Abstract
A technique for anatomic reconstruction of the anterolateral complex addressing anterolateral rotatory instability both in primary anterior cruciate ligament reconstruction and in revision cases is presented. The extra-articular reconstruction is performed with a pedicle strip of iliotibial tract, fixed on the anatomic origin and insertion points of the anterolateral ligament of the knee in a double-bundle V-shaped fashion.
Anterolateral rotatory instability of the knee is a combination of anterior translation and internal rotation of the tibia as a result of combined injury of the anterior cruciate ligament (ACL) and secondary restraints that clinically presents with a positive pivot shift. Persistent rotational instability is related to poor functional outcomes and patient dissatisfaction after ACL reconstruction.1 Modern anatomic ACL reconstruction techniques still are unable to completely restore normal knee joint biomechanics and rotatory stability in most cases.2, 3 Recent studies have shown that such rotational instability is correlated to injuries of the anterolateral complex (anterolateral ligament [ALL] and capsule, lateral meniscus, iliotibial tract [ITT]), in addition to ACL tears.4 Despite extra-articular reconstructions having been used to control the pivot-shift phenomenon, recent reports on the anatomy of the ALL5 have shifted attention to more anatomic reconstruction, respecting the origin and insertion points of this structure. Therefore, the aim of this study was to present a technique for anatomic ALL reconstruction using a strip of ITT (Video 1).
Technique
Access Route for ALL Reconstruction
With the knee at 90° of flexion, a 4- to 5-cm-long hockey-stick incision6 is performed on the lateral aspect of the knee from the lateral femoral condyle to the Gerdy tubercle. The peroneal nerve is located distal to the surgical field and is not in danger during the procedure. After dissection of the skin and subcutaneous tissue, the ITT is visualized.
Graft Harvesting
The central portion of the ITT is identified, and a strip of ITT is harvested in line with its fibers in a distal-to-proximal direction (Fig 1). A graft measuring 0.5 cm wide and at least 14 cm long is gently dissected, leaving its distal insertion on the Gerdy tubercle (Fig 2).
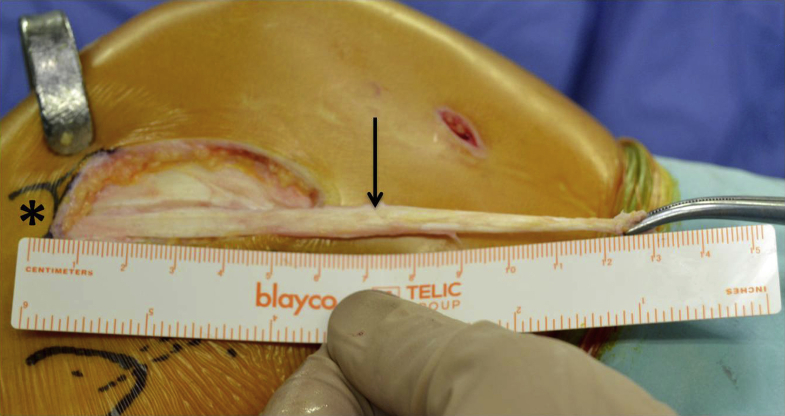
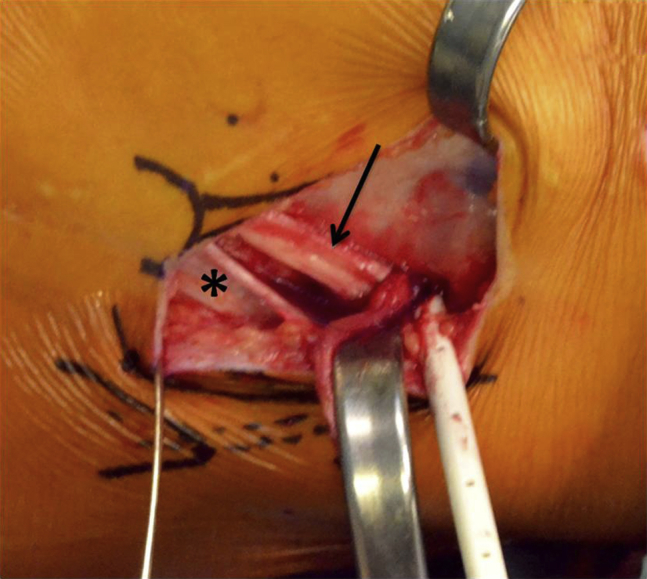
Fig 1.
After identification of the central portion of the iliotibial tract (arrow), a strip is harvested in line with its fibers in a distal-to-proximal direction. A left knee is shown.
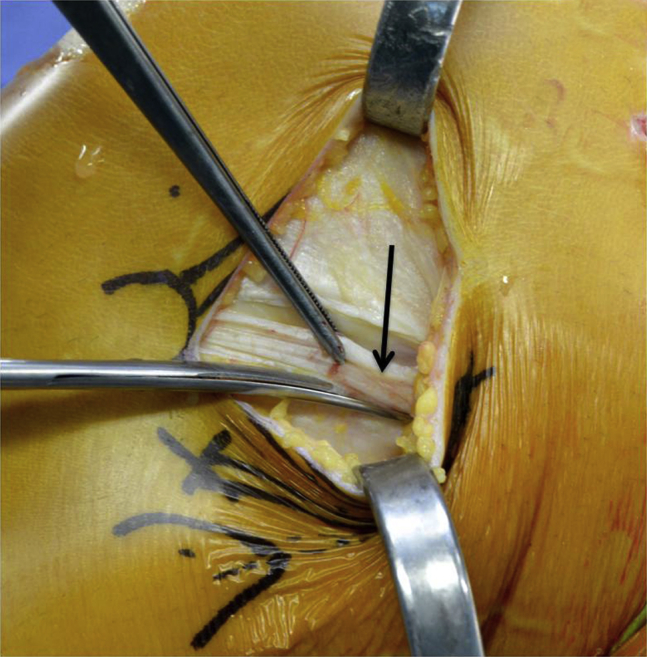
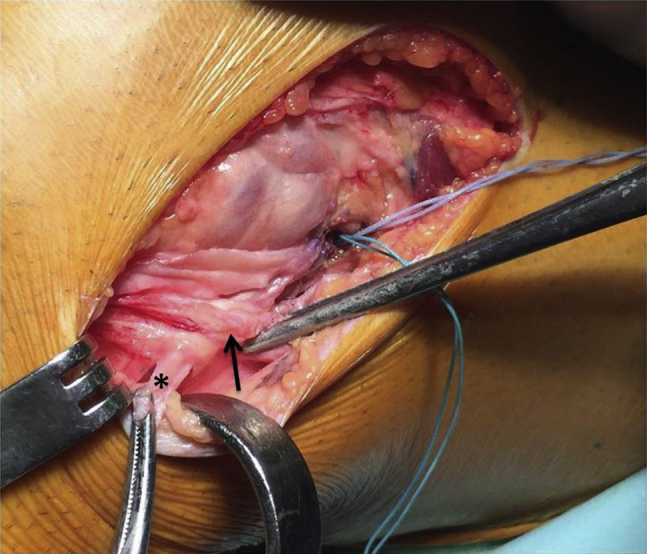
Fig 2.
An iliotibial tract graft (arrow) measuring approximately 0.5 cm wide and 14 cm long is gently dissected, leaving its distal insertion on the Gerdy tubercle (asterisk). A left knee is shown.
ALL Reconstruction
After identification of the lateral collateral ligament and popliteus tendon, the femoral anatomic insertion of the ALL is identified.5, 7, 8, 9, 10 The point is located just proximal and posterior to the lateral femoral epicondyle, where a 2.4-mm K-wire is inserted; any possible interference with the femoral ACL tunnel should be carefully avoided. The distance between the Gerdy tubercle and the K-wire is calculated, usually corresponding to approximately 4 cm. A second 2.4-mm K-wire is placed at the anatomic tibial insertion of the ALL, midway between the Gerdy tubercle and fibular head. The point is routinely located approximately 22 mm from the center of the Gerdy tubercle and 11 mm below the joint line.5, 7, 8 The distance between the 2 K-wires is calculated as well. This distance corresponds to the bundle that will anatomically replace the ALL. A suture is looped over the 2 K-wires, and tension is checked during range of motion between 0° and 90° of flexion, with the aim being to obtain a bundle, reproducing the ALL, that is tight in extension and slack in flexion (Fig 3). In case of improper tension, the K-wires are repositioned. With the knee in full extension, the graft is marked at the level of the femoral K-wire starting from the Gerdy tubercle, corresponding to the first bundle of the reconstruction. Then, a second mark is made 3 cm proximally to the first mark, and a third mark is made at the middle point between the first 2 marks. A No. 2 suture wire is looped at the level of the third mark, and the graft is doubled and whipstitched with No. 2 suture wire using a crisscrossing stitch for a length of 1.5 cm (Fig 4). This will leave about 4 cm for the first bundle (from the femoral insertion to the Gerdy tubercle) and a loop of 1.5 cm to be filled in the femoral socket. Finally, the free end of the graft is whipstitched using a crisscrossing stitch for a length of 1.5 cm. Socket drilling is performed on both sides under the ITT, with a diameter of 6 mm and depth of 20 mm on the femoral side and a diameter of 4.5 mm and depth of 20 mm on the tibial side. Moreover, careful soft-tissue clearance at the entrance of both sockets is achieved to ensure easy subsequent graft and anchor passage. The suture wire at the level of the loop is passed through the eyelet of a 6.5-mm knotless anchor (SwiveLock; Arthrex) (Fig 4) and then fixed on the femoral side with the knee in full extension and neutral rotation (Fig 5). The whipstitched wire of the free end of the graft is passed through the eyelet of a 4.75-mm-diameter knotless anchor (SwiveLock) and fixed on the tibial side under the ITT (Fig 6), always with the knee in full extension and neutral rotation (Fig 7).
Fig 3.
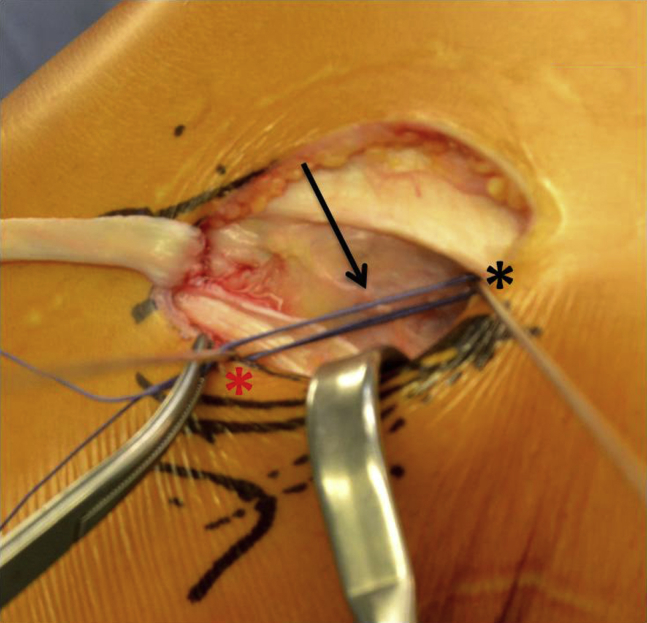
A suture is looped over the 2 K-wires, and tension is checked during range of motion between 0° and 90° of flexion, the aim being to obtain a bundle, reproducing the anterolateral ligament, that is tight in extension and slack in flexion. A left knee is shown. The arrow indicates the suture wire, the black asterisk indicates the K-wire on the femoral insertion point, and the red asterisk indicates the K-wire on the tibial insertion point.
Fig 4.
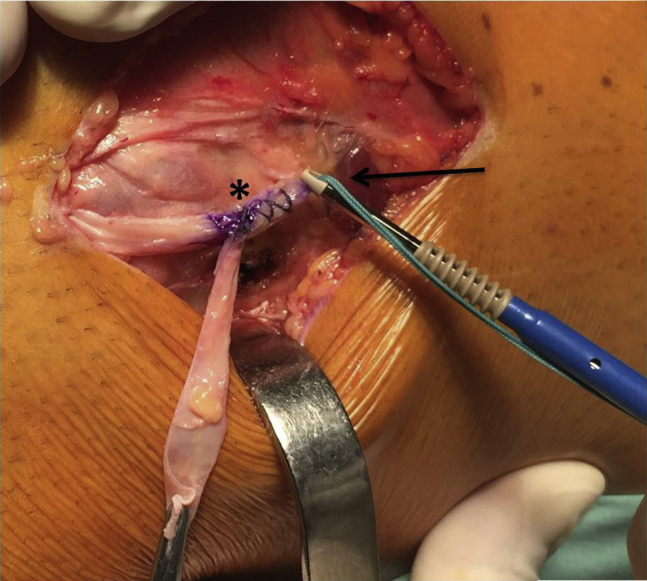
A No. 2 suture wire is looped at the level of the third mark, and the graft is doubled and whipstitched with No. 2 suture wire using a crisscrossing stitch for a length of 1.5 cm. The suture wire at the level of the loop is passed through the eyelet of a 6.5-mm knotless anchor (SwiveLock). A left knee is shown. The arrow indicates the suture wire looped on the graft passed through the anchor eyelet, and the asterisk indicates the graft whipstitched with a crisscrossing suture.
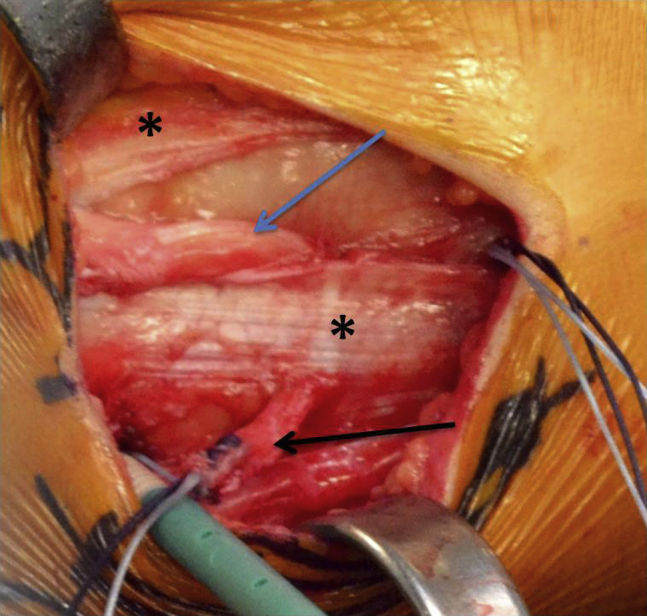
Fig 5.
Fixation of the first bundle (arrow) of the graft on the femoral side with the knee in full extension and neutral rotation. A left knee is shown. The asterisk indicates the iliotibial tract.
Fig 6.
After fixation of the first bundle on the femoral side with the knee in full extension and neutral rotation, the second bundle (asterisk) is passed under the iliotibial tract (arrow). A left knee is shown.
Fig 7.
Tibial fixation of the graft is performed, always with the knee in full extension and neutral rotation. A left knee is shown. The asterisks indicate the iliotibial tract, the blue arrow indicates the first bundle, and the black arrow indicates the second bundle.
The final construct consists of 2 bundles: the first, starting from the Gerdy tubercle to the femoral insertion of the ALL, being an anterolateral capsule reinforcement and the second, fixed on the anatomic insertion points of the ALL, corresponding to the reconstructed ALL (Fig 8). Both bundles are tight in extension and slack in flexion, becoming tight at 30° of knee flexion and internal rotation. Finally, the ITT is sutured with simple stitches before wound closure (Table 1).
Fig 8.
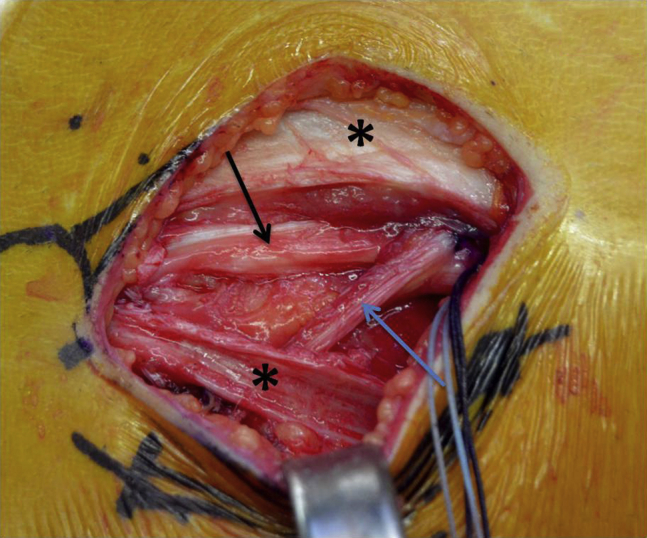
Final view shown in a left knee. The first bundle (black arrow), starting from the Gerdy tubercle to the femoral insertion of the anterolateral ligament (ALL), is an anterolateral capsule reinforcement; the second bundle (blue arrow), fixed on the anatomic insertion points of the ALL, corresponds to the reconstructed ALL. The asterisks indicate the iliotibial tract.
Table 1.
Advantage, Indications, Step-by-Step Technique, Risks, and Tips and Tricks
| Advantage |
| The described technique provides a double-bundle reconstruction of the ALL and capsule. |
| Indications |
| High-grade preoperative pivot shift |
| High-risk sport activity (pivoting) |
| Revision |
| Step-by-step technique |
| Mark the epicondylus, Gerdy tubercle, fibular head, tibial plateau, and posterior aspect of the muscular interseptum. |
| Mark the anatomic insertion on the tibia and femur. |
| Perform an incision from the epicondylus to midway between the Gerdy tubercle and fibular head. |
| Perform an incision of the fascia lata along its fibers from the Gerdy tubercle in a proximal direction. |
| Obtain a graft that is at least 14 cm in length and 5 mm in width. |
| Place a 2.4-mm K-wire at the anatomic insertion of the ALL on the femur and tibia. |
| Check tension with suture—the goal is a graft that is tight in extension and slack in flexion. |
| Mark the graft just distal to the femoral wire. |
| Mark the graft 30 mm proximal to the first mark. |
| Determine and mark the middle between first 2 marks. |
| Loop the graft at this level with a suture wire. |
| Whipstitch for a length of 15 mm. |
| Use a drill sleeve. |
| Drill the femoral hole (6 mm in diameter and 20 mm in depth) with regular flute length, avoiding confluence with the femoral tunnel for the ACL, when performed with an AM portal or outside-in technique—this can be obtained under arthroscopic visualization before ACL graft fixation and/or drilling the 2 femoral tunnels parallel. |
| Accurately clean the margin of the femoral hole. |
| Pass the suture wire at the level of the loop through the eyelet of a 6.5-mm SwiveLock tenodesis anchor. |
| In full extension, fix the graft on the femoral side. |
| Make a small incision close to the tibial K-wire into the ITT to shuttle the second strand of the graft between the capsule and the posterior and distal part of the ITT. |
| In extension, mark the graft at the proximal level of the K-wire. |
| Mark the graft 15 mm distal to the first mark. |
| Whipstitch for the length of 15 mm beginning at the first mark. |
| Use a drill sleeve. |
| Drill the femoral hole 4.5 mm in diameter and 20 mm in depth with regular flute length. |
| Accurately clean the margin of the tibial hole. |
| Pass the suture wire of the free end of the graft through the eyelet of a 4.75-mm-diameter knotless anchor (SwiveLock). |
| In full extension, fix the graft on the tibial side. |
| Risks |
| Anchor protrusion |
| ALL femoral socket and ACL femoral tunnel confluence |
| Excessive constraint of tibial internal rotation |
| Lateral geniculate artery bleeding while harvesting fascia lata strip |
| Tips and tricks |
| Fix the graft with the knee in full extension and neutral rotation: This will result in a graft that is tight in extension and slack in flexion, becoming tight at knee flexion and internal rotation. |
| Carefully evaluate the femoral insertion point, checking isometry before fixation. We suggest a point that is proximal and posterior to the epicondyle to obtain a graft that is tight in extension and slack in flexion. |
| After femoral fixation, note that the residual FiberWire (Arthrex) of the SwiveLock tenodesis anchor can be used for additional fixation of the graft. |
| Fix the graft under the fascia lata to allow ITT suture and closure over the graft. |
ACL, anterior cruciate ligament; ALL, anterolateral ligament; AM, anteromedial; ITT, iliotibial tract.
Discussion
ACL tears are one of the most common injuries of the knee.11 Despite good clinical results of ACL reconstruction techniques having been reported by many authors, concerns remain about the ability to fully restore rotational stability of the knee and control the pivot-shift phenomenon.3 The role of secondary restraints of the lateral aspect of the knee has been clearly shown in the past, so several lateral extra-articular procedures have been proposed.12, 13, 14 However, their indications are still controversial in the literature.3, 15, 16, 17 Recently, the ALL has been described as a distinct structure extending proximally and posteriorly to the lateral epicondyle to a point midway between the Gerdy tubercle and fibular head.7 Therefore, techniques have shifted from nonanatomic procedures to procedures attempting to reproduce the anatomy, and techniques for anatomic ALL reconstruction have been proposed using soft-tissue grafts such as gracilis tendon and fascia lata.18, 19, 20, 21 However, because the ALL is a part of a more complex ligamentous structure (anterolateral complex) involving the whole lateral capsule extending from anterior to posterior, acting along with the ACL in controlling the pivot-shift phenomenon, often injured in the case of acute ACL tears,22 an anterolateral capsule reinforcement in addition to anatomic ALL reconstruction could be useful with the goal to control rotatory loads.
The aim of this report is to present a technique for a double-bundle anatomic reconstruction of the anterolateral complex using a strip of ITT. The first bundle reinforces the anterolateral capsule, and the second bundle corresponds to the course of the native ALL. Indications for the proposed technique are higher grades of the pivot-shift test, high-risk athletes, and revision surgery. A strip of ITT has been widely used in the past for extra-articular nonanatomic tenodesis,12, 13, 14 with good results at long-term follow-up.15, 23, 24, 25 Moreover, the biomechanical effect of such procedures in controlling rotational stability of the knee has also been shown with the aid of navigation.6, 17 However, all these techniques, acting with nonanatomic behavior, took advantage from the long lever arm not reproducing the anatomy of the lateral aspect of the knee. For this reason, concern about possible overconstraint of the lateral aspect of the knee still exists.26, 27 Given that, historically, ACL reconstructions have moved from nonanatomic procedures to techniques trying to maximize the replication of ACL anatomy, it is our belief that recent knowledge of the anatomy and function of the anterolateral complex emphasizes the development of extra-articular procedures that more anatomically replicate the complex anatomy of the lateral aspect of the knee, with the aim to control rotational stability, avoiding any possible overconstraint.
However, there is a lack of literature addressing the real advantage of anatomic ALL reconstruction. To our knowledge, there is only one article reporting the results of an anatomic ALL reconstruction at 2 years of follow-up, with excellent results in terms of rotational stability, failure rate, and complications.18
The proposed technique has some disadvantages. First, because a minimum graft size of 14 cm in length is needed to perform such a technique, at this time, an additional incision to approach the lateral compartment is performed. The future direction is to develop a harvesting device to perform the technique in a minimally invasive fashion. However, the second incision allows the surgeon to properly place the graft, properly tension the graft, and fix it easily under the ITT. Second, because the ITT is another important secondary restraint of the knee, the use of a strip of ITT could weaken such a structure.26, 27 Nevertheless, strips of ITT have been widely used for extra-articular tenodesis in the past,12, 13, 14 with no relation in long-term follow-up results15, 23, 24, 25 in terms of osteoarthritis. Moreover, the reconstruction is performed under the ITT, which can be sutured at the end of the procedure. Concerning fixation, the use of bone sockets on both the femoral side and tibial side with anchors acting as interference screws seems to be adequate for biological and mechanical fixation, even if care must be taken to avoid confluence with the ACL tunnel on the femoral side.
This study has some limitations. First, no biomechanical tests were performed to compare the described technique with other ALL reconstruction techniques or lateral extra-articular tenodesis. However, considering the biomechanical properties of the anterolateral complex of the knee,26, 27 the use of a strip of ITT fixed with anchors in bone sockets seems to be biomechanically adequate. Another limitation is that no clinical and radiologic results are reported. However, because we have only recently started to perform the proposed technique, we have no sufficient cases with an adequate minimum follow-up period. In conclusion, the proposed technique in our current practice has replaced the old nonanatomic lateral tenodesis (Coker-Arnold modification of the MacIntosh technique) with the same indications: severe knee instabilities with pivot shift graded 3+, high-risk or high-level athletes, and revision surgery.
Footnotes
The authors report the following potential conflict of interest or source of funding: A.F. receives support from Arthrex. E.M. receives support from Arthrex. A.D.C. receives support from Arthrex.
Supplementary Data
Anatomic reconstruction of the anterolateral complex addressing anterolateral rotatory instability both in primary anterior cruciate ligament reconstruction and in revision cases is presented. A left knee is shown. The reconstruction is performed with a pedicle strip of iliotibial tract, fixed on the anatomic origin and insertion points of the anterolateral ligament of the knee in a double-bundle V-shaped fashion.
References
- 1.Musahl V., Hoshino Y., Becker R., Karlsson J. Rotatory knee laxity and the pivot shift. Knee Surg Sports Traumatol Arthrosc. 2012;20:601–602. doi: 10.1007/s00167-011-1844-y. [DOI] [PubMed] [Google Scholar]
- 2.Eriksson E. How good are the results of ACL reconstruction? Knee Surg Sports Traumatol Arthrosc. 1997;5:137. doi: 10.1007/s001670050040. [DOI] [PubMed] [Google Scholar]
- 3.Ferretti A., Monaco E., Vadalà A. Rotatory instability of the knee after ACL tear and reconstruction. J Orthop Traumatol. 2014;15:75–79. doi: 10.1007/s10195-013-0254-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tanaka M., Vyas D., Moloney G., Bedi A., Pearle A.D., Musahl V. What does it take to have a high-grade pivot shift? Knee Surg Sports Traumatol Arthrosc. 2012;20:737–742. doi: 10.1007/s00167-011-1866-5. [DOI] [PubMed] [Google Scholar]
- 5.Monaco E., Ferretti A., Labianca L. Navigated knee kinematics after cutting of the ACL and its secondary restraint. Knee Surg Sports Traumatol Arthrosc. 2012;20:870–877. doi: 10.1007/s00167-011-1640-8. [DOI] [PubMed] [Google Scholar]
- 6.Monaco E., Labianca L., Conteduca F., De Carli A., Ferretti A. Double bundle or single bundle plus extraarticular tenodesis in ACL reconstruction? A CAOS study. Knee Surg Sports Traumatol Arthrosc. 2007;15:1168–1174. doi: 10.1007/s00167-007-0368-y. [DOI] [PubMed] [Google Scholar]
- 7.Claes S., Vereecke E., Maes M., Victor J., Verdonk P., Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223:321–328. doi: 10.1111/joa.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hughston J.C. A surgical approach to the medial and posterior ligaments of the knee. Clin Orthop Relat Res. 1973;(91):29–33. doi: 10.1097/00003086-197303000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Helito C.P., Demange M.K., Bonadio M.B. Radiographic landmarks for locating the femoral origin and tibial insertion of the knee anterolateral ligament. Am J Sports Med. 2014;42:2356–2362. doi: 10.1177/0363546514543770. [DOI] [PubMed] [Google Scholar]
- 10.Daggett M., Ockuly A.C., Cullen M. Femoral origin of the anterolateral ligament: An anatomic analysis. Arthroscopy. 2016;32:835–841. doi: 10.1016/j.arthro.2015.10.006. [DOI] [PubMed] [Google Scholar]
- 11.Frank R.M., Verma N.N. Graft selection in revision ACL reconstruction. In: Bach B.R. Jr., Provencher M.T., editors. ACL surgery: How to get it right the first time and what to do if it fails. SLACK; Thorofare, NJ: 2010. pp. 217–229. [Google Scholar]
- 12.Lemaire M., Combelles F. Plastic repair with fascia lata for old tears of the anterior cruciate ligament (author's transl) Rev Chir Orthop Reparatrice Appar Mot. 1980;66:523–525. [in French] [PubMed] [Google Scholar]
- 13.Losee R.E., Johnson T.R., Southwick W.O. Anterior subluxation of the lateral tibial plateau. A diagnostic test and operative repair. J Bone Joint Surg Am. 1978;60:1015–1030. [PubMed] [Google Scholar]
- 14.Ireland J., Trickey E.L. Macintosh tenodesis for anterolateral instability of the knee. J Bone Joint Surg Br. 1980;62:340–345. doi: 10.1302/0301-620X.62B3.7410466. [DOI] [PubMed] [Google Scholar]
- 15.Marcacci M., Zaffagnini S., Giordano G., Iacono F., Presti M.L. Anterior cruciate ligament reconstruction associated with extra-articular tenodesis: A prospective clinical and radiographic evaluation with 10- to 13-year follow-up. Am J Sports Med. 2009;37:707–714. doi: 10.1177/0363546508328114. [DOI] [PubMed] [Google Scholar]
- 16.Duthon V.B., Magnussen R.A., Servien E., Neyret P. ACL reconstruction and extra-articular tenodesis. Clin Sports Med. 2013;32:141–153. doi: 10.1016/j.csm.2012.08.013. [DOI] [PubMed] [Google Scholar]
- 17.Colombet P.D. Navigated intra-articular ACL reconstruction with additional extra-articular tenodesis using the same hamstring graft. Knee Surg Sports Traumatol Arthrosc. 2011;19:384–389. doi: 10.1007/s00167-010-1223-0. [DOI] [PubMed] [Google Scholar]
- 18.Sonnery-Cottet B., Thaunat M., Freychet B., Pupim B.H., Murphy C.G., Claes S. Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-year follow-up. Am J Sports Med. 2015;43:1598–1605. doi: 10.1177/0363546515571571. [DOI] [PubMed] [Google Scholar]
- 19.Smith J.O., Yasen S.K., Lord B., Wilson A.J. Combined anterolateral ligament and anatomic anterior cruciate ligament reconstruction of the knee. Knee Surg Sports Traumatol Arthrosc. 2015;23:3151–3156. doi: 10.1007/s00167-015-3783-5. [DOI] [PubMed] [Google Scholar]
- 20.Helito C.P., Bonadio M.B., Gobbi R.G. Combined intra- and extra-articular reconstruction of the anterior cruciate ligament: The reconstruction of the knee anterolateral ligament. Arthrosc Tech. 2015;4:e239–e244. doi: 10.1016/j.eats.2015.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kernkamp W.A., van de Velde S.K., Bakker E.W., van Arkel E.R. Anterolateral extra-articular soft tissue reconstruction in anterolateral rotatory instability of the knee. Arthrosc Tech. 2015;4:e863–e867. doi: 10.1016/j.eats.2015.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ferretti A., Monaco E., Fabbri M., Maestri B., De Carli A. Prevalence and classification of injuries of anterolateral complex in acute anterior cruciate ligament tears. Arthroscopy. 2017;33:147–154. doi: 10.1016/j.arthro.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 23.Vadalà A.P., Iorio R., De Carli A. An extra-articular procedure improves the clinical outcome in anterior cruciate ligament reconstruction with hamstrings in female athletes. Int Orthop. 2013;37:187–192. doi: 10.1007/s00264-012-1571-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dejour D., Vanconcelos W., Bonin N., Saggin P.R. Comparative study between mono-bundle bone-patellar tendon-bone, double-bundle hamstring and mono bundle bone-patellar tendon-bone combined with a modified Lemaire extra-articular procedure in anterior cruciate ligament reconstruction. Int Orthop. 2013;37:193–199. doi: 10.1007/s00264-012-1718-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ferretti A., Monaco E., Ponzo A. Combined intra-articular and extra-articular reconstruction in anterior cruciate ligament-deficient knee: 25 years later. Arthroscopy. 2016;32:2039–2047. doi: 10.1016/j.arthro.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 26.Kittl C., El-Daou H., Athwal K.K. The role of the anterolateral structures and the ACL in controlling laxity of the intact and ACL-deficient knee. Am J Sports Med. 2016;44:345–354. doi: 10.1177/0363546515614312. [DOI] [PubMed] [Google Scholar]
- 27.Rahnemai-Azar A.A., Miller R.M., Guenther D. Structural properties of the anterolateral capsule and iliotibial band of the knee. Am J Sports Med. 2016;44:892–897. doi: 10.1177/0363546515623500. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Anatomic reconstruction of the anterolateral complex addressing anterolateral rotatory instability both in primary anterior cruciate ligament reconstruction and in revision cases is presented. A left knee is shown. The reconstruction is performed with a pedicle strip of iliotibial tract, fixed on the anatomic origin and insertion points of the anterolateral ligament of the knee in a double-bundle V-shaped fashion.