Abstract
Purpose
The objective of this study was to elucidate the long-term prognosis of patients with implantable cardioverter-defibrillators (ICDs) in Korea.
Materials and Methods
We enrolled 405 patients (age, 57.7±16.7 years; 311 men) who had undergone ICD implantation. The patients were divided into three groups: heart failure (HF) and ICD for primary (group 1, n=118) and secondary prevention (group 2, n=93) and non-HF (group 3, n=194). We compared appropriate and inappropriate ICD therapy delivery among the groups and between high- (heart rate ≥200 /min) and low-rate (<200 /min) ICD therapy zones.
Results
During the follow-up period (58.9±49.8 months), the annual appropriate ICD therapy rate was higher in group 2 (10.4%) than in groups 1 and 3 (6.1% and 5.9%, respectively, p<0.001). There were no significant differences in annual inappropriate ICD therapy rate among the three groups. In group 1, the annual appropriate ICD therapy rate was significantly lower in patients with a high-rate versus a low-rate therapy zone (4.5% and 9.6%, respectively, p=0.026). In group 3, the annual inappropriate ICD therapy rate was significantly lower in patients with a high-rate versus a low-rate therapy zone (3.1% and 4.0%, respectively, p=0.048).
Conclusion
Appropriate ICD therapy rates are not low in Korean patients with ICD, relative to prior large-scale studies in Western countries. Appropriate and inappropriate ICD therapy could be reduced by a high-rate therapy zone in patients with HF and ICD for primary prevention, as well as non-HF patients, respectively.
Keywords: Heart failure, implantable cardioverter-defibrillator, primary prevention, sudden cardiac death
INTRODUCTION
Implantable cardioverter-defibrillators (ICDs) are effective in improving survival in patients who have experienced sudden cardiac arrest.1,2,3,4 Previous large-scale randomized trials have shown that ICDs are also beneficial in patients at high risk who have not experienced sudden cardiac arrest, such as selective patients with heart failure (HF) with reduced ejection fraction.5,6,7,8,9 According to the 2013 American College of Cardiology Foundation/American Heart Association guidelines for the management of HF, ICD implantation is recommended for primary prevention of sudden cardiac death in patients with HF with an ejection fraction ≤35% and New York Heart Association (NYHA) functional class II or III on optimal medical therapy, based on Class of Recommendation (I) and Level of Evidence (A).10 The MADIT-RIT trial showed that inappropriate ICD therapy and all-cause mortality can be reduced by programming a high-rate ICD therapy zone.11 However, inappropriate and unnecessary ICD therapies remain challenging problems. In addition, the complication rate related to ICD implantation is not negligible.12 The long-term prognosis of Asian patients with HF and ICD for primary prevention is not well-known. The purpose of this study was to elucidate annual ICD therapy rates and the effects of a high-rate ICD therapy zone in Korean patients with ICD.
MATERIALS AND METHODS
The study design was approved by an Institutional Review Board and was conducted in compliance with the Declaration of Helsinki. We consecutively enrolled 405 patients (age, 57.7±16.7 years; 311 men) who underwent ICD or cardiac resynchronization therapy-defibrillator (CRT-D) implantation between October 1997 and March 2015 in the Severance ICD and CRT registry. The patients were divided into three groups: HF with ICD or CRT-D for primary (group 1) and secondary prevention (group 2) and non-HF with ICD for primary and secondary prevention (group 3). ICDs and CRT-Ds were implanted according to the contemporary guidelines for ICD and CRT-D implantation.13,14,15 Patients with an ICD or CRT-D were seen for follow-up at the outpatient clinic every 3 months or on special occasions, including ICD alarm and ICD therapy delivery. We reviewed medical records to obtain information on baseline clinical characteristics, electrocardiography, cardiac imaging studies (including echocardiography, computed tomography, and magnetic resonance images), coronary angiography, clinical diagnoses, ICD indications, defibrillator types, appropriate and inappropriate ICD therapy, and mortality. HF was defined as a left ventricular ejection fraction ≤40% and included non-ischemic (including dilated cardiomyopathy) and ischemic HF. Non-HF heart disease included inherited primary arrhythmia syndrome (Brugada syndrome, long QT syndrome, early repolarization syndrome, catecholaminergic polymorphic ventricular tachycardia, and idiopathic ventricular fibrillation); hypertrophic, restrictive, and arrhythmogenic right ventricular cardiomyopathies; and congenital heart disease. ICD indications were classified as primary and secondary prevention of sudden cardiac death. Secondary prevention was defined as prevention in patients who had experienced sudden cardiac arrest or sustained ventricular tachyarrhythmia. In contrast, primary prevention was defined as prevention in patients who had not previously experienced sudden cardiac arrest or sustained ventricular tachyarrhythmia. Defibrillator types included single- and dual-chamber ICDs and CRT-D. High- and low-rate ICD therapy zones, defined according to the heart rate that triggers ICD therapy, were set at ≥200 /min and <200 /min, respectively. A high-rate ICD therapy zone was set according to the physicians' discretion. Appropriate ICD therapy was defined as anti-tachycardial pacing and ICD shock for ventricular tachyarrhythmia. In contrast, inappropriate ICD therapy was defined as anti-tachycardial pacing and ICD shock for arrhythmias other than ventricular tachyarrhythmia. Outcomes included appropriate and inappropriate ICD therapy delivery and all-cause mortality. We compared the annual numbers of patients who experienced appropriate and inappropriate ICD therapy and mortality among the patients in the three groups. We also analyzed the annual numbers of patients who experienced appropriate and inappropriate ICD therapy and mortality between patients with high- and low-rate ICD therapy zones in each group.
Statistical analyses
The results are expressed as means±standard deviations for continuous data and numbers (%) for categorical data. We compared clinical parameters among the groups using Student's t-test or ANOVA for normally distributed continuous data and the χ2 test for categorical data. The Kaplan-Meier method was used to analyze cumulative incidence rates for appropriate and inappropriate ICD therapy and mortality. Appropriate and inappropriate ICD therapy and all-cause mortality among the groups were compared by log-rank test. A p value <0.05 was considered significant. Data were analyzed using the Statistical Package for the Social Sciences, version 20.0 (IBM Corporation, Armonk, NY, USA).
RESULTS
Baseline characteristics and appropriate/inappropriate ICD therapy in each group
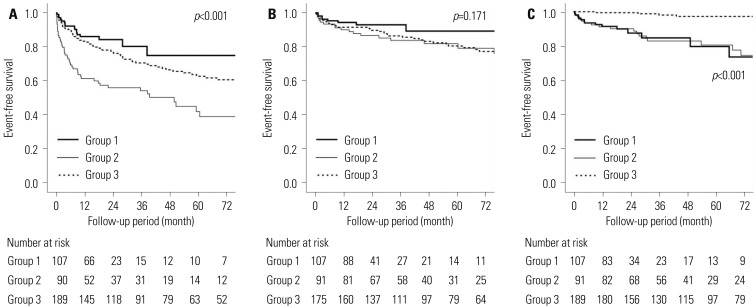
Table 1 shows the baseline characteristics of all 405 patients stratified by group, including 118 patients in group 1, 93 patients in group 2, and 194 patients in group 3. The diagnoses of patients in group 3 were as follows: idiopathic ventricular fibrillation in 60 patients, Brugada syndrome in 47 patients, long QT syndrome in 13 patients, early repolarization syndrome in 6 patients, and catecholaminergic polymorphic ventricular tachycardia in 1 patient. The patients were followed for 58.9±49.8 months. The patients in group 1 had a significantly higher NYHA functional class, lower ejection fraction, higher frequency of non-ischemic HF, and fewer single-chamber ICDs than the patients in group 2. The patients in group 1 were significantly older, more often female, had higher frequencies of hypertension, diabetes mellitus, atrial fibrillation, a lower ejection fraction, fewer single-chamber ICDs, and less frequent high-rate ICD therapy zone than the patients in group 3. Significantly more patients in group 2 experienced appropriate ICD therapy per year than the patients in group 1 (Table 2, Fig. 1A). However, there were no significant differences in annual inappropriate ICD therapy and annual mortality between groups 1 and 2 (Table 2, Fig. 1B). There were no significant differences in the annual number of patients who received appropriate and inappropriate ICD therapy between groups 1 and 3 (p=0.309 and 0.126, respectively) (Fig. 1). However, annual mortality was significantly higher in groups 1 and 2 than in group 3 (Table 2, Fig. 1C). Ten (8.5%), 20 (21.5%), and 39 (20.1%) patients experienced inappropriate ICD therapy in groups 1, 2, and 3, respectively. In groups 1 and 2, the causes of inappropriate ICD therapy were atrial fibrillation (14 patients), noise sensing (8 patients), T wave oversensing (3 patients), sinus tachycardia (3 patients), and supraventricular tachycardia (2 patients). In group 3, the causes of inappropriate ICD therapy were sinus tachycardia (11 patients), atrial fibrillation (8 patients), noise sensing (7 patients), supraventricular tachycardia (6 patients), T wave oversensing (4 patients), and unknown cause (3 patients).
Table 1. Baseline Characteristics of the Patients in Each Group.
| Group 1 (n=118) | Group 2 (n=93) | Group 3 (n=194) | p value | |
|---|---|---|---|---|
| Age (yr) | 65.5±12.2 | 64.6±13.4 | 49.7±16.8 | <0.001* |
| Male, n (%) | 79 (66.9) | 70 (75.3) | 162 (83.5) | 0.003† |
| Hypertension, n (%) | 52 (44.1) | 47 (50.5) | 41 (21.1) | <0.001* |
| Diabetes, n (%) | 47 (39.8) | 27 (29.0) | 15 (7.7) | <0.001* |
| Atrial fibrillation, n (%) | 41 (34.7) | 18 (19.4) | 11 (5.7) | <0.001* |
| NYHA functional class | 2.5±0.6 | 2.0±0.9 | <0.001 | |
| Ejection fraction (%) | 23.6±6.6 | 33.2±12.3 | 61.7±11.3 | <0.001‡ |
| Etiology, n (%) | ||||
| Non-ischemic HF | 78 (66.1) | 45 (48.4) | 0.010 | |
| Ischemic HF | 40 (33.9) | 48 (51.6) | 0.010 | |
| IPAS | 127 (65.5) | |||
| HCMP | 37 (19.1) | |||
| ARVC | 13 (6.7) | |||
| CHD | 12 (6.2) | |||
| RCMP | 3 (1.5) | |||
| Miscellanea | 2 (1.0) | |||
| β-blocker use, n (%) | 81 (68.6) | 72 (77.4) | 150 (77.3) | 0.187 |
| Amiodarone use, n (%) | 21 (17.8) | 36 (38.7) | 13 (6.7) | <0.001‡ |
| ACEI/ARB use, n (%) | 105 (89.0) | 78 (83.9) | 31 (16.0) | <0.001* |
| Defibrillator type, n (%) | ||||
| Single-chamber | 37 (31.4) | 60 (64.5) | 141 (72.7) | <0.001‡ |
| Dual-chamber | 42 (35.6) | 29 (31.2) | 53 (27.3) | 0.257 |
| CRT-D | 39 (33.1) | 4 (4.3) | 0 (0.0) | <0.001 |
| High-rate ICD therapy zone, n (%) | 56 (47.5) | 45 (48.4) | 129 (66.5) | 0.001† |
ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker; ARVC, arrhythmogenic right ventricular cardiomyopathy; CHD, congenital heart disease; CRT-D, cardiac resynchronization therapy-defibrillator; HCMP, hypertrophic cardiomyopathy; HF, heart failure; ICD, implantable cardioverter-defibrillator; IPAS, inherited primary arrhythmia syndrome; NYHA, New York Heart Association; RCMP, restrictive cardiomyopathy.
*Group 3 is significantly different from groups 1 and 2, †Group 3 is significantly different from groups 1, ‡The three groups are significantly different from each other.
Table 2. Outcomes of the Patients in Each Group.
| Group 1 (n=118) | Group 2 (n=93) | Group 3 (n=194) | p value | |
|---|---|---|---|---|
| Follow-up period (months) | 31.7±33.5 | 61.8±42.7 | 73.9±54.4 | <0.001* |
| Patients who experienced appropriate ICD therapy, annual (%) | 6.1 | 10.4 | 5.9 | <0.001† |
| Patients who experienced inappropriate ICD therapy, annual (%) | 3.2 | 4.2 | 3.2 | 0.171 |
| Annual mortality (%) | 4.5 | 3.8 | 0.4 | <0.001‡ |
ICD, implantable cardioverter-defibrillator.
*The three groups are significantly different from each other, †Group 2 is significantly different from groups 1 and 3, ‡Group 3 is significantly different from groups 1 and 2.
Fig. 1. Appropriate (A) and inappropriate (B) implantable cardioverter-defibrillator (ICD) therapy, and all-cause mortality (C) in patients in three groups. Group 1, heart failure (HF) and ICD for primary prevention; group 2, HF and ICD for secondary prevention; group 3, non-HF and ICD.
High- and low-rate ICD therapy zones(Table 3)
Table 3. Baseline Characteristics and Outcomes in the Patients of a High- and Low-Rate ICD Therapy Zone in Each Group.
| Group 1 | Group 2 | Group 3 | ||||
|---|---|---|---|---|---|---|
| High-rate (n=56)* | Low-rate (n=60)* | High-rate (n=45)* | Low-rate (n=47)* | High-rate (n=129)* | Low-rate (n=64)* | |
| Age (yr) | 66.2±13.0 | 64.8±11.7 | 61.8±13.4 | 67.1±13.2 | 49.3±16.2 | 50.1±17.9 |
| Male, n (%) | 40 (71.4) | 37 (61.7) | 33 (73.3) | 37 (78.7) | 105 (81.4) | 57 (89.1) |
| Hypertension, n (%) | 31 (55.4)† | 20 (33.3)† | 21 (46.7) | 25 (53.2) | 25 (19.4) | 16 (25.0) |
| Diabetes, n (%) | 27 (48.2) | 19 (31.7) | 14 (31.1) | 13 (27.7) | 7 (5.4) | 8 (12.5) |
| Ischemic HF, n (%) | 24 (42.9) | 16 (26.7) | 21 (46.7) | 26 (55.3) | 0 (0) | 0 (0) |
| NYHA functional class | 2.5±0.6 | 2.6±0.5 | 1.9±0.9 | 2.1±0.9 | − | − |
| Ejection fraction (%) | 23.8±8.3 | 23.4±4.5 | 33.5±12.1 | 33.0±12.7 | 63.5±10.4† | 58.3±12.2† |
| Defibrillator type, n (%) | ||||||
| Single-chamber | 21 (37.5) | 14 (23.3) | 32 (71.1) | 28 (59.6) | 101 (78.3)† | 39 (60.9)† |
| Dual-chamber | 34 (60.7) | 45 (75.0) | 11 (24.4) | 18 (38.3) | 28 (21.7)† | 25 (39.1)† |
| CRT-D | 1 (1.8) | 1 (1.7) | 2 (4.4) | 1 (2.1) | 0 (0) | 0 (0) |
| Follow-up period (month) | 34.3±30.7 | 24.6±23.7 | 68.5±46.4 | 55.4±38.8 | 83.9±53.3† | 51.9±48.1† |
| Patients who experienced ICD therapy (%) | ||||||
| Appropriate, annual | 3.7† | 10.6† | 9.3 | 11.5 | 5.3 | 8.3 |
| Inappropriate, annual | 1.9 | 5.7 | 4.3 | 4.1 | 2.7† | 5.4† |
| Annual mortality | 5.0 | 4.0 | 1.9 | 6.0 | 0.4 | 0.4 |
CRT-D, cardiac resynchronization therapy-defibrillator; HF, heart failure; ICD, implantable cardioverter-defibrillator; NYHA, New York Heart Association.
*ICD therapy zone has been changed in 2, 1, and 1 patient in group 1, 2, and 3, respectively, †p<0.05.
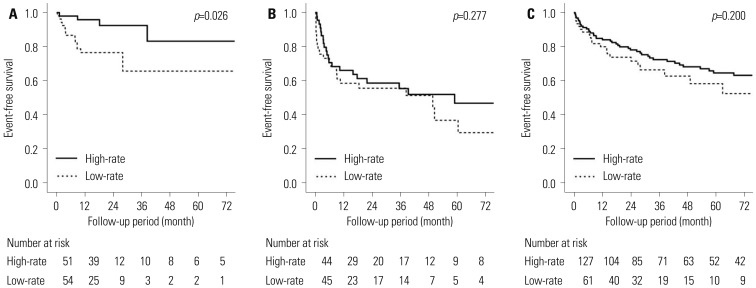
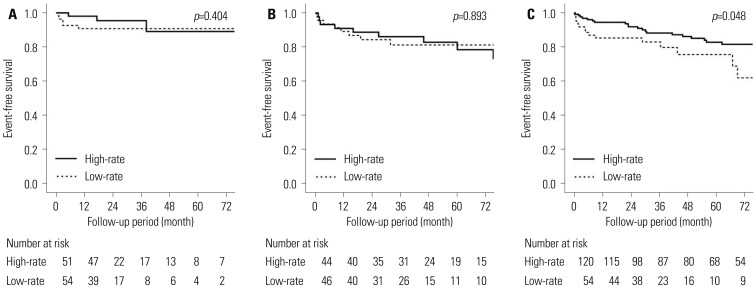
Among patients in group 1, 56 patients (47.5%) had a high-rate ICD therapy zone. Hypertension was significantly more frequent among patients with a high-rate ICD therapy zone than a low-rate ICD therapy zone. Patients with a high-rate ICD therapy zone experienced appropriate ICD therapy significantly less frequently than patients with a low-rate ICD therapy zone, when assessed annually (3.7% and 10.6%, respectively, p=0.026) (Fig. 2A). There were no significant differences in annual numbers of patients who experienced inappropriate ICD therapy between patients with a high- or low-rate ICD therapy zone (1.9% and 5.7%, respectively, p=0.404) (Fig. 3A). There were also no significant differences in annual mortality between the patients with a high- or low-rate ICD therapy zone (5.0% and 4.0%, respectively, p=0.487).
Fig. 2. Appropriate implantable cardioverter-defibrillator (ICD) therapy according to ICD therapy zones (high-rate ICD therapy zone vs. low-rate ICD therapy zone) in group 1 (A), 2 (B), and 3 (C). Group 1, heart failure (HF) and ICD for primary prevention; group 2, HF and ICD for secondary prevention; group 3, non-HF and ICD.
Fig. 3. Inappropriate implantable cardioverter-defibrillator (ICD) therapy according to ICD therapy zones (high-rate ICD therapy zone vs. low-rate ICD therapy zone) in group 1 (A), 2 (B), and 3 (C). Group 1, heart failure (HF) and ICD for primary prevention; group 2, HF and ICD for secondary prevention; group 3, non-HF and ICD.
Among patients in group 2, 45 patients (48.4%) had a high-rate ICD therapy zone. There was no significant difference in the baseline characteristics between patients of a high- and low-rate ICD therapy zone. There were no significant differences in the annual numbers of patients who experienced appropriate ICD therapy between the patients with a high- or low-rate ICD therapy zone (9.3% and 11.5%, respectively, p=0.277) (Fig. 2B). There were no significant differences in the annual numbers of patients who experienced inappropriate ICD therapy between the patients with a high- or low-rate ICD therapy zone (4.3% and 4.1%, respectively, p=0.893) (Fig. 3B).
Among patients in group 3, 129 patients (66.5%) had a high-rate ICD therapy zone. Dual-chamber ICD was significantly more frequent in patients of a low-rate ICD therapy zone than a high-rate ICD therapy zone. Patients with a high-rate ICD therapy zone experienced inappropriate ICD therapy significantly less frequently than patients with a low-rate ICD therapy zone, when assessed annually (2.7% and 5.7%, respectively, p=0.048) (Fig. 3C). There were no significant differences in the annual numbers of patients who experienced appropriate ICD therapy between the patients with a high- or low-rate ICD therapy zone (5.5% and 8.8%, respectively, p=0.200) (Fig. 2C). There were also no significant differences in annual mortality between patients with a high- or low-rate ICD therapy zone (0.3% and 0.4%, respectively, p=0.227).
DISCUSSION
This was a cohort study using real-world ICD registry data. The main findings of the present study are that 1) the annual proportions of the patients in groups 1, 2, and 3 who experienced appropriate ICD therapy were 6.1, 10.4, and 5.9%, respectively; 2) for patients in group 1, the annual appropriate ICD therapy rate was significantly lower in patients with a high-rate ICD therapy zone than in patients with a low-rate ICD therapy zone; and 3) for patients in group 3, the annual inappropriate ICD therapy rate was significantly lower in patients with a high-rate ICD therapy zone than in patients with a low-rate ICD therapy zone.
Previous prospective randomized trials and real-world registry data on ICDs for primary prevention of sudden cardiac death
Many previous large-scale prospective randomized trials have shown that survival benefits can be obtained by ICD use in patients with HF and a reduced ejection fraction. In the previous studies evaluating the use of ICDs for primary prevention of sudden cardiac death, the following annual appropriate ICD therapy rates have been reported and are presented in the order of publication date: 17% in the MADIT-II trial,16 7.4% in the DEFINITE trial,8 5.1% in the SCD-HeFT trial,9 5.4% in the PREPARE study,17 and 5.2% in the MADIT-RIT trial.11 The annual inappropriate ICD therapy rates were as follows: 8.9% in the DEFINITE trial,8 2.4% in the SCD-HeFT trial,9 3.1% in the PREPARE study,17 and 3.4% in the MADIT-RIT trial.11 Previous real-world registry data have included appropriate and inappropriate ICD therapy rates in patients with ICD for primary prevention. Swedish registry data indicated annual appropriate and inappropriate ICD therapy rates of 6.0% and 2.4% in 865 patients with an ICD for primary prevention, respectively.18 Israeli registry data revealed that annual appropriate ICD therapy rates were 3.9% and 8.4% and that annual inappropriate ICD therapy rates were 2.0% and 1.8% in 1766 and 583 patients with an ICD for primary or secondary prevention, respectively.19 Appropriate and inappropriate ICD therapy rates tend to decrease over time. This may be because unnecessary ICD therapy can be avoided using a high-rate ICD therapy zone and delayed detection time. There is a paucity of real-world ICD registry data for Asian patients with HF. According to Japanese registry data on patients with chronic HF, fatal arrhythmic events occurred in 16.1% and 8.9% of patients who met class I and IIa indications for ICD implantation, respectively.20 A retrospective study on Korean patients with HF reported a sudden cardiac death rate of 8% during 40 months of follow-up in patients who met the ICD indications for primary prevention.21 In the present study, the annual appropriate and inappropriate ICD therapy rates in patients with HF using an ICD for primary prevention are comparable with those of the recent prospective randomized trials and real-world registry data.
High- and low-rate ICD therapy zones
In patients with HF and ICD for primary prevention, high appropriate and inappropriate ICD shock rates have been associated with a high risk of mortality.22 The PainFREE Rx II trial showed that anti-tachycardial pacing was effective for reducing appropriate ICD shock for fast ventricular tachycardia.23 The MADIT-RIT and ADVANCE III trials showed that a high-rate ICD therapy zone and long-detection interval could reduce in-appropriate and unnecessary ICD shocks.11,24 In the present study, a high-rate ICD therapy zone was associated with a low appropriate ICD therapy rate in patients with HF and ICD for primary prevention. However, a high-rate ICD therapy zone was not associated with inappropriate ICD therapy rate or mortality in these patients. Although we could not completely differentiate necessary ICD therapy from unnecessary ICD therapy in appropriate ICD therapy, the present results suggest that a high-rate ICD therapy zone could reduce unnecessary ICD therapy in patients with HF and ICD for primary prevention. In our analysis, it was difficult to say whether the ventricular tachyarrhythmia treated by ICD therapy would have been fatal without ICD.
In the present study, a high-rate ICD therapy zone was associated with a low inappropriate ICD therapy rate in the non-HF patients. Since the patients in group 3 were younger than the patients with groups 1 and 2, they could have higher physical activity. Therefore, there may be a high probability of inappropriate ICD therapy for sinus tachycardia in non-HF patients. In this study, the most common cause of inappropriate ICD therapy was also sinus tachycardia in group 3. The present results suggest that a high-rate ICD therapy zone might reduce inappropriate ICD therapy for sinus tachycardia in non-HF patients with ICD.
It is not clear why a high-rate ICD therapy zone did not reduce ICD therapy delivery in the patients in groups 2. We speculate that unnecessary ICD therapies for non-sustained ventricular tachyarrhythmia did not occur frequently in patients with HF and ICD for secondary prevention.
Inappropriate ICD therapy
The common causes of inappropriate ICD shock are atrial fibrillation, supraventricular tachycardia, and abnormal sensing in patients with prior myocardial infarction who are using an ICD for primary prevention.25 In Korean patients, atrial fibrillation is a predictor of inappropriate shock.26 In the present study, the most common cause of inappropriate ICD therapy in patients with HF was atrial fibrillation. However, in non-HF patients, the most common cause of inappropriate ICD therapy was sinus tachycardia. Age and underlying heart disease could contribute to the difference in the main causes of inappropriate ICD therapy. Higher incidence of atrial fibrillation occurred in patients with HF due to older age and reduced ejection fraction. In contrast, high physical activity levels and high incidence of sinus tachycardia were more likely in non-HF patients as they were younger and had a preserved ejection fraction. Due to high numbers of oversensing issues, management of ICD hardware and meticulous ICD programming are necessary to reduce inappropriate ICD therapy.
Study limitations
This was a cohort study based on real-world registry data rather than a prospective randomized trial. It was difficult to differentiate between necessary and unnecessary ICD therapy in the patients who experienced appropriate ICD therapy. Additionally, data about the arrhythmia detection interval of the ICDs were not available in all patients. Large-scale prospective randomized trials in Asian patients are necessary.
In conclusion, appropriate ICD therapy rates are not low in Korean patients with ICD, relative to prior large-scale studies in Western countries. Appropriate and inappropriate ICD therapy could be reduced by a high-rate therapy zone in patients with HF and ICD for primary prevention and non-HF patients, respectively.
ACKNOWLEDGEMENTS
This study was supported by a CMB-Yuhan research grant from Yonsei University College of Medicine (6-2015-0173), research-grants from the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministryof Education, Science and Technology (NRF-2012R1A2A2 A02045367, 2010-0021993), and from the Korean Healthcare technology R&D project funded by the Ministry of Health & Welfare (HI12C1552, HI16C0058, HI15C1200).
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Wever EF, Hauer RN, van Capelle FL, Tijssen JG, Crijns HJ, Algra A, et al. Randomized study of implantable defibrillator as first-choice therapy versus conventional strategy in postinfarct sudden death survivors. Circulation. 1995;91:2195–2203. doi: 10.1161/01.cir.91.8.2195. [DOI] [PubMed] [Google Scholar]
- 2.A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. The antiarrhythmics versus implantable defibrillators (AVID) investigators. N Engl J Med. 1997;337:1576–1583. doi: 10.1056/NEJM199711273372202. [DOI] [PubMed] [Google Scholar]
- 3.Connolly SJ, Gent M, Roberts RS, Dorian P, Roy D, Sheldon RS, et al. Canadian implantable defibrillator study (CIDS): a randomized trial of the implantable cardioverter defibrillator against amiodarone. Circulation. 2000;101:1297–1302. doi: 10.1161/01.cir.101.11.1297. [DOI] [PubMed] [Google Scholar]
- 4.Kuck KH, Cappato R, Siebels J, Rüppel R. Randomized comparison of antiarrhythmic drug therapy with implantable defibrillators in patients resuscitated from cardiac arrest: the Cardiac Arrest Study Hamburg (CASH) Circulation. 2000;102:748–754. doi: 10.1161/01.cir.102.7.748. [DOI] [PubMed] [Google Scholar]
- 5.Moss AJ, Hall WJ, Cannom DS, Daubert JP, Higgins SL, Klein H, et al. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. Multicenter automatic defibrillator implantation trial investigators. N Engl J Med. 1996;335:1933–1940. doi: 10.1056/NEJM199612263352601. [DOI] [PubMed] [Google Scholar]
- 6.Buxton AE, Lee KL, Fisher JD, Josephson ME, Prystowsky EN, Hafley G. A randomized study of the prevention of sudden death in patients with coronary artery disease. Multicenter unsustained tachycardia trial investigators. N Engl J Med. 1999;341:1882–1890. doi: 10.1056/NEJM199912163412503. [DOI] [PubMed] [Google Scholar]
- 7.Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002;346:877–883. doi: 10.1056/NEJMoa013474. [DOI] [PubMed] [Google Scholar]
- 8.Kadish A, Dyer A, Daubert JP, Quigg R, Estes NA, Anderson KP, et al. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med. 2004;350:2151–2158. doi: 10.1056/NEJMoa033088. [DOI] [PubMed] [Google Scholar]
- 9.Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225–237. doi: 10.1056/NEJMoa043399. [DOI] [PubMed] [Google Scholar]
- 10.WRITING COMMITTEE MEMBERS. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:e240–e327. doi: 10.1161/CIR.0b013e31829e8776. [DOI] [PubMed] [Google Scholar]
- 11.Moss AJ, Schuger C, Beck CA, Brown MW, Cannom DS, Daubert JP, et al. Reduction in inappropriate therapy and mortality through ICD programming. N Engl J Med. 2012;367:2275–2283. doi: 10.1056/NEJMoa1211107. [DOI] [PubMed] [Google Scholar]
- 12.Kirkfeldt RE, Johansen JB, Nohr EA, Jørgensen OD, Nielsen JC. Complications after cardiac implantable electronic device implantations: an analysis of a complete, nationwide cohort in Denmark. Eur Heart J. 2014;35:1186–1194. doi: 10.1093/eurheartj/eht511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gregoratos G, Abrams J, Epstein AE, Freedman RA, Hayes DL, Hlatky MA, et al. ACC/AHA/NASPE 2002 guideline update for implantation of cardiac pacemakers and antiarrhythmia devices: summary article: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (ACC/AHA/NASPE committee to update the 1998 pacemaker guidelines) Circulation. 2002;106:2145–2161. doi: 10.1161/01.cir.0000035996.46455.09. [DOI] [PubMed] [Google Scholar]
- 14.Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA, 3rd, Freedman RA, Gettes LS, et al. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (writing committee to revise the ACC/AHA/NASPE 2002 guideline update for implantation of cardiac pacemakers and antiarrhythmia devices): developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. Circulation. 2008;117:e350–e408. doi: 10.1161/CIRCUALTIONAHA.108.189742. [DOI] [PubMed] [Google Scholar]
- 15.Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA, 3rd, Freedman RA, Gettes LS, et al. 2012 ACCF/AHA/HRS focused update incorporated into the ACCF/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines and the Heart Rhythm Society. Circulation. 2013;127:e283–e352. doi: 10.1161/CIR.0b013e318276ce9b. [DOI] [PubMed] [Google Scholar]
- 16.Moss AJ, Greenberg H, Case RB, Zareba W, Hall WJ, Brown MW, et al. Long-term clinical course of patients after termination of ventricular tachyarrhythmia by an implanted defibrillator. Circulation. 2004;110:3760–3765. doi: 10.1161/01.CIR.0000150390.04704.B7. [DOI] [PubMed] [Google Scholar]
- 17.Wilkoff BL, Williamson BD, Stern RS, Moore SL, Lu F, Lee SW, et al. Strategic programming of detection and therapy parameters in implantable cardioverter-defibrillators reduces shocks in primary prevention patients: results from the PREPARE (primary prevention parameters evaluation) study. J Am Coll Cardiol. 2008;52:541–550. doi: 10.1016/j.jacc.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 18.Sjöblom J, Kalm T, Gadler F, Ljung L, Frykman V, Rosenqvist M, et al. Efficacy of primary preventive ICD therapy in an unselected population of patients with reduced left ventricular ejection fraction. Europace. 2015;17:255–261. doi: 10.1093/europace/euu219. [DOI] [PubMed] [Google Scholar]
- 19.Sabbag A, Suleiman M, Laish-Farkash A, Samania N, Kazatsker M, Goldenberg I, et al. Contemporary rates of appropriate shock therapy in patients who receive implantable device therapy in a real-world setting: from the Israeli ICD registry. Heart Rhythm. 2015;12:2426–2433. doi: 10.1016/j.hrthm.2015.08.020. [DOI] [PubMed] [Google Scholar]
- 20.Satake H, Fukuda K, Sakata Y, Miyata S, Nakano M, Kondo M, et al. Current status of primary prevention of sudden cardiac death with implantable cardioverter defibrillator in patients with chronic heart failure--a report from the CHART-2 study. Circ J. 2015;79:381–390. doi: 10.1253/circj.CJ-14-0925. [DOI] [PubMed] [Google Scholar]
- 21.Kim J, Choi EK, Lee MH, Kang DY, Sung YJ, Lee DW, et al. The relevance of the primary prevention criteria for implantable cardioverter defibrillator implantation in Korean symptomatic severe heart failure patients. Korean Circ J. 2012;42:173–183. doi: 10.4070/kcj.2012.42.3.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Poole JE, Johnson GW, Hellkamp AS, Anderson J, Callans DJ, Raitt MH, et al. Prognostic importance of defibrillator shocks in patients with heart failure. N Engl J Med. 2008;359:1009–1017. doi: 10.1056/NEJMoa071098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wathen MS, DeGroot PJ, Sweeney MO, Stark AJ, Otterness MF, Adkisson WO, et al. Prospective randomized multicenter trial of empirical antitachycardia pacing versus shocks for spontaneous rapid ventricular tachycardia in patients with implantable cardioverter-defibrillators: pacing fast ventricular tachycardia reduces shock therapies (PainFREE Rx II) trial results. Circulation. 2004;110:2591–2596. doi: 10.1161/01.CIR.0000145610.64014.E4. [DOI] [PubMed] [Google Scholar]
- 24.Gasparini M, Proclemer A, Klersy C, Kloppe A, Lunati M, Ferrer JB, et al. Effect of long-detection interval vs standard-detection interval for implantable cardioverter-defibrillators on antitachycardia pacing and shock delivery: the ADVANCE III randomized clinical trial. JAMA. 2013;309:1903–1911. doi: 10.1001/jama.2013.4598. [DOI] [PubMed] [Google Scholar]
- 25.Daubert JP, Zareba W, Cannom DS, McNitt S, Rosero SZ, Wang P, et al. Inappropriate implantable cardioverter-defibrillator shocks in MADIT II: frequency, mechanisms, predictors, and survival impact. J Am Coll Cardiol. 2008;51:1357–1365. doi: 10.1016/j.jacc.2007.09.073. [DOI] [PubMed] [Google Scholar]
- 26.Yang JH, Byeon K, Yim HR, Park JW, Park SJ, Huh J, et al. Predictors and clinical impact of inappropriate implantable cardioverter-defibrillator shocks in Korean patients. J Korean Med Sci. 2012;27:619–624. doi: 10.3346/jkms.2012.27.6.619. [DOI] [PMC free article] [PubMed] [Google Scholar]