Abstract
Scapholunate ligament (SLL) injury is the most frequent injury of the intrinsic carpal ligaments. The dorsal part of the SLL is the most important part for the stability of the scapholunate joint, and tears of this part and at least one of its secondary capsular attachments cause scapholunate dissociation. The arthroscopic technique most frequently used for acute injuries is reduction and fixation with Kirschner wires, and techniques that involve a primary repair of the injured ligament are performed by open surgery with efficient results. However, they lead to significant stiffness of the wrist due to injury to the soft tissue caused by damage to the secondary dorsal stabilizers; the dorsal blood supply; and in many cases, the proprioceptive innervation of the posterior interosseous nerve. We present an all-arthroscopic technique for the direct repair of acute injuries of the dorsal part of the SLL using bone anchors, complemented by a dorsal arthroscopic plication that reconstructs the dorsal capsulo-scapholunate septum of the scapholunate complex.
Scapholunate ligament (SLL) injury is the most frequent injury of the intrinsic carpal ligaments and is mostly the result of a fall over an outstretched hand.1 The dorsal part of the SLL is the most important part for the stability of the scapholunate joint, and its insertion into the dorsal capsule creates the dorsal capsulo-scapholunate septum (DCSS).2 Tears of the SLL and at least one of its secondary capsular attachments cause scapholunate dissociation. In scapholunate dissociation, the best results are obtained at the acute stage or within the first 2 months after the injury, especially with partial tears. The arthroscopic technique most frequently used in these injuries is reduction and fixation with Kirschner wires.3, 4 Techniques for dorsal capsular reinforcement are described later,5 but none of these techniques involve a primary repair of the injured ligament, as is performed in open surgery.6 The most used technique for open surgery in complete acute tears is a direct repair of the SLL by bone anchors or transosseous tunnels, adding a dorsal capsular reinforcement.7, 8 These techniques are generally efficient, but they lead to significant stiffness of the wrist. When performing a dorsal capsulotomy, we are damaging the secondary dorsal stabilizers9; the dorsal blood supply of the lunate, scaphoid, and SLL10; and in many cases, the proprioceptive innervation of the posterior interosseous nerve (PIN).11 We present an all-arthroscopic technique for the direct repair of injuries of the dorsal part of the SLL by bone anchors, complemented by a dorsal arthroscopic plication that reconstructs the DCSS of the scapholunate complex (Table 1).
Table 1.
Advantages and Limitations of Arthroscopic Treatment
| Advantages |
| The technique avoids the dorsal approach and damage to the soft tissue, allowing a higher range of joint mobility. |
| It avoids injury to the posterior interosseous nerve, which plays an important role in the proprioception of the wrist. |
| It protects against injury to the SLL vascular dorsal supply, increasing its healing potential. |
| It prevents damage to the secondary dynamic stabilizers, such as the intercarpal dorsal ligament and dorsal radiocarpal ligament. |
| It allows verification of the correct placement and introduction of the implants, as well as the correct reduction of the scapholunate interval. |
| It reconstructs the important dorsal portion of the SLL with a direct anatomic biological repair. |
| Limitations |
| This is a complex technique with a large learning curve. |
| It requires previous wrist arthroscopic skills. |
| It requires specific materials for arthroscopy. |
SLL, scapholunate ligament.
Indications
The ideal candidates are patients with a partial or complete injury, whether acute or subacute, with competent secondary stabilizers and without chondral involvement, that is, a pre-dynamic scapholunate instability, according to the classification of Garcia-Elias et al.,12 in which the SLL still maintains some potential for healing and scarring and the state of the tissue permits direct repair. This technique can be used in both isolated injuries and SLL tears associated with a distal radius fracture. Chronic injuries or nonreducible instability is not included in the indications.
Technique
For the SLL capsuloligamentous repair technique, we mainly use the 3-4, 6R, midcarpal ulnar (MCU), and midcarpal radial (MCR) arthroscopic portals (Fig 1, Video 1). The patient is placed in the prone position with the arm on a hand table. We use the Arc Wrist Tower (Acumed, Hillsboro, OR) for traction, a 2.5-mm arthroscope (Arthrex, Naples, FL), and a 2.9-mm shaver (Smith & Nephew, Andover, MA). The possibility of performing the arthroscopic procedure both vertically and horizontally by using a specific traction system provides comfort and allows us to simultaneously perform arthroscopy and fluoroscopy.
Fig 1.
Arthroscopic portals used in technique: 3-4, 6R, midcarpal ulnar (MCU), midcarpal radial (MCR).
Diagnostic Arthroscopy and Preparation of Scapholunate Joint
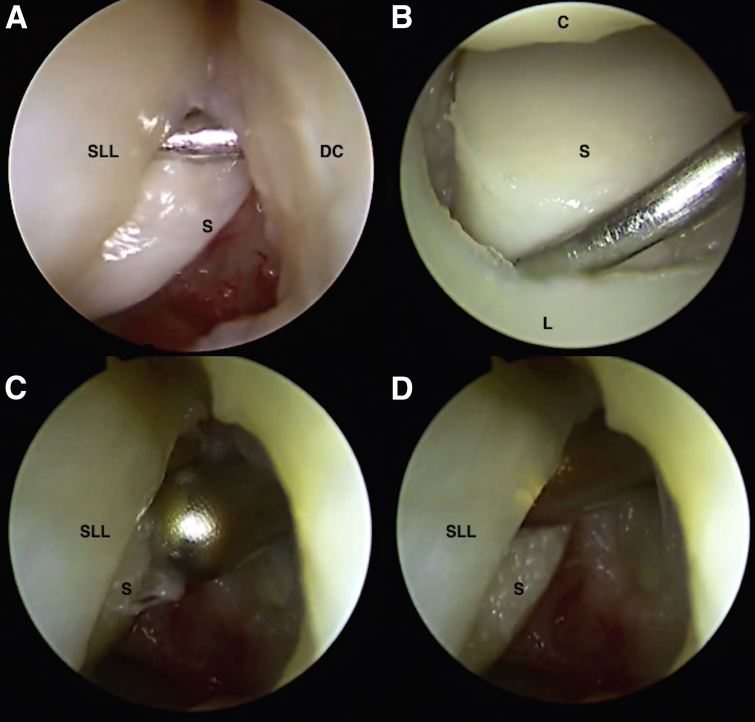
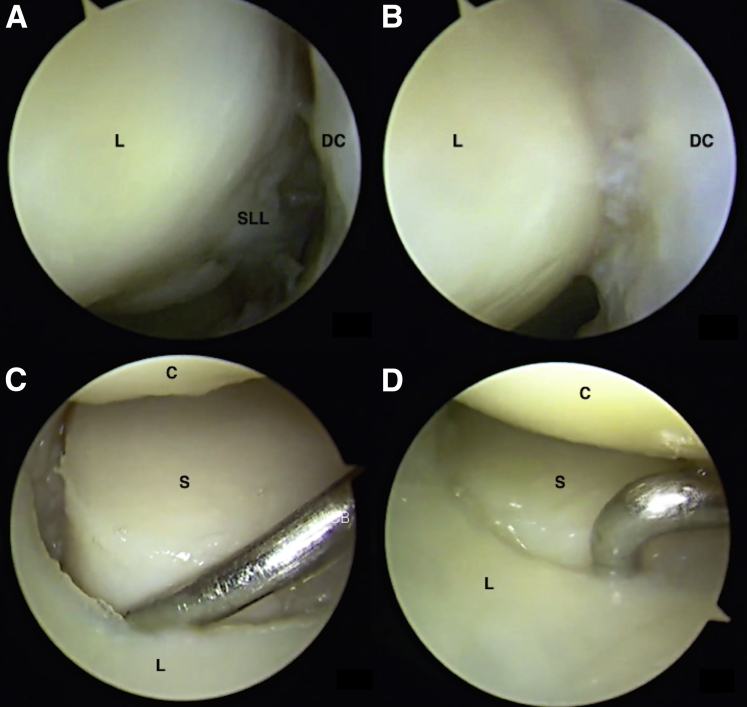
We begin the procedure by performing a dry diagnostic arthroscopy through the previously mentioned portals. We evaluate and classify the injury of the SLL and associated injuries through the radiocarpal and midcarpal portals (Fig 2 A and B).
Fig 2.
(A) Evaluation of a complete tear of the scapholunate ligament (SLL). The arthroscope is in the 6R portal, and the probe is in the 3-4 portal. The probe can be introduced between the scaphoid and the lunate. (B) With the arthroscope in the midcarpal ulnar portal and probe in the midcarpal radial portal, the scapholunate instability (Geissler grade III) at the midcarpal joint is evaluated. (C, D) Cleaning of the fibers and scar material and cruentation of the insertion of the SLL on the scaphoid. The arthroscope is in the 6R portal, and the shaver is in the 3-4 portal. A left wrist is shown. (C, capitate; DC, dorsal capsule; L, lunate; S, scaphoid.)
Acute injuries of the SLL and early subacute injuries of Geissler grade II or III with integrity of the articular cartilage and reducible carpus are suitable for repair. It is mandatory that the tissue of the injured ligament is of good quality, allowing its repair.
We clean the fibers and scar material. We perform the cruentation of the insertion of the SLL on the scaphoid or its insertion on the lunate, according to where the ligament has been detached, and debridement and cruentation of the dorsal capsule (Fig 2 C and D).
Scapholunate Reduction, Anchor Insertion, and Ligamentous Suturing
Through the radiocarpal and midcarpal portals, we verify the proper alignment of the scapholunate joint, and if necessary, we can reduce possible misalignments in both height and rotation. Using Kirschner wires as a joystick to perform the reduction may be useful, and sometimes one Kirschner wire between the radius and lunate is needed to maintain the radiolunate alignment.
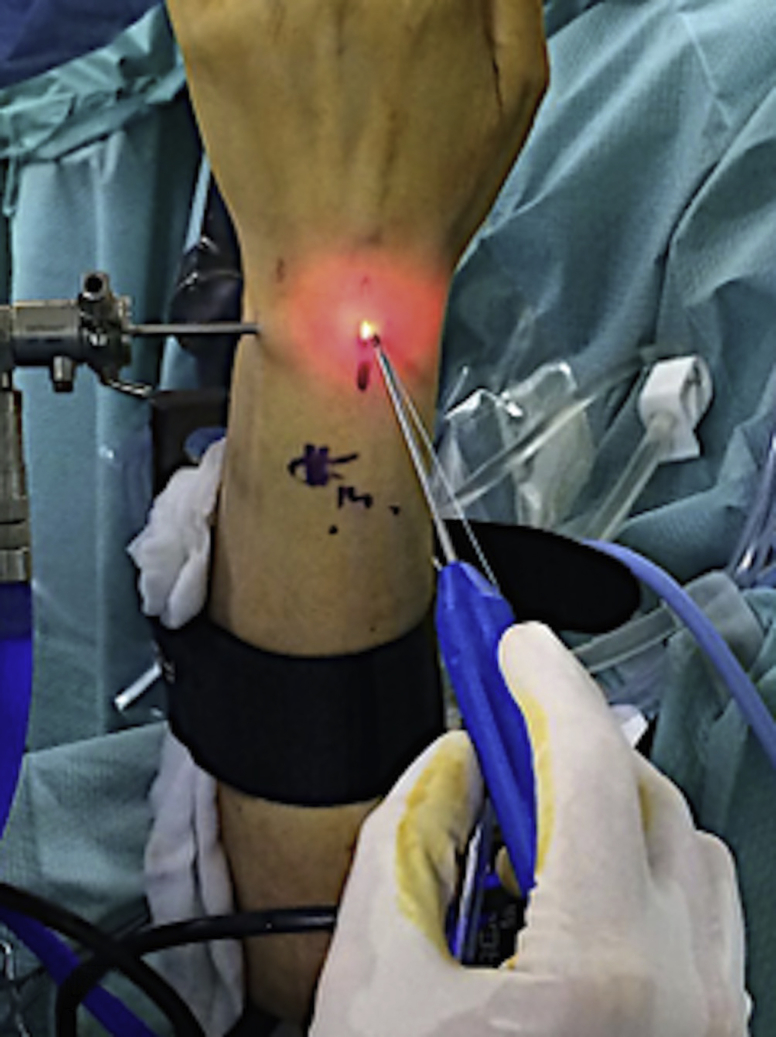
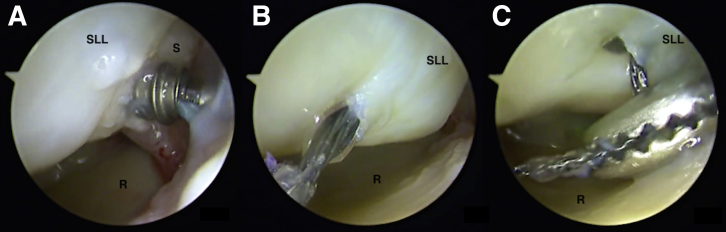
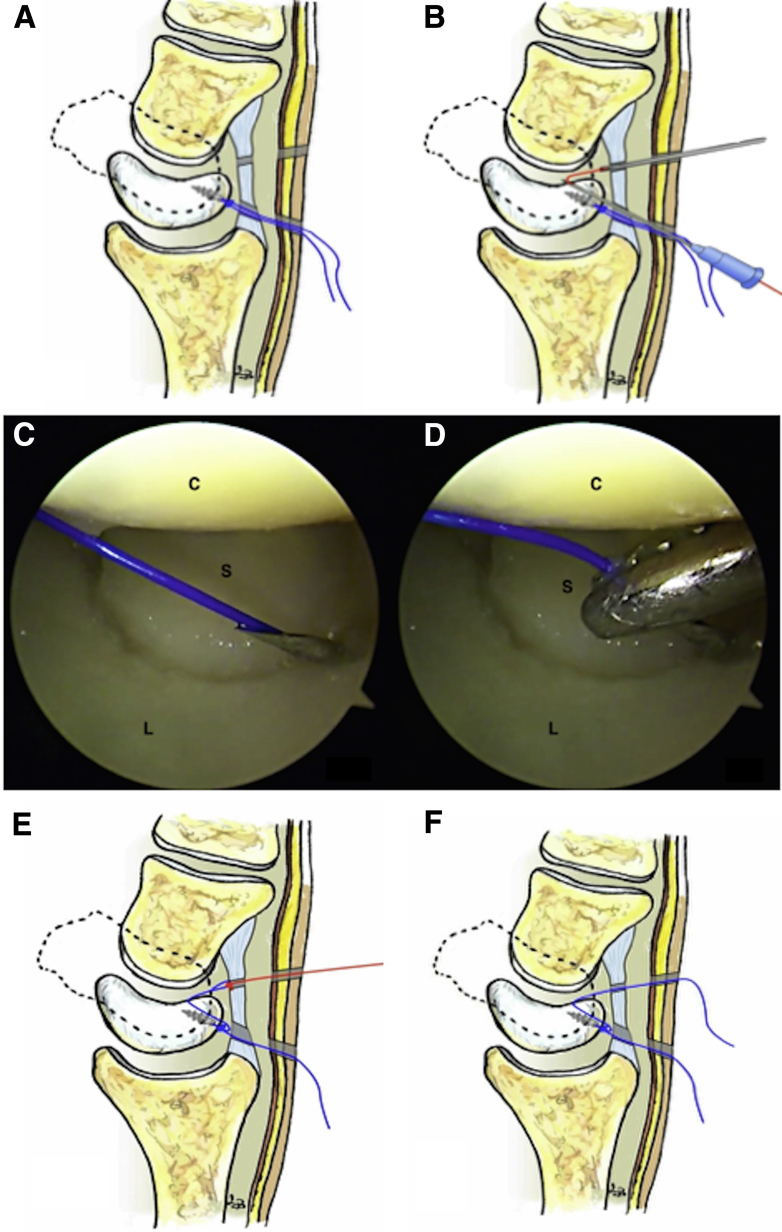
With the arthroscope in the 6R portal and with direct vision of the dorsal portion of the SLL, we use the 3-4 portal and may add the 4-5 portal when necessary. We introduce the initiating wire of the anchor through the 3-4 portal and perforate at the dorsal edge of the scaphoid or the lunate according to where the ligament has been detached. We then introduce a 2.2-mm Micro Corkscrew anchor (Arthrex) through the 3-4 portal (Fig 3), and we thread it into the perforated hole (Fig 4A) until it is completely buried in the articular surface. We leave the anchor sutures at the 3-4 portal, and using a 70° TFCC SutureLasso (Arthrex) from the 3-4 portal, we cross the SLL remains from dorsal to proximal, recovering the nitinol loop through the same portal (Fig 4 B and C) with a Mini Suture Hook (Arthrex). By using the loop, we pass one of the implant sutures through a detached edge of the ligament, and we pull it out again through the 3-4 portal. After this, with the help of a knot pusher, we tie both sutures over the implant, keeping a simple stitch through the SLL, with the sutures tied and uncut (Fig 5 A and B).
Fig 3.
With the arthroscope in the 6R portal, we use the 3-4 portal as a working portal. The bone anchor is introduced through the 3-4 portal. A left wrist is shown.
Fig 4.
The arthroscope is in the 6R portal, with direct vision of the dorsal portion of the scapholunate ligament (SLL) in a left wrist. (A) We introduce the anchor through the 3-4 portal and place it at the dorsal edge of the scaphoid or lunate according to the spot where the ligament has been detached. (B) Using a 70° TFCC SutureLasso from the 3-4 portal, we cross the SLL remains. (C) Recovery of nitinol loop through the 3-4 portal. (R, radius; S, scaphoid.)
Fig 5.
(A, B) Using a knot pusher, we tie both sutures over the implant, leaving a simple stitch through the scapholunate ligament (SLL), with the sutures tied and uncut. (C, D) The arthroscope is in the 6R portal. Complete repair of the SLL tear is shown in a left wrist. In this case we have used 2 sutures. The first has been cut after knot tying. The second, after knot tying, remains uncut and through the 3-4 portal (arrow). These sutures are used to complete the dorsal reinforcement. (L, lunate.)
More than one bone anchor may be needed to complete the SLL repair. The disposition of the anchors, whether in the scaphoid or in the lunate (or both), will depend on the location and characteristics of the rupture. Regardless, if we use more than one anchor, the sutures of one of them must not be cut on finalizing the knot because they will be used for the following dorsal plication (Fig 5 C and D). We change the arthroscope to the MCU portal and verify the correct alignment between the scaphoid and lunate, as well as their stability.
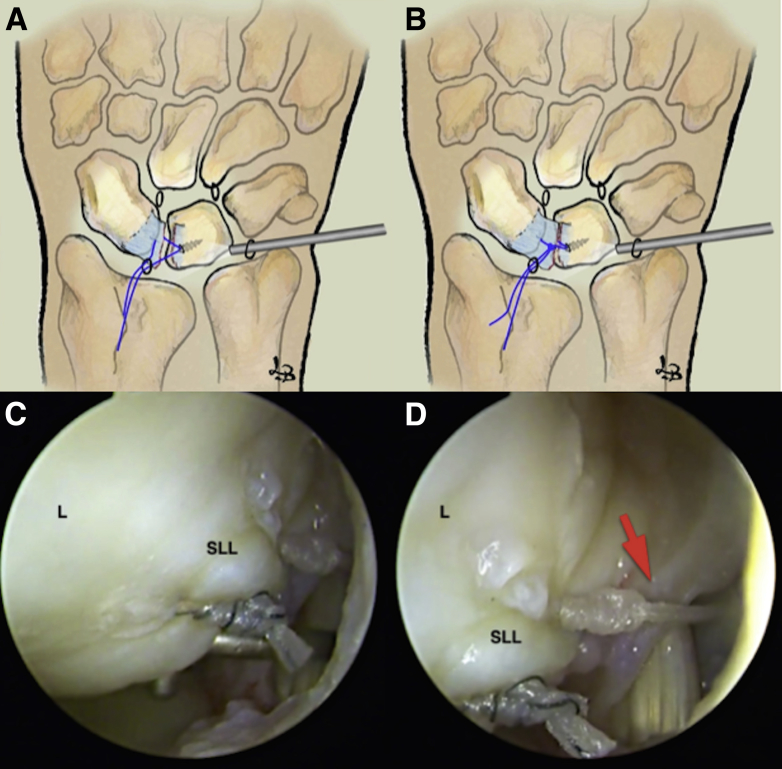
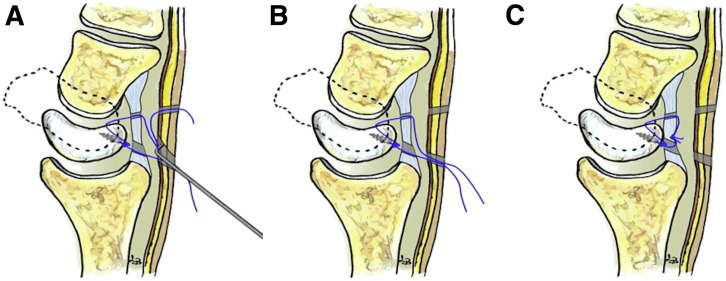
Dorsal Capsulodesis (Dorsal Capsular Reinforcement)
With the arthroscope through the 6R portal, we introduce an 18-gauge needle, with a nylon suture inside, through the 3-4 portal. We direct the needle from the proximal edge of the SLL to the midcarpal joint, through the ligament's tissue (Fig 6 A and B). Changing the arthroscope to the MCU portal, we verify that the 18-gauge needle with the suture crosses the SLL to the midcarpal joint. We introduce the nylon suture through the needle and recover it, using a grasper, through the MCR portal (Fig 6 C and D). The result is a nylon suture with one end entering the 3-4 portal through the SLL, from the radiocarpal space to the midcarpal joint, exiting through the MCR portal. We knot the proximal end of the nylon suture to one of the implant's sutures, and pulling the distal end of the nylon suture, we recover the implant's suture that we have knotted through the MCR portal (Fig 6 E and F).
Fig 6.
(A-D) Through the 3-4 portal, we direct the needle, with a nylon suture inside, to the midcarpal joint, through the ligament's tissue, and we recover the nylon suture with the arthroscope in the midcarpal ulnar portal and the grasper through the midcarpal radial portal. (E, F) We knot the proximal end of the nylon suture to one of the implant's sutures, and pulling the distal end of the nylon suture, we recover the implant's suture that we have knotted through the midcarpal radial portal. (C, capitate; L, lunate; S, scaphoid.)
With the help of a probe, we recover the suture from the MCR portal from the 3-4 portal incision through the existing space between the dorsal capsule and the extensor tendons (Fig 7). We must be careful not to recover the suture through the subcutaneous space because it could tighten the extensor digitorum communis (EDC) tendons (Table 2). Because these portals are created in the radial edge of the EDC and the suture runs parallel to the tendons, the risk of catching the EDC tendons in the suture is very low. We view through the MCU portal and visualize the scapholunate dorsal interval at the midcarpal joint. Again, we knot the implant's sutures, giving the correct tension to observe the reduction of the scapholunate interval. We perform the step of knotting by withdrawing the tower's traction to facilitate reduction by the suture.
Fig 7.
(A, B) We recover the suture from the midcarpal radial portal from the 3-4 portal incision through the existing space between the dorsal capsule and the extensor tendons. These portals are created in the radial edge of the extensor digitorum communis, and the suture runs parallel to the tendons. (C) Final composition after knotting, with complete dorsal plication or reinforcement.
Table 2.
Complications and Prevention
| Complication | Prevention |
|---|---|
| Chondral injuries and osteolysis due to protrusion and implant loosening | Precision should be used in the placement of the implant, and the surgeon should ensure its complete introduction into the articular surface. |
| Rupture of ligament flap on passing the suture through the tissue | Care should be taken when passing the suture through a flap that must have sufficient tissue. The surgeon should attempt to pass the suture with a precise movement and, if possible, in a single attempt. |
| Entrapment of extensor digitorum communis tendons on performing the dorsal capsular reinforcement | The surgeon should ensure that the recovery of the suture, as from the midcarpal joint and the radiocarpal one, is performed through the interval between the dorsal capsule and the tendons and not through the subcutaneous space. |
| Recurrence of the initial injury due to the distension or rupture of the repair | The surgeon should adhere to the indications and protocols of immobilization and rehabilitation. |
Finalization of Capsuloligamentous Suture
Once reduction is verified, we test the scapholunate joint's stability from the midcarpal portals. Viewing through the 6R portal, we can observe the scapholunate dorsal interval closure with the capsular plication performed by reconstructing the dorsal capsuloligamentous union of the scapholunate complex (Fig 8). It is important not to try to introduce the arthroscope through the 3-4 portal because the dorsal capsulodesis would prevent this. We leave a 1.5-mm Kirschner wire, stabilizing the scapholunate interval, and finish the procedure by suturing the portals. Thus, we obtain a simple suture of the SLL over its insertion in the scaphoid or in the lunate, complemented by a dorsal arthroscopic capsulodesis.
Fig 8.
(A, B) With the arthroscope in the 6R portal, we can observe the scapholunate dorsal interval closure with the capsular plication performed by reconstructing the dorsal capsuloligamentous union of the scapholunate complex. (C) With the arthroscope in the midcarpal ulnar portal and the probe in the midcarpal radial portal, there is scapholunate instability before the repair of the scapholunate ligament (SLL) and the dorsal reinforcement. (D) With the arthroscope in the midcarpal ulnar portal and the probe in the midcarpal radial portal, the complete restoration of the scapholunate joint stability is checked after finishing the technique. A left wrist is shown. (C, capitate; DC, dorsal capsule; L, lunate; S, scaphoid.)
Postoperative Management
After surgery, we place a forearm splint, allowing mobility of the fingers and elbow. The stitches are removed 2 weeks after surgery; the forearm splint is maintained for up to 4 weeks, when we remove the Kirschner wire and place a removable wrist brace. The patient then begins a specific rehabilitation protocol.
Discussion
The SLL is a complex formed by an intrinsic component, which is the ligament itself, divided into 3 portions (volar, proximal, and dorsal), and an extrinsic component, formed by the radioscaphocapitate ligament, radiolunate ligament, dorsal radiocarpal ligament, dorsal intercarpal ligament, scapho-trapezium ligament, and DCSS.2, 12 The proximal portion is less important in scapholunate stability and consists of fibrocartilage tissue. Dorsal and volar portions are integrated with the corresponding ligaments and capsule.13
The dorsal portion of the SLL is the thickest and strongest part, and it is the most important portion in scapholunate stability.14 The DCSS forms part of the dorsal scapholunate complex, and recent studies have suggested its importance in stability function.2
The dorsal and volar portions are vascularized structures. The dorsal portion receives vascularization mainly through the dorsal capsuloligamentous union, whereas the volar portion receives it mainly through the radioscapholunate ligament or ligament of Testut.15 Therefore, these are portions of the ligament that have healing potential if they are repaired in the acute phase and if their vascular supply is not affected.
Classically, several open surgery techniques have been described for direct SLL repair in acute cases in which there is a repairable ligament. Through a dorsal approach, surgeons have performed direct suturing, performed transosseous suturing, or used bone anchors for the ligament reattachment. Satisfactory results have been published with these techniques.6, 7, 8
In addition to damage to the soft tissue with an increase in fibrosis and articular stiffness, the dorsal approach used in the treatment of scapholunate injuries almost always causes an injury to the PIN, which has an important role in the proprioception of the SLL and may result in the fundamental dynamic stability and functional recovery.11 Furthermore, during the approach and dorsal capsulotomy, the vascular supply of the scapholunate complex is affected, which also weakens the healing capacity of the injured ligament. Finally, the dorsal secondary stabilizers are also damaged in this surgical approach.16
The arthroscopic technique for SLL repair with capsular dorsal reinforcement has the advantage of avoiding injuries of the periarticular soft tissue and provides a dependable and stable primary repair of the dorsal portion of the ligament in cases of acute or subacute scapholunate injuries if there is enough tissue in good condition to be repaired (Table 3). The use of the 3-4, 6R, MCU, and MCR arthroscopic portals avoids injury of the PIN, minimizes damage to the dorsal vascular supply of the scapholunate complex, and avoids injury of the secondary stabilizers. All these aspects may permit the proper healing of the ligament after the primary repair, and this can be beneficial for the recovery of mobility and functioning of the wrist.
Table 3.
Pearls and Pitfalls
| The ideal candidates are patients with a partial or complete injury, either acute or early subacute (<3-4 wk). |
| The arthroscopic portals we use are the 3-4, 6R, MCU, and MCR portals. |
| From the 6R portal, we have the best view of the proximal and dorsal part of the SLL. |
| The cleaning of the fibers and scar material and the cruentation of the insertion of the SLL are important to stimulate healing. |
| It is mandatory that the tissue of the injured ligament is of good quality, allowing its repair. Non-acute cases may have friable tissue. |
| The 3-4 portal is used as the working portal, introducing the anchor and passing the sutures through the SLL. |
| In a small wrist, it is sometimes necessary to use the 4-5 portal as an accessory working portal. |
| Sometimes, to improve the scapholunate reduction, we need to use the Kirschner wires as a joystick, and sometimes one Kirschner wire between the radius and lunate is needed to maintain the radiolunate alignment. |
| We use a knot pusher, performing a sliding knot to reattach the ligament. The knot must not be cut. |
| To perform the dorsal arthroscopic capsulodesis, we pass one of the sutures through the SLL to the midcarpal joint, and we recover it through the MCR portal and through the subcutaneous space to the 3-4 portal. Then, we have to knot the sutures again to complete the dorsal plication. |
| When we have a complete SLL tear associated with a fracture, we must finish the intra-articular procedures first. Once we perform the dorsal capsulodesis, the 3-4 portal must not be used anymore because the dorsal plication can be damaged. |
MCR, midcarpal radial; MCU, midcarpal ulnar; SLL, scapholunate ligament.
The use of bone anchors for the repair and their location on the edge of the injury provide a higher resistance to the suture and the reinsertion. The association of a dorsal capsular reinforcement, which reconstructs the dorsal capsuloligamentous union, may increase the resistance and scapholunate stability.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
All-arthroscopic technique for direct repair of the injuries of the dorsal part of the scapholunate ligament by bone anchors complemented by arthroscopic dorsal capsular reinforcement. For this technique, we use the 3-4, 6R, midcarpal ulnar, and midcarpal radial arthroscopic portals. The arthroscopic technique for SLL repair with dorsal capsular reinforcement has the advantage of avoiding injuries to the periarticular soft tissue, and it provides a dependable and stable primary repair of the dorsal portion of the ligament in cases of acute or subacute scapholunate injuries.
References
- 1.Manuel J., Moran S.L. The diagnosis and treatment of scapholunate instability. Hand Clin. 2010;26:129–144. doi: 10.1016/j.hcl.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Overstraeten L.V., Camus E.J., Wahegaonkar A. Anatomical description of the dorsal capsulo-scapholunate septum (DCSS)—Arthroscopic staging of scapholunate instability after DCSS sectioning. J Wrist Surg. 2013;2:149–154. doi: 10.1055/s-0033-1338256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lindau T.R. The role of arthroscopy in carpal instability. J Hand Surg Eur. 2016;41:35–47. doi: 10.1177/1753193415616276. [DOI] [PubMed] [Google Scholar]
- 4.White N.J., Rollick N.C. Injuries of the scapholunate interosseous ligament: An update. J Am Acad Orthop Surg. 2015;23:691–703. doi: 10.5435/JAAOS-D-14-00254. [DOI] [PubMed] [Google Scholar]
- 5.Mathoulin C.L., Dauphin N., Wahegaonkar A.L. Arthroscopic dorsal capsuloligamentous repair in chronic scapholunate ligament tears. Hand Clin. 2011;27:563–572. doi: 10.1016/j.hcl.2011.07.003. xi. [DOI] [PubMed] [Google Scholar]
- 6.Kalainov M., Cohen M.S. Treatment of traumatic scapholunate dissociation. J Hand Surg Am. 2009;34:1317–1319. doi: 10.1016/j.jhsa.2009.03.019. [DOI] [PubMed] [Google Scholar]
- 7.Szabo R.M. Scapholunate ligament repair with capsulodesis reinforcement. J Hand Surg Am. 2008;33:1645–1654. doi: 10.1016/j.jhsa.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 8.Luchetti R., Atzei A., Cozzolino R., Fairplay T. Current role of open reconstruction of the scapholunate ligament. J Wrist Surg. 2013;2:116–125. doi: 10.1055/s-0033-1343092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berger R.A. The anatomy of the ligaments of the wrist and distal radioulnar joints. Clin Orthop Relat Res. 2001;(383):32–40. doi: 10.1097/00003086-200102000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Dubey P.P., Chauhan N.K., Siddiqui M.S., Verma A.K. Study of vascular supply of lunate and consideration applied to Kienbock disease. Hand Surg. 2011;16:9–13. doi: 10.1142/S021881041100500X. [DOI] [PubMed] [Google Scholar]
- 11.Hagert E., Persson J.K. Desensitizing the posterior interosseous nerve alters wrist proprioceptive reflexes. J Hand Surg Am. 2010;35:1059–1066. doi: 10.1016/j.jhsa.2010.03.031. [DOI] [PubMed] [Google Scholar]
- 12.Garcia-Elias M., Lluch A.L., Stanley J.K. Three-ligament tenodesis for the treatment of scapholunate dissociation: Indications and surgical technique. J Hand Surg Am. 2006;31:125–134. doi: 10.1016/j.jhsa.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 13.Binder A.C., Kerfant N., Wahegaonkar A.L., Tandara A.A., Mathoulin C.L. Dorsal wrist capsular tears in association with scapholunate instability: Results of an arthroscopic dorsal capsuloplasty. J Wrist Surg. 2013;2:160–167. doi: 10.1055/s-0032-1333426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sokolow C., Saffar P. Anatomy and histology of the scapholunate ligament. Hand Clin. 2001;17:77–81. [PubMed] [Google Scholar]
- 15.Hixson M.L., Stewart C. Microvascular anatomy of the radioscapholunate ligament of the wrist. J Hand Surg Am. 1990;15:279–282. doi: 10.1016/0363-5023(90)90108-4. [DOI] [PubMed] [Google Scholar]
- 16.Elsaidi G.A., Ruch D.S., Kuzma G.R., Smith B.P. Dorsal wrist ligament insertions stabilize the scapholunate interval: Cadaver study. Clin Orthop Relat Res. 2004;425:152–157. doi: 10.1097/01.blo.0000136836.78049.45. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
All-arthroscopic technique for direct repair of the injuries of the dorsal part of the scapholunate ligament by bone anchors complemented by arthroscopic dorsal capsular reinforcement. For this technique, we use the 3-4, 6R, midcarpal ulnar, and midcarpal radial arthroscopic portals. The arthroscopic technique for SLL repair with dorsal capsular reinforcement has the advantage of avoiding injuries to the periarticular soft tissue, and it provides a dependable and stable primary repair of the dorsal portion of the ligament in cases of acute or subacute scapholunate injuries.