Abstract
Background
Accountable Care Organizations (ACO) attempt to provide the most efficient and effective care to patients within a region. We hypothesize that patients who undergo surgery closer to home have improved survival due to proximity of preoperative and post-discharge care.
Study Design
All (17,582) institutional American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) patients with a documented zip code and predicted risk who underwent surgery at our institution (2005–2014) were evaluated. Travel times were calculated by Google Maps, and patients were stratified by 1 hour of travel (local vs regional). Multivariable logistic regression and Cox Proportional Hazard models were used to evaluate the NSQIP risk-adjusted effects of travel time on operative morbidity, mortality, and long-term survival.
Results
Median travel time was 65 minutes with regional patients demonstrating significantly higher rates of ascites, hypertension, diabetes, disseminated cancer, >10% weight-loss, higher ASA, higher predicted risk of morbidity and mortality and lower functional status (all p<0.01). After adjusting for ACS NSQIP predicted risk, travel time was not significantly associated with 30-day mortality (OR 1.06, p=0.42) or any major morbidities (all p>0.05). However, survival analysis demonstrated travel time is an independent predictor of long-term mortality (OR 1.24, p<0.001)
Conclusions
Patients traveling farther for care at a quaternary center had higher rates of comorbidities and predicted risk of complications. Additionally, travel time predicts risk-adjusted long-term mortality, suggesting a major focus of ACOs will need to be integration of care at the periphery of their region.
Keywords: Travel Distance, Access to Care, Accountable Care Organizations, NSQIP
Introduction and Objective
The Patient Protection and Affordable Care Act (PPACA) continues to change the delivery and finances of healthcare across the United States through three major goals1–4: improved access to care, improved quality of care, and decreased cost of care. These include increasing access to care through insurance reform, the control of healthcare costs and a redesign of the delivery system through payment reform and the development of Accountable Care Organizations (ACOs)1,5. Initiated by the Center for Medicare and Medicaid Innovation (CMS), ACOs are responsible for the healthcare of an assigned patient population6. Physicians, hospitals, insurance companies, or municipalities can organize ACOs. These ACOs are led by either reorganized health systems or newly formed arrangements between independent physicians, hospitals and other providers. These programs receive initial payments on a fee-for-service basis. Several months to a year later following evaluation of the quality and cost of care the providers of care either receive bonuses or return monies5.
Tertiary and quaternary referral centers classically have large catchment areas that span wide regions resulting in long travel times for patients to receive surgical care7. Long travel times to these centers complicate the coordination of care across all phases. Preoperatively distance can delay diagnoses for patients living farther from referral centers8. During the hospitalization these patients sometimes also experience longer hospitals stays and increased mortality8–11. After discharge the responsibility for care typically returns to the patient’s primary care physician.
The ACS NSQIP provides an outstanding tool to evaluate preoperative risk factors, postoperative complications and 30-day outcomes12–14. The recent reorganization of our quaternary care institution into an ACO provided the opportunity to utilize our ACS NSQIP data to evaluate coordination of care prior to reorganization to identify improvement opportunities. We hypothesize that patients traveling further for surgical care have similar short-term outcomes despite having high risk of complications due to increased comorbidities compared to those patients receiving care close to home.
Patients and Methods
Patients
The University of Virginia Health Sciences Institutional Review Board approved the study with waiver of patient consent (Protocol #18801). Our ACS NSQIP database allowed identification of patients undergoing surgery at our academic medical center from 2005 to 2014. Using the unique case number identifier for cases at our institution we extracted all variables, including predicted risks of mortality and morbidity, from yearly Participant Use Files (PUFs), for further assessment. Patients without a home address were excluded from the analysis.
Distance Analysis
Travel times between each patient’s home address and the medical center address were calculated using Google Maps (Alphabet Inc. Mountain View, CA). These calculations do not acknowledge traffic but provide a standard travel time given distance and posted speed limit for each patient. A travel time of one hour was used to divide patients into local (<60 minutes) and regional (>60 minutes) groups.
Definitions
Standard ACS NSQIP variables were used to compare baseline and demographic factors between our patient populations. Previously validated NSQIP 30-day outcomes including mortality, readmission, and major morbidities were also compared. Long-term survival for each patient was assessed using Virginia Department of Health data included in our institutional Clinical Data Repository (CDR). Finally, estimated costs and actual charges were obtained from our institutional finance office through the CDR for cost analysis.
Statistical Analysis
The primary outcome was long-term survival after general surgery operations. Secondary outcomes included 30-day outcomes (mortality, readmission, complications) as well as total hospital cost. Statistical analyses were performed using student’s t-test and Mann-Whitney U-test as appropriate for continuous variables and chi-squared test for categorical variables. Additionally, survival analysis was performed with Kaplan Meier and Cox proportional hazards models. All analyses were performed using SAS version 9.4 (SAS Company, Cary NC) with an alpha set at 0.05 and all tests two-sided.
Results
Preoperative Comorbidity Incidence
A total of 17,582 cases were identified with a median travel time of 65 minutes and median distance of 54 miles. There were 8,006 (45.5%) cases in the local group traveling less than 1 hour and 9,576 (54.5%) cases in the regional group traveling more than 1 hour. Table 1 demonstrates the demographic and preoperative variables for each group. The regional group had higher rates of transfer status (6.3 vs 2.9%, p<0.0001), inpatient surgery (68.9 vs 56.2%, p<0.0001), and American Society of Anesthesiology (ASA) Classification >2 (48.7 vs 41.0%, p<0.0001) as well as higher rates of several medical comorbidities including ascites (2.2 vs 1.5%, p=0.0003), diabetes mellitus (18.6 vs 17.0%, p=0.004), hypertension (49.3 vs 46.1%, p<0.0001), disseminated cancer (4.3 vs 2.8%, p<0.0001), and steroid use (7.3 vs 4.8%, p<0.0001). Additionally, patients who travel further were more likely to have non-independent functional status (3.7 vs 3.0%, p=0.035), ventilator dependence (1.0 vs 0.7%, p=0.025) and > 10% weight loss in the past 6 months (6.1 vs 3.3%, p<0.0001). Finally, the predicted risk of both 30-day morbidity (12.7 vs 9.9%, p<0.0001) and 30-day mortality (1.5 vs 1.3%, p<0.0001) were significantly higher in the regional group compared to local cases driving less than 1 hour.
Table 1.
Preoperative Data
| Preoperative variables | < 1 hour | > 1 hour | p Value |
|---|---|---|---|
| Female sex, n (%) | 4,898 (61.18) | 5,722 (59.75) | 0.054 |
| White, n (%) | 6,287 (78.53) | 8,229 (85.93) | <0.0001 |
| Age, y, mean ± SD | 53.7 ± 16.4 | 53.8 ± 15.4 | 0.966 |
| BMI, kg/m2, mean ± SD | 30.8 ± 9.8 | 31.4 ± 10.2 | 0.010 |
| Transfer, n (%) | 231 (2.89) | 599 (6.27) | <0.0001 |
| Outpatient, n (%) | 3,504 (43.77) | 2,975 (31.07) | <0.0001 |
| Travel miles, mean ± SD | 22.7 ± 15.4 | 111.7 ± 63.6 | <0.0001 |
| Travel minutes, mean ± SD | 32.7 ± 15.8 | 118.0 ± 55.8 | <0.0001 |
| ASA > 2, n (%) | 3,280 (40.96) | 4,663 (48.69) | <0.0001 |
| Steroid use, n (%) | 383 (4.78) | 701 (7.32) | <0.0001 |
| Ascites, n (%) | 118 (1.47) | 212 (2.21) | 0.0003 |
| Congestive heart failure, n (%) | 33 (0.41) | 38 (0.40) | 0.873 |
| Chronic obstructive pulmonary disease, n (%) | 241 (3.01) | 329 (3.44) | 0.113 |
| Hypertension, n (%) | 3,694 (46.14) | 4,718 (49.27) | <0.0001 |
| Tobacco, n (%) | 1,716 (21.43) | 2,142 (22.37) | 0.136 |
| Dialysis dependent, n (%) | 166 (2.07) | 200 (2.09) | 0.944 |
| Diabetes, n (%) | 1,362 (17.01) | 1,783 (18.62) | 0.004 |
| Disseminated cancer, n (%) | 227 (2.84) | 412 (4.3) | <0.0001 |
| Dependent functional status, n (%) | 243 (3.04) | 355 (3.71) | 0.035 |
| Systemic sepsis, n (%) | 485 (6.06) | 445 (4.65) | <0.0001 |
| Ventilator dependent, n (%) | 58 (0.72) | 100 (1.04) | 0.025 |
| >10% weight loss, n (%) | 266 (3.32) | 582 (6.08) | <0.0001 |
| Emergency case, n (%) | 1,307 (16.33) | 788 (8.23) | <0.0001 |
| Predicted risk of morbidity, %, mean ± SD | 9.91 ± 12.6 | 12.72 ± 13.6 | <0.0001 |
| Predicted risk of 30-day mortality, %, mean ± SD | 1.33 ± 6.0 | 1.49 ± 6.1 | <0.0001 |
ASA, American Society of Anesthesiology.
Outcomes By Travel Distance
Table 2 demonstrates operative and postoperative characteristics between the local and regional groups. Patients in the regional group traveling more than 1 hour for surgical care had longer mean operative times (157.4 ± 114.7 vs 126.6 ± 95.0 minutes, p<0.0001) and total hospital length of stay (5.2 ± 10.2 vs 3.8 ± 8.4 days, p<0.0001) as well as preoperative hospital length of stay (0.78 ± 4.83 vs 0.55 ± 2.86 days, p<0.0001). Postoperative complication rates were higher in the regional group, however, prolonged ventilation >48 hours (2.4 vs 1.9%, p=0.026), wound infection (3.5 vs 2.4%, p<0.0001), and return to the operating room (5.3 vs 3.9%, p<0.0001) were the only variables to reach statistical significance between the groups. Despite the difference in predicted risk of 30-day mortality there was not statistical difference in actual 30-day mortality (1.4 vs 1.3%, p=0.50). The mortality difference was borne out over longer follow-up including 90-day mortality (2.9 vs 2.5%, p=0.053) and 1-year mortality (6.3 vs 5.1%, p=0.001). Finally, hospital cost ($17,600 vs $13,600, p<0.0001), hospital charges ($52,200 vs $40,300, p<0.0001), and physician charges ($19,700 vs $15,100, p<0.0001) were all significantly higher in the regional group traveling more than 1 hour for surgical care.
Table 2.
Postoperative Complications and Long-Term Outcomes
| Postoperative variables | < 1 hour | > 1 hour | p Value |
|---|---|---|---|
| Operative time, min, mean ± SD | 126.6 ± 95.0 | 157.4 ± 114.7 | <0.0001 |
| Length of stay, d, mean ± SD | 3.8 ± 8.4 | 5.2 ± 10.2 | <0.0001 |
| Cardiac arrest, n (%) | 33 (0.41) | 47 (0.49) | 0.441 |
| Myocardial infarction | 311 (3.14) | 300 (3.31) | 0.161 |
| Stroke, n (%) | 140 (1.17) | 250 (1.26) | 0.230 |
| Reintubation, n (%) | 120 (1.5) | 175 (1.83) | 0.091 |
| > 48 h ventilation, n (%) | 153 (1.91) | 230 (2.4) | 0.026 |
| Pulmonary embolism, n (%) | 37 (0.46) | 53 (0.55) | 0.398 |
| Pneumonia, n (%) | 77 (0.96) | 112 (1.17) | 0.183 |
| Wound infection, n (%) | 190 (2.37) | 337 (3.52) | <0.0001 |
| Urinary tract infection, n (%) | 157 (1.96) | 210 (2.19) | 0.284 |
| Renal failure, n (%) | 45 (0.56) | 62 (0.65) | 0.469 |
| Return to the operating room, n (%) | 313 (3.91) | 509 (5.32) | <0.0001 |
| 30-d readmission, n (%) | 67 (0.84) | 108 (1.13) | 0.053 |
| Mortality, n (%) | |||
| 30-d | 101 (1.26) | 132 (1.38) | 0.500 |
| 90-d | 196 (2.45) | 280 (2.92) | 0.053 |
| 1-y | 408 (5.1) | 60 (6.33) | 0.001 |
| Hospital charges, $, mean ± SD | 40,312 ± 77,446 | 52,225 ± 100,408 | <0.0001 |
| Hospital cost, $, mean ± SD | 13,647 ± 27,426 | 17,648 ± 32,754 | <0.0001 |
| Physician charges, $, mean ± SD | 15,109 ± 21,271 | 19,680 ± 41, 402 | <0.0001 |
Long-term Survival By Travel Distance
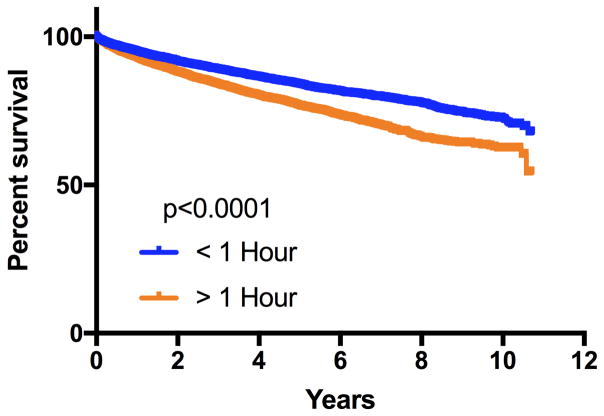
Kaplan Meier survival analysis is illustrated in Figure 1 with significantly increased long-term mortality in the regional group compared to the local group (p<0.0001). Table 3 contains results of the Cox Proportional Hazards modeling which demonstrates travel time independently predicts risk adjusted long-term mortality with a hazards ratio of 1.2 for every hour traveled (p<0.0001).
Figure 1.
Kaplan Meier long-term survival analysis.
Table 3.
Cox Proportional Hazards Model
| Parameter | Hazard ratio | p Value |
|---|---|---|
| Travel hours | 1.2 | <0.0001 |
| Predicted risk of 30-d mortality | 324.2 | <0.0001 |
| Year of surgery | 1.1 | <0.0001 |
Discussion
Patients traveling further for surgical care had higher predicted risk of morbidity and mortality secondary to increased preoperative comorbidities and surgical risk factors. Despite these differences, there was no difference in actual 30-day mortality based on travel time. However, there were higher rates of wound infection, reoperation, and prolonged ventilation in the regional group traveling more than 1 hour. Importantly, healthcare related costs and charges were significantly higher in the regional group. Finally, survival analysis demonstrated increased long-term mortality in the regional group that became apparent by 90-days and persisted over the 10-year study period.
As the nation moves toward an ACO model of care delivery this study demonstrated an important finding that tertiary care centers will provide care for the highest-risk surgical patients at the periphery of their region. These high-risk individuals with significantly higher rates of medical comorbidities require higher resource utilization as demonstrated by our cost analysis15–19. Specific attention to this population will be critical during the roll out of ACO’s to mitigate financial risk in the care of these patients20,21. However, it is reassuring that we demonstrate better than expected 30-day outcomes for the regional patients.
While some surgical risk factors such as transfer status, inpatient surgery and ASA >2 are higher in the regional group it is important to note the increased prevalence of emergency cases in the local patients. This suggests that our regional patients likely undergo surgery at their local centers for emergency care. We are unable to determine the impact and outcomes of this practice in the current study, however it will be important to understand this interaction since ACOs will require outstanding outcomes in the care of all patients in the most cost effective manner1,22. Future areas of research should focus on travel distance and level of care for emergency patients to define optimal management for them.
Long-term survival analysis demonstrated a difference in the two groups which begin to diverge at 90-days, with a clear survival advantage for local patients by 1-year post operatively. As we move toward bundled payments and 90-day, instead of 30-day outcome measures these factors will become more important.1,2,23,24. The financial implications of these changes will require new models to mitigate variability or risk corridors, to allow for cost shifting. The present study demonstrated the need to include patient location and distance from the quaternary care center into these models to adequately adjust for financial risk. While the ACSNSQIP database has become the gold standard for surgical outcome assessment, future work will need to shift from measurement of 30-day outcomes to more long-term effects of surgical intervention13.
Limitations of this study include a retrospective single center design mitigated by the use of the prospectively collected and validated ACS NSQIP database. Additionally, to evaluate fully the impact within the ACO territory would require further access to identified patient level data from all surgical cases at all institutions in the region. Finally, the future impacts of the PPACA are susceptible to the shifting political environment in which current policies were developed and are being implemented.
In conclusion this data demonstrated that quaternary care centers can expect to have higher risk surgical patients travel from the periphery of their care region. Despite differences in predicted risk of 30-day morbidity and mortality we demonstrate outcomes with no difference in actual 30-day survival. However, long-term survival analysis reveals disparities based on travel distance that suggests improved coordination of care is required for this high-risk population. Future research and implementation of ACO’s will require focus on methods to integrate care in the periphery of regions, as well as development of cost models to account for varying financial risk that includes travel distance.
Acknowledgments
Support: Research reported in this publication was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Numbers T32HL007849 and NIH T32AI0074.
Footnotes
Disclosure Information: Nothing to disclose.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Presented at the Southern Surgical Association 128th Annual Meeting, Palm Beach, FL, December 2016.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Britt LD, Hoyt DB, Jasak R, et al. Health care reform: impact on American surgery and related implications. Ann Surg. 2013;258:517–526. doi: 10.1097/SLA.0b013e3182a507de. [DOI] [PubMed] [Google Scholar]
- 2.Miller DC, Ye Z, Gust C, Birkmeyer JD. Anticipating the effects of accountable care organizations for inpatient surgery. JAMA Surg. 2013;148:549–554. doi: 10.1001/jamasurg.2013.1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ellimoottil C, Miller S, Ayanian JZ, Miller DC. Effect of insurance expansion on utilization of inpatient surgery. JAMA Surg. 2014;149:829–836. doi: 10.1001/jamasurg.2014.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bruch R. A Sea Change in Medicine: Current Shifts in the Delivery and Payment of Medical Care. N C Med J. 2016;77:261–264. doi: 10.18043/ncm.77.4.261. [DOI] [PubMed] [Google Scholar]
- 5.Hawken SR, Herrel LA, Ellimoottil C, et al. Understanding pre-enrollment surgical outcomes for hospitals participating in Medicare Accountable Care Organizations. Am J Surg. 2016;211:998–1004. doi: 10.1016/j.amjsurg.2015.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berkowitz SA, Ishii L, Schulz J, Poffenroth M. Academic Medical Centers Forming Accountable Care Organizations and Partnering With Community Providers: The Experience of the Johns Hopkins Medicine Alliance for Patients. Acad Med. 2016;91:328–332. doi: 10.1097/ACM.0000000000000976. [DOI] [PubMed] [Google Scholar]
- 7.Shahan CP, Bell T, Paulus E, Zarzaur BL. Emergency general surgery outcomes at safety net hospitals. J Surg Res. 2015;196:113–117. doi: 10.1016/j.jss.2015.02.044. [DOI] [PubMed] [Google Scholar]
- 8.Cote CL, Singh S, Yip AM, et al. Increased distance from the tertiary cardiac center is associated with worse 30-day outcomes after cardiac operations. Ann Thorac Surg. 2015;100:2213–2218. doi: 10.1016/j.athoracsur.2015.05.058. [DOI] [PubMed] [Google Scholar]
- 9.Chou S, Deily ME, Li S. Travel distance and health outcomes for scheduled surgery. Med Care. 2014;52:250–257. doi: 10.1097/MLR.0000000000000082. [DOI] [PubMed] [Google Scholar]
- 10.Jackson KL, Glasgow RE, Hill BR, et al. Does travel distance influence length of stay in elective colorectal surgery? Dis Colon Rectum. 2013;56:367–373. doi: 10.1097/DCR.0b013e31827e939e. [DOI] [PubMed] [Google Scholar]
- 11.Massarweh NN, Chiang YJ, Xing Y, et al. Association between travel distance and metastatic disease at diagnosis among patients with colon cancer. J Clin Oncol. 2014;32:942–948. doi: 10.1200/JCO.2013.52.3845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen ME, Bilimoria KY, Ko CY, Hall BL. Development of an American College of Surgeons National Surgery Quality Improvement Program: morbidity and mortality risk calculator for colorectal surgery. J Am Coll Surg. 2009;208:1009–1016. doi: 10.1016/j.jamcollsurg.2009.01.043. [DOI] [PubMed] [Google Scholar]
- 13.Raval MV, Cohen ME, Ingraham AM, et al. Improving American College of Surgeons National Surgical Quality Improvement Program risk adjustment: incorporation of a novel procedure risk score. J Am Coll Surg. 2010;211:715–723. doi: 10.1016/j.jamcollsurg.2010.07.021. [DOI] [PubMed] [Google Scholar]
- 14.Merkow RP, Ju MH, Chung JW, et al. Underlying reasons associated with hospital readmission following surgery in the United States. JAMA. 2015;313:483–495. doi: 10.1001/jama.2014.18614. [DOI] [PubMed] [Google Scholar]
- 15.Geyer BC, Peak DA, Velmahos GC, et al. Cost savings associated with transfer of trauma patients within an accountable care organization. Am J Emerg Med. 2016;34:455–458. doi: 10.1016/j.ajem.2015.11.067. [DOI] [PubMed] [Google Scholar]
- 16.Herzlinger RE, Schleicher SM, Mullangi S. Health care delivery innovations that integrate care? Yes!: But integrating what? JAMA. 2016;315:1109–1110. doi: 10.1001/jama.2016.0505. [DOI] [PubMed] [Google Scholar]
- 17.Rudnicki M, Armstrong JH, Clark C, et al. Expected and unexpected consequences of the Affordable Care Act: the impact on patients and surgeons-pro and con arguments. J Gastrointest Surg. 2016;20:351–360. doi: 10.1007/s11605-015-3032-8. [DOI] [PubMed] [Google Scholar]
- 18.Scally CP, Thumma JR, Birkmeyer JD, Dimick JB. Impact of surgical quality improvement on payments in Medicare patients. Ann Surg. 2015;262:249–252. doi: 10.1097/SLA.0000000000001069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schwartz DA, Hui X, Schneider EB, et al. Worse outcomes among uninsured general surgery patients: does the need for an emergency operation explain these disparities? Surgery. 2014;156:345–351. doi: 10.1016/j.surg.2014.04.039. [DOI] [PubMed] [Google Scholar]
- 20.Gani F, Lucas DJ, Kim Y, et al. Understanding variation in 30-day surgical readmission in the era of accountable care: effect of the patient, surgeon, and surgical subspecialties. JAMA Surg. 2015;150:1042–1049. doi: 10.1001/jamasurg.2015.2215. [DOI] [PubMed] [Google Scholar]
- 21.Scott JW, Salim A, Sommers BD, et al. Racial and regional disparities in the effect of the Affordable Care Act’s Dependent Coverage Provision on young adult trauma patients. J Am Coll Surg. 2015;221:495–501. e491. doi: 10.1016/j.jamcollsurg.2015.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Colla CH, Goodney PP, Lewis VA, et al. Implementation of a pilot accountable care organization payment model and the use of discretionary and nondiscretionary cardiovascular care. Circulation. 2014;130:1954–1961. doi: 10.1161/CIRCULATIONAHA.114.011470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Axelrod DA, Millman D, Abecassis MM. US Health Care Reform and Transplantation, Part II: impact on the public sector and novel health care delivery systems. Am J Transplant. 2010;10:2203–2207. doi: 10.1111/j.1600-6143.2010.03247.x. [DOI] [PubMed] [Google Scholar]
- 24.Chu DZ. Future of surgery: accountable care organizations and the end of private practice? J Am Coll Surg. 2011;213:810–811. doi: 10.1016/j.jamcollsurg.2011.09.007. [DOI] [PubMed] [Google Scholar]