Abstract
Talar bone cysts can develop as a result of osteochondral lesions of the talus. This can be a source of deep ankle pain. Open debridement and bone grafting of the bone cysts requires extensive soft tissue dissection and malleolar osteotomy. Removal of normal cartilage of the talus is frequently required to approach the bone cysts. Alternatively, the cysts can be grafted arthroscopically with minimal disruption of the normal cartilage surface. The key to success is careful preoperative planning with a computed tomogram of the ankle. Bone cyst of the posterior half of the talar body can be grafted via posterior ankle endoscopy. Bone cyst of the anterior half of the talar body can be debrided and grafted via anterior talar osseous portals. The purpose of this technical note is to describe a minimally invasive approach of curettage and bone grafting of the talar bone cysts with preservation of the articular surfaces.
Development of talar bone cysts can be attributed to the formation of osteochondral lesions (OCLs).1 Large bone cysts are frequently associated with large OCLs. Debridement of the OCL and resection of the underlying subchondral bone create an access to the underlying bone cyst. Debridement and bone grafting of the cyst can be performed without the need for removal of the normal cartilage adjacent to the OCL.2, 3, 4 Open debridement and bone grafting frequently imply that extensive soft tissue dissection is needed. In general, malleolar osteotomy would allow proper access to the lesion.5 An arthroscopic approach would reduce the surgical trauma and eliminate the need for osteotomy.5 Previously reported arthroscopic techniques approach bone cysts through the OCL.2, 3, 4, 6 This is feasible for a large OCL with a subchondral cyst adjacent to the lesion.
Subchondral cysts can develop as a result of the valve mechanism of the damaged cartilage allowing unidirectional intrusion of fluid from the joint space into the subchondral bone.1 Both stress shielding by pressurized fluid and osteocyte death may cause cyst growth.7 By this mechanism, huge subchondral bone cysts can form as a result of a small defect in the subchondral plate.1 In this case, normal cartilage adjacent to the OCL may need to be removed to achieve adequate visualization and debridement of the cyst wall during the arthroscopic procedures.8 In addition, the cyst might become uncontained and the bone graft of the cyst can drop into the ankle joint and become an intra-articular loose body.8 Moreover, reconstruction of the cartilaginous articular surface is difficult, if not impossible. The present technical note describes the arthroscopic approaches of debridement and bone grafting of talar bone cysts with minimal disruption of the normal cartilage surface. This procedure is indicated for talar bone cysts associated with small OCLs or intact articular surface but contraindicated if the cyst is adjacent to a large OCL or there is significant osteoarthrosis of the ankle joint (Table 1).
Table 1.
Pearls and Pitfalls of Arthroscopic Curettage and Bone Grafting of Talar Bone Cysts of the Right Ankle
| Pearls | Pitfalls |
|---|---|
| 1. Careful preoperative planning with computed tomogram is the key to success. | 1. It is not suitable for bone cysts adjacent to a large osteochondral lesion (OCL). |
| 2. Posterior talar bone cysts can be treated with posterior ankle endoscopy. | 2. It is not suitable in case of significant osteoarthrosis of the ankle. |
| 3. Anterior talar bone cysts can be approached with anterior osseous portals. | |
| 4. A trans-OCL portal can approach the bone cyst and eliminate the valve mechanism of OCL. |
Technique
Preoperative Planning and Patient Positioning
Preoperative computed tomogram is useful for preoperative planning and determination of the optimal arthroscopic approach and portals to be used (Fig 1). The posterior talar bone cyst can be approached through posterior ankle endoscopy with the patient in prone position.5, 8, 9 Anterior talar bone cyst can be approached through various trans-OCL and anterior bone portals, with the patient in supine position. The portals chosen should be closest to the cyst wall so that a minimum amount of bone is removed to access the bone cyst. The portals should be spaced out to avoid crowding of instruments and incomplete visualization and curettage.8
Fig 1.
Preoperative computed tomogram of the illustrated case. Transverse (A) and sagittal (B) views of the posterior talar cyst confirmed that the cyst is best approached by the posterior ankle endoscopy (arrows). Transverse (C) and sagittal (D) views of the anterior talar cyst showed that the cyst can be approached via the anterolateral bone portal (arrowheads).
A 4.0-mm 30° arthroscope (Dyonics, Smith & Nephew, Andover, MA) is used for the posterior ankle endoscopy and a 2.7-mm 30° arthroscope (Henke-Sass Wolf, Tuttlingen, Germany) is used for the anterior talar bone cyst endoscopy. A thigh tourniquet is applied to provide a bloodless operative field.
Portal Placement of Posterior Ankle Endoscopy
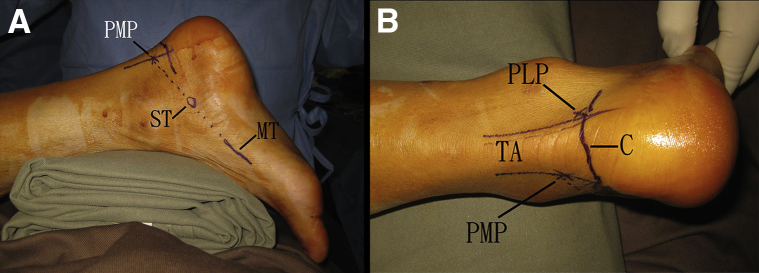
Posterior ankle endoscopy is performed with the posteromedial and posterolateral portals.9 The posterolateral portal is located at the lateral side of the Achilles tendon just above the posterior calcaneal tubercle. The posteromedial portal is located at the intersection between the medial border of the Achilles tendon and the line projecting from the undersurfaces of the sustentaculum tali and first metatarsal (Fig 2).5, 8, 10 More proximal placement of the posteromedial portal can reduce the risk of impingement of the posterior tibial neurovascular bundle by the instrument via this portal.11 Moreover, the plantar wall of the posterior talar cyst can be easily accessed via this modified posteromedial portal.8
Fig 2.
Posterior ankle endoscopy, with the patient in a prone position. (A) The posteromedial portal (PMP) is located at the intersection of the medial border of the Achilles tendon and the line joining the undersurfaces of the sustentaculum tali (ST) and first metatarsal (MT). (B) The posterolateral portal (PLP) is located at the lateral side of the Achilles tendon (TA) just above the posterior calcaneal tubercle (C).
Exploration, Curettage, and Bone Grafting of Posterior Talar Bone Cyst
The posterolateral portal is the viewing portal and the posterior talar tubercle is resected with an arthroscopic acromionizer (Dyonics; Smith & Nephew) via the posteromedial portal. The scope is switched to the posteromedial portal. The cut surface of the posterior talus is drilled with a 1.6-mm Kirschner wire (K-wire; Zimmer, Warsaw, IN) via the posterolateral portal. Extrusion of viscid gelatinous material implies that the bone cyst is reached (Fig 3).5 The K-wire is replaced with a 1.25-mm guidewire (Synthes, West Chester, PA). The posterior talus is then drilled with a 2.7-mm cannulated drill bit (Synthes) along the guidewire. After that, the 1.25-mm guidewire is replaced with a 2.8-mm guidewire (Synthes) and the posterior talus is drilled with a 5-mm cannulated drill bit (Synthes). Starting from this drill hole, the posterior wall of the bone cyst is resected with the acromionizer. The membranous lining of the cyst wall is resected with an arthroscopic shaver (Dyonics; Smith & Nephew), and microfracture of the cyst wall is performed with an arthroscopic awl (Smith & Nephew) (Fig 4). The cyst is then packed with autologous cancellous bone graft (harvested from the iliac crest) by means of a 3.5-mm drill sleeve (Synthes) (Fig 5). The posterolateral and posteromedial portals can be interchanged as the viewing and working portals for the procedure.
Fig 3.
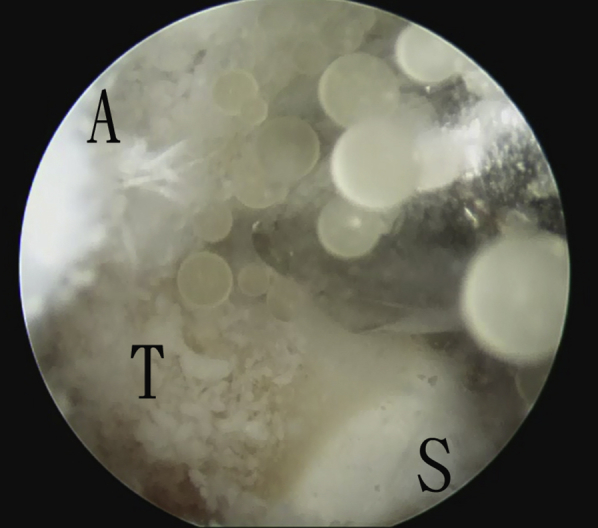
Posterior ankle endoscopy, with the patient in a prone position. The posteromedial portal is the viewing portal, and the posterolateral portal is the working portal. Extrusion of viscid gelatinous material during drilling of the posterior talus (T) implies that the posterior bone cyst is entered. (A, ankle joint; S, posterior subtalar joint.)
Fig 4.
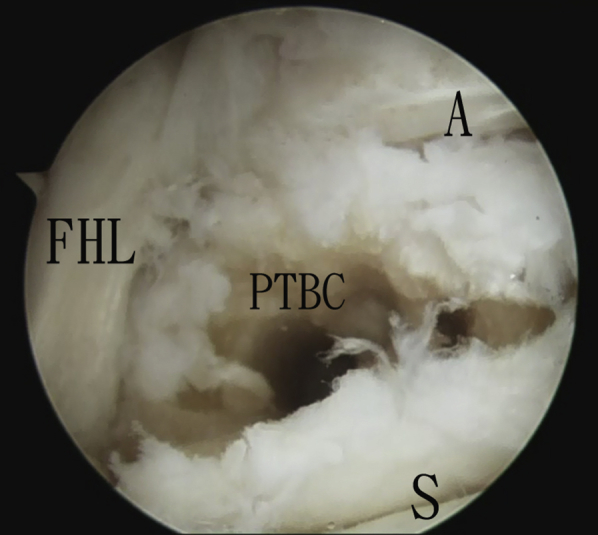
Posterior ankle endoscopy, with the patient in a prone position. Using the posterolateral portal as the viewing portal, the posterior cyst wall is resected and the posterior talar bone cyst is exposed. (A, ankle joint; FHL, flexor hallucis longus tendon; PTBC, posterior talar bone cyst; S, subtalar joint.)
Fig 5.
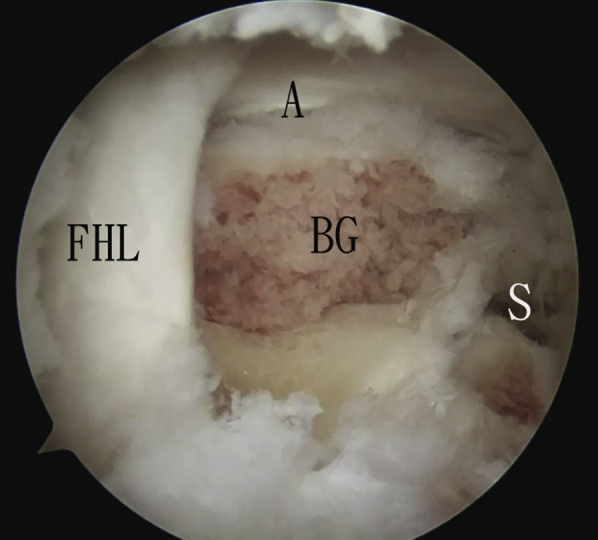
Posterior ankle endoscopy, with the patient in a prone position. The posteromedial portal is the viewing portal. The posterior talar bone cyst is packed with cancellous bone graft. (A, ankle joint; BG, bone graft; FHL, flexor hallucis longus tendon; S, subtalar joint.)
Portal Placement for Endoscopy of the Anterior Talar Bone Cyst
The patient is turned to supine position for anterior talar bone cyst endoscopy. Anterior ankle arthroscopy is performed through the standard anteromedial and anterolateral portals. The articular surfaces are examined for any OCL. In the illustrated case, the anterior talar bone cyst is associated with a lateral OCL. The anteromedial portal is the viewing portal. The OCL is debrided and the underlying subchondral bone is drilled with a 1.25-mm guidewire (Synthes) via the anterolateral portal. The ankle is plantarflexed to facilitate drilling of the subchondral bone. The trans-OCL portal is created by drilling of the subchondral bone with a 2.7-mm cannulated drill (Synthes) along the guidewire. After that, the 1.25-mm guidewire is exchanged with a 2.8-mm guidewire (Synthes). The trans-OCL portal is enlarged with a 5-mm cannulated drill (Synthes) along the 2.8-mm guidewire. A Wissinger rod (Richard Wolf, Knittlingen, Germany) is inserted via the anterolateral ankle portal and the trans-OCL portal. The arthroscope-cannula is inserted along the rod into the trans-OCL portal tract. The rod is then removed and the arthroscope is inserted into the cannula. The anterolateral bone portal that is at the lateral talar facet just anterior to the lateral malleolus is the other portal for the anterior talar bone cyst endoscopy of this illustrated case. The anterolateral bone portal is drilled with a 1.25-mm guidewire (Synthes) aiming the bone cyst. The anterolateral bone portal tract is sequentially enlarged by drilling with a 2.7-mm cannulated drill (Synthes) along the guidewire; exchange to a 2.8-mm guidewire (Synthes) and drilling with a 5-mm cannulated drill (Synthes) along the 2.8-mm guidewire (Fig 6).
Fig 6.
The patient is in a supine position. (A) Ankle arthroscopy. With the anteromedial ankle portal as the viewing portal, a Wissinger rod is inserted into the trans--osteochondral lesion (OCL) portal tract via the anterolateral ankle portal. (B) The arthroscope cannula is inserted into the trans-OCL portal tract along the Wissinger rod. (C) The arthroscope is in the trans-OCL portal (ToP). The anterolateral bone portal (ALBP) is created with a cannulated drill. (D) With the trans-OCL portal as the viewing portal, a guidewire is inserted from lateral (Lat) to medial (med). (C, anterior ankle capsule; OCL, osteochondral lesion; T, talar body.)
Debridement of the Cyst, Microfracture of the Cyst Walls and Bone Grafting
Trans-OCL portal is the viewing portal. The membranous lining of the cyst wall is resected with an arthroscopic shaver (Dyonics, Smith & Nephew) via the anterolateral bone portal (Fig 7). After debridement, the walls of the bone cavity are microfractured with an arthroscopic awl (Smith & Nephew) (Fig 8). The cavity is then packed with autologous cancellous bone graft by means of a 3.5-mm drill sleeve (Synthes) (Fig 9). The trans-OCL and anterolateral bone portals are interchanged as the viewing and working portals during the steps of microfracture and bone grafting. Ankle arthroscopy is repeated to confirm fill up of bone graft up to the surfaces of the bone portals and there is no loose bone graft dropping in the joint (Fig 10, Video 1). Postoperatively, the ankle is immobilized in a short leg cast for 6 to 8 weeks.
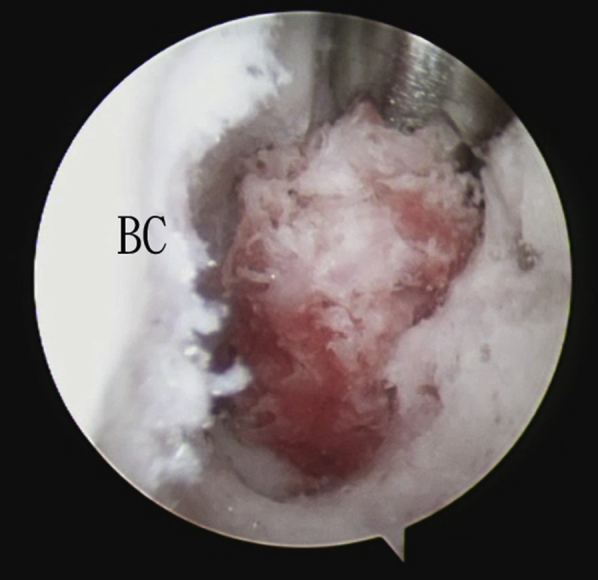
Fig 7.

The patient is in a supine position, and the trans--osteochondral lesion portal is the viewing portal. The membranous lining (M) of the anterior talar bone cyst (BC) is debrided with an arthroscopic shaver via the anterolateral bone portal.
Fig 8.

The patient is in a supine position, and the trans--osteochondral lesion portal is the viewing portal. Microfracture of the cyst wall (BC) is performed with an arthroscopic awl via the anterolateral bone portal.
Fig 9.
The patient is in a supine position, and the anterolateral bone portal is the viewing portal. The bone cyst (BC) is packed with cancellous bone graft by means of a drill sleeve via the trans--osteochondral lesion portal.
Fig 10.
The patient is in a supine position. Bone grafting is completed. (A) With the anteromedial ankle portal as the viewing portal, the cyst is grafted up to the surface of the osteochondral lesion (OCL). (B) With the anterolateral ankle portal as the viewing portal, the cyst is grafted up to the surface of the anterolateral bone portal (ALBP). The transverse (C) and sagittal (D) views of the postoperative computed tomogram show that the talar bone cysts have been filled up with bone graft. (LT, lateral facet of talar body; T, talar dome.)
Discussion
Careful preoperative planning with computed tomogram is the key to success for arthroscopic debridement and bone grafting of talar bone cysts.8 The posterior surface is the trapdoor of the talar body after removal of the posterior talar tubercle. Posterior ankle endoscopy can effectively address bone cysts of the posterior half of the talar body.8 However, it is difficult to access the cyst at the anterior half of the talar body, which results in excessive bone removal before reaching the anterior cyst. Various osseous portals at the talar neck (extrachondral), the talar dome (chondral), and talar facets (chondral) have been described for the anterior talar cysts.8 The extrachondral portal at the talar neck has the advantage of preservation of the articular surfaces. However, access to the cyst is usually limited, and a significant amount of bone may need to be removed before the cyst of the talar body can be reached. Osseous portal should be avoided at the talar dome, except the trans-OCL portal. Besides access to the bone cyst, the trans-OCL portal can also damage the valve mechanism of the OCL, which has been proposed as a mechanism of bone cyst formation. Osseous portals can be created at the medial and lateral talar facets, which bear 16% and 8% of the body weight, respectively. Intraoperative 3-dimensional imaging can be helpful for proper placement of the osseous portal tracts.
Compared with fluoroscopic guided curettage and bone grafting of the talar cyst,12 the arthroscopic approach can have better assessment of completeness of debridement.8 This reported technique has better preservation of the articular surface than conventional arthroscopic techniques and is particularly suitable for bone cysts associated with small OCLs.
The advantages of this minimally invasive technique include better cosmetic result, minimum soft tissue dissection, clear visualization of the cyst, no osteotomy, and preservation of the articular cartilage. The potential risk of this technique includes iatrogenic fracture of the talus, injuries to the posterior tibial neurovascular bundle, flexor hallucis longus tendon, collateral ligaments of the ankle, and the intermediate dorsal cutaneous branch of the superficial peroneal nerve and the saphenous nerve (Table 2). This is a technically difficult procedure and should be reserved for the experienced foot and ankle arthroscopists.
Table 2.
Advantages and Risks of Arthroscopic Curettage and Bone Grafting of Talar Bone Cysts of the Right Ankle
| Advantages | Risks |
|---|---|
| 1. Better cosmetic result | 1. Iatrogenic fracture of the talus |
| 2. Minimal soft tissue dissection | 2. Posterior tibial neurovascular bundle |
| 3. Clear visualization of the cyst | 3. Flexor hallucis longus tendon |
| 4. No osteotomy needed | 4. Collateral ligaments of the ankle |
| 5. Preservation of the articular cartilage | 5. Intermediate dorsal cutaneous branch of superficial peroneal nerve |
| 6. Saphenous nerve |
Footnotes
The author reports that he has no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Arthroscopic curettage and bone grafting of talar bone cysts of the right ankle. With the patient in a supine position, posterior ankle endoscopy is performed through the posteromedial and posterolateral portals. The posterior talus is drilled and the posterior wall of the posterior talar bone cyst is resected. The cyst is then packed with cancellous bone graft. Next, anterior ankle arthroscopy is performed, and the trans--osteochondral lesion (OCL) portal is created with the anteromedial portal as the viewing portal. The anterolateral bone portal is created with the trans-OCL portal as the viewing portal. The cyst wall is debrided and microfractured. The anterior bone cyst is packed with cancellous bone graft.
References
- 1.van Dijk C.N., Reilingh M.L., Zengerink M., van Bergen C.J.A. Osteochondral defects in the ankle: Why painful? Knee Surg Sports Traumatol Arthrosc. 2010;18:570–580. doi: 10.1007/s00167-010-1064-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Koulalis D., Schultz W. Massive intraosseous ganglion of the talus: Reconstruction of the articular surface of the ankle joint. Arthroscopy. 2000;16:E14. doi: 10.1053/jars.2000.8949. [DOI] [PubMed] [Google Scholar]
- 3.Ogilvie-Harris D.J., Sarrosa E.A. Arthroscopic treatment of post-traumatic cysts of the talus. Arthroscopy. 2000;16:197–201. doi: 10.1016/s0749-8063(00)90036-7. [DOI] [PubMed] [Google Scholar]
- 4.Uysal M., Akpinar S., Ozalay M. Arthroscopic debridement and grafting of an intraosseous talar ganglion. Arthroscopy. 2005;21:1269e1–1269e4. doi: 10.1016/j.arthro.2005.07.012. [DOI] [PubMed] [Google Scholar]
- 5.Lui T.H. Arthroscopic bone grafting of talar bone cyst using posterior ankle arthroscopy. J Foot Ankle Surg. 2013;52:529–532. doi: 10.1053/j.jfas.2013.03.034. [DOI] [PubMed] [Google Scholar]
- 6.Lu J.Y., Tang K.L., Deng Y.L. Operative treatment of bone cyst of talus through the arthroscope: a report of 1 case. Zhongguo Gu Shang. 2008;21:232. [PubMed] [Google Scholar]
- 7.Cox L.G., Lagemaat M.W., van Donkelaar C.C. The role of pressurized fluid in subchondral bone cyst growth. Bone. 2011;49:762–768. doi: 10.1016/j.bone.2011.06.028. [DOI] [PubMed] [Google Scholar]
- 8.Lui T.H. Endoscopic curettage and bone grafting of huge talar bone cyst with preservation of cartilaginous surfaces: Surgical planning. Foot Ankle Surg. 2014;20:248–252. doi: 10.1016/j.fas.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 9.van Dijk C.N., Scholten P.E., Krips R. A 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy. 2000;16:871–876. doi: 10.1053/jars.2000.19430. [DOI] [PubMed] [Google Scholar]
- 10.Lui T.H. Flexor hallucis longus tendoscopy: A technical note. Knee Surg Sports Traumatol Arthrosc. 2009;17:107–110. doi: 10.1007/s00167-008-0623-x. [DOI] [PubMed] [Google Scholar]
- 11.Lui T.H., Chan L.K. Posterior ankle and hindfoot endoscopy: A cadaveric study. Foot Ankle Surg. 2016;22:186–190. doi: 10.1016/j.fas.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 12.Cebesoy O. Intraosseous ganglion of the talus treated with the talonavicular joint approach without exposing the ankle joint. J Am Podiatr Med Assoc. 2007;97:424–427. doi: 10.7547/0970424. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic curettage and bone grafting of talar bone cysts of the right ankle. With the patient in a supine position, posterior ankle endoscopy is performed through the posteromedial and posterolateral portals. The posterior talus is drilled and the posterior wall of the posterior talar bone cyst is resected. The cyst is then packed with cancellous bone graft. Next, anterior ankle arthroscopy is performed, and the trans--osteochondral lesion (OCL) portal is created with the anteromedial portal as the viewing portal. The anterolateral bone portal is created with the trans-OCL portal as the viewing portal. The cyst wall is debrided and microfractured. The anterior bone cyst is packed with cancellous bone graft.