Abstract
The meniscal root attachments are critical for meniscal function by securing the menisci in place and allowing optimal shock absorption in the knee. Successful meniscal root repair has been shown to restore the knee's tibiofemoral contact pressure to the same state as an intact meniscus. Although there have been multiple different repair techniques described, there is no report in the literature regarding the use of 2 simple cinch-loop sutures for a meniscal root repair. This article presents an arthroscopic lateral meniscal root repair technique involving the use of 2 simple cinch-loop configuration sutures and tibial suture anchor fixation.
The meniscal root attachments are critical for meniscal function by securing the menisci in place and allowing optimal shock absorption in the knee. Recently, studies have shown the importance of posterior root integrity to maintain mean contact pressure across the tibiofemoral joint.1, 2, 3, 4, 5 Meniscal root tears detrimentally impair meniscal kinematics and biomechanics through meniscal extrusion, ultimately rendering the meniscus nonfunctional and leading to degenerative arthritis in the knee.6, 7, 8, 9 For the meniscus to function properly, it must be securely attached to the tibial plateau.3, 4 Furthermore, it has been shown that successful meniscal root repair can restore tibiofemoral contact pressure to the same state as an intact meniscus.1, 2, 4, 7, 10 Different suture configurations for meniscal root repair have been tested biomechanically.10, 11, 12, 13 However, there is no report in the literature regarding the use of 2 simple cinch-loop sutures for a meniscal root repair. This article presents an arthroscopic lateral meniscal root repair technique involving the use of 2 simple cinch-loop configuration sutures and tibial suture anchor fixation.
Surgical Technique
Lateral meniscal root tears are most commonly associated with anterior cruciate ligament (ACL) tears.14, 15, 16 This is the situation in the described case. The root repair is performed prior to ACL reconstruction, but final tibial fixation is completed after ACL reconstruction.
Objective Diagnosis
Root tears of the lateral meniscus can be difficult to diagnose preoperatively on magnetic resonance imaging if the meniscofemoral ligaments are intact.17 However, on some occasions, the lateral root tear is seen nicely on the coronal views on magnetic resonance imaging (Fig 1). These tears are common with ACL tears, so one must carefully probe the lateral meniscal root at the time of surgery (Fig 2).
Fig 1.
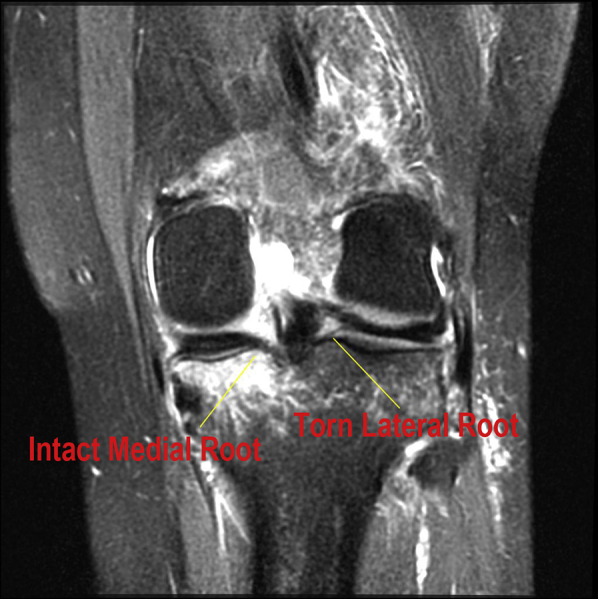
Left knee magnetic resonance image, coronal view. The intact medial meniscal root (left) is attached to the tibia. The torn lateral meniscal root (right) is above the anatomic attachment point.
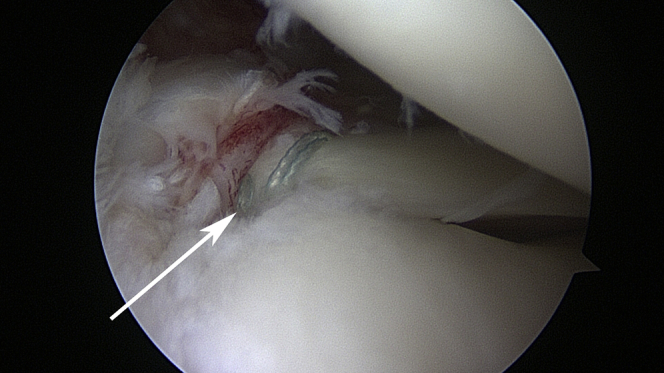
Fig 2.
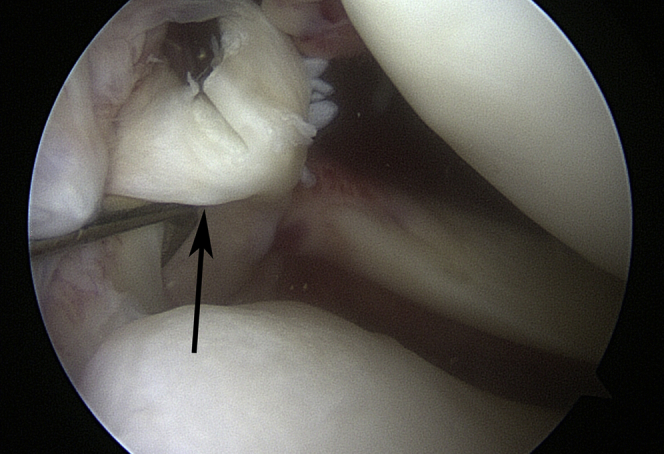
Left knee viewed through lateral portal, with patient lying supine. The torn lateral meniscal root is visualized arthroscopically (arrow). During anterior cruciate ligament reconstruction, it is important to probe the anatomic root to ensure proper attachment because lateral meniscal root tears often go undiagnosed with concomitant anterior cruciate ligament tears.
Patient Positioning
This surgical technique involves the patient lying supine, with easy manipulation of the affected joint. A foot-holding mechanism is recommended to keep the knee at the desired degree of flexion during the procedure.
Passage of Meniscal Root Cinch Sutures
An arthroscopic curette is used to debride the normal root attachment on the posterolateral tibia for the lateral meniscus. Sutures in the root of the lateral meniscus can be placed from either a standard lateral or medial parapatellar portal because pathologic elevation of the root of the lateral meniscus off the lateral tibial plateau after a tear makes suture placement just as accessible from the medial portal. The first step in suturing the root of the lateral meniscus is placement of a PassPort Cannula (Arthrex, Naples, FL) through the chosen portal for suture passage; this facilitates suture management to avoid inadvertent development of a soft-tissue bridge with suture passage, which is frustrating to deal with (Fig 3). In this case, the cannula was placed in the medial parapatellar portal. Suturing is performed with a Knee Scorpion device (Arthrex) (Video 1). A No. 0 FiberWire (Arthrex) folded in its midportion is loaded into the lower jaw of the device. Partially deploying the needle with the trigger “captures” the suture, thus preparing it for passage (Fig 4).
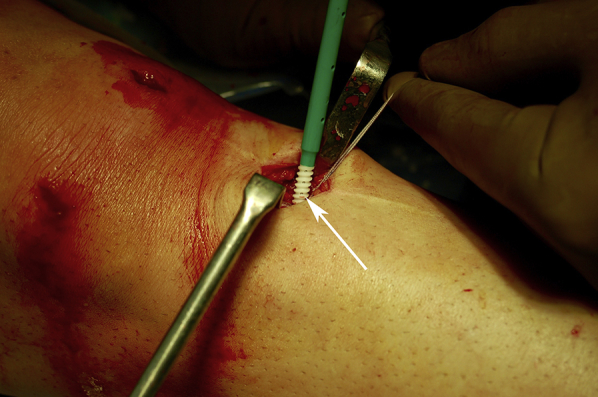
Fig 3.
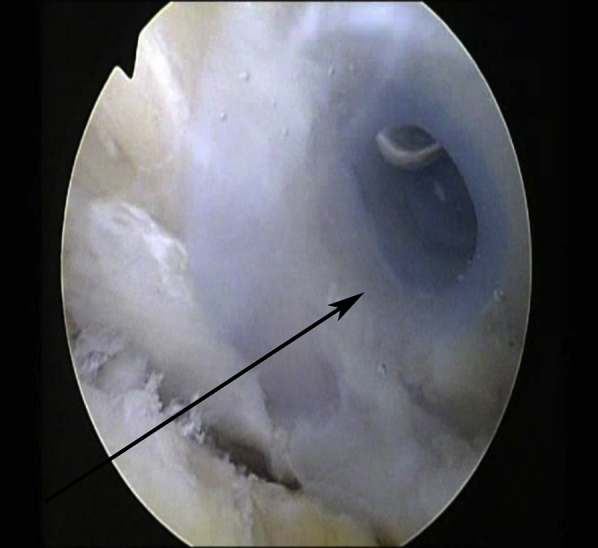
Left knee viewed through lateral portal, with patient lying supine. The PassPort Cannula (arrow), 8 mm in diameter and 20 mm long, is in place through the anteromedial portal. This allows for passage of meniscal root sutures and avoidance of troublesome portal soft-tissue bridges.
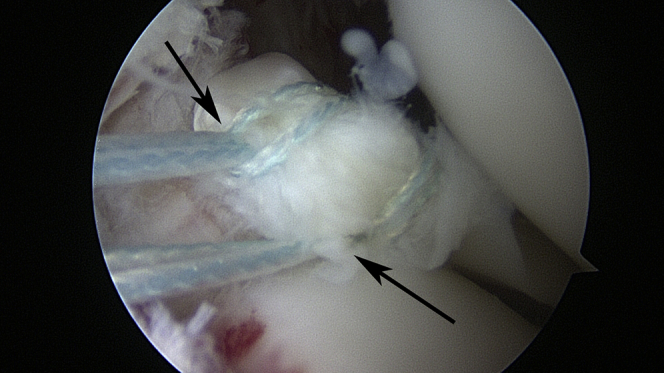
Fig 4.
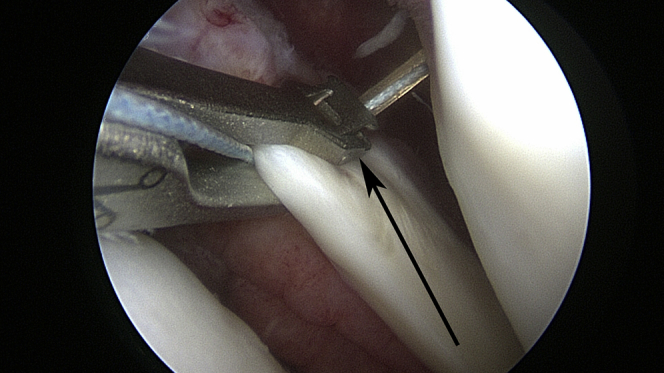
Left knee viewed from lateral portal, with patient lying supine. The folded No. 0 FiberWire is passed through the attachment of the posterior horn root of the lateral meniscus with a Knee Scorpion device, which is delivered through the joint through a PassPort Cannula in the anteromedial portal. Squeezing the Knee Scorpion handles passes the needle with the No. 0 FiberWire suture through the lateral meniscal root as a loop to allow for the cinch configuration. The top jaw of the Knee Scorpion captures the suture in one step because it is self-retrieving (arrow). The Knee Scorpion, now with the attached suture loop, is then removed from the joint through the PassPort Cannula.
While the surgeon is viewing laterally with the arthroscope, the Knee Scorpion is brought through the medial portal through the PassPort Cannula for the first suture pass. The lower jaw of the opened Knee Scorpion is placed under the root of the lateral meniscus near its normal bony attachment. The trigger of the Knee Scorpion is deployed and the upper jaw then captures the suture so that pulling the Knee Scorpion out of the joint brings the No. 0 FiberWire suture out of the PassPort Cannula as one simple step of both passing and retrieving the suture. Firing the Knee Scorpion trigger again releases the No. 0 FiberWire suture as a U-shaped loop outside the PassPort Cannula. Next, the 2 free ends of the No. 0 FiberWire suture are passed through this loop, thereby creating a “cinch” configuration as the 2 free ends are pulled to slide the cinch down to the posterior horn of the lateral meniscus. The cinch suture is then retrieved with a looped grasping device (Arthrex) above the posterior horn of the lateral meniscus and pulled out the lateral portal so as to be out of the way prior to drilling the bone socket. The aforementioned steps are repeated so that 2 cinch-type sutures are placed in the posterior horn root of the lateral meniscus (Fig 5).
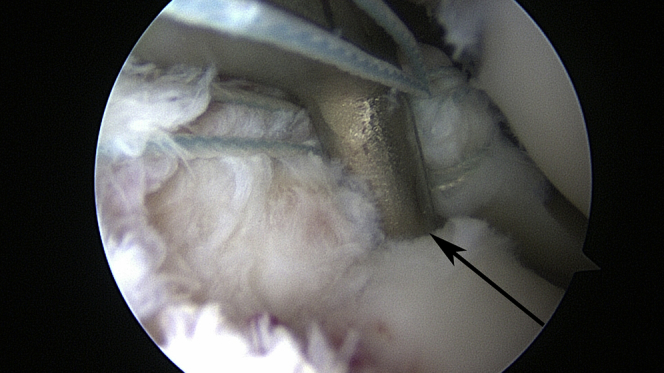
Fig 5.
Left knee viewed from lateral portal, with patient lying supine. Outside the joint through the PassPort Cannula in the anteromedial portal, the 2 free ends of the No. 0 FiberWire suture are passed through the loop to create the cinch configuration. The cinch is then slid down to the posterior horn of the lateral meniscus by pulling on the free ends of the No. 0 FiberWire suture. This suturing process is repeated so that there are two No. 0 FiberWire cinch-loop sutures (arrows) in place in the lateral meniscal root.
Creation of Tibial Bone Socket
Next, attention is directed toward the creation of a tibial bone socket to reduce the lateral meniscal root securely to bone. This requires drilling from the tibia up into the joint, which necessitates anterior tibial exposure. Because this root repair is being performed concomitantly with an ACL reconstruction, a 2-cm medial tibial incision is made medial and just proximal to the tibial tuberosity, which can also be used to create the tibial tunnel for the ACL reconstruction. The periosteum is mobilized to expose the bone. Retrodrilling from inside the joint is performed with a 6.0-mm FlipCutter (Arthrex)—a 3.5-mm-diameter pin that converts to a 6.0-mm reamer. An ACL tibial aiming device (Arthrex) is positioned through the medial portal with the tip of the guide intra-articularly at the normal anatomic attachment for the lateral meniscal root (Figs 6 and 7).
Fig 6.
Left knee viewed laterally, with patient lying supine. The tibial anterior cruciate ligament aiming guide (Arthrex) is passed through the medial portal PassPort Cannula and positioned (arrow) at the anatomic attachment of the posterior root of the lateral meniscus off the posterior-central-lateral tibial plateau. This serves as a guide for the FlipCutter retrocutting device and allows drill entrance in the joint at the appropriate location to create the tibial bone socket for the lateral meniscal root repair.
Fig 7.

Left knee, with patient lying supine. The tibial anterior cruciate ligament aiming guide and guide sleeve (arrows) (Arthrex) are viewed from outside the knee. The knee is flexed to 60°, and the guide is passed through the medial portal and positioned arthroscopically at the anatomic insertion of the posterior root of the lateral meniscus. The 6.0-mm-diameter FlipCutter is drilled as a 3.5-mm guide pin through the guide sleeve across the tibia to the point of the aimer in the joint through the small medial tibia incision, which also will be used for creation of the anterior cruciate ligament tibial socket.
With the surgeon viewing laterally with the arthroscope and holding the ACL aiming guide sleeve securely to the proximal tibia, the 3.5-mm FlipCutter pin is drilled up into the joint, exiting out the posterior-central-lateral tibia at the point of the ACL tibial aimer (Fig 4). In hard tibial bone, the hole for the FlipCutter can be predrilled with a 3.5-mm drill bit to make for easier passage of the 3.5-mm FlipCutter pin. The next step is to slide back the guide sleeve from the FlipCutter pin so that the ACL tibial aimer can be removed through the PassPort Cannula, leaving the pin in place. The guide sleeve is then tapped 7 mm into the bone of the proximal tibia marked by a hub at that point. This ensures access to this drill hole in the tibia. The FlipCutter device is then deployed as a 6.0-mm reamer from a straight pin by squeezing the button of the FlipCutter device that is out the proximal tibia (Fig 8). With the surgeon drilling in the forward setting, a socket is retrodrilled to a depth of 15 mm in the posterior tibia with the FlipCutter. With the surgeon still drilling in the forward setting, the FlipCutter is brought back into the joint. During the drilling process, the arthroscope can be moved to the medial portal so that an arthroscopic shaver (Arthrex) can be used from the lateral portal to remove bone debris from creating this tibial socket (Fig 8). The FlipCutter is then converted back to a straight pin by squeezing the button so that it can be removed through the guide sleeve of the proximal tibia.
Fig 8.
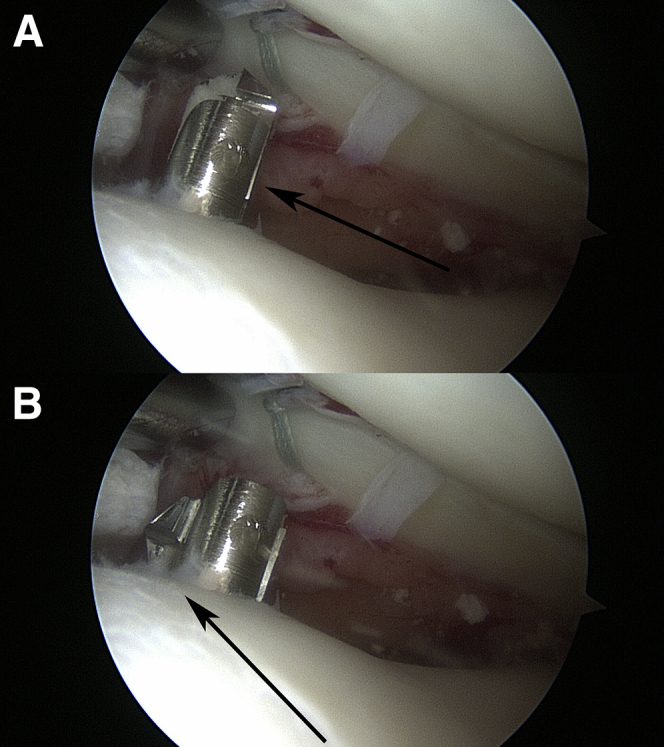
Left knee viewed through lateral portal, with patient lying supine. (A) Once the FlipCutter is drilled across the tibia into the joint as a 3.5-mm pin (arrow), the button on the pin is depressed and slid forward. (B) This “flips” the pin into a 6.0-mm retrodrill (arrow). One should note that the shaver is passed through the medial portal to allow removal of bone fragments from the tibial reaming process. The socket is cut to the appropriate depth of 15 mm, delivered back into the joint and “unflipped” with the button on the device, and removed from the joint through the guide sleeve. Importantly, the guide sleeve is tapped 7 mm into the proximal-medial tibia, which provides a preserved conduit for later suture passage.
Suture Passage Into Tibial Socket
The next step is to pass a No. 2 FiberStick suture (Arthrex) in its red plastic sheath to be retrieved on the joint side as a suture shuttle for the two No. 0 FiberWire cinch sutures in the posterior horn of the lateral meniscus. This is prepared by folding the FiberStick suture in half and passing the folded end in the sheath, which is facilitated by the fact that half of the suture is pre-stiffened to where the folded loop is just coming out the end of the plastic sheath. This sheath loaded with the No. 2 FiberStick suture is then passed through the still-engaged guide sleeve 7 mm in the tibia into the joint (Fig 9). With the surgeon viewing medially, a looped suture grasper from the lateral portal is used to retrieve this loop of the No. 2 FiberStick suture below the posterior horn of the lateral meniscus and pull it out the lateral portal. This No. 2 FiberStick loop out the lateral portal is then used to shuttle the two No. 0 FiberWire cinch sutures from the posterior root of the lateral meniscus into the created tibial socket to secure the root of the lateral meniscus here with fixation on the proximal tibia. Pulling on the 2 cinch sutures out the small hole from the proximal tibia securely reduces the root to the bone socket to enhance bony reattachment of the root.
Fig 9.
Left knee viewed laterally, with patient lying supine. A No. 2 TigerStick suture (left arrow) (Arthrex) in its red sheath is passed through the guide sleeve that had been tapped in place in the proximal-medial tibia. This enters the joint in the created tibial socket, and the suture is retrieved through the anteromedial portal to shuttle back the two No. 0 FiberWire cinch-loop sutures (right arrow) placed in the torn lateral meniscal root.
Tibial Fixation of Meniscal Root Sutures
Secure cortical fixation of the 2 cinch sutures in the root of the lateral meniscus is performed on the tibia with a 4.75-mm BioComposite SwiveLock anchor (Arthrex). A 2.4-mm guide pin is drilled 1.5 cm distal to the FlipCutter tibial hole. This is over-reamed with a 4.5-mm reamer to a depth of 20 mm to accept the 19.1-mm-long SwiveLock anchor. The tibial cortex is tapped with a 4.5-mm tap because this bone is generally hard. With the knee flexed to 60°, the free ends of the 2 cinch sutures are passed through the eyelet of the SwiveLock anchor, pulled tight, and secured in the reamed hole by holding the paddle of the SwiveLock anchor and turning the knob of the handle clockwise until the SwiveLock anchor is flush to the bone (Fig 10). The completed lateral meniscal root repair can then be seen arthroscopically when viewed from the lateral portal (Fig 11).
Fig 10.
Left knee, with patient lying supine. The two No. 0 FiberWire lateral meniscal root sutures exiting out the small 3.5-mm tibial drill hole from the FlipCutter are passed through the eyelet of a 4.75-mm BioComposite SwiveLock anchor. A 2.4-mm drill pin is inserted into the proximal-medial tibia 1.5 cm distal to the hole with the 2 FiberWire cinch-loop sutures (arrow). This pin is then over-reamed to a depth of 20 mm with a 4.5-mm reamer. Next, with the knee flexed to approximately 60°, the SwiveLock anchor is gently tapped into the 4.5-mm reamed hole and then screwed in, holding the paddle handle until the anchor is flush to the tibial cortex to optimize fixation. This completes the lateral meniscal root repair.
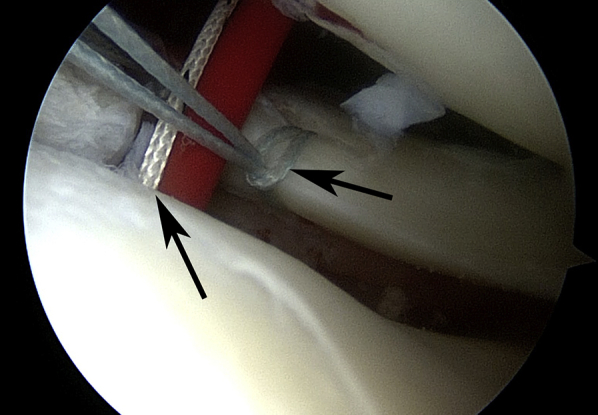
Fig 11.
Left knee viewed laterally. Final arthroscopic confirmation of secure fixation for the posterior root repair of the lateral meniscus is performed. The two No. 0 FiberWire cinch sutures have been pulled down through the FlipCutter socket hole (arrow), pulling the meniscal root securely to its anatomic bony attachment.
Discussion
The meniscal root attachments aid meniscal function by securing the menisci to bone anteriorly and posteriorly; for the meniscus to function properly, it must be properly attached to the tibial plateau.3, 4 Recently, studies have shown the importance of posterior root integrity to maintain mean contact pressure across the tibiofemoral joint.1, 4, 5, 7, 10 Furthermore, it has been shown that successful meniscal root repair constitutes the restoration of the knee's tibiofemoral contact pressure to the same state as an intact meniscus.1, 2, 4, 7, 10
Clinically, meniscal root tears detrimentally impair meniscal kinematics and biomechanics through meniscal extrusion, ultimately rendering the meniscus nonfunctional and leading to degenerative arthritis in the knee, particularly with medial meniscal tears.18, 19, 20 Lateral meniscal root tears have been associated more commonly with ACL tears.14, 15, 16 Repairing the lateral meniscal root has been shown to enhance stability in an experimental mode.7, 21
Recent attention has focused on meniscal root tears and their subsequent repair from both an anatomic and nonanatomic approach to set treatment parameters.2, 22, 23, 24, 25 To date, few studies have investigated individual biomechanical properties of meniscus–suture fixation techniques used for meniscal root repairs.10, 11, 25 LaPrade et al.24 evaluated the two–simple suture technique, modified Mason-Allen technique, and 1 and 2 double-locking loop techniques for meniscal root repair. They found that resistance to failure for all 4 techniques was well above the threshold for the normal rehabilitation forces placed on a root repair. Likewise, Mitchell et al.11 studied the effects of 4 different repair constructs using a No. 0 FiberWire, including a single (simple) suture, double (2 simple) sutures, a loop stitch, and a locking loop stitch. They found that although none of these constructs sufficiently replicated the native load-to-failure strength of the meniscal root, the locking loop stitch came the closest. There have been no reported biomechanical or clinical studies with use of a 2 cinch-type suture configuration for meniscal root repair. The advantages of a cinch suture include ease of placement and the resultant loop through the meniscus; this could potentially improve strength compared with other configurations such as simple sutures.
A lateral meniscal root tear in combination with an ACL tear was repaired arthroscopically through a bone socket. It was facilitated by use of the Knee Scorpion, an arthroscopic suturing device designed specifically for the knee, being more low profile than the Scorpion Suture Passer (Arthrex) used in the shoulder commonly for rotator cuff repair (Tables 1 and 2). Another potential advantage of the described technique is creation of a bone socket in the posterior-lateral tibial meniscal root attachment site to enhance bleeding and biological incorporation of the root reattachment (Table 1). This is performed with an inside-out reaming technique with the FlipCutter. Finally, cortical tibial fixation is easily achieved with use of a SwiveLock anchor as opposed to tying sutures over a button, which has been described.7, 26 Overall, these technological advancements simplify performance of meniscal root repair, which can be a challenging procedure, in an efficient, time-preserving manner.
Table 1.
Advantages and Disadvantages of Arthroscopic Lateral Meniscal Root Repair With Use of 2 Cinch-Loop Sutures
| Advantages |
| Ease of suture passage with intra-articular Knee Scorpion |
| Good meniscal fixation with 2 cinch sutures in root tissue |
| Knee Scorpion is flexible so other preferred suture configurations can be used |
| Secure fixation of lateral meniscal root to bone socket |
| Drilling root repair socket from medial tibial incision allows for only one tibial incision because tibial socket is drilled through this same incision |
| Ease of tibial fixation using SwiveLock anchor for cortical fixation |
| Quick, efficient root repair procedure, which takes less valuable operating room time |
| Disadvantages |
| Pulling a bit of lateral meniscal root tissue into bone socket could theoretically shorten meniscus |
| Risk of suture cutout from meniscal root with range of motion and/or joint loading |
| Specialized instrumentation is necessary |
Table 2.
Pearls and Pitfalls of Arthroscopic Lateral Meniscal Root Repair With Use of 2 Cinch-Loop Sutures
| The PassPort Cannula should be used in the medial portal for suture placement and creation of the cinch configuration to avoid a portal soft-tissue bridge or suture entrapment. |
| If easier suture passage is achieved through the lateral portal with the Knee Scorpion, then the surgeon should just move the PassPort Cannula laterally to do so. Ultimate shuttling of the 2 cinch sutures into the tibial bone socket is the same. |
| In hard tibial bone, the surgeon can predrill with a 3.5-mm drill with the anterior cruciate ligament tibial aimer to create a pathway for the 3.5-mm FlipCutter to then be passed more easily across the tibia into the joint. |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: P.A.S. receives support from Arthrex (consultancy fees, research support, royalties for Knee Scorpion) and Spinal Simplicity (stock or stock options). J.A.B. receives support from Arthrex (funded travel and accommodations for a mandatory coordinator meeting).
Supplementary Data
Combined arthroscopic repair of a lateral meniscal root avulsion and anterior cruciate ligament (ACL) tear in a left knee. With the patient in the supine position, it is essential that the knee is held at the proper angle of flexion with a foot holder. As the narration describes the root repair technique, it is vital to remember that the drilling of the root repair socket from the medial tibial incision allows for only one tibial incision as the ACL tibial socket is drilled through this same incision. Likewise, the lateral meniscal root is securely attached to the bone through the 2 cinch sutures and tibial fixation with the SwiveLock.
References
- 1.Geeslin A.G., Civitarese D., Turnbull T.L., Dornan G.J., Fuso F.A., LaPrade R.F. Influence of lateral meniscal posterior root avulsions and the meniscofemoral ligaments on tibiofemoral contact mechanics. Knee Surg Sports Traumatol Arthrosc. 2016;24:1469–1477. doi: 10.1007/s00167-015-3742-1. [DOI] [PubMed] [Google Scholar]
- 2.Bhatia S., LaPrade C.M., Ellman M.B., LaPrade R.F. Meniscal root tears: Significance, diagnosis, and treatment. Am J Sports Med. 2014;42:3016–3030. doi: 10.1177/0363546514524162. [DOI] [PubMed] [Google Scholar]
- 3.Ahn J.H., Lee Y.S., Chang J.Y., Chang M.J., Eun S.S., Kim S.M. Arthroscopic all inside repair of the lateral meniscus root tear. Knee. 2009;16:77–80. doi: 10.1016/j.knee.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 4.Allaire R., Muriuki M., Gilbertson L., Harner C.D. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 5.Perez-Blanca A., Espejo-Baena A., Amat Trujillo D. Comparative biomechanical study on contact alterations after lateral meniscus posterior root avulsion, transosseous reinsertion, and total meniscectomy. Arthroscopy. 2016;32:624–633. doi: 10.1016/j.arthro.2015.08.040. [DOI] [PubMed] [Google Scholar]
- 6.LaPrade R.F., LaPrade C.M., James E.W. Recent advances in posterior meniscal root repair techniques. J Am Acad Orthop Surg. 2015;23:71–76. doi: 10.5435/JAAOS-D-14-00003. [DOI] [PubMed] [Google Scholar]
- 7.LaPrade C.M., Jansson K.S., Dornan G., Smith S.D., Wijdicks C.A., LaPrade R.F. Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am. 2014;96:471–479. doi: 10.2106/JBJS.L.01252. [DOI] [PubMed] [Google Scholar]
- 8.Fairbank T.J. Knee joint changes after meniscectomy. J Bone Joint Surg Br. 1948;30:664–670. [PubMed] [Google Scholar]
- 9.Berthiaume M.J., Raynauld J.P., Martel-Pelletier J. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis. 2005;64:556–563. doi: 10.1136/ard.2004.023796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anz A.W., Branch E.A., Saliman J.D. Biomechanical comparison of arthroscopic repair constructs for meniscal root tears. Am J Sports Med. 2014;42:2699–2706. doi: 10.1177/0363546514549445. [DOI] [PubMed] [Google Scholar]
- 11.Mitchell R., Pitts R., Kim Y.M., Matava M.J. Medial meniscal root avulsion: A biomechanical comparison of 4 different repair constructs. Arthroscopy. 2016;32:111–119. doi: 10.1016/j.arthro.2015.07.013. [DOI] [PubMed] [Google Scholar]
- 12.Feucht M.J., Grande E., Brunhuber J., Burgkart R., Imhoff A.B., Braun S. Biomechanical evaluation of different suture techniques for arthroscopic transtibial pull-out repair of posterior medial meniscus root tears. Am J Sports Med. 2013;41:2784–2790. doi: 10.1177/0363546513502464. [DOI] [PubMed] [Google Scholar]
- 13.Feucht M.J., Grande E., Brunhuber J. Biomechanical evaluation of different suture materials for arthroscopic transtibial pull-out repair of posterior meniscus root tears. Knee Surg Sports Traumatol Arthrosc. 2015;23:132–139. doi: 10.1007/s00167-013-2656-z. [DOI] [PubMed] [Google Scholar]
- 14.Feucht M.J., Bigdon S., Bode G. Associated tears of the lateral meniscus in anterior cruciate ligament injuries: Risk factors for different tear patterns. J Orthop Surg Res. 2015;10:34. doi: 10.1186/s13018-015-0184-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.De Smet A.A., Blankenbaker D.G., Kijowski R., Graf B.K., Shinki K. MR diagnosis of posterior root tears of the lateral meniscus using arthroscopy as the reference standard. AJR Am J Roentgenol. 2009;192:480–486. doi: 10.2214/AJR.08.1300. [DOI] [PubMed] [Google Scholar]
- 16.Brody J.M., Lin H.M., Hulstyn M.J., Tung G.A. Lateral meniscus root tear and meniscus extrusion with anterior cruciate ligament tear. Radiology. 2006;239:805–810. doi: 10.1148/radiol.2393050559. [DOI] [PubMed] [Google Scholar]
- 17.Pula D.A., Femia R.E., Marzo J.M., Bisson L.J. Are root avulsions of the lateral meniscus associated with extrusion at the time of acute anterior cruciate ligament injury?: A case control study. Am J Sports Med. 2014;42:173–176. doi: 10.1177/0363546513506551. [DOI] [PubMed] [Google Scholar]
- 18.Kim J.H., Chung J.H., Lee D.H., Lee Y.S., Kim J.R., Ryu K.J. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: A prospective comparison study. Arthroscopy. 2011;27:1644–1653. doi: 10.1016/j.arthro.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 19.Kim S.B., Ha J.K., Lee S.W. Medial meniscus root tear refixation: Comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy. 2011;27:346–354. doi: 10.1016/j.arthro.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 20.Ahn J.H., Lee Y.S., Yoo J.C., Chang M.J., Park S.J., Pae Y.R. Results of arthroscopic all-inside repair for lateral meniscus root tear in patients undergoing concomitant anterior cruciate ligament reconstruction. Arthroscopy. 2010;26:67–75. doi: 10.1016/j.arthro.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 21.Schillhammer C.K., Werner F.W., Scuderi M.G., Cannizzaro J.P. Repair of lateral meniscus posterior horn detachment lesions: A biomechanical evaluation. Am J Sports Med. 2012;40:2604–2609. doi: 10.1177/0363546512458574. [DOI] [PubMed] [Google Scholar]
- 22.Johannsen A.M., Civitarese D.M., Padalecki J.R., Goldsmith M.T., Wijdicks C.A., LaPrade R.F. Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sports Med. 2012;40:2342–2347. doi: 10.1177/0363546512457642. [DOI] [PubMed] [Google Scholar]
- 23.Moon H.K., Koh Y.G., Kim Y.C., Park Y.S., Jo S.B., Kwon S.K. Prognostic factors of arthroscopic pull-out repair for a posterior root tear of the medial meniscus. Am J Sports Med. 2012;40:1138–1143. doi: 10.1177/0363546511435622. [DOI] [PubMed] [Google Scholar]
- 24.LaPrade C.M., LaPrade M.D., Turnbull T.L., Wijdicks C.A., LaPrade R.F. Biomechanical evaluation of the transtibial pull-out technique for posterior medial meniscal root repairs using 1 and 2 transtibial bone tunnels. Am J Sports Med. 2015;43:899–904. doi: 10.1177/0363546514563278. [DOI] [PubMed] [Google Scholar]
- 25.LaPrade R.F., LaPrade C.M., Ellman M.B., Turnbull T.L., Cerminara A.J., Wijdicks C.A. Cyclic displacement after meniscal root repair fixation: A human biomechanical evaluation. Am J Sports Med. 2015;43:892–898. doi: 10.1177/0363546514562554. [DOI] [PubMed] [Google Scholar]
- 26.Ahn J.H., Wang J.H., Yoo J.C., Noh H.K., Park J.H. A pull out suture for transection of the posterior horn of the medial meniscus: Using a posterior trans-septal portal. Knee Surg Sports Traumatol Arthrosc. 2007;15:1510–1513. doi: 10.1007/s00167-007-0310-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Combined arthroscopic repair of a lateral meniscal root avulsion and anterior cruciate ligament (ACL) tear in a left knee. With the patient in the supine position, it is essential that the knee is held at the proper angle of flexion with a foot holder. As the narration describes the root repair technique, it is vital to remember that the drilling of the root repair socket from the medial tibial incision allows for only one tibial incision as the ACL tibial socket is drilled through this same incision. Likewise, the lateral meniscal root is securely attached to the bone through the 2 cinch sutures and tibial fixation with the SwiveLock.


