 2011;15(3):127–134. doi: 10.5213/inj.2011.15.3.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Adejuwon AS, Femi-Akinlosotu OM, Omirinde JO, Owolabi OR, Afodun AM. Launaea taraxacifolia ameliorates cisplatin-induced hepatorenal injury. Eur J Med Plants. 2014;4(5):528–541. [Google Scholar]
- 33.Zipp T, Schelling JR. Diabetic nephropathy. In: Hricik DE, Miller RT, Sedor JR, editors. Nephrology Secrets. Hanley and Belfus Inc. Medical Publishers; Philadelphia: 2003. pp. 105–108. [Google Scholar]
- 34.Danduga RC, Kumar GS, Kumar KP, Swamy BM, Kishore KV. Nephroprotective activity of Cissampelos pareira extract against cisplatin induced nephrotoxic rats. Am J Pharm Tech Res. 2015;5:480–488. [Google Scholar]
- 35.Palipoch S, Punsawad C. Biochemical and histological study of rat liver and kidney injury induced by cisplatin. J Toxicol Pathol. 2013;26(3):293–299. doi: 10.1293/tox.26.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Atessahin A, Yilmaz S, Karahan I, Ceribasi AO, Karaoglu A. Effects of lycopene against cisplatin-induced nephrotoxicity and oxidative stress in rats. Toxicology. 2005;212(2–3):116–123. doi: 10.1016/j.tox.2005.04.016. [DOI] [PubMed] [Google Scholar]
- 37.Portilla D, Li S, Nagothu K, et al. Metabolomic study of cisplatin-induced nephrotoxicity. Kidney Int. 2006;69(12):2194–2204. doi: 10.1038/sj.ki.5000433. [DOI] [PubMed] [Google Scholar]
- 38.Noori S, Mahboob T. Antioxidant effect of carnosine pretreatment on cisplatin-induced renal oxidative stress in rats. Indian J Clin Biochem. 2010;25(1):86–91. doi: 10.1007/s12291-010-0018-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hye Khan MA, Sattar MA, Abdullah NA, Johns EJ. Influence of cisplatin-induced renal failure on the alpha-1-adrencoeptor subtype causing vasoconstriction in the kidney of the rat. Eur J Pharmacol. 2007;569(1–2):110–118. doi: 10.1016/j.ejphar.2007.04.063. [DOI] [PubMed] [Google Scholar]
- 40.Ognjanović BI, Djordjević NZ, Matić MM, et al. Lipid peroxidative damage on cisplatin exposure and alterations in antioxidant defense system in rat kidneys: a possible protective effect of selenium. Int J Mol Sci. 2012;13(2):1790–1803. doi: 10.3390/ijms13021790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ajith TA, Usha S, Nivitha V. Ascorbic acid and α-tocopherol protect anticancer drug cisplatin-induced nephrotoxicity in mice. Clin Chim Acta. 2007;375(1–2):82–86. doi: 10.1016/j.cca.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 42.Naziroglu M, Karaoglu A, Aksoy AO. Selenium and high dose vitamin E administration protects cisplatin-induced oxidative damage to renal, liver and lens tissues in rats. Toxicology. 2004;195(2–3):221–230. doi: 10.1016/j.tox.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 43.Appenroth D, Winnefeld K, Schroter H, Rost M. Beneficial effect of N-acetylcysteine on cisplatin nephrotoxicity in rats. J Appl Toxicol. 1993;13(3):189–192. doi: 10.1002/jat.2550130309. [DOI] [PubMed] [Google Scholar]
- 44.Dickey DT, Muldoon LL, Doolittle ND, Peterson DR, Kraemer DF, Neuwalt EA. Effect of N-acetylcysteine route of administration on chemoprotection against cisplatin-induced toxicity in rat models. Cancer Chemother Pharmacol. 2008;62(2):235–241. doi: 10.1007/s00280-007-0597-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhao C, Shichi H. Prevention of acetaminophen-induced cataract by a combination of diallyl disulfide and N-acetylcysteine. J Ocul Pharmacol Ther. 1998;14(4):345–355. doi: 10.1089/jop.1998.14.345. [DOI] [PubMed] [Google Scholar]
- 46.Conesa EL, Valero F, Nadal JC, Fenoy FJ, Lopez B, Arregui B. N-acetylcysteine improves renal medullary hypoperfusion in acute renal failure. Am J Physiol. 2001;281(3):R730–R737. doi: 10.1152/ajpregu.2001.281.3.R730. [DOI] [PubMed] [Google Scholar]
- 47.Abdelrahman AM, Al-Salam S, Al-Mahruqi AS, Al-Husseni IS, Mansour MA, Ali BH. N-acetylcysteine improves renal hemodynamics in rats with cisplatin-induced nephrotoxicity. J Appl Toxicol. 2010;30(1):15–21. doi: 10.1002/jat.1465. [DOI] [PubMed] [Google Scholar]
- 48.Das J, Roy A, Sil PC. Mechanism of the protective action of taurine in toxin and drug induced organ pathophysiology and diabetic complications. Food Funct. 2012;3(12):1251–1264. doi: 10.1039/c2fo30117b. [DOI] [PubMed] [Google Scholar]
- 49.Schuller-Levis G, Quinn MR, Wright C, Park E. Taurine protects against oxidant-induced lung injury: possible mechanisms of action. Adv Exp Med Biol. 1994;359:31–39. doi: 10.1007/978-1-4899-1471-2_4. [DOI] [PubMed] [Google Scholar]
- 50.Chen YX. Protective action of taurine on ischemia reperfusion liver injury in rats and its mechanisms. Chin Med J Engl. 1993;73(5):276–279. [PubMed] [Google Scholar]
- 51.Lyman NW, Hemalatha C, Viscuso RL, Jacobs MG. Cisplatin-induced hypocalcemia and hypomagnesemia. Arch Intern Med. 1980;140(11):1513–1514. [PubMed] [Google Scholar]
- 52.Ripps H, Shen W. Taurine: a very essential amino acid. Mol Vis. 2012;18:2673–2686. [PMC free article] [PubMed] [Google Scholar]


