Abstract
Objective
To assess the feasibility of a Mindfulness-based stress reduction (MBSR) program for adolescents with widespread chronic pain and other functional somatic symptoms, and to make preliminary assessments of its clinical utility.
Study design
Three cohorts of subjects completed an 8-week MBSR program. Child- and parent-completed measures were collected at baseline and 8 and 12 weeks later. Measures included the Functional Disability Inventory (FDI), the Fibromyalgia/Symptom Impact Questionnaire (FIQR/SIQR), the Pediatric Quality of Life Inventory (PedsQL), the Multidimensional Anxiety Scale (MASC2), and the Perceived Stress Scale (PSS). Subjects and parents were interviewed following the program to assess feasibility.
Results
Fifteen of 18 subjects (83%) completed the 8-week program. No adverse events occurred. Compared with baseline scores, significant changes were found in mean scores on the FDI (33% improvement, p=0.026), FIQR/SIQR (26% improvement, p=0.03), and MASC2 (child: 12% improvement, p=0.02; parent report: 17% improvement, p=0.03) at 8 weeks. MASC2 scores (child and parent) and PSS scores were significantly improved at 12 weeks. More time spent doing home practice was associated with better outcomes in the FDI and FIQR/SIQR (44% and 26% improvement, respectively). Qualitative interviews indicated that subjects and parents reported social support as a benefit of the MBSR class, as well as a positive impact of MBSR on activities of daily living, and on pain and anxiety.
Conclusions
MBSR is a feasible and acceptable intervention in adolescents with functional somatic syndromes, and has preliminary evidence for improving functional disability, symptom impact, and anxiety, with consistency between parent and child measures.
Trial registration
ClinicalTrials.gov: NCT02190474
Keywords: chronic pain, quality of life, fibromyalgia, irritable bowel syndrome
Functional somatic syndromes include conditions such as chronic fatigue syndrome, irritable bowel syndrome, fibromyalgia, chronic unexplained pain, and symptoms attributed to chronic Lyme disease.1–4 At least 13% of primary care visits are attributable to functional somatic syndromes.5–7 These syndromes are prevalent, costly, and may be debilitating.8 Patients with these syndromes often have psychiatric comorbidities, primarily anxiety or depression.9–11 Many medical specialties have archetypal functional syndromes that may reflect similar underlying pathophysiology. Patients seen by different medical subspecialists often are labeled as having certain functional syndromes associated with the subspecialty (e.g. irritable bowel syndrome for gastroenterologists; fibromyalgia for rheumatologists), but the syndrome may actually be more similar than they are different.12, 13
Many functional somatic syndromes are associated with dysfunctional CNS processing14, 15 and may persist: 85% of patients with juvenile fibromyalgia continue to have symptoms into adulthood, and 50% of these patients meet diagnostic criteria for fibromyalgia.16 Children with unexplained recurrent abdominal pain are at increased risk of developing fibromyalgia.17
As is true of many conditions that tend to be resistant to conventional treatments, patients with functional somatic syndromes often seek therapies outside of mainstream care.18–20
Among the more promising interventions for functional somatic syndromes are mind-body therapies that can address both psychological and somatic symptoms.21 Furthermore, nonpharmacologic interventions are especially appealing in light of risks of adverse effects of psychotropic medications and analgesics, the stigma of being “medicated”, and the effect of the intervention on the CNS 22–24 Mindfulness-based stress reduction (MBSR) involves meditation training, patient education, yoga exercises, and group support.25–27 The standard 8-week MBSR curriculum for adults consists of weekly instructor-led group sessions (2.5 hours long with meditation practice, discussions, and skill-building activities), a full-day retreat, and 45–60 minutes of practice daily.25, 27 Clinical trials in adults have shown that various forms of mindfulness meditation result in improvement in pain, physical function, anxiety, and depression.28–32 There are also data that support the use of MBSR in children and adolescents both for reducing perceived stress and for improving psychological health.33 In this pilot study, we assessed the feasibility of an MBSR program for adolescents with widespread chronic pain and other persistent somatic symptoms, and to make preliminary assessments of its clinical utility.
Methods
Subjects were 12–18 years of age (one 10-year old participated) and had symptoms consistent with fibromyalgia, chronic fatigue, musculoskeletal pain, headache, abdominal pain-related bowel dysfunction, perceived cognitive impairment, or other non-specific symptoms that had been present for ≥3 months, were associated with some degree of disability (e.g., missing school), and were not attributable to an organic medical disorder despite adequate evaluation (ClinicalTrials.gov: NCT02190474).
Potential subjects were excluded if they had a chronic autoimmune or inflammatory condition, had a serious illness within 90 days of enrollment, used opioid analgesics, or screened positive on the Columbia-Suicide Severity Rating Scale at enrollment. Written informed consent/assent was obtained from parents and subjects. All subjects received $200 for participation. The study was approved by the Human Investigation Committee of Yale University.
Subjects attended weekly 1.5-hour group sessions for eight weeks and one 4-hour retreat, all led by an experienced MBSR instructor. Assignments were 15–25 minute guided (step-by-step) daily home practice using audio recordings from the instructor. We condensed the standard adult MBSR protocol, but retained core curricular elements, while modifying it to be both developmentally appropriate and logistically feasible for adolescents. Subjects were assessed at baseline, 8 weeks (at the end of the MBSR program), and at 12 weeks. Subjects received a daily text message using a secure mobile data broadcast service (callfire.com) to remind them to record minutes of home practice (if any) and to minimize recall bias. Parents of subjects were encouraged, but not required, to participate in a concurrent parent group to encourage familiarity with the MBSR program. The parent groups listened to the weekly audio recordings of guided meditations given to study subjects, and were instructed not to encourage nor to practice MBSR with their children.
Measures
Measures included the Functional Disability Inventory (FDI), which assesses physical and functional impairment in adolescents with chronic pain.34, 35 Scores range from 0–60, with higher scores indicating greater functional disability, and can be categorized as No/Minimal (0–12), Moderate (13–29), or Severe (>30) Disability.34, 36 A 7.8-point change in the FDI has been empirically determined to be the minimal clinically important difference in adolescents.37
We used the Fibromyalgia Impact Questionnaire-Revised (FIQR) for subjects who met diagnostic criteria for fibromyalgia (n=7), and the analogue Symptom Impact Questionnaire-Revised (SIQR) for subjects who did not meet diagnostic criteria for fibromyalgia (n=8).38, 39 A 14% change in the FIQR has been empirically determined as a minimal clinically important difference in adults.40 The FDI and FIQR were our primary measures.
We assessed health-related quality of life with the Pediatric Quality of Life Inventory 4.0 adolescent form (PedsQL).41 We also used the Child and Adolescent Mindfulness Measure (CAMM), a 10-item questionnaire assessing mindfulness skills.42 CAMM scores are positively correlated with quality of life, academic competence, and social skills and negatively correlated with somatic complaints, internalizing symptoms, and externalizing behavior problems. We assessed subjects’ stress with the Perceived Stress Scale43 (PSS), a 14-item scale that assesses perceived stress of life situations in adolescents44 and adults, and has well-established validity in relation to physiological stress responses45 and anxiety and depressive disorders.46 We assessed anxiety with the Multidimensional Anxiety Scale for Children47 (MASC2), consisting of 50 items distributed across six domains: Physical Symptoms, Social Anxiety, Harm Avoidance, Separation Anxiety/Phobias, Generalized Anxiety, and Obsessive-Compulsive symptoms.48 Parents completed parent versions of the MASC2 and PedsQL.
Qualitative Interviews
We interviewed each subject-parent dyad together after the 8-week session in a semi-structured, open-ended manner. These 15–20 minute interviews explored three broad areas: the feasibility and practicality of meeting weekly for eight weeks (e.g., participating during the school year); the structure and content of the MBSR course (e.g., age-appropriateness of instructions, class size and length, feasibility of home practice); and perspectives on clinical and psychosocial benefits realized through mindfulness practice. Interviews conducted by two investigators (AA and TRW) were audio recorded and transcribed verbatim (Transcription Plus, LLC, Bristol, CT). Data analysis followed the constant comparative approach.51 After each cohort, the transcripts were reviewed and emerging themes in the data were identified.
Statistical Analyses
We report results of matched-pair t-tests of the difference in means for each measure in each group. Because of the relatively small sample size and the potential for underlying non-normality of the results, differences in distributions between baseline and week 8 and between baseline and week 12 were also tested for significance with Wilcoxon matched-pairs signed-rank tests. All analyses were conducted using Stata (Version 14.1, StataCorp, College Station, TX). The level of statistical significance was set at 0.05 (two sided).
RESULTS
Three cohorts (4–7 subjects in each group) enrolled between January and November 2015: Cohort 1 (January – March 2015, n=7); Cohort 2 (April – June 2015; n=4); and Cohort 3 (September – November 2015, n=4).
Of the 22 potential subjects who were screened, 21 met eligibility criteria. Of the 21, three were invited to enroll in the program but declined (one of the three had a scheduling conflict). Three subjects withdrew before completing all sessions. One subject (a 15-year-old girl) withdrew after 6 weeks of MBSR because she was hospitalized for depression, a diagnosis that preceded enrollment in the study. Another subject (a 12-year-old boy) dropped out after one session;. his mother did not return phone calls so we do not know why he dropped out. The mother of the third subject (a 12-year-old boy) reported that his symptoms resolved after he was treated for a supposed infection with an intestinal parasite.
Ages of the 15 who participated ranged from 10 to 18 years (median: 14); 11 were female. The most commonly reported symptoms included chronic widespread pain/fibromyalgia (n=7), fatigue (n=6), and other musculoskeletal pain/arthralgia (n=6). Subjects were referred by community and university clinicians and through announcements in regional newsmagazines. Characteristics of the subjects are shown in Table I.
Results are shown in Table II. There was no missing data. After completing the MBSR program, scores on the FDI, FIQR/SIQR, MASC2, and PSS improved in 13/15 (87%), 12/15 (80%), 12/15 (80%), and 9/15 (60%) respectively. Nine of 15 (60%) subjects and eight of 15 (53%) parents reported improvement on the PedsQL. There were statistically significant pre-post differences in mean scores of the FDI (33% improvement, p=0.026), the FIQR/SIQR (26% improvement, p=0.03), and MASC2 (child: 12% improvement, p=0.02; parent: 17% improvement, p=0.03) using Wilcoxon Matched-Pairs Signed-Rank Tests. The changes were also statistically significant (p<0.05) in matched-pairs t-test analyses. Differences in MASC2 scores remained statistically significant at 12-weeks (compared with baseline) for both child (p=0.047) and parent reports (p=0.004). There were statistically significant changes in the PSS at 12-weeks (p=0.01) but not at 8-weeks (p=0.27). Similarly, PedsQL scores improved more at 12-weeks (child: mean improvement of 5.4 points, parent: mean improvement of 9.2 points) then at 8-weeks (child: mean improvement of 4.6 points, parent: mean improvement of 1.0 points), though none of these differences were statistically significant. Six of the 15 subjects (40%) had clinically important (>7.8 point) improvements in the FDI, and 9 of 15 (60%) subjects had clinically important (>14%) improvements in the FIQR/SIQR. Adjunct groups for parents were available for two of the three cohorts. Participation of parents was inconsistent: a parent attended a session 66% of the time.
Home Practice
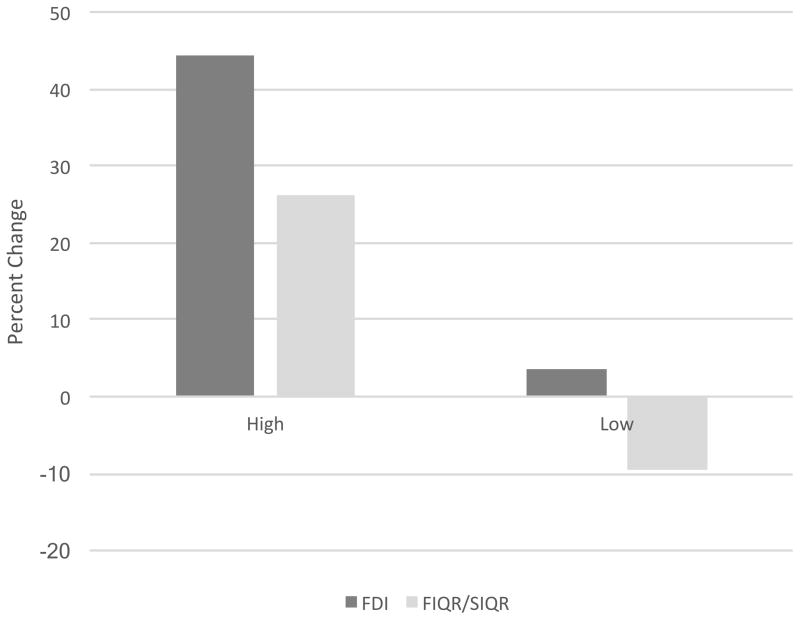
Only one subject reported not doing any home practice. The remaining subjects (n=14) reported a median of 434 minutes (range=0–1736 minutes) of formal practice. It appeared that the amount of home practice was associated with improvement. In a median-split analysis, higher amounts of home practice over 8 weeks (top 50% of sample) had 44% improvements in FDI scores and 26% improvements in FIQR/SIQR scores. Lower amounts of home practice (bottom 50% of sample) had 4% improvements in FDI scores and 9% worsening in the FIQR/SIQR (Figure).
Figure.
In a median-split analysis, higher amounts of home practice over 8 weeks (top 50% of sample) had 44% improvements in FDI scores and 26% improvements in FIQR/SIQR scores. In contrast, lower amounts of home practice (bottom 50% of sample) had 4% improvements in FDI scores and 9% worsening in the FIQR/SIQR.
There were no adverse effects attributed to MBSR.
Qualitative Analyses
Major themes were mindfulness teachings had a positive impact on daily life, on pain and anxiety, and on social support.
Sessions focused on using mindfulness teachings to help address somatic symptoms. One subject noted that MBSR training helped her reframe her symptoms into a more manageable pattern using a mindful awareness approach: “I used to look at them as one big problem and now I’m able to break it down. So instead of my entire body hurts, I can pinpoint it. I’d be like, ‘Oh, my knee really hurts and my wrist really hurts’ and then I can go about my day. Thinking about it that way, as opposed to ‘my entire body hurts,’ because when I think about it like that, I get really sluggish, and then I kind of drive myself into that mindset.”
One subject stated that the course “was nothing like I thought it would be, but in the best way possible. I never thought I would learn ways to actually minimize my pain and minimize some of my symptoms,” and another subject declared, “I had no idea that that would be a way for someone with symptoms, like what the people in my group and myself had...I didn’t think that would ever work and I didn’t think it could be used to work in that way, so it was really cool. It’s like a different way of dealing with something or helping to deal with something.”
One mother discussed her son’s school attendance: “I definitely saw a difference towards the…last few weeks. I saw a decrease in the talking and complaining about symptoms…prior to [the course] he went through this stretch of about two weeks - there was a pattern - at the end of the second week, he would start to talk about being really exhausted. Then the pain, a headache would accompany that, and then there would be one to two days out of school. That has lengthened to about five to six weeks….So that’s huge.”
One subject’s comments set her apart from all the rest, when she said after completing the course, “I had a set way of thinking when I came in, and I still have that set way of thinking coming out of it”. She continued that she was “forced to” attend the program by her mother. She refused all home practice, and did not feel that mindfulness training affected her life.
The ability to self-regulate and employ mindfulness techniques in daily life helped with pain and anxiety symptoms: “It [MBSR] just makes me focus on what I’m doing so I’m not like all over the place, and I’m not focusing all on my pain.” Another subject stated, “The symptoms would come and I would practice or if it was in school…I would just focus on my breath and then it wouldn’t be completely gone, but it would decrease in annoyingness.”
One subject found the yoga aspect of the program particularly helpful: “I had stopped snowboarding for four years because I thought I couldn’t do it anymore, and recently I actually got to go again, and I did the yoga before and afterwards, and it was the first time in a long, long time that I was able to do something I liked in a sport without feeling insane amount of pain afterwards.”
One mother noted that the time commitment was a potential barrier, but symptomatic relief made the program worthwhile. Describing her daughter’s response, she noted, “I think she found it very helpful because, like for the very first class, she was very hesitant to go. And I think it was like the second or third class, and she was still giving me a hard time about going, and I told her she had the option not to go anymore…. and she said, ‘But it’s helping my joint pain.’ So…she hasn’t given me a problem of going since.”
Subjects, parents, and investigators noted that the MBSR cohorts fostered a supportive group atmosphere. Subjects’ regularly noted that they felt camaraderie during eight weeks of weekly meetings with peers who shared similar health challenges: “I see I’m not the only one feeling the way I do, and people as young as me…have the same thing. Anne [the instructor] did an amazing job of gaining our trust in telling her story, and we all got to tell our stories, so we all got to know each other. It wasn’t like a doctor experience that we’re all so used to - like our doctor saying ‘suck it up, it’ll get better.”
Another subject noted, “…when we’d be asked questions, they could help me explain when I couldn’t put into words. Like, they understood enough when I was talking about my situation.” This subject’s mother echoed this sentiment: “You can’t truly understand what somebody with chronic health issues is going through unless you’ve gone through it or are close to somebody who’s going through it, and to have this group, that even though they all had different specific issues they could all relate to the results of those issues, to the school issues and the friends and all of that, and so I think that was good mentally and emotionally for all the kids aside from the skills they learned.”
Discussion
Our study demonstrates that it is feasible to recruit and to retain adolescents with serious functional somatic syndromes in an 8-week MBSR intervention, and to collect these data including a 12-week follow-up. The study also provides preliminary evidence that MBSR may be effective in improving functional disability, symptom impact, and anxiety.
In our sample of 15 subjects, 40% showed clinically meaningful change (>7.8 points)52 on the FDI; 87% showed some improvement in the score. Although the magnitude of changes tended to diminish at 12-weeks, most scores on quality of life scores continued to improve at 12-weeks. Subjects reported incorporating mindfulness practices into their daily lives as convenient and practical, outside the formal structure of the MBSR classes. Subjects also expressed positive feelings about group dynamics and a growing sense of cohesion and familiarity with others during the program.
Previous data support incorporating parents in psychological therapies that reduce pain in children with painful conditions.53, 54 Parents who participated in the concurrent groups reported value in the sessions while learning to incorporate some aspects of mindfulness in their own lives. Parents reported that weekly participation served as a means of stress reduction in a supportive setting with other parents of children suffering from chronic symptoms, who often had school-related difficulties (such as absenteeism and poor performance). Furthermore, our data demonstrate consistent changes in parent and child scores in anxiety (MASC2) and quality of life (PedsQL) measures. It is possible that parents’ participation in the concurrent groups could have confounded the results, but the sporadic participation of the parents reduces the likelihood that this is a significant issue.
For adolescents with functional somatic pain syndromes, it is plausible that therapeutic approaches focusing on quality of life and symptomatic relief may be more relevant than trying to search for an elusive organic disease. Furthermore, measures of anxiety showed improvement, consistent with other recent studies showing an association between chronic pain, anxiety disorders, and behavioral interventions, as up to two-thirds of children with chronic pain may also suffer from anxiety disorders.52, 55
Functional somatic pain syndromes are common and often challenging to treat in children, and nonpharmacologic therapies are often desired. Kashikar-Zuck et al have demonstrated the efficacy of cognitive behavioral therapy (CBT) in adolescents with fibromyalgia.56, 57 Despite the promise of CBT interventions in this population, there are many barriers to widespread implementation, as CBT is often delivered by doctoral- or masters-level psychologists in one-on-one office settings (though some group programs exist), so availability is limited. Furthermore, some insurers require that patients have a psychiatric diagnosis before they will pay for individual CBT, which may prevent adolescents (and parents) from getting psychological care. Cherkin et al reported that outcomes of CBT and of MBSR were equivalent in adults with chronic low back pain.58
Mindfulness meditation has received widespread media attention and has been incorporated into many corporate, healthcare, and community settings. More than 40 randomized controlled trials of mindfulness interventions (primarily MBSR) have been published for adult patients with a number of conditions, with the greatest effects reported for people with anxiety, depression, and chronic pain.59 Neuroimaging studies of mindfulness meditation show neuroplastic changes in the function and structure of brain regions associated with regulation of emotion, attention, and self-awareness. 60 Mindfulness meditation can reduce circulating levels of interleukin-6, a marker of systemic inflammation.61 Although many nonpharmacological interventions to control pain involve the production of endogenous opioids,62–64 recent evidence shows that mindfulness meditation can further reduce pain via non-opioid pathways.65, 66
Despite the popularity of mindfulness meditation programs, there are limited data that support the use of mindfulness programs in children and adolescents. Sibinga et al developed MBSR interventions for HIV-infected urban youth67 and for children in school-based settings68 and demonstrated improvement in psychological functioning, including statistically significant benefits in anxiety and perceived stress, similar to our findings. Previous studies had trouble with recruitment and retention of children with chronic pain for mindfulness interventions.69 The majority of subjects (83%) who started our MBSR program completed the program.
In our interviews with subjects and parents, positive group dynamics, trust in the instructor, symptomatic relief, and a sense of belonging and empowerment were noted as contributing to our high rates of retention.
Limitations of our study include the small sample size and lack of a comparison group, as well as the reliance on self-report instruments. However, the use of child and parent measures was a strength, especially because anxiety and quality of life scores were consistent between parents and children. Furthermore, it is plausible that nonspecific effects such as being part of a group enhanced the specific effects of MBSR. Indeed, a recent meta-analysis found that nonspecific and contextual effects were responsible for 75% of treatment effects in clinical trials in patients with osteoarthritis.70 To minimize recall bias, subjects received daily text message reminders to record amount of home practice. We doubt that these messages affected adherence to the home practice, because most subjects (80%) reported at least one full week without any home practice, despite having received the daily text reminders.
Other limitations were that the subjects were mostly White and middle class, which may have limited participation to those who had support for and means to attend eight weekly sessions, often held at a considerable distance from their homes. Subjects tended to be from home environments with at least one involved parent who was proactive about seeking care for the child. Whether these findings can be translated to more diverse populations is unknown.
In conclusion, mindfulness mediation is an appealing and safe intervention that is feasible to deliver, and was associated with clinically and statistically significant improvements in pain and functionality measures in this study. Chronic stress is associated with the development and exacerbation of functional somatic pain conditions. There are limited but promising data for both the feasibility of mindfulness-based interventions in children, as well as the promise of MBSR as a primary treatment for chronic pain conditions. Further randomized studies of MBSR in children, with appropriate controls, may provide more precise estimates of specific vs. nonspecific effects of MBSR and can further elucidate the place of mindfulness interventions in care plans for functional somatic syndromes in children.
Table 1.
Characteristics of the subjects (n=15)
| Age-years (mean, range) | 14.8 (10–18) |
| Sex (female) | 11/15 |
| Race | White (13) |
| Unknown (2) | |
| Ethnicity | Non-Hispanic/Latino (13) |
| Hispanic/Latino (2) | |
| Parent Educational Attainment* | High School (4) |
| Some College or Undergraduate Degree (6) | |
| Graduate or Post-graduate (5) | |
| Symptoms (number reporting) | Fibromyalgia (7) |
| Fatigue (6) | |
| Musculoskeletal pain/arthralgia (6) | |
| Functional abdominal pain/irritable bowel syndrome (5) | |
| Headache/migraine (5) | |
| Anxiety (4) | |
| Depression (2) | |
| Other (reported once)** | Panic attacks, dizziness, post Lyme disease symptoms, nausea, vomiting |
Father or Mother
Subjects all reported more than one symptom
Table 2.
Baseline scores and mean changes in outcome measures at 8-weeks and 12-weeks
| CHILD REPORTS | BASELINE | WEEK 8 | WEEK 12 | ||
|---|---|---|---|---|---|
| Mean (Range) | Mean (Range) | p-value1 | Mean (Range) | p-value2 | |
|
Functional Disability Inventory (FDI) (0–60) Higher scores indicate more physical challenges in their daily activities |
20.5 (2–39) | 13.7 (1–44) | 0.026* | 17.0 (0–45) | 0.14 |
|
Fibromyalgia/Symptom Impact Questionnaire (FIQR/SIQR) (0–100) Higher scores indicate more pronounced symptoms |
41.6 (10–71) | 30.6 (6–64) | 0.03* | 31.5 (4–84) | 0.21 |
|
Child and Adolescent Mindfulness Measure (CAMM) (0–40) Higher scores indicate higher levels of mindfulness |
26.7 (12–38) | 26.3 (15–40) | 0.38 | 28.4 (14–40) | 0.93 |
|
Multidimensional Anxiety Scale for Children (MASC2) (0–100) Higher scores indicate more severe anxiety symptoms |
60.8 (12–103) | 53.3 (4–82) | 0.02* | 50.7 (2–91) | 0.047* |
|
Perceived Stress Scale (PSS-14) (0–56) Higher scores indicate higher perceptions of their lives to be stressful |
26.5 (11–45) | 24.4 (12–35) | 0.27 | 20.3 (8–35) | 0.01* |
|
Pediatric Quality of Life Inventory (PedsQL) Teen (0–100) Higher scores indicate better health-related quality of life |
57.2 (26–85) | 61.8 (32–92) | 0.41 | 62.6 (24–89) | 0.18 |
| PARENT REPORTS | |||||
|
Multidimensional Anxiety Scale for Parents (MASC2) (0–100) Higher scores indicate more severe anxiety symptoms |
58.7 (27–115) | 48.7 (16–105) | 0.03* | 42.5 (21–89) | 0.004* |
|
Pediatric Quality of Life Inventory (PedsQL) Parent (0–100) Higher scores indicate better health-related quality of life |
55.2 (13–80) | 56.2 (21–84) | 0.93 | 64.4 (26–96) | 0.09 |
Baseline to week 8 differences
Baseline to week 12 differences
Statistically significant at α=0.05
Acknowledgments
We thank Gowri Ananthanarayanan MS, who provided database management; Krista Basile, MHS, and Maxine Fields, BS, who provided administrative support; Auguste H. Fortin, VI, MD, MPH, who provided guidance in mindfulness interventions; Danielle Eve Greenman, MD, Alexandra Hua, MPH, and Niloufar Mersaditabari, DPsych, who assisted with MBSR groups and data collection; Carla E. Marin, PhD, who analyzed anxiety measures; Paul L. McCarthy, MD, who referred study subjects; Daniel J. Clauw, MD, and Peter H. Van Ness, PhD, MPH; who provided guidance in study design; Rajita Sinha, PhD, who provided space for the MBSR groups; Lawrence A. Vitulano, PhD, who provided guidance in behavioral interventions; and E. Vincent S. Faustino, MD, MHS, Judson Brewer, MD, PhD, and Scott Mist, PhD, MAcOM, who served as the independent monitoring committee. We are especially grateful to our study subjects and families.
Supported by the National Center for Complementary and Integrative Health (K23AT006703), National Center for Advancing Translational Science at the National Institutes of Health (NIH), and NIH roadmap for Medical Research (Clinical and Translational Science Award UL1 TR001863).
Abbreviations and Acronyms
- CNS
Central Nervous System
- FDI
Functional Disability Inventory
- FIQR/SIQR
Fibromyalgia/Symptom Impact Questionnaire
- MASC2
Multidimensional Anxiety Scale
- MBSR
Mindfulness-based Stress Reduction
- PedsQL
Pediatric Quality of Life Inventory
- PSS
Perceived Stress Scale
Footnotes
Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIH.
The authors declare no conflicts of interest.
References
- 1.Hatcher S, Arroll B. Assessment and management of medically unexplained symptoms. BMJ. 2008;336:1124–8. doi: 10.1136/bmj.39554.592014.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shapiro ED, Dattwyler R, Nadelman RB, Wormser GP. Response to meta-analysis of Lyme borreliosis symptoms. Int J Epidemiol. 2005;34:1437–9. doi: 10.1093/ije/dyi241. author reply 40–3. [DOI] [PubMed] [Google Scholar]
- 3.Rask CU, Ornbol E, Fink PK, Skovgaard AM. Functional somatic symptoms and consultation patterns in 5- to 7-year-olds. Pediatrics. 2013;132:e459–67. doi: 10.1542/peds.2013-0159. [DOI] [PubMed] [Google Scholar]
- 4.Moulin V, Akre C, Rodondi PY, Ambresin AE, Suris JC. A qualitative study of adolescents with medically unexplained symptoms and their parents. Part 1: Experiences and impact on daily life. J Adolesc. 2015;45:307–16. doi: 10.1016/j.adolescence.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 5.van der Weijden T, van Velsen M, Dinant GJ, van Hasselt CM, Grol R. Unexplained complaints in general practice: prevalence, patients’ expectations, and professionals’ test-ordering behavior. Med Decis Making. 2003;23:226–31. doi: 10.1177/0272989X03023003004. [DOI] [PubMed] [Google Scholar]
- 6.Ring A, Dowrick CF, Humphris GM, Davies J, Salmon P. The somatising effect of clinical consultation: what patients and doctors say and do not say when patients present medically unexplained physical symptoms. Soc Sci Med. 2005;61:1505–15. doi: 10.1016/j.socscimed.2005.03.014. [DOI] [PubMed] [Google Scholar]
- 7.Konnopka A, Kaufmann C, Konig HH, Heider D, Wild B, Szecsenyi J, et al. Association of costs with somatic symptom severity in patients with medically unexplained symptoms. Journal of psychosomatic research. 2013;75:370–5. doi: 10.1016/j.jpsychores.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 8.Bourke J. Fibromyalgia and chronic fatigue syndrome: management issues. Adv Psychosom Med. 2015;34:78–91. doi: 10.1159/000369087. [DOI] [PubMed] [Google Scholar]
- 9.Ali A, Vitulano L, Lee R, Weiss TR, Colson ER. Experiences of patients identifying with chronic Lyme disease in the healthcare system: a qualitative study. BMC family practice. 2014;15:79. doi: 10.1186/1471-2296-15-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bujoreanu S, Randall E, Thomson K, Ibeziako P. Characteristics of medically hospitalized pediatric patients with somatoform diagnoses. Hosp Pediatr. 2014;4:283–90. doi: 10.1542/hpeds.2014-0023. [DOI] [PubMed] [Google Scholar]
- 11.Janssens KA, Zijlema WL, Joustra ML, Rosmalen JG. Mood and Anxiety Disorders in Chronic Fatigue Syndrome, Fibromyalgia, and Irritable Bowel Syndrome: Results From the LifeLines Cohort Study. Psychosomatic medicine. 2015;77:449–57. doi: 10.1097/PSY.0000000000000161. [DOI] [PubMed] [Google Scholar]
- 12.Wessely S, White PD. There is only one functional somatic syndrome. The British journal of psychiatry : the journal of mental science. 2004;185:95–6. doi: 10.1192/bjp.185.2.95. [DOI] [PubMed] [Google Scholar]
- 13.Clauw DJ. Fibromyalgia and related conditions. Mayo Clin Proc. 2015;90:680–92. doi: 10.1016/j.mayocp.2015.03.014. [DOI] [PubMed] [Google Scholar]
- 14.Chang L, Berman S, Mayer EA, Suyenobu B, Derbyshire S, Naliboff B, et al. Brain responses to visceral and somatic stimuli in patients with irritable bowel syndrome with and without fibromyalgia. Am J Gastroenterol. 2003;98:1354–61. doi: 10.1111/j.1572-0241.2003.07478.x. [DOI] [PubMed] [Google Scholar]
- 15.Phillips K, Clauw DJ. Central pain mechanisms in chronic pain states--maybe it is all in their head. Best Pract Res Clin Rheumatol. 2011;25:141–54. doi: 10.1016/j.berh.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kashikar-Zuck S, Cunningham N, Sil S, Bromberg MH, Lynch-Jordan AM, Strotman D, et al. Long-term outcomes of adolescents with juvenile-onset fibromyalgia in early adulthood. Pediatrics. 2014;133:e592–600. doi: 10.1542/peds.2013-2220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alfven G. Recurrent pain, stress, tender points and fibromyalgia in childhood: an exploratory descriptive clinical study. Acta paediatrica. 2012;101:283–91. doi: 10.1111/j.1651-2227.2011.02491.x. [DOI] [PubMed] [Google Scholar]
- 18.Ali A, McCarthy PL. Complementary and integrative methods in fibromyalgia. Pediatrics in review / American Academy of Pediatrics. 2014;35:510–8. doi: 10.1542/pir.35-12-510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kenney D, Jenkins S, Youssef P, Kotagal S. Patient Use of Complementary and Alternative Medicines in an Outpatient Pediatric Neurology Clinic. Pediatr Neurol. 2016 doi: 10.1016/j.pediatrneurol.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 20.Hung A, Kang N, Bollom A, Wolf JL, Lembo A. Complementary and Alternative Medicine Use Is Prevalent Among Patients with Gastrointestinal Diseases. Digestive diseases and sciences. 2015;60:1883–8. doi: 10.1007/s10620-014-3498-3. [DOI] [PubMed] [Google Scholar]
- 21.Masi AT, White KP, Pilcher JJ. Person-centered approach to care, teaching, and research in fibromyalgia syndrome: justification from biopsychosocial perspectives in populations. Semin Arthritis Rheum. 2002;32:71–93. doi: 10.1053/sarh.2002.33717. [DOI] [PubMed] [Google Scholar]
- 22.Hussain SZ, Hyman PE. Psychotropic medications for pediatric functional gastrointestinal disorders. J Pediatr Gastroenterol Nutr. 2014;59:280–7. doi: 10.1097/MPG.0000000000000445. [DOI] [PubMed] [Google Scholar]
- 23.Cunningham NR, Jagpal A, Tran ST, Kashikar-Zuck S, Goldschneider KR, Coghill RC, et al. Anxiety Adversely Impacts Response to Cognitive Behavioral Therapy in Children with Chronic Pain. J Pediatr. 2016;171:227–33. doi: 10.1016/j.jpeds.2016.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Joshi SV. Teamwork: the therapeutic alliance in pediatric pharmacotherapy. Child Adolesc Psychiatr Clin N Am. 2006;15:239–62. doi: 10.1016/j.chc.2005.08.004. [DOI] [PubMed] [Google Scholar]
- 25.Kabat-Zinn J, Santorelli S. Mindfulness-based stress reduction professional training resource manual. Worcester, MA: Center for Mindfulness in Medicine, Health Care and Society; 1999. [Google Scholar]
- 26.Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits. A meta-analysis. J Psychosom Res. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 27.Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Delacorte Press; 1990. [Google Scholar]
- 28.Kaplan KH, Goldenberg DL, Galvin-Nadeau M. The impact of a meditation-based stress reduction program on fibromyalgia. Gen Hosp Psychiatry. 1993;15:284–9. doi: 10.1016/0163-8343(93)90020-o. [DOI] [PubMed] [Google Scholar]
- 29.Goldenberg D, Kaplan K, Nadeau M, Brodeur C, Smith S, Schmid C. A Controlled Study of a Stress-Reduction, Cognitive- Behavioral Treatment Program in Fibromyalgia. Journal Of Musculoskeletal Pain. 1994;2:53–66. [Google Scholar]
- 30.von Weiss D. Use of mindfulness meditation for fibromyalgia. Am Fam Physician. 2002;65:380, 4. [PubMed] [Google Scholar]
- 31.Hsu MC, Schubiner H, Lumley MA, Stracks JS, Clauw DJ, Williams DA. Sustained pain reduction through affective self-awareness in fibromyalgia: a randomized controlled trial. J Gen Intern Med. 2010;25:1064–70. doi: 10.1007/s11606-010-1418-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Crowe M, Jordan J, Burrell B, Jones V, Gillon D, Harris S. Mindfulness-based stress reduction for long-term physical conditions: A systematic review. Aust N Z J Psychiatry. 2016;50:21–32. doi: 10.1177/0004867415607984. [DOI] [PubMed] [Google Scholar]
- 33.Perry-Parrish C, Copeland-Linder N, Webb L, Sibinga EM. Mindfulness-Based Approaches for Children and Youth. Curr Probl Pediatr Adolesc Health Care. 2016 doi: 10.1016/j.cppeds.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 34.Flowers SR, Kashikar-Zuck S. Measures of juvenile fibromyalgia: Functional Disability Inventory (FDI), Modified Fibromyalgia Impact Questionnaire-Child Version (MFIQ-C), and Pediatric Quality of Life Inventory (PedsQL) 3.0 Rheumatology Module Pain and Hurt Scale. Arthritis Care Res (Hoboken) 2011;63(Suppl 11):S431–7. doi: 10.1002/acr.20639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Degotardi PJ, Klass ES, Rosenberg BS, Fox DG, Gallelli KA, Gottlieb BS. Development and evaluation of a cognitive-behavioral intervention for juvenile fibromyalgia. Journal of pediatric psychology. 2006;31:714–23. doi: 10.1093/jpepsy/jsj064. [DOI] [PubMed] [Google Scholar]
- 36.Kashikar-Zuck S, Flowers SR, Claar RL, Guite JW, Logan DE, Lynch-Jordan AM, et al. Clinical utility and validity of the Functional Disability Inventory among a multicenter sample of youth with chronic pain. Pain. 2011;152:1600–7. doi: 10.1016/j.pain.2011.02.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sil S, Arnold LM, Lynch-Jordan A, Ting TV, Peugh J, Cunningham N, et al. Identifying treatment responders and predictors of improvement after cognitive-behavioral therapy for juvenile fibromyalgia. Pain. 2014;155:1206–12. doi: 10.1016/j.pain.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bennett RM, Friend R, Jones KD, Ward R, Han BK, Ross RL. The Revised Fibromyalgia Impact Questionnaire (FIQR): validation and psychometric properties. Arthritis Res Ther. 2009;11:R120. doi: 10.1186/ar2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res (Hoboken) 2010;62:600–10. doi: 10.1002/acr.20140. [DOI] [PubMed] [Google Scholar]
- 40.Bennett RM, Bushmakin AG, Cappelleri JC, Zlateva G, Sadosky AB. Minimal clinically important difference in the fibromyalgia impact questionnaire. J Rheumatol. 2009;36:1304–11. doi: 10.3899/jrheum.081090. [DOI] [PubMed] [Google Scholar]
- 41.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Medical care. 2001;39:800–12. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 42.Greco LA, Baer RA, Smith GT. Assessing mindfulness in children and adolescents: development and validation of the Child and Adolescent Mindfulness Measure (CAMM) Psychol Assess. 2011;23:606–14. doi: 10.1037/a0022819. [DOI] [PubMed] [Google Scholar]
- 43.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 44.Fields S, Leraas K, Collins C, Reynolds B. Delay discounting as a mediator of the relationship between perceived stress and cigarette smoking status in adolescents. Behav Pharmacol. 2009:20. doi: 10.1097/FBP.0b013e328330dcff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dickerson SS, Kemeny ME. Acute stressors and cortisol responses: a theoretical integration and synthesis of laboratory research. Psychol Bull. 2004;130:355–91. doi: 10.1037/0033-2909.130.3.355. [DOI] [PubMed] [Google Scholar]
- 46.Chorpita BF, Barlow DH. The development of anxiety: the role of control in the early environment. Psychol Bull. 1998;124:3–21. doi: 10.1037/0033-2909.124.1.3. [DOI] [PubMed] [Google Scholar]
- 47.March J. Manual for the Multidimensional Anxiety Scale for Children. 2. North Tonawanda, NY: Multi-Health Systems; 2012. (MASC 2) [Google Scholar]
- 48.March J. The Multidimensional Anxiety Scale for Children (MASC): Factor Structure, Reliability, and Validity. J Am Acad Child Adolesc Psychiatry. 1997;36:554–65. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- 49.Silverman WK, Fleisig W, Rabian B, Peterson RA. Childhood Anxiety Sensitivity Index. J Clin Child Psychol. 1991;20:162–8. [Google Scholar]
- 50.Peterson RA, Reiss S. Anxiety Sensitivity bzdex Manual. 2. Worthington, OH: International Diagnostic Systems; 1992. [Google Scholar]
- 51.Hewitt-Taylor J. Use of constant comparative analysis in qualitative research. Nurs Stand. 2001;15:39–42. doi: 10.7748/ns2001.07.15.42.39.c3052. [DOI] [PubMed] [Google Scholar]
- 52.Cunningham NR, Jagpal A, Tran ST, Kashikar-Zuck S, Goldschneider KR, Coghill RC, et al. Anxiety Adversely Impacts Response to Cognitive Behavioral Therapy in Children with Chronic Pain. J Pediatr. 2016 doi: 10.1016/j.jpeds.2016.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Eccleston C, Palermo TM, Fisher E, Law E. Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database Syst Rev. 2012;8:CD009660. doi: 10.1002/14651858.CD009660.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Palermo TM, Holley AL. The importance of the family environment in pediatric chronic pain. JAMA Pediatr. 2013;167:93–4. doi: 10.1001/jamapediatrics.2013.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Knook LM, Konijnenberg AY, van der Hoeven J, Kimpen JL, Buitelaar JK, van Engeland H, et al. Psychiatric disorders in children and adolescents presenting with unexplained chronic pain: what is the prevalence and clinical relevancy? Eur Child Adolesc Psychiatry. 2011;20:39–48. doi: 10.1007/s00787-010-0146-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kashikar-Zuck S, Ting TV, Arnold LM, Bean J, Powers SW, Graham TB, et al. Cognitive behavioral therapy for the treatment of juvenile fibromyalgia: a multisite, single-blind, randomized, controlled clinical trial. Arthritis Rheum. 2012;64:297–305. doi: 10.1002/art.30644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sil S, Kashikar-Zuck S. Understanding why cognitive-behavioral therapy is an effective treatment for adolescents with juvenile fibromyalgia. Int J Clin Rheumtol. 2013:8. doi: 10.2217/IJR.13.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cherkin DC, Sherman KJ, Balderson BH, Cook AJ, Anderson ML, Hawkes RJ, et al. Effect of Mindfulness-Based Stress Reduction vs Cognitive Behavioral Therapy or Usual Care on Back Pain and Functional Limitations in Adults With Chronic Low Back Pain: A Randomized Clinical Trial. JAMA. 2016;315:1240–9. doi: 10.1001/jama.2016.2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Goyal M, Singh S, Sibinga EM, Gould NF, Rowland-Seymour A, Sharma R, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med. 2014;174:357–68. doi: 10.1001/jamainternmed.2013.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tang YY, Holzel BK, Posner MI. The neuroscience of mindfulness meditation. Nat Rev Neurosci. 2015;16:213–25. doi: 10.1038/nrn3916. [DOI] [PubMed] [Google Scholar]
- 61.Creswell JD, Taren AA, Lindsay EK, Greco CM, Gianaros PJ, Fairgrieve A, et al. Alterations in Resting-State Functional Connectivity Link Mindfulness Meditation With Reduced Interleukin-6: A Randomized Controlled Trial. Biol Psychiatry. 2016 doi: 10.1016/j.biopsych.2016.01.008. [DOI] [PubMed] [Google Scholar]
- 62.Abhishek A, Doherty M. Mechanisms of the placebo response in pain in osteoarthritis. Osteoarthritis Cartilage. 2013;21:1229–35. doi: 10.1016/j.joca.2013.04.018. [DOI] [PubMed] [Google Scholar]
- 63.McDonald JL, Cripps AW, Smith PK. Mediators, Receptors, and Signalling Pathways in the Anti-Inflammatory and Antihyperalgesic Effects of Acupuncture. Evidence-based complementary and alternative medicine : eCAM. 2015;2015:975632. doi: 10.1155/2015/975632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lund I, Ge Y, Yu LC, Uvnas-Moberg K, Wang J, Yu C, et al. Repeated massage-like stimulation induces long-term effects on nociception: contribution of oxytocinergic mechanisms. Eur J Neurosci. 2002;16:330–8. doi: 10.1046/j.1460-9568.2002.02087.x. [DOI] [PubMed] [Google Scholar]
- 65.Zeidan F, Adler-Neal AL, Wells RE, Stagnaro E, May LM, Eisenach JC, et al. Mindfulness-Meditation-Based Pain Relief Is Not Mediated by Endogenous Opioids. J Neurosci. 2016;36:3391–7. doi: 10.1523/JNEUROSCI.4328-15.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zeidan F, Emerson NM, Farris SR, Ray JN, Jung Y, McHaffie JG, et al. Mindfulness Meditation-Based Pain Relief Employs Different Neural Mechanisms Than Placebo and Sham Mindfulness Meditation-Induced Analgesia. J Neurosci. 2015;35:15307–25. doi: 10.1523/JNEUROSCI.2542-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sibinga EM, Kerrigan D, Stewart M, Johnson K, Magyari T, Ellen JM. Mindfulness-based stress reduction for urban youth. J Altern Complement Med. 2011;17:213–8. doi: 10.1089/acm.2009.0605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sibinga EM, Webb L, Ghazarian SR, Ellen JM. School-Based Mindfulness Instruction: An RCT. Pediatrics. 2016;137:1–8. doi: 10.1542/peds.2015-2532. [DOI] [PubMed] [Google Scholar]
- 69.Jastrowski Mano KE, Salamon KS, Hainsworth KR, Anderson Khan KJ, Ladwig RJ, Davies WH, et al. A randomized, controlled pilot study of mindfulness-based stress reduction for pediatric chronic pain. Alternative therapies in health and medicine. 2013;19:8–14. [PubMed] [Google Scholar]
- 70.Zou K, Wong J, Abdullah N, Chen X, Smith T, Doherty M, et al. Examination of overall treatment effect and the proportion attributable to contextual effect in osteoarthritis: meta-analysis of randomised controlled trials. Ann Rheum Dis. 2016 doi: 10.1136/annrheumdis-2015-208387. [DOI] [PMC free article] [PubMed] [Google Scholar]