Abstract
Advances in surgical technique and our knowledge of anterior cruciate ligament (ACL) anatomy have resulted in a marked increase in options for ACL reconstruction. Currently, patient age and activity level, surgeon preference and experience, and cost are factors influencing the type of reconstruction recommended to address knee instability. We present a simplified transtibial method of ACL reconstruction using a single-bundle, doubled tibialis anterior allograft. This method uses fixation with a suspensory device on the femur and a bio-composite interference screw on the tibia. We recommend this simplified technique for primary ACL reconstruction because it minimizes total steps, thus limiting variance, maximizing efficiency, and reducing potential technical error.
Anterior cruciate ligament (ACL) reconstruction is one of the most common procedures performed by orthopaedic surgeons with the goal of restoring functional stability.1 Advances in surgical technique have resulted in a marked improvement in outcomes, and current options for surgical reconstruction are numerous.2, 3 The choice of reconstruction technique is dependent on surgeon experience and numerous patient factors, in balance with considerations of cost, efficacy, and long-term outcomes. We propose a single-bundle transtibial method using a doubled tibialis anterior allograft fixed with a suspensory device on the femoral cortex and a bio-composite interference screw in the tibia. We believe this technique simplifies ACL reconstruction by limiting the number of steps with an aim at reducing potential errors while providing an anatomic reconstruction.
Surgical Technique
ACL reconstruction (Video 1) is performed by combining general anesthesia and a continuous-infusion femoral nerve catheter (0.2% ropivacaine) left in place for 72 hours to maximize pain control and minimize need for systemic narcotics. The patient is placed supine on a standard operating table, and full examination of the knee is performed including grading of the Lachman, anterior drawer, and pivot-shift tests. A lateral post is placed high on the thigh, and the leg is prepared and draped in sterile fashion. The leg is allowed to hang laterally over the side of the table and flexed to a minimum of 90°. A lateral parapatellar portal is then made with a No. 11 blade even with the distal pole of the patella, creating an incision larger at the skin than the joint (one-way valve). A complete diagnostic evaluation is performed using lactated Ringer solution with epinephrine (1 mL of 1:1,000 per 5 L) and gravity flow. Concomitant meniscal or chondral pathology is noted and addressed. A medial working portal is then created with a No. 11 blade after localization with a spinal needle. The portal is placed just proximal and medial to the anterior horn of the medial meniscus. A 4.5-mm vacuum shaver is introduced through a medial working portal, and the torn fibers of the ACL are debrided minimally, focusing on those subluxated anteriorly and the midsubstance elements that are displaced. Care is taken to preserve remnants at the tibial and femoral footprints to ensure anatomic tunnel placement. A notchplasty should not be necessary if a 30° arthroscope is properly positioned.
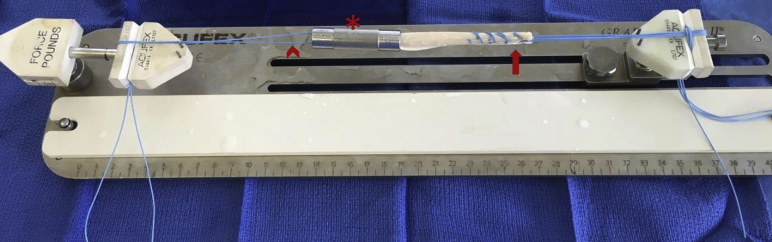
The allograft construct is prepared on the back table while the patient undergoes anesthesia or after the diagnostic arthroscopy. All allografts (Community Tissue Services, Kettering, OH) are fresh frozen and average 8.0 mm in diameter when doubled. The graft is thawed at room temperature in sterile normal saline solution. An interlocking whipstitch (No. 2 Ti-Cron; Medtronic, Minneapolis, MN) is placed at each extreme (approximately 15 mm) with care taken to leave at least 30 mm of non-stitched tendon for intraosseous and intra-articular elements of the graft. The goal is to leave no suture on the graft once in situ to maximize the biological surface for healing. The graft is then doubled over a free suture and sized to the nearest 0.5 mm using Acufex sizing tubes (Smith & Nephew, Andover, MA). The graft is pre-tensioned to 10 N using the Graftmaster II system (Smith & Nephew), and the sizing tube is placed over the folded end to prevent swelling as the tendon warms to room temperature (Fig 1). The graft is covered with a sponge soaked in lactated Ringer solution while under tension.
Fig 1.
Anterior cruciate ligament allograft preparation using Graftmaster II system. The ends of the tibialis anterior allograft are whipstitched with No. 2 Ti-Cron (arrow), and the graft is then doubled over a free suture (chevron). The graft is sized to the nearest 0.5 mm, the appropriate sizing tube is placed over the folded (femoral) end (asterisk), and the graft is tensioned to 10 N.
The arthroscope (viewing from the lateral portal) is used to identify the anatomic tibial footprint of the ACL. The tibial guide (Acufex Director Elbow Aimer; Smith & Nephew) is placed into the medial portal and directed over the tibial footprint (Fig 2). A hemostat can be used to dilate the medial portal to ease passage of the aiming guide. The angle of the guide is set to 55° to ensure adequate tibial tunnel length, which can be ascertained once the bullet portion is placed on the tibial cortex. An incision is then made using a No. 15 blade over the medial tibia, halfway between the posterior cortex and medial border of the patellar tendon. A 2.7-mm guide pin is used to set the trajectory of the tibial tunnel. The guide pin enters the joint approximately 3 mm anterior to the tip of the elbow aimer, which is placed in the posterior fibers of the ACL footprint remnants. The tibia is then drilled with a cannulated bone-harvesting drill bit to match the graft diameter with the sizing cannula acting as a soft-tissue protector. Morcellized bone graft from the flutes of the drill are saved for grafting into the tibial bone tunnel prior to placement of the final interference screw. The knee is then flexed past 90°, and the over-the-top femoral guide (Acufex; Smith & Nephew) is introduced through the tibial tunnel. The location of the ACL origin is confirmed using the clock-face reference technique (Fig 3).
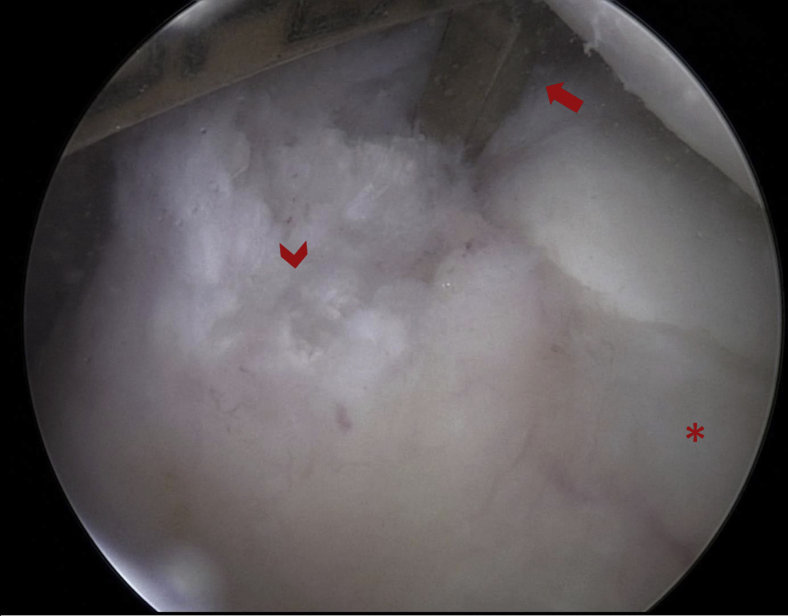
Fig 2.
Arthroscopic view of the tibial footprint of the anterior cruciate ligament in a left knee viewing from the lateral portal. The elbow aiming tibial guide (arrow) is placed so that the tip is at the posterior aspect of the remnant anterior cruciate ligament stump. This allows the guide pin to pass through the center of the tibial footprint (chevron). The posterior border of the anterior horn of the lateral meniscus (asterisk) can also be used to help confirm the footprint location.
Fig 3.
Arthroscopic view of the femoral footprint of the anterior cruciate ligament in a left knee viewing from the lateral portal. The over-the-top guide (arrow) is placed through the tibial tunnel (chevron) and seated at the proposed location of the femoral tunnel. Remnants of the native anterior cruciate ligament (asterisk) are used to confirm anatomic placement of the tunnel at the 1:30 clock-face position.
The femoral guide is selected with a size equivalent to the diameter of the graft divided by 2 (rounding down). This may lead to some posterior wall compromise but does not affect suspensory femoral fixation and allows for a more anatomic graft placement. The femoral guide pin is then advanced through the lateral cortex until it breaches the skin (the knee does not have to be hyperflexed). A protective handle is secured onto the tip to facilitate pulling the construct retrograde into the knee. A 20- to 25-mm femoral socket is then created under direct arthroscopic visualization with a calibrated endoscopic acorn drill matching the diameter of the graft. The acorn drill is removed, and a 4.5-mm cannulated drill is used to complete the tunnel. The total femoral tunnel length is assessed using the drill calibrations, and a final measure is gained as the lateral cortex is traversed. The folded end of the allograft is lassoed through the continuous-loop EndoButton CL Ultra (Smith & Nephew) that correlates with the total femoral tunnel length minus the desired graft insertion length (at least 20 mm) (Fig 4). It is necessary to select an EndoButton length at least 5 mm longer than the femoral tunnel length to allow for flipping of the extracortical titanium element after exiting the femoral cortex. The graft-EndoButton construct is then passed through the graft sizing tube one final time to compress the added mass (line-to-line drilling). The lead sutures for the button are loaded through the islet in the guide pin, and the pin is pulled through the lateral thigh. The button is advanced until it is past the lateral femoral cortex and flipped. Flipping of the button is confirmed by achieving toggle feedback and then pulling retrograde on the tibial end of the graft to secure the button against the external femoral cortex. The knee is brought into extension for this, and tibial fixation with a tapered bio-interference screw and sheath (Intrafix; DePuy Mitek, Raynham, MA) is performed while this tension is maintained. Harvested bone graft is packed into the sheath after it is inserted, prior to the interference screw placement. We do not routinely cycle the knee before tibial fixation is performed because the graft was pre-tensioned to allow for creep. The residual end of the graft, including the Ti-Cron sutures, is cut, and a rongeur is used to remove any exposed sheath. The knee is examined arthroscopically to ensure no loose bodies or graft impingement is noted. The tibial wound is irrigated, and the wounds are closed. Radiographs are obtained in the postanesthesia care unit to confirm adequate positioning of the tunnels and EndoButton (Fig 5).
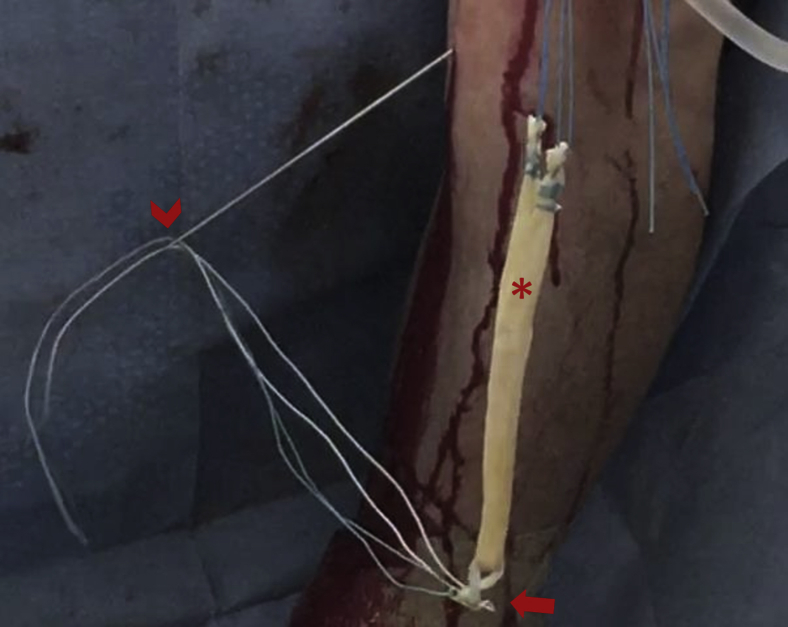
Fig 4.
Passage of the prepared allograft (asterisk) through the EndoButton (arrow). The lead sutures for the button are passed through the islet in the guide pin (chevron). Care is taken to seat the loop of the EndoButton at the same portion of the allograft where the free suture was used for tensioning.
Fig 5.
Postoperative anteroposterior and lateral radiographs of the left knee after anterior cruciate ligament reconstruction. The tibial tunnels (chevrons) are visualized, and the EndoButton (arrows) is seated in the appropriate position on the lateral femoral cortex. The interference screw (asterisks) can be visualized in the posterior aspect of the tibial tunnel.
Postoperatively, patients are instructed on a rehabilitation protocol with progression dependent on achieving functional milestones (Table 1). This includes immediate crutch-assisted weight bearing as tolerated with a knee immobilizer for protection only during the period of quadriceps inhibition while the nerve block remains in effect. Routine follow-up is conducted at 2 and 6 weeks as well as 3, 6, 12, and 24 months postoperatively. Patients are allowed to return to sports after all goals of physical therapy have been met (Table 1).
Table 1.
Rehabilitation Protocol Based on Achievement of Functional Milestones After Anterior Cruciate Ligament Reconstruction
| Phase | Timeline | Focus and Goals |
|---|---|---|
| 1 | 0-2 wk | Protection, edema management, ROM, muscle activation |
| 2 | 2-4 wk | ROM, gait, knee control |
| 3 | 1-3 mo | Strength and balance |
| 4 | 3-5 mo | Walking-jogging program, agility, plyometrics |
| 5 | ≥5 mo | Sport-specific training, agility, plyometrics |
ROM, range of motion.
Discussion
Anatomic single-bundle ACL reconstruction has evolved significantly since its first description.4 Surgical reconstruction of the ACL can be compared on the basis of many criteria including biomechanical properties, biology, and technical difficulty of the procedure. As technology continues to improve, surgeon comfort and ease of procedure become critical to ensure consistent anatomic reconstruction and improved clinical outcomes. Therefore, we present a simplified technique for primary ACL reconstruction. We prefer this technique because as a single allograft doubled, the tibialis anterior allograft is easy to prepare. In addition, because there are only 2 strands instead of 4, the graft can be subtly repositioned with the interference screw if the tibial tunnel is slightly nonanatomic. This is more difficult to achieve with 4-stranded soft-tissue allografts, which tend to splay and not translate in the tibial tunnel. Lastly, suspensory fixation is our preferred femoral fixation technique because it eliminates any potential complications of intra-articular hardware and simplifies revision reconstruction.
Pearls and pitfalls of our reconstruction technique can be found in Table 2. Controversy exists in the literature regarding multiple aspects of our surgical technique. Relative technical advantages and potential limitations of our reconstruction technique are listed in Table 3. First, the use of tibialis anterior allografts for reconstruction of the ACL has been questioned.17 However, recent data have shown that outcomes with tibialis anterior allograft are good in the correct patient population.18, 19, 20 Second, transtibial femoral drilling has come under scrutiny; however, in a widely cited study the trans-tibial group and accessory portal drilling group did not differ in their rate of revision ACL reconstruction.21 We have shown that it is technically feasible to achieve an anatomic femoral tunnel through a transtibial method (Fig 3). Lastly, there is not a consensus regarding single- versus double-bundle ACL reconstruction. We believe the single-bundle reconstruction shown here is technically easier than any current double-bundle technique.
Table 2.
Pearls and Pitfalls of Single-Bundle Transtibial Surgical Technique
| Technique | Pearl | Pitfall |
|---|---|---|
| Joint preparation | Sufficient graft debridement should be performed to identify the anatomic footprints. | Too much remnant graft may lead to impingement or cyclops lesions. |
| Arthroscope orientation | The wall of the lateral condyle should be kept perpendicular to the arthroscope. | Losing orientation of the femoral footprint may lead to nonanatomic tunnel placement. |
| Tibial tunnel placement | The tip of the elbow guide should be placed at the posterior portion of the anterior cruciate ligament footprint. | Placement of the tunnel too anteriorly leads to impingement and the inability to re-create the anatomic femoral tunnel. |
| Femoral tunnel placement | An over-the-top guide equivalent to the radius of the graft should be used so that the tunnel is not too anterior. | Placing the guide too high on the wall leads to a vertical or nonanatomic graft orientation. |
| EndoButton placement | The minimal button loop length should be calculated as follows: Femoral tunnel length − Length of graft tunnel + 5 mm. | Not receiving “toggle” feedback when seating the button indicates the button has not exited the cortex. The graft is not fixed proximally. |
| Tibial Intrafix placement | The tibia should be packed with bone graft after the sheath is placed. The screw can be strategically placed to subtly translate the graft if desired. | Not seating the screw and sheath flush with the cortex may predispose to symptomatic hardware. |
Table 3.
Potential Advantages and Limitations of Single-Bundle Transtibial Anterior Cruciate Ligament Reconstruction Using Tibialis Anterior Allograft
| Advantages | Limitations | |
|---|---|---|
| Tibialis anterior allograft | • Limits donor-site morbidity • Speeds up immediate postoperative recovery • Shortens operative time5 |
• Risk of rerupture in young and active patients6, 7, 8, 9 • Risk of disease transmission or structural compromise by terminal sterilization2 • Cost of allograft10 |
| Transtibial femoral drilling | • Isometric graft decreases strain11 • Longer tunnel lengths12 • No risk of damaging articular cartilage on medial femoral condyle13 |
• Harder to achieve anatomic femoral tunnel14 • Decreased joint kinematics at time 0 compared with anteromedial drilling15 |
| Suspensory femoral fixation | • Graft can be placed more posteriorly; no need to worry about posterior femoral blowout • Minimal potential for intra-articular femoral hardware • Easier to perform revision surgery |
• Does not achieve compressive fixation of tendon to bone • Possible tunnel widening due to windshield-wiper effect |
| Single-bundle reconstruction | • Easier surgical technique • Outcomes similar to double-bundle reconstruction16 |
• Decreased time 0 kinematics compared with double bundle • Native anatomy is not completely restored |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: M.R. receives support from Synthes. D.C. receives support from Synthes. Funds were given to Oregon Health and Science University for attendance of the AO basic course.
Supplementary Data
Transtibial reconstruction of anterior cruciate ligament using doubled tibialis anterior allograft. The graft is prepared on the back table while the patient is positioned. A standard examination and diagnostic knee arthroscopy are performed. The tibial tunnel is set first using a shoulder aiming guide and pin and then drilled to the exact diameter of the graft using a cigar-shaped drill. The femoral tunnel is set using an over-the-top offset guide placed through the tibial tunnel. The femoral socket is drilled 25 mm deep with an acorn drill matching the exact diameter of the graft. The remainder of the intraosseous tunnel is created using a 4.5-mm flexible drill. The graft is then loaded onto a continuous-loop EndoButton and passed through the tibial and femoral tunnels using the lead sutures until the button exits the lateral femoral cortex and is flipped. The knee is brought into extension, and retrograde tension is placed on the graft while it is being secured into the tibial tunnel using a screw and sheath construct.
References
- 1.Maletis G.B., Inacio M.C., Desmond J.L., Funahashi T.T. Reconstruction of the anterior cruciate ligament: Association of graft choice with increased risk of early revision. Bone Joint J. 2013;95-B:623–628. doi: 10.1302/0301-620X.95B5.30872. [DOI] [PubMed] [Google Scholar]
- 2.Cohen S.B., Sekiya J.K. Allograft safety in anterior cruciate ligament reconstruction. Clin Sport Med. 2007;26:597–605. doi: 10.1016/j.csm.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 3.West R.V., Harner C.D. Graft selection in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2005;13:197–207. doi: 10.5435/00124635-200505000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Chambat P., Guier C., Sonnery-Cottet B., Fayard J.M., Thaunat M. The evolution of ACL reconstruction over the last fifty years. Int Orthop. 2013;37:181–186. doi: 10.1007/s00264-012-1759-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cooper M.T., Kaeding C. Comparison of the hospital cost of autograft versus allograft soft-tissue anterior cruciate ligament reconstructions. Arthroscopy. 2010;26:1478–1482. doi: 10.1016/j.arthro.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 6.Lenehan E.A., Payne W.B., Askam B.M., Grana W.A., Farrow L.D. Long-term outcomes of allograft reconstruction of the anterior cruciate ligament. Am J Orthop (Belle Mead NJ) 2015;44:217–222. [PubMed] [Google Scholar]
- 7.van Eck C.F., Schkrohowsky J.G., Working Z.M., Irrgang J.J., Fu F.H. Prospective analysis of failure rate and predictors of failure after anatomic anterior cruciate ligament reconstruction with allograft. Am J Sports Med. 2012;40:800–807. doi: 10.1177/0363546511432545. [DOI] [PubMed] [Google Scholar]
- 8.Tejwani S.G., Chen J., Funahashi T.T., Love R., Maletis G.B. Revision risk after allograft anterior cruciate ligament reconstruction: Association with graft processing techniques, patient characteristics, and graft type. Am J Sport Med. 2015;43:2696–2705. doi: 10.1177/0363546515589168. [DOI] [PubMed] [Google Scholar]
- 9.Spindler K.P., Parker R.D., Andrish J.T. Prognosis and predictors of ACL reconstructions using the MOON cohort: A model for comparative effectiveness studies. J Orthop Res. 2013;31:2–9. doi: 10.1002/jor.22201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barrera Oro F., Sikka R.S., Wolters B. Autograft versus allograft: An economic cost comparison of anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:1219–1225. doi: 10.1016/j.arthro.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 11.Xu Y., Liu J., Kramer S. Comparison of in situ forces and knee kinematics in anteromedial and high anteromedial bundle augmentation for partially ruptured anterior cruciate ligament. Am J Sports Med. 2011;39:272–278. doi: 10.1177/0363546510383479. [DOI] [PubMed] [Google Scholar]
- 12.Chang C.B., Choi J.Y., Koh I.J., Lee K.J., Lee K.H., Kim T.K. Comparisons of femoral tunnel position and length in anterior cruciate ligament reconstruction: Modified transtibial versus anteromedial portal techniques. Arthroscopy. 2011;27:1389–1394. doi: 10.1016/j.arthro.2011.06.013. [DOI] [PubMed] [Google Scholar]
- 13.Lubowitz J.H. Anteromedial portal technique for the anterior cruciate ligament femoral socket: Pitfalls and solutions. Arthroscopy. 2009;25:95–101. doi: 10.1016/j.arthro.2008.10.012. [DOI] [PubMed] [Google Scholar]
- 14.Riboh J.C., Hasselblad V., Godin J.A., Mather R.C., III Transtibial versus independent drilling techniques for anterior cruciate ligament reconstruction: A systematic review, meta-analysis, and meta-regression. Am J Sports Med. 2013;41:2693–2702. doi: 10.1177/0363546513506979. [DOI] [PubMed] [Google Scholar]
- 15.Chen Y., Chua K.H., Singh A. Outcome of single-bundle hamstring anterior cruciate ligament reconstruction using the anteromedial versus the transtibial technique: A systematic review and meta-analysis. Arthroscopy. 2015;31:1784–1794. doi: 10.1016/j.arthro.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 16.Chen G., Wang S. Comparison of single-bundle versus double-bundle anterior cruciate ligament reconstruction after a minimum of 3-year follow-up: A meta-analysis of randomized controlled trials. Int J Clin Exp Med. 2015;8:14604–14614. [PMC free article] [PubMed] [Google Scholar]
- 17.Singhal M.C., Gardiner J.R., Johnson D.L. Failure of primary anterior cruciate ligament surgery using anterior tibialis allograft. Arthroscopy. 2007;23:469–475. doi: 10.1016/j.arthro.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 18.Nyland J., Caborn D.N., Rothbauer J., Kocabey Y., Couch J. Two-year outcomes following ACL reconstruction with allograft tibialis anterior tendons: A retrospective study. Knee Surg Sport Traumatol Arthrosc. 2003;11:212–218. doi: 10.1007/s00167-003-0371-x. [DOI] [PubMed] [Google Scholar]
- 19.Snow M., Campbell G., Adlington J., Stanish W.D. Two to five year results of primary ACL reconstruction using doubled tibialis anterior allograft. Knee Surg Sport Traumatol Arthrosc. 2010;18:1374–1378. doi: 10.1007/s00167-009-0997-4. [DOI] [PubMed] [Google Scholar]
- 20.Lawhorn K.W., Howell S.M., Traina S.M., Gottlieb J.E., Meade T.D., Freedberg H.I. The effect of graft tissue on anterior cruciate ligament outcomes: A multicenter, prospective, randomized controlled trial comparing autograft hamstrings with fresh-frozen anterior tibialis allograft. Arthroscopy. 2012;28:1079–1086. doi: 10.1016/j.arthro.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 21.Duffee A., Magnussen R.A., Pedroza A.D., Flanigan D.C., Kaeding C.C. Transtibial ACL femoral tunnel preparation increases odds of repeat ipsilateral knee surgery. J Bone Joint Surg Am. 2013;95:2035–2042. doi: 10.2106/JBJS.M.00187. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transtibial reconstruction of anterior cruciate ligament using doubled tibialis anterior allograft. The graft is prepared on the back table while the patient is positioned. A standard examination and diagnostic knee arthroscopy are performed. The tibial tunnel is set first using a shoulder aiming guide and pin and then drilled to the exact diameter of the graft using a cigar-shaped drill. The femoral tunnel is set using an over-the-top offset guide placed through the tibial tunnel. The femoral socket is drilled 25 mm deep with an acorn drill matching the exact diameter of the graft. The remainder of the intraosseous tunnel is created using a 4.5-mm flexible drill. The graft is then loaded onto a continuous-loop EndoButton and passed through the tibial and femoral tunnels using the lead sutures until the button exits the lateral femoral cortex and is flipped. The knee is brought into extension, and retrograde tension is placed on the graft while it is being secured into the tibial tunnel using a screw and sheath construct.