Definition
A bruise, also known as a ‘contusion’ or ‘ecchymosis,’ is a small haemorrhagic spot that results from extravasation of blood; it is found in the skin or mucous membrane and presents as a non-elevated, rounded or irregular, blue or purplish patch.1
Introduction
Cosmetic treatments amounted to £2.3 billion in the United Kingdom in 2010, and this amount was estimated to reach £3.6 billion in 2015 with 9 out of 10 of these procedures being nonsurgical and generating 75 percent of the market share.2 However, downtime following a cosmetic procedure is an important consideration for patients prior to undergoing a treatment. Bruising is often a tell-tale sign that a patient has had something done and can lead to some embarrassment and unsolicited questions.1 In addition to the negative cosmetic effect of a bruise, facial bruising may also lead some to assume spousal abuse.3
Incidence
Localized reactions such as bruising are by far the most common adverse event encountered with procedures such as dermal filler or botulinum toxin injections. The incidence is variable and dependent on many factors. One study4 reports the incidence of bruising following dermal fillers to be between 19 and 24 percent, and another study5 reports the incidence as high as 68 percent.
Minimizing the Risk
(A) Patient factors. Many factors can influence the risk of bruising; therefore, it is important to take a full medical history prior to undertaking treatment with particular reference to previous treatments and susceptibility to bruising, haematological and liver disease, coagulopathies, and medication, including prescribed and over the counter. Older patients with thin and fragile skin and slower repair mechanisms are likely to be more prone to bruising and slower to recover.1 Alcohol increases clotting time and increases risk of bruising. Patients should avoid alcohol 24 hours prior to treatment.1 Patients who are malnourished may be in a higher risk group; vitamin C deficiency and iron deficiency increases risk of bruising and prolongs healing time.
Medication. Many prescribed medications, such as aspirin,1 clopidogril, warfarin, non-Vitamin K-dependent oral anticoagulants (e.g., dabigatran, apixaban, and rivaroxaban), heparin, and the low molecular weight heparins all affect blood clotting and will increase the risk of haemorrhage and bruising. These are often prescribed in atrial fibrillation, thromboembolic disease, mechanical heart valves, and in patients with a high risk of or previous cardiovascular or cerebrovascular infarction. These medications should not be stopped without specialist advice and should not be discontinued for an aesthetic procedure. If aspirin is being taken for another indication, such as analgesia, this should be avoided for one week prior to the treatment being performed.6 Similarly, non-steroidal anti-inflammatory (NSAID) medications,7 (e.g., ibuprofen, naproxen, diclofenac, celecoxib, and meloxicam) should be avoided for a similar period of time. Corticosteroids will also increase the risk of bruising as they increase the fragility of capillaries within the skin.1 If a patient is taking a prescribed medication, the risks and benefits of the procedure should be discussed prior to consent being obtained. If a patient decides to proceed, they should be counselled about the increased risks.
Herbal and vitamin supplements. Over-the-counter herbal and vitamin supplements are becoming increasingly common and can have an influence on clotting time and increase the risk of bruising. In particular, fish oils7,8 omega-3 fatty acids,9 garlic,6–9 high-dose Vitamin E,6–9 gingko biloba,6–9 and St. John’s wort8,9 may all lead to greater bruising. The general consensus is that these should be avoided for two weeks prior to surgical procedures.
(B) Practitioner factors. Practitioners should have a good knowledge of venous and arterial vessels of the face to avoid puncturing larger vessels.1 Careful inspection of the skin with all make-up removed should be done to identify any superficial vessels, which can then be avoided.6 Lighting is important to be able to see underlying vessels and other aids, such as a magnifying loop or VeinViewer® Flex6 (Christie Medical Holdings, Inc., Memphis, Tennessee), may offer a greater advantage. Ensure the treatment room is not too hot as such an environment may cause vasodilatation.
Correct positioning of the patient can reduce the risk of bruising by preventing any unnecessary movement and trauma. The ideal patient position is semi-reclined at a 30-degree angle with the head supported by a head rest.6 Also, the practitioner’s injecting hand may be braced to the patient to avoid movement.6
A fanning or threading technique with a sharp needle into the dermal or immediate subdermal plane is more likely to result in bruising when compared to a single or serial puncture technique.4,11 Less bruising is observed when using the depot or aliquot technique with product placed at the supra-periosteal level.8
Larger gauge needles are more likely to damage blood vessels and lead to bruising.1 Where possible, smaller gauge needles are preferable,8 but this may be in part dependent on the product being injected. Administration of botulinum toxin should be via a 30G needle. The use of a 32G needle did not show any statistical difference in the rate of bruising compared with a 30G needle.12
There is some evidence that the use of a fanning technique with a blunt-ended cannula reduces the incidence of bruising,3,13,14 although very thin cannulas can still cause considerable trauma. Cannulas are also generally longer than their counterpart needles and; therefore, less entry points are needed, again minimizes the risk of bruising.6,8
Increased rate of injection and volume are both linked to greater incidence of bruising6,8 with treatments performed more slowly and with less volume having better outcomes in turns of local reactions including bruising.1
There is some evidence that cooling the skin using a contact cooling device prior to injection reduces the incidence of ecchymosis by 60 to 88 percent.15
There are reports in the literature that prophylaxis with Arnica montana leads to less bruising following cosmetic surgery which was statistically significant on Day 1 and Day 7 when compared to a control group.9
(C) Product factors. The use of adrenaline (epinephrine) with lidocaine can limit bruising as the adrenaline leads to a vasoconstriction of surrounding vessels and inhibits the activation of eosinophils which play a part in bruising.8 Adrenaline should be used with caution as it will cause blanching of the skin and may the mask the symptoms of an acute necrosis. Hyaluronic acid has innate anti-thrombotic qualities.
Areas of caution
-
¥
Periorbital region (particularly the lateral canthus where the skin is thin and veins more superficial)3
-
¥
Perioral region and oral commissures
-
¥
Temporal region
Treatment
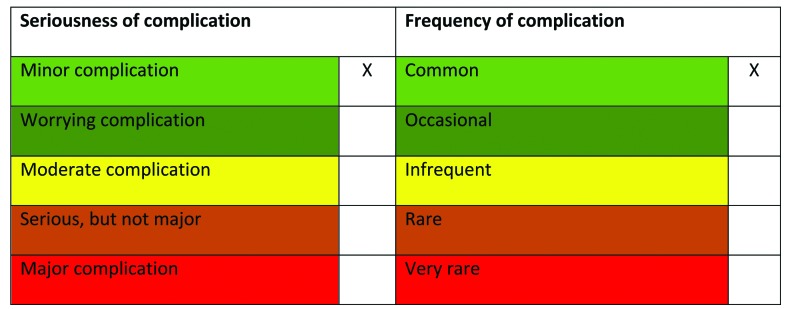
As part of an informed consent, patients should be prepared for bruising which may in rare cases be difficult to camouflage and may inhibit social activities, particularly those patients in high-risk groups. When obtaining consent, use appropriate language for the patient (e.g., black eye). Ecchymosis will usually resolve in healthy individuals within 10 to 14 days but it may persist for longer. The application of cold packs within the first 48 hours followed by heat can aid resolution.
Application of local compression following injection reduces bruising risk1,6 as does the use of a cold compress1,8 to encourage vasoconstriction.6
The topical application of arnica,1 vitamin K8, or bromelain1 can lead to a reduction in the development of a bruise and may also increase the speed of resolution,16,17 Bromelain is an enzyme derived from pineapple that can be taken at a dose of 200 to 400mg three times per day to speed healing and help the body clear metabolic waste following an injury.1
Persistent bruising or hemosiderin staining as a result of ecchymosis may be amenable to laser treatment with devices, such as the pulsed dye light (VBeam®, Syneron Candela, Irvine, California) or potassium titanyl phosphate (KTP) laser, where hemoglobin serves as the chromophore.8 Patients who develop bruising should be advised to stay out of the sun initially to limit the risk of persistent staining.8
Vigorous exercise can increase blood pressure and aggravate any bruising that is developing; therefore, exercise should be avoided for the first 24 hours following an aesthetic procedure.1,8 Patients should also be advised to avoid extreme heat.
Finally, if unacceptable bruising does develop, camouflage make-up may be applied.
Hematoma
Rather than forming a bruise, if there is a collection of blood beneath the skin or within the muscle, this may become trapped resulting in a firm mass appearing. The blood within the hematoma is initially liquefied and can often be aspirated and drained if it is dealt with before it becomes completely solid. A hematoma will almost always naturally resolve over several weeks or months as the body breaks it down through normal processes. If a hematoma is very large or is causing damage to surround tissue due to compression, it may be removed surgically. Hematomas rarely occur following nonsurgical aesthetic procedures.1
Refer
Bruising will normally resolve spontaneously within 10 to 14 days and is best managed conservatively. However, if bruising is particularly distressing or a hematoma has developed, it is best to review the patient as soon as possible. Keep contemporaneous notes with good documentation and photography. Reassurance is often all that is required or simple measures included in this document.
Hematoma development may need referral to a colleague for aspiration and drainage or surgical excision if it is causing compression to nerves or vessels. A patient who experiences bruising that fails to resolve over time or worsens over time should be referred to his or her general practitioner as this may be a sign of an underlying medical condition and should be investigated further.
References
- 1.Brennan C. Stop “cruising for a bruising”: mitigating bruising in aesthetic medicine. Plast Surg Nurs. 2014;34(2):75–79. doi: 10.1097/PSN.0000000000000040. quiz 80–81. [DOI] [PubMed] [Google Scholar]
- 2.Department of Health. Review of the Regulation of Cosmetic Interventions. Apr, 2013.
- 3.Niamtu J., III Filler injection with micro-cannula instead of needles. Dermatol Surg. 2009;35(12):2005–2008. doi: 10.1111/j.1524-4725.2009.01323.x. [DOI] [PubMed] [Google Scholar]
- 4.Glogau RG, Kane MAC. Effect of injection techniques on the rate of local adverse events in patients implanted with nonanimal hyaluronic acid gel dermal fillers. Dermatol Surg. 2008;34(s1):S105–S109. doi: 10.1111/j.1524-4725.2008.34251.x. [DOI] [PubMed] [Google Scholar]
- 5.Tzikas TL. Evaluation of the radiance FN soft tissue filler for facial soft tissue augmentation. Arch Facial Plast Surg. 2004;6(4):234–239. doi: 10.1001/archfaci.6.4.234. [DOI] [PubMed] [Google Scholar]
- 6.Hamman MS, Goldman MP. Minimizing bruising following fillers and other cosmetic injectables. J Clin Aesthet Dermatol. 2013;6(8):16–18. [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen JL. Understanding, avoiding, and managing dermal filler complications. Dermatol Surg. 2008;34:S92–S99. doi: 10.1111/j.1524-4725.2008.34249.x. [DOI] [PubMed] [Google Scholar]
- 8.Funt D, Pavicic T. Dermal fillers in aesthetics: an overview of adverse events and treatment approaches. Clin Cosmet Investig Dermatol. 2013;6:295–316. doi: 10.2147/CCID.S50546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nettar K, Maas C. Facial filler and neurotoxin complications. Facial Plast Surg. 2012;28:288–293. doi: 10.1055/s-0032-1312695. [DOI] [PubMed] [Google Scholar]
- 10.Broughton G, II, Crosby MA, Coleman J, Rohrich RJ. Use of herbal supplements and vitamins in plastic aurgery: a practical review. Plast Reconstr Surg. 2007;119(3):48e–66e. doi: 10.1097/01.prs.0000252661.72071.8d. [DOI] [PubMed] [Google Scholar]
- 11.Gladstone HB, Cohen JL. Adverse effects when injecting facial fillers. Semin Cutan Med Surg. 2007;26(1):34–39. doi: 10.1016/j.sder.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 12.Price KM, Williams ZY, Woodward JA. Needle preference in patients receiving cosmetic botulinum toxin type A. Dermatol Surg. 2010;36(1):109–112. doi: 10.1111/j.1524-4725.2009.01391.x. [DOI] [PubMed] [Google Scholar]
- 13.Fulton J, Caperton C, Weinkle S, Dewandre L. Filler injections with the blunt-tip microcannula. J Drugs Dermatol. 2012;11(9):1098–1103. [PubMed] [Google Scholar]
- 14.Zeichner JA, Cohen JL. Use of blunt tipped cannulas for soft tissue fillers. J Drugs Dermatol. 2012;11(1):70–72. [PubMed] [Google Scholar]
- 15.Nestor MS, Ablon GR, Stillman MA. The use of a contact cooling device to reduce pain and ecchymosis associated with dermal filler injections. J Clin Aesthet Dermatol. 2010;3(3):29–34. [PMC free article] [PubMed] [Google Scholar]
- 16.MacKay D, Miller AL. Nutritional support for wound healing. Altern Med Rev. 2003;8(4):359–377. [PubMed] [Google Scholar]
- 17.Leu S, Havey J, White LE, et al. Accelerated resolution of laser-induced bruising with topical 20% arnica: a rater-blinded randomized controlled trial. Br J Dermatol. 2010;163(3):557–563. doi: 10.1111/j.1365-2133.2010.09813.x. [DOI] [PubMed] [Google Scholar]