Abstract
Introduction: We aimed to study the procedural characteristics, efficacy and safety of cryoballoon ablation (CBA) versus radiofrequency ablation (RFA) for catheter ablation of paroxysmal atrial fibrillation (AF).
Methods: A systematic literature search was performed using PubMed, EMBASE, Web of Science, and Cochrane Central Register of Controlled Trials to clinical trials comparing CBA and RFA for AF. Outcomes were evaluated for efficacy, procedure characteristics and safety. For each study, odd ratio (OR) and 95% confidence intervals (CIs) were calculated for endpoints for both approaches.
Results: We analyzed a total of 9,957 participants (3,369 in the CBA and 6,588 in RFA group) enrolled in 16 clinical trials. No significant difference was observed between CBA and RFA with regards to freedom from atrial arrhythmia at 12-months, recurrent atrial arrhythmias or repeat catheter ablation. CBA group had a significantly higher transient phrenic nerve injury (OR 14.19, 95% CI: 6.92-29.10; p<0.001) and persistent phrenic nerve injury (OR 4.62, 95% CI: 1.97-10.81; p<0.001); and a significantly lower pericardial effusion/cardiac tamponade (OR 0.43, 95% CI: 0.26-0.72; p=0.001), and groin site complications (OR 0.60, 95% CI: 0.38-0.93; p=0.02). No significant difference was observed in overall complications, stroke/thromboembolic events, major bleeding, and minor bleeding.
Conclusion: CBA was non-inferior to RFA for catheter ablation of paroxysmal AF. RF ablation was associated with a higher groin complications and pericardial effusion/cardiac tamponade, whereas CBA was associated with higher rates of transient and persistent phrenic nerve injury.
Keywords: Catheter Ablation, Cryoballoon, Radiofrequency, Atrial Fibrillation
Introduction
Approximately 2.7 to 6.1 million patients suffer from atrial fibrillation (AF) in USA.[1] The incidence rate has been estimated to be approximately 0.4%, which continues to grow with aging population, improvement in medical therapies and longer survival with heart disease.[2] Since Haïssaguerre's seminal observation identifying pulmonary veins as triggers for AF, there has been a dramatic increase in the number of patients undergoing catheter-based pulmonary vein isolation over the past 15 years.[3] In 2012, the Heart Rhythm Society/ European Heart Rhythm Association/ European Cardiac Arrhythmia Society issued a Class I recommendation for catheter ablation in patients with antiarrhythmic refractory symptomatic paroxysmal AF and class IIa recommendation in patients with symptomatic AF prior to initiating antiarrhythmic therapy.[4] Despite scientific advancements in mapping and catheters for radiofrequency (RF) ablation, data from multicenter registries have shown that only about 75% of patients with paroxysmal AF achieve durable maintenance of sinus rhythm.[3] These observations have catalyzed the development of alternative techniques and energy sources for catheter ablation with the aim of simplifying the procedure and improving outcomes. The conventional RF ablation using irrigated catheter has also evolved from its point-by-point approach to circumferential approach and now includes contact-sensing and phased duty-cycled RFA technology. A recent network meta-analysis by Kabunga et al explored the 3 most commonly used AF ablation strategies to compare outcomes of RFA using conventional irrigated catheter, phased duty-cycled RFA, and cryoballoon ablation (CBA). However, since their report, 7 additional prospective and randomized trials have been added to the literature comparing RFA and CBA. We aimed to compare the efficacy, procedural characteristics and complications of both the approaches and provide with the most updated evidence on this topic.
Methods
The present review was performed according to Cochrane Collaboration and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statements.
Search Strategy
We performed electronic searches on PubMed, The Cochrane Library, EMBASE, EBSCO, Web of Science and CINAHL databases from the inception through April 14, 2016 to identify trials comparing RFA and CBA in patients with paroxysmal AF. We combined the terms (“radiofrequency”) AND (“cryoballoon” OR “cryoablation”) AND (“atrial fibrillation”) as keywords or medical subject heading terms. All references of the retrieved articles were reviewed for further identification of potentially relevant studies. The identified studies were systematically assessed using the inclusion and exclusion criteria described below.
Eligibility Criteria
The eligibility criteria for our systematic review and meta-analysis included
Human subjects undergoing catheter ablation for paroxysmal AF using conventional RFA, CBA, or phase-duty cycled RFA.
Reported clinical outcomes, procedure time and complications.
Literature published in English.
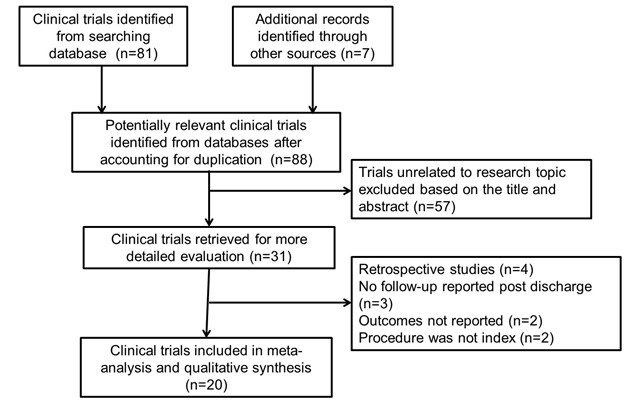
Either randomized controlled trials (RCTs) or prospective cohort studies. Studies that did not have randomized or matched cohorts were excluded. Retrospective studies, abstracts, case reports, conference presentations, editorials, reviews, and expert opinions were excluded. We used the longest available follow-up data from individual studies for our analysis. All the data was extracted and jadad score calculated independently by 2 reviewers (JG and RC). Discrepancies between the two reviewers were resolved by discussion and consensus. Final results were reviewed by senior investigator (AN) (Figure 1).
Figure 1. Process of study selection for randomized and prospective trials.
Outcomes
The primary efficacy outcome in our study was "freedom from any atrial arrhythmia at 12 months", "recurrent atrial arrhythmias", and "need for repeat ablation". Studies reporting only acute procedural success rates were excluded from efficacy analysis. Secondary procedural outcomes included “procedural time” and “fluoroscopy time”.
The primary safety outcome was the combined endpoint of “all-cause mortality”, “overall complications”, “stroke or thromboembolism event”, “major bleeding”, “minor bleeding”, “groin site complications (including arteriovenous fistulae, pseudoaneurysms and hematomas requiring any intervention or prolonged hospital stay)”, “transient phrenic nerve injury” (resolved immediate post-procedure), “persistent phrenic nerve injury”, “pericardial effusion or cardiac tamponade” (requiring intervention), “atrio-esophageal fistula”, and “pulmonary vein stenosis”. For analysis, the conventional and duty-phased RFA strategies for ablation were grouped together in the RFA group.
Statistical Analysis
Random effects model was used to estimate the odds ratio (OR) and respective 95% confidence intervals (CI) using Cochrane Collaborative software, RevMan 5.3. Measure of heterogeneity between the studies was assessed using the chi square test and was considered significant if I2>50%. All p values were 2-sided, and p value of <0.05 was considered significant.
Quality Appraisal And Publication Bias
Assessment of risk of bias for each selected study was performed according to PRISMA 2009 guidelines. Qualitative evaluation of bias using the following key parameters were performed for each study:
Clear definition of study population.
Clear definition of outcomes and outcome assessment.
Independent assessment of outcome parameters.
Sufficient duration of follow-up.
Selective loss during follow-up.
Important confounders and prognostic factors identified.
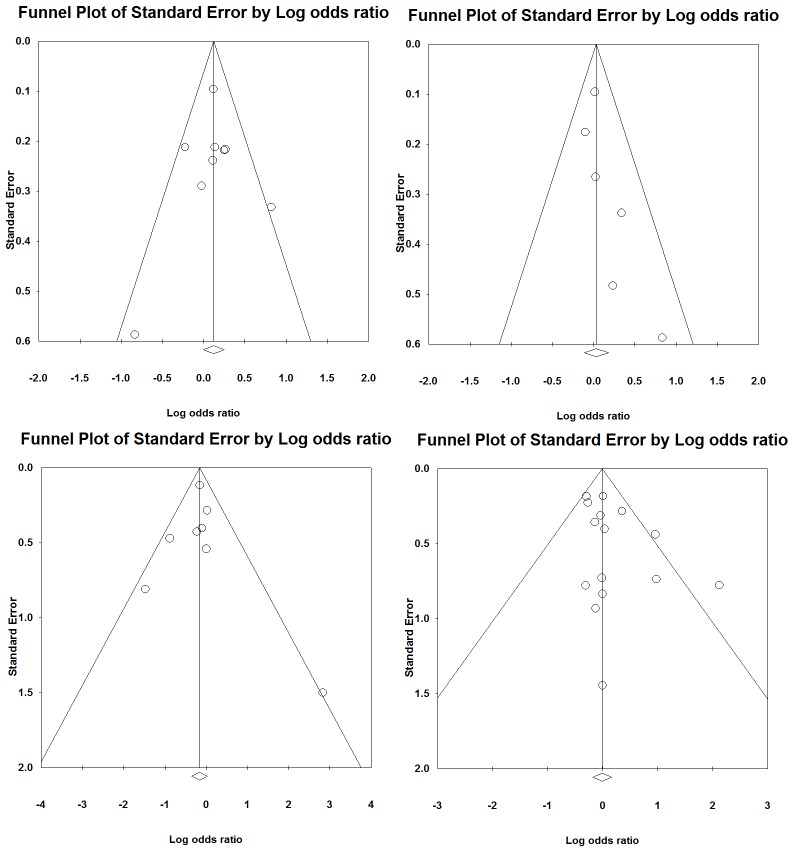
Evidence of publication bias was investigated visually using funnel plots and analyzed using Egger and Begg methods.
Results
A total of 88 studies were identified after exclusion of duplicate or irrelevant references (Figure 1). After a detailed evaluation of these studies, 16 relevant studies were included, that incorporated a total of 9,957 participants (3,369 in the CBA and 6,588 in RFA group) undergoing catheter ablation for paroxysmal AF. Of these, 5 were RCTs[5-9] and 11 were prospective observational studies.[11-20] The characteristics of these trials, mean follow-up periods and mode of arrhythmia detection are described in Table 1.
Table 1. Characteristics of the included studies.
CBA= Cryoballoon ablation; RFA= Radiofrequency ablation; RCT=Randomized Controlled trial; P;OS = Prospective Observational Study; CB-1 = Cryoballoon 1st generation; CB-2= Cryoballoon 2nd generation; NS=Not specified; C-IRF= Conventional Irrigated Radiofrequency catheter; PRF= Duty-cycled phased radiofrequency; CS-IRF=contact sensing-radiofrequency; PVI=Pulmonary Vein Isolation
| Name of Study | Year | Type of trial | Cryoballoon characteristics | CBA, n | Radiofrequency characteristics | RFA, n | Follow-up duration (mean, months) | Mode of follow-up for arrhythmia detection | Jadad Score | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Generation | Size | Type of RFA | Approach for ablation | ||||||||
| Kuck et al | 2016 | RCT | CB-1;CB-2 | 23 and 28 mm | 374 | C - IRF | point by point | 376 | 18 months | 24h Holter monitor | 3 |
| Hunter et al | 2015 | RCT | CB-1 | 23 and 28 mm | 78 | C - IRF | point by point | 77 | 12 months | 7 day Holter | 3 |
| Luik et al | 2015 | RCT | CB-1 | 23 and 28 mm | 156 | C-IRF | NS | 159 | 12 months | 7 day Holter or event recorder | 3 |
| Pérez-Castellano et al | 2014 | RCT | CB-1 | 23 or 28 mm | 25 | C-IRF | point by point | 25 | 12 months | Insertable cardiac monitor | 3 |
| Schmidt et al | 2013 | RCT | NS | 28 mm | 33 | C-IRF | NS | 33 | NS | NS | 3 |
| Khoueiry et al | 2016 | P; OS | CB-1; CB-2 | 28 mm | 311 | C-IRF and CS-IRF | Circumferential PVI | 376 | 14 months | 24h Holter monitor | NA |
| Schmidt et al | 2016 | P; OS | NS | 23 and 28 mm | 607 | C-IRF | NS | 1699 | 12 months | 12 lead ECG | NA |
| Straube et al | 2016 | P; OS | NS | 23 and 28 mm | 193 | C-IRF and CS-IRF | NS | 180 | 17 months | 24h Holter monitor | NA |
| Squara et al | 2015 | P; OS | CB-2 | 23 and 28 mm | 178 | CF-IRF | Circumferential PVI | 198 | 12 months | 24h Holter monitor | NA |
| Wasserlauf et al | 2015 | P; OS | CB-1; CB-2 | 23 and 28 mm | 101 | C-IRF | NS | 100 | 12 months | 24h to 48h Holter monitor | NA |
| Jourda et al | 2015 | P; OS | CB-2 | NS | 75 | CF-RFA | NS | 75 | 12 months | 24h Holter monitor | NA |
| Knecht et al | 2014 | P; OS | CB-1 | 23 or 28 mm | 71 | C-IRF | Circumferential PVI | 71 | 28 months | 7 day Holter | NA |
| Mugnai et al | 2014 | P; OS | CB-1 | 28 mm | 136 | C-IRF | Circumferential PVI | 260 | 23 months | 24h Holter monitor | NA |
| Schmidt et al | 2014 | P; OS | NS | 23 or 28 mm | 905 | C-IRF | NS | 2870 | NS | NS | NA |
| Gaita et al | 2011 | P; OS | CB-1 | 23 or 28 mm | 36 | C-IRF | point by point | 36 | NS | NS | NA |
| Kojodjojo et al | 2010 | P; OS | CB-1 | 28 mm | 90 | C-IRF | Circumferential PVI | 53 | 14 months | 24h Holter monitor | NA |
Quality Assessment And Publication Bias
Overall, there were clear definitions of the study population, outcomes, and assessment in most component studies, but blinded assessment of outcomes was not reported in all studies resulting in potential bias. Jadad score was calculated for all RCTs with a mean Jadad score of 3 indicating that the studies involved were of high quality (Table 1). No significant publication bias was observed using funnel plots (Egger’s test and Begg’s test had p values >0.05 for all analyses) (Supplementary appendix Table 1, Supplementary appendix, Figure 1).
Supplement Table 1. Summary of Egger’s and Begg’s test for publication bias.
P value of <0.05 indicates publication bias
| CBA versus RFA | Egger’s test p-value | Begg’s test p-value |
|---|---|---|
| Freedom from atrial fibrillation | 0.83 | 1.00 |
| Recurrent atrial arrhythmia | 0.12 | 0.06 |
| Repeat ablation | 0.97 | 0.71 |
| Overall complications | 0.09 | 0.48 |
Supplementary Figure 1. Funnel plots evaluating publication bias in all studies: a) Freedom from atrial arrhythmias at 12 months; b) Recurrent atrial arrhythmias; c) Repeat ablation within 12 months since index ablation; d) Overall acute complications.
Baseline Characteristics
In the participant studies, there were no significant differences between the two groups in terms of age, gender, body mass index, left ventricular ejection fraction (LVEF), hypertension or coronary artery disease. A higher prevalence of diabetes was observed (p<0.05) in CBA group whereas left atrial diameter (LAD) and stroke or thromboembolic events were significantly greater in patients with RFA group. No significant heterogeneity was observed for stroke and diabetes. However, a significant heterogeneity was observed in LAD (Table 2). On sub-analysis of LAD only in prospective trials, the standard mean difference was found to be -0.13 (95% CI -0.26 to -0.001; p=0.04) with no significant heterogeneity (I2=1.05).
Table 2. Baseline demographics of study population.
CBA=Cryoballoon ablation; RFA=Radiofrequency Ablation; RR=Relative Risk; SWD=Standardized Mean Difference; LVEF= Left Ventricular Ejection Fraction; BMI=Body-mass index; LAD= Left atrial diameter; TIA=Transient Ischemic Attack; CAD=Coronary artery disease
| Baseline Characteristic | CBA | RFA | N | Studies (n) | RR or SWD (95% CI) | Heterogeneity | P for overall effect | |
|---|---|---|---|---|---|---|---|---|
| P value | I2 (%) | |||||||
| Age, yrs | 59.2 | 60.1 | 3,138 | 11 | -0.08 (-0.19 to 0.03) | 0.01 | 53.3 | 0.14 |
| Males, % | 70.3% | 70.5% | 6,411 | 15 | 0.99 (0.97 to 1.03) | 0.53 | 0 | 0.91 |
| BMI | 27.0 | 26.7 | 2,125 | 5 | 0.05 (-0.12 to 0.22) | 0.007 | 71.6 | 0.58 |
| LVEF, % | 60.6% | 60.0% | 1,687 | 7 | 0.04 (-0.12 to 0.21) | 0.02 | 57.8 | 0.58 |
| LAD, mm | 40.4 | 41.1 | 5,315 | 7 | -0.18(-0.32 to -0.05) | 0.01 | 61.6 | 0.008 |
| Stroke/TIA, % | 4.9% | 7.7% | 502 | 10 | 0.77 (0.63 to 0.93) | 0.61 | 0 | 0.008 |
| Hypertension, % | 46.8% | 48.1% | 5,337 | 16 | 0.96 (0.90 to 1.03) | 0.02 | 44.9 | 0.24 |
| Diabetes, % | 7.4% | 6.5% | 718 | 14 | 1.17 (1.01 to 1.36) | 0.58 | 0 | 0.04 |
| CAD, % | 11.9% | 13.6% | 1,219 | 8 | 0.93 (0.82 to 1.04) | 0.6 | 0 | 0.21 |
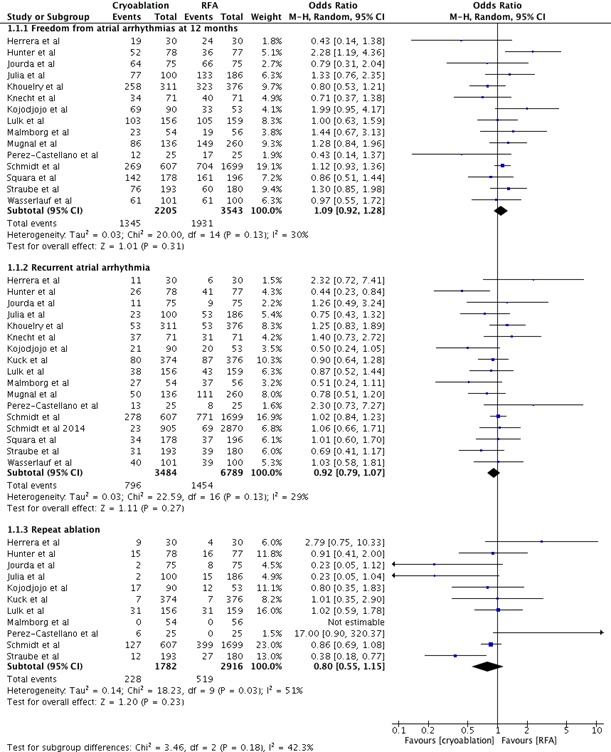
Assessment of Efficacy
The clinical outcomes were assessed off anti-arrhythmic therapy in 7 trials,[5-08,14-16] on anti-arrhythmic therapy in 4 trials[10-12,18] and this information was not available for 5 trials.[9,13,17,19,20] No significant difference was observed between CBA and RFA in freedom from atrial arrhythmia at 12-months follow-up (OR 1.13; 95% confidence interval [CI]: 0.96-1.33), recurrent atrial arrhythmias (OR 1.03; 95% CI 0.89-1.20) or repeat ablation (OR 0.83; 95% CI 0.61-1.12) (Figure 2). No significant heterogeneity was observed.
Figure 2. Forest plot demonstrating primary efficacy outcomes in patients with atrial fibrillation undergoing cryoablation versus radiofrequency ablation.
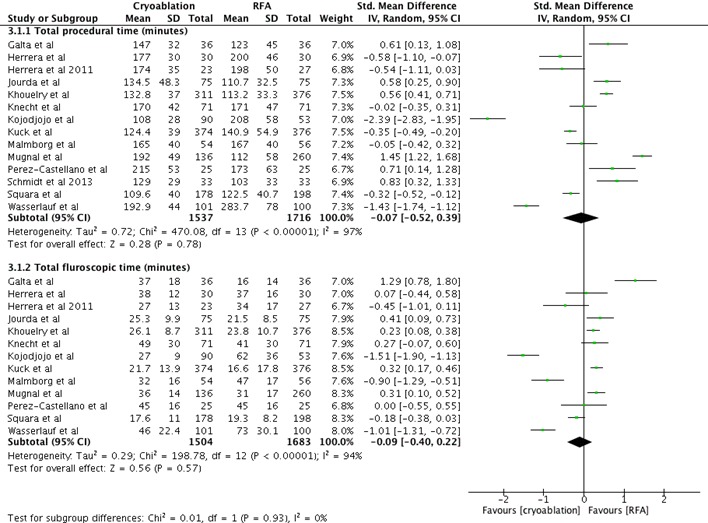
Assessment of Procedural Duration
The total procedure time was not significantly different between CBA and RFA groups (Standard mean difference [SMD] 0.02, 95% CI -0.52 to 0.55; I2=98%). Similarly, the total fluoroscopy time was not significantly different between the two groups (SMD 0.01, 95% CI -0.34 to 0.35; I2=95%) (Figure 3). Significant heterogeneity was observed in both these measures.
Figure 3. Forest plot demonstrating procedural outcomes of cryoablation versus radiofrequency ablation.
Assessment of Safety and Complications
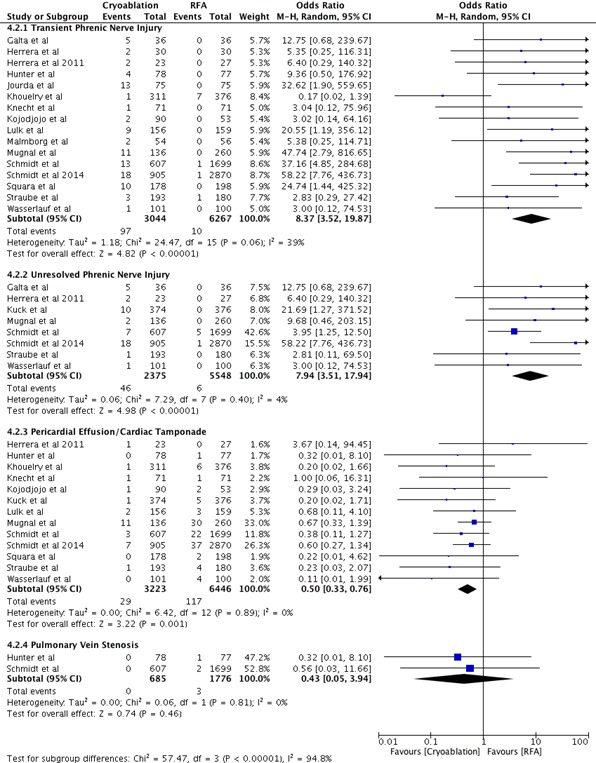
The all-cause mortality (OR 0.99, 95% CI 0.07-14.75; I2=55%) for CBA and RFA respectively, Figure 4) and overall complications (7.5% vs. 6.9% for CBA and RFA respectively, (OR 1.06, 95% CI 0.84-1.34; I2=31%) p=0.62; Figure 5a) were not significantly different. Among individual complications, CBA group had significantly lower groin site complications (1.35% vs. 1.74%, p=0.02; OR 0.60, 95% CI 0.38 - 0.93) and lower hemodynamically significant pericardial effusion/cardiac tamponade (0.56% vs. 1.37%, p=0.001), as compared to RFA respectively, higher rates of transient phrenic nerve injury (3% vs. 0.06%, p<0.001; OR 14.19, 95% CI 6.92-29.10) and persistent phrenic nerve injury (1.24% vs. 0.17%, p<0.001; OR 4.62, 95% CI 1.97-10.81) a for CBA and RFA respectively. No significant difference was observed in stroke/thromboembolic events, major bleeding, and minor bleeding (Figure 5a and b). There were no reports of atrio-esophageal fistula or pulmonary vein stenosis.
Figure 4. Forest plot demonstrating all-cause mortality in patients with atrial fibrillation undergoing cryoablation versus radiofrequency ablation.
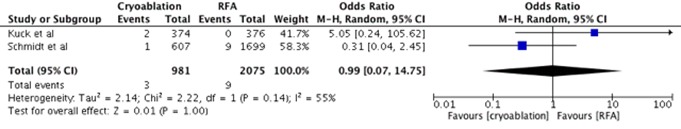
Figure 5A. Forest plot demonstrating safety outcomes - overall acute complications, stroke/thromboembolism, major bleeding, minor bleeding and groin site complications in patients with atrial fibrillation undergoing cryoablation versus radiofrequency ablation.
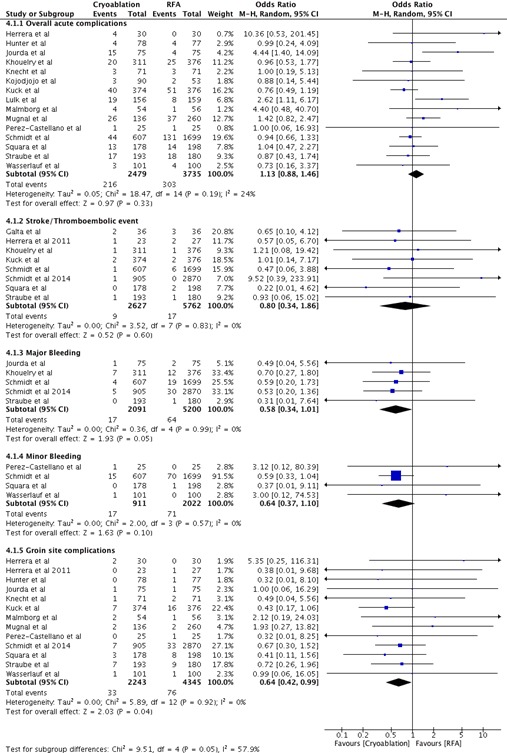
Figure 5B. Forest plot demonstrating safety outcomes - transient and unresolved phrenic nerve injury, pericardial effusion/tamponade and pulmonary vein stenosis in patients with atrial fibrillation undergoing cryoablation versus radiofrequency ablation.
Analysis of Data from Randomized Controlled Trials Only
Assessment of Efficacy
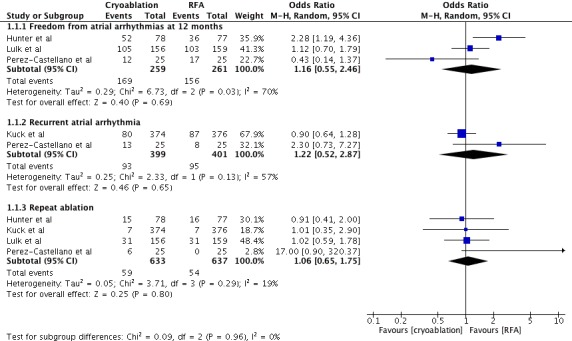
Cryoablation and Radiofrequency ablation had comparable rates of freedom from atrial arrhythmia (OR: 1.16, 95% CI: 0.55-2.46; I2=70%), recurrent atrial arrhythmias (OR: 1.22, 95% CI: 0.52-2.87; I2=57%) and need for a repeat ablation (OR: 1.06, 95% CI: 0.65-1.75; I2=19) (Supplementary appendix, Figure 2).
Supplementary Figure 2. Forest plot demonstrating primary efficacy endpoints (randomized controlled trials only) in patients with atrial fibrillation undergoing cryoablation versus radiofrequency ablation.
Assessment of Procedural Duration
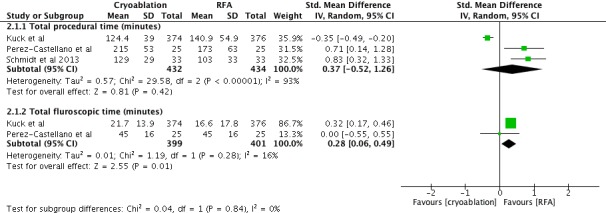
Cryoablation group was associated with increased total fluoroscopy time (Standard mean difference 0.28, 95% CI: 0.06 - 0.49; I2=16%) and similar total procedural time (Standard mean difference: 0.37; 95% CI: -0.52 – 1.26; I2=93%) compared to RFA group (Supplementary appendix, Figure 3).
Supplementary Figure 3. Forest plot demonstrating procedural outcomes (randomized controlled trials only) in patients with atrial fibrillation undergoing cryoablation versus radiofrequency ablation.
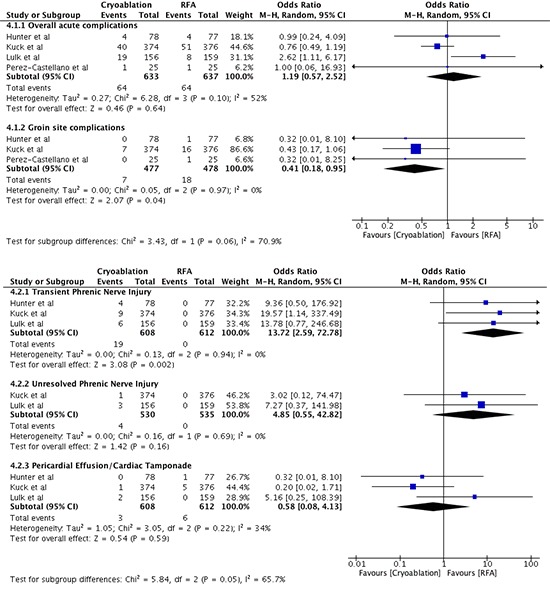
Assessment of Safety and Complications
The overall complications were similar in both the groups (10.11% versus 10.04%; OR: 1.19, 95% CI 0.57-2.52). Among individual complications, CBA group had significantly lower groin site complications (1.46% versus 3.76% for RFA group; OR: 0.41, 95% CI 0.18 – 0.95) and higher rates of transient phrenic nerve injury (3.1% versus 0 events in RFA group; OR 13.72, 95% CI 2.59 – 72.78) compared to RFA group. No significant difference was observed in unresolved phrenic nerve injury and significant pericardial effusion/cardiac tamponade between the two groups (Supplementary appendix, Figure 4).
Supplementary Figure 4. Forest plot demonstrating safety outcomes (randomized controlled trials only) - overall acute complications, groin site complications, transient and unresolved phrenic nerve injury and pericardial effusion/tamponade in patients with atrial fibrillation undergoing cryoablation versus radiofrequency ablation.
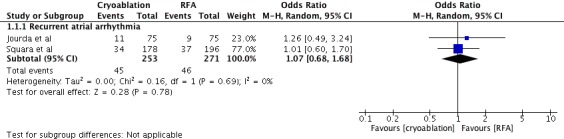
Analysis of Data from Trials Evaluating 2nd Generation CBA and Contact-Force RFA
In the sub-analysis, evaluating 2nd generation CBA (CBA-2) and RFA using contact force-sensing (CF-RFA) catheters, only 2 trials were included.[13,15] In these trials both groups had comparable rates of recurrent atrial arrhythmias (17.8% versus 17%; OR 1.07, 95% CI 0.68 – 1.68) ( appendix, Figure 5).
Supplementary Figure 5. Forest plot demonstrating primary efficacy endpoints in studies evaluating 2nd generation CBA catheter versus contact-sensing RFA catheter.
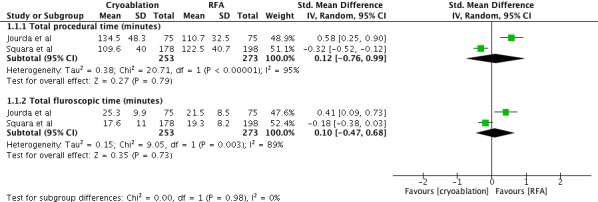
Cryoablation was associated with similar total procedural time (Standard mean difference: 0.12; 95% CI: -0.76 - 0.99; I2=95%) and total fluoroscopy time (Standard mean difference: 0.10; 95% CI: -0.47 - 0.68; I2=89%) as RFA (Supplementary appendix, Figure 6).
Supplementary Figure 6. Forest plot demonstrating procedural outcomes in studies evaluating 2nd generation CBA catheter versus contact-sensing RFA catheter.
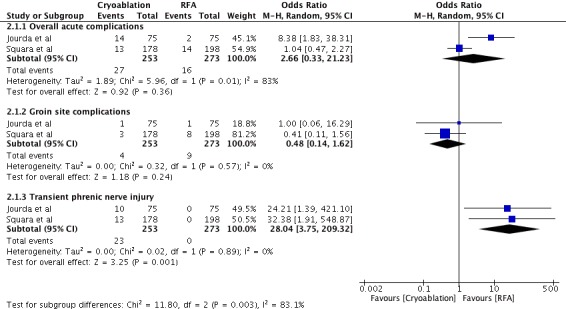
The overall complications were similar in both the groups (10.6% versus 5.8%; OR 2.66, 95% CI 0.33 – 21.23, I2=83%). CBA group (2nd generation) had higher rates of transient phrenic nerve injury (9% versus 0 events in RFA group; OR 28.04, 95% CI 3.75 – 209.32) as compare to RFA group. No difference was observed in groin site complications (1.6% versus 3.2%; OR 0.48, 95% CI 0.14 – 1.62) between the two groups (Supplementary appendix, Figure 7).
Supplementary Figure 7. Forest plot demonstrating safety outcomes – overall acute complications, groin site complications and transient phrenic nerve injury in studies evaluating 2nd generation CBA catheter and contact-sensing RFA catheter.
Discussion
To the best of our knowledge, this is the largest meta-analysis of prospective and RCTs comparing the overall efficacy, safety and procedural characteristics of CBA with RFA in patients with paroxysmal AF. Our analysis suggests that CBA and RFA do not differ in terms of efficacy, procedural times, and overall complications. However, the analysis of individual complications demonstrated increased incidence of transient and persistent phrenic nerve injury and reduced hemodynamically significant pericardial effusion/cardiac tamponade and groin site complications with CBA as compared to RFA. No significant difference was observed in rates of major and minor bleeding and stroke/thromboembolic events. Interestingly there were no reports of atrio-esophageal fistula and pulmonary vein stenosis in both groups.
Freedom from Atrial Arrhythmia
Our study demonstrated no difference between CBA and RFA in rates of freedom from atrial arrhythmias at 12 months follow-up, recurrent atrial arrhythmias and repeat ablations. Traditionally, point-by-point ablation is expected to have gaps in ablation lines and hence more recurrence compared to the “single-shot” approach offered by CBA.[21] Improved outcomes have been reported with RFA since the introduction of contact force-sensing catheter technology.[22] However, this modality was not used consistently in our component studies and pooled together with traditional RFA (Table 1). Hanninen et al have previously reported a higher incidence of recurrent arrhythmia with CBA compared to RFA, especially atrioventricular nodal reentrant tachycardia.[23] There have been two prior meta-analyses on this subject by Xu et al[24] and Kabunga et al.[25] We only included prospective and RCTs in our analysis as opposed to the prior meta-analyses, and incorporated data from 7 additional contemporary trials since the last meta-analysis. Our data did not detect any evidence of superiority in efficacy with either of the two modalities. Even after restricting the analysis to RCTs, no difference in the primary efficacy endpoints was observed between the two groups. Subgroup-analysis comparing the 2nd generation CBA with contact force-sensing RFA also demonstrated no significant difference in the primary efficacy end-points between the two groups (although results should be interpreted with caution in view of only 2 trials).
Procedural Characteristics
Contrary to the findings from prior meta-analyses by Xu et al[24] and Kabunga et al,[25] we found no significant difference in procedural characteristics including total procedural duration and fluoroscopy time. However, this needs to be interpreted with caution as a significant heterogeneity was observed in both these outcomes. The grouping of different techniques of RFA and different generations of CBA catheters could be a possible contributor to the significant heterogeneity observed in the participant studies.
Upon separate analysis of only the RCTs, there was reduced total fluoroscopic times in RFA group as compared to CBA group with no significant heterogeneity. The longer fluoroscopy times may be related to the impact of a learning curve for CBA. A steep learning curve with CBA has been shown in a large single center study even at a later stage in well-experienced center.[26] In the trials comparing only 2nd generation CBA catheters with contact-sense RFA catheters, no difference was observed, although significant heterogeneity persisted. This could possibly be due to local variations in experience and varied preferences in ablation technique.
Secondary Safety Outcomes and Associated Complications
Overall complications rate observed was similar to registry data previously reported by Deshmukh et al[27] and Cappato et al.[3] Although no significant difference in overall complications was observed between the two groups, it is imperative to discuss the pattern of individual complications observed with the two approaches. Higher incidence of groin-site complications were seen with RFA as compared to CBA with the effect persisting in the sub-analysis with RCTs. This can potentially be explained by increased groin injuries, which may be caused by the two-sheath system often used with RFA (a radiofrequency catheter and a separate mapping catheter).[28,29] Unfortunately, the included studies did not mention the number of sheaths used during the procedure to better quantify the role of this effect.
Additionally an increased incidence of hemodynamically significant pericardial effusion/cardiac tamponade was observed in the RFA group. However no difference was observed in the subgroup analysis for RCTs only. A total of 12 trials reported this complication[5-7,10,11,13,14,16-18,20] of which 3 were RCT’s.[5-7] Number of transeptal punctures is a major factor contributing to development of cardiac tamponade or significant pericardial effusion.[30] In 6 trials, the use of a single or double transeptal puncture was not specified[5,7,11,13,14,18] a double transeptal puncture approach was performed in 2 trials[16,20] and a single transeptal puncture for CBA and double for RFA was performed in 4 trials.[6,10,12,17] The use of double transeptal puncture approach with RFA could have likely contributed to an increased incidence of cardiac tamponade in this group. However similar results were not observed in the subgroup analysis (RCT’s only). This could be potentially due to the use of double transeptal approach in majority patients in both CBA and RFA groups (although this was not specified in the RCTs).
Cryoablation was predominantly complicated by transient and unresolved phrenic nerve injury. One of the potential reasons for this association could be from the forward pressure exerted during CBA with the sheath for achieving a satisfactory circumferential seal around the target pulmonary vein. This motion likely pushes the atrium closer to surrounding structures including the phrenic nerve. Majority of phrenic nerve injuries were transient and spontaneously resolved with progression of approximately 1.3% injuries to persistent phrenic nerve injury at 12 months.[31,32]
Study Limitations
Potential sources of bias in our study include combination of 1st and 2nd generation CBA catheters into one group and different approaches of RFA in a single group (irrigated catheters, contact force-sensing catheters and duty-cycled phased RFA) and inclusion of data from prospective non-randomized trials. Additionally, there was a lack of uniformity in the participant trials in protocol for detection of recurrent AF; specifically, the follow-up periods, mode of arrhythmia detection, inclusion of patients on anti-arrhythmic therapy for assessment of efficacy outcomes. We tried to eliminate some of these biases by performing a sub-analysis of RCTs, which demonstrated results similar to original analysis with both groups showing similar efficacy, procedural characteristics, and complications profile.
Conclusions
Our analysis demonstrates that the two technologies for catheter ablation of AF are equivalent in efficacy, procedural characteristics and overall complications with higher rates of groin site complications and significant pericardial effusion/cardiac tamponade in the RFA group and phrenic nerve injury in the CBA group. Based on these data, we believe that currently, there is insufficient evidence to suggest superiority of one ablation strategy over the other for pulmonary vein isolation. Our study highlights the need for better technologies that would help us achieve a more efficient and durable pulmonary vein isolation.
Disclosures
None.
References
- 1.January Craig T, Wann L Samuel, Alpert Joseph S, Calkins Hugh, Cigarroa Joaquin E, Cleveland Joseph C, Conti Jamie B, Ellinor Patrick T, Ezekowitz Michael D, Field Michael E, Murray Katherine T, Sacco Ralph L, Stevenson William G, Tchou Patrick J, Tracy Cynthia M, Yancy Clyde W. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J. Am. Coll. Cardiol. 2014 Dec 02;64 (21):e1–76. doi: 10.1016/j.jacc.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 2.Colilla Susan, Crow Ann, Petkun William, Singer Daniel E, Simon Teresa, Liu Xianchen. Estimates of current and future incidence and prevalence of atrial fibrillation in the U.S. adult population. Am. J. Cardiol. 2013 Oct 15;112 (8):1142–7. doi: 10.1016/j.amjcard.2013.05.063. [DOI] [PubMed] [Google Scholar]
- 3.Cappato Riccardo, Calkins Hugh, Chen Shih-Ann, Davies Wyn, Iesaka Yoshito, Kalman Jonathan, Kim You-Ho, Klein George, Natale Andrea, Packer Douglas, Skanes Allan, Ambrogi Federico, Biganzoli Elia. Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ Arrhythm Electrophysiol. 2010 Feb;3 (1):32–8. doi: 10.1161/CIRCEP.109.859116. [DOI] [PubMed] [Google Scholar]
- 4.Calkins Hugh, Kuck Karl Heinz, Cappato Riccardo, Brugada Josep, Camm A John, Chen Shih-Ann, Crijns Harry J G, Damiano Ralph J, Davies D Wyn, DiMarco John, Edgerton James, Ellenbogen Kenneth, Ezekowitz Michael D, Haines David E, Haissaguerre Michel, Hindricks Gerhard, Iesaka Yoshito, Jackman Warren, Jalife Jose, Jais Pierre, Kalman Jonathan, Keane David, Kim Young-Hoon, Kirchhof Paulus, Klein George, Kottkamp Hans, Kumagai Koichiro, Lindsay Bruce D, Mansour Moussa, Marchlinski Francis E, McCarthy Patrick M, Mont J Lluis, Morady Fred, Nademanee Koonlawee, Nakagawa Hiroshi, Natale Andrea, Nattel Stanley, Packer Douglas L, Pappone Carlo, Prystowsky Eric, Raviele Antonio, Reddy Vivek, Ruskin Jeremy N, Shemin Richard J, Tsao Hsuan-Ming, Wilber David. 2012 HRS/EHRA/ECAS Expert Consensus Statement on Catheter and Surgical Ablation of Atrial Fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design. Europace. 2012 Apr;14 (4):528–606. doi: 10.1093/europace/eus027. [DOI] [PubMed] [Google Scholar]
- 5.Kuck Karl-Heinz, Brugada Josep, Fürnkranz Alexander, Metzner Andreas, Ouyang Feifan, Chun K R Julian, Elvan Arif, Arentz Thomas, Bestehorn Kurt, Pocock Stuart J, Albenque Jean-Paul, Tondo Claudio. Cryoballoon or Radiofrequency Ablation for Paroxysmal Atrial Fibrillation. N. Engl. J. Med. 2016 Jun 09;374 (23):2235–45. doi: 10.1056/NEJMoa1602014. [DOI] [PubMed] [Google Scholar]
- 6.Hunter Ross J, Baker Victoria, Finlay Malcolm C, Duncan Edward R, Lovell Matthew J, Tayebjee Muzahir H, Ullah Waqas, Siddiqui M Shoaib, McLEAN Ailsa, Richmond Laura, Kirkby Claire, Ginks Matthew R, Dhinoja Mehul, Sporton Simon, Earley Mark J, Schilling Richard J. Point-by-Point Radiofrequency Ablation Versus the Cryoballoon or a Novel Combined Approach: A Randomized Trial Comparing 3 Methods of Pulmonary Vein Isolation for Paroxysmal Atrial Fibrillation (The Cryo Versus RF Trial). J. Cardiovasc. Electrophysiol. 2015 Dec;26 (12):1307–14. doi: 10.1111/jce.12846. [DOI] [PubMed] [Google Scholar]
- 7.Luik Armin, Radzewitz Andrea, Kieser Meinhard, Walter Marlene, Bramlage Peter, Hörmann Patrick, Schmidt Kerstin, Horn Nicolas, Brinkmeier-Theofanopoulou Maria, Kunzmann Kevin, Riexinger Tobias, Schymik Gerhard, Merkel Matthias, Schmitt Claus. Cryoballoon Versus Open Irrigated Radiofrequency Ablation in Patients With Paroxysmal Atrial Fibrillation: The Prospective, Randomized, Controlled, Noninferiority FreezeAF Study. Circulation. 2015 Oct 06;132 (14):1311–9. doi: 10.1161/CIRCULATIONAHA.115.016871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pérez-Castellano Nicasio, Fernández-Cavazos Roberto, Moreno Javier, Cañadas Victoria, Conde Asunción, González-Ferrer Juan J, Macaya Carlos, Pérez-Villacastín Julián. The COR trial: a randomized study with continuous rhythm monitoring to compare the efficacy of cryoenergy and radiofrequency for pulmonary vein isolation. Heart Rhythm. 2014 Jan;11 (1):8–14. doi: 10.1016/j.hrthm.2013.10.014. [DOI] [PubMed] [Google Scholar]
- 9.Schmidt Boris, Gunawardene Melanie, Krieg Detlef, Bordignon Stefano, Fürnkranz Alexander, Kulikoglu Mehmet, Herrmann Wilfried, Chun K R Julian. A prospective randomized single-center study on the risk of asymptomatic cerebral lesions comparing irrigated radiofrequency current ablation with the cryoballoon and the laser balloon. J. Cardiovasc. Electrophysiol. 2013 Aug;24 (8):869–74. doi: 10.1111/jce.12151. [DOI] [PubMed] [Google Scholar]
- 10.Khoueiry Z, Albenque J-P, Providencia R, Combes S, Combes N, Jourda F, Sousa P A, Cardin C, Pasquie J-L, Cung T T, Massin F, Marijon E, Boveda S. Outcomes after cryoablation vs. radiofrequency in patients with paroxysmal atrial fibrillation: impact of pulmonary veins anatomy. Europace. 2016 Sep;18 (9):1343–51. doi: 10.1093/europace/euv419. [DOI] [PubMed] [Google Scholar]
- 11.Schmidt Martin, Dorwarth Uwe, Andresen Dietrich, Brachmann Johannes, Kuck Karlheinz, Kuniss Malte, Willems Stephan, Deneke Thomas, Tebbenjohanns Jürgen, Gerds-Li Jin-Hong, Spitzer Stefan, Senges Jochen, Hochadel Matthias, Hoffmann Ellen. German ablation registry: Cryoballoon vs. radiofrequency ablation in paroxysmal atrial fibrillation--One-year outcome data. Heart Rhythm. 2016 Apr;13 (4):836–44. doi: 10.1016/j.hrthm.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 12.Straube Florian, Dorwarth Uwe, Ammar-Busch Sonia, Peter Timo, Noelker Georg, Massa Thomas, Kuniss Malte, Ewertsen Niels Christian, Chun Kyoung Ryul Julian, Tebbenjohanns Juergen, Tilz Roland, Kuck Karl Heinz, Ouarrak Taoufik, Senges Jochen, Hoffmann Ellen. First-line catheter ablation of paroxysmal atrial fibrillation: outcome of radiofrequency vs. cryoballoon pulmonary vein isolation. Europace. 2016 Mar;18 (3):368–75. doi: 10.1093/europace/euv271. [DOI] [PubMed] [Google Scholar]
- 13.Squara Fabien, Zhao Alexandre, Marijon Eloi, Latcu Decebal Gabriel, Providencia Rui, Di Giovanni Giacomo, Jauvert Gaël, Jourda Francois, Chierchia Gian-Battista, De Asmundis Carlo, Ciconte Giuseppe, Alonso Christine, Grimard Caroline, Boveda Serge, Cauchemez Bruno, Saoudi Nadir, Brugada Pedro, Albenque Jean-Paul, Thomas Olivier. Comparison between radiofrequency with contact force-sensing and second-generation cryoballoon for paroxysmal atrial fibrillation catheter ablation: a multicentre European evaluation. Europace. 2015 May;17 (5):718–24. doi: 10.1093/europace/euv060. [DOI] [PubMed] [Google Scholar]
- 14.Wasserlauf Jeremiah, Pelchovitz Daniel J, Rhyner John, Verma Nishant, Bohn Martha, Li Zhi, Arora Rishi, Chicos Alexandru B, Goldberger Jeffrey J, Kim Susan S, Lin Albert C, Knight Bradley P, Passman Rod S. Cryoballoon versus radiofrequency catheter ablation for paroxysmal atrial fibrillation. Pacing Clin Electrophysiol. 2015 Apr;38 (4):483–9. doi: 10.1111/pace.12582. [DOI] [PubMed] [Google Scholar]
- 15.Jourda François, Providencia Rui, Marijon Eloi, Bouzeman Abdeslam, Hireche Hassiba, Khoueiry Ziad, Cardin Christelle, Combes Nicolas, Combes Stéphane, Boveda Serge, Albenque Jean-Paul. Contact-force guided radiofrequency vs. second-generation balloon cryotherapy for pulmonary vein isolation in patients with paroxysmal atrial fibrillation-a prospective evaluation. Europace. 2015 Feb;17 (2):225–31. doi: 10.1093/europace/euu215. [DOI] [PubMed] [Google Scholar]
- 16.Knecht Sven, Sticherling Christian, von Felten Stefanie, Conen David, Schaer Beat, Ammann Peter, Altmann David, Osswald Stefan, Kühne Michael. Long-term comparison of cryoballoon and radiofrequency ablation of paroxysmal atrial fibrillation: a propensity score matched analysis. Int. J. Cardiol. 2014 Oct 20;176 (3):645–50. doi: 10.1016/j.ijcard.2014.06.038. [DOI] [PubMed] [Google Scholar]
- 17.Mugnai Giacomo, Chierchia Gian-Battista, de Asmundis Carlo, Sieira-Moret Juan, Conte Giulio, Capulzini Lucio, Wauters Kristel, Rodriguez-Mañero Moises, Di Giovanni Giacomo, Baltogiannis Giannis, Ciconte Giuseppe, Saitoh Yukio, Juliá Justo, Brugada Pedro. Comparison of pulmonary vein isolation using cryoballoon versus conventional radiofrequency for paroxysmal atrial fibrillation. Am. J. Cardiol. 2014 May 01;113 (9):1509–13. doi: 10.1016/j.amjcard.2014.01.425. [DOI] [PubMed] [Google Scholar]
- 18.Schmidt Martin, Dorwarth Uwe, Andresen Dietrich, Brachmann Johannes, Kuck Karl-Heinz, Kuniss Malte, Lewalter Thorsten, Spitzer Stefan, Willems Stephan, Senges Jochen, Jünger Claus, Hoffmann Ellen. Cryoballoon versus RF ablation in paroxysmal atrial fibrillation: results from the German Ablation Registry. J. Cardiovasc. Electrophysiol. 2014 Jan;25 (1):1–7. doi: 10.1111/jce.12267. [DOI] [PubMed] [Google Scholar]
- 19.Gaita Fiorenzo, Leclercq Jean François, Schumacher Burghard, Scaglione Marco, Toso Elisabetta, Halimi Franck, Schade Anja, Froehner Steffen, Ziegler Volker, Sergi Domenico, Cesarani Federico, Blandino Alessandro. Incidence of silent cerebral thromboembolic lesions after atrial fibrillation ablation may change according to technology used: comparison of irrigated radiofrequency, multipolar nonirrigated catheter and cryoballoon. J. Cardiovasc. Electrophysiol. 2011 Sep;22 (9):961–8. doi: 10.1111/j.1540-8167.2011.02050.x. [DOI] [PubMed] [Google Scholar]
- 20.Kojodjojo Pipin, O'Neill Mark D, Lim Phang Boon, Malcolm-Lawes Louisa, Whinnett Zachary I, Salukhe Tushar V, Linton Nicholas W, Lefroy David, Mason Anthony, Wright Ian, Peters Nicholas S, Kanagaratnam Prapa, Davies D Wyn. Pulmonary venous isolation by antral ablation with a large cryoballoon for treatment of paroxysmal and persistent atrial fibrillation: medium-term outcomes and non-randomised comparison with pulmonary venous isolation by radiofrequency ablation. Heart. 2010 Sep;96 (17):1379–84. doi: 10.1136/hrt.2009.192419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chae Sanders, Oral Hakan, Good Eric, Dey Sujoya, Wimmer Alan, Crawford Thomas, Wells Darryl, Sarrazin Jean-Francois, Chalfoun Nagib, Kuhne Michael, Fortino Jackie, Huether Elizabeth, Lemerand Tammy, Pelosi Frank, Bogun Frank, Morady Fred, Chugh Aman. Atrial tachycardia after circumferential pulmonary vein ablation of atrial fibrillation: mechanistic insights, results of catheter ablation, and risk factors for recurrence. J. Am. Coll. Cardiol. 2007 Oct 30;50 (18):1781–7. doi: 10.1016/j.jacc.2007.07.044. [DOI] [PubMed] [Google Scholar]
- 22.Jarman Julian W E, Panikker Sandeep, DAS Moloy, Wynn Gareth J, Ullah Waqas, Kontogeorgis Andrianos, Haldar Shouvik K, Patel Preya J, Hussain Wajid, Markides Vias, Gupta Dhiraj, Schilling Richard J, Wong Tom. Relationship between contact force sensing technology and medium-term outcome of atrial fibrillation ablation: a multicenter study of 600 patients. J. Cardiovasc. Electrophysiol. 2015 Apr;26 (4):378–84. doi: 10.1111/jce.12606. [DOI] [PubMed] [Google Scholar]
- 23.Hanninen Mikael, Yeung-Lai-Wah Nicole, Massel David, Gula Lorne J, Skanes Allan C, Yee Raymond, Klein George J, Manlucu Jaimie, Leong-Sit Peter. Cryoablation versus RF ablation for AVNRT: A meta-analysis and systematic review. J. Cardiovasc. Electrophysiol. 2013 Dec;24 (12):1354–60. doi: 10.1111/jce.12247. [DOI] [PubMed] [Google Scholar]
- 24.Xu Junxia, Huang Yingqun, Cai Hongbin, Qi Yue, Jia Nan, Shen Weifeng, Lin Jinxiu, Peng Feng, Niu Wenquan. Is cryoballoon ablation preferable to radiofrequency ablation for treatment of atrial fibrillation by pulmonary vein isolation? A meta-analysis. PLoS ONE. 2014;9 (2) doi: 10.1371/journal.pone.0090323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kabunga P, Phan K, Ha H, Sy RW. Meta-analysis of contemporary atrial fibrillation ablation strategiesirrigated radiofrequency versus duty-cycled phased radiofrequency versus cryoballoon ablation. JACC: Clinical Electrophysiology. 2016;0:0–0. doi: 10.1016/j.jacep.2015.12.013. [DOI] [PubMed] [Google Scholar]
- 26.Vogt Jürgen, Heintze Johannes, Gutleben Klaus J, Muntean Bogdan, Horstkotte Dieter, Nölker Georg. Long-term outcomes after cryoballoon pulmonary vein isolation: results from a prospective study in 605 patients. J. Am. Coll. Cardiol. 2013 Apr 23;61 (16):1707–12. doi: 10.1016/j.jacc.2012.09.033. [DOI] [PubMed] [Google Scholar]
- 27.Deshmukh Abhishek, Patel Nileshkumar J, Pant Sadip, Shah Neeraj, Chothani Ankit, Mehta Kathan, Grover Peeyush, Singh Vikas, Vallurupalli Srikanth, Savani Ghanshyambhai T, Badheka Apurva, Tuliani Tushar, Dabhadkar Kaustubh, Dibu George, Reddy Y Madhu, Sewani Asif, Kowalski Marcin, Mitrani Raul, Paydak Hakan, Viles-Gonzalez Juan F. In-hospital complications associated with catheter ablation of atrial fibrillation in the United States between 2000 and 2010: analysis of 93 801 procedures. Circulation. 2013 Nov 05;128 (19):2104–12. doi: 10.1161/CIRCULATIONAHA.113.003862. [DOI] [PubMed] [Google Scholar]
- 28.Calkins Hugh, Kuck Karl Heinz, Cappato Riccardo, Brugada Josep, Camm A John, Chen Shih-Ann, Crijns Harry J G, Damiano Ralph J, Davies D Wyn, DiMarco John, Edgerton James, Ellenbogen Kenneth, Ezekowitz Michael D, Haines David E, Haissaguerre Michel, Hindricks Gerhard, Iesaka Yoshito, Jackman Warren, Jalife José, Jais Pierre, Kalman Jonathan, Keane David, Kim Young-Hoon, Kirchhof Paulus, Klein George, Kottkamp Hans, Kumagai Koichiro, Lindsay Bruce D, Mansour Moussa, Marchlinski Francis E, McCarthy Patrick M, Mont J Lluis, Morady Fred, Nademanee Koonlawee, Nakagawa Hiroshi, Natale Andrea, Nattel Stanley, Packer Douglas L, Pappone Carlo, Prystowsky Eric, Raviele Antonio, Reddy Vivek, Ruskin Jeremy N, Shemin Richard J, Tsao Hsuan-Ming, Wilber David. 2012 HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design: a report of the Heart Rhythm Society (HRS) Task Force on Catheter and Surgical Ablation of Atrial Fibrillation. Developed in partnership with the European Heart Rhythm Association (EHRA), a registered branch of the European Society of Cardiology (ESC) and the European Cardiac Arrhythmia Society (ECAS); and in collaboration with the American College of Cardiology (ACC), American Heart Association (AHA), the Asia Pacific Heart Rhythm Society (APHRS), and the Society of Thoracic Surgeons (STS). Endorsed by the governing bodies of the American College of Cardiology Foundation, the American Heart Association, the European Cardiac Arrhythmia Society, the European Heart Rhythm Association, the Society of Thoracic Surgeons, the Asia Pacific Heart Rhythm Society, and the Heart Rhythm Society. Heart Rhythm. 2012 Apr;9 (4):632–696.e21. doi: 10.1016/j.hrthm.2011.12.016. [DOI] [PubMed] [Google Scholar]
- 29.Wilber David J, Pappone Carlo, Neuzil Petr, De Paola Angelo, Marchlinski Frank, Natale Andrea, Macle Laurent, Daoud Emile G, Calkins Hugh, Hall Burr, Reddy Vivek, Augello Giuseppe, Reynolds Matthew R, Vinekar Chandan, Liu Christine Y, Berry Scott M, Berry Donald A. Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA. 2010 Jan 27;303 (4):333–40. doi: 10.1001/jama.2009.2029. [DOI] [PubMed] [Google Scholar]
- 30.De Ponti Roberto, Cappato Riccardo, Curnis Antonio, Della Bella Paolo, Padeletti Luigi, Raviele Antonio, Santini Massimo, Salerno-Uriarte Jorge A. Trans-septal catheterization in the electrophysiology laboratory: data from a multicenter survey spanning 12 years. J. Am. Coll. Cardiol. 2006 Mar 07;47 (5):1037–42. doi: 10.1016/j.jacc.2005.10.046. [DOI] [PubMed] [Google Scholar]
- 31.Andrade Jason G, Dubuc Marc, Guerra Peter G, Macle Laurent, Rivard Lena, Roy Denis, Talajic Mario, Thibault Bernard, Khairy Paul. Cryoballoon ablation for atrial fibrillation. Indian Pacing Electrophysiol J. 2012 Mar;12 (2):39–53. doi: 10.1016/s0972-6292(16)30479-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Andrade Jason G, Khairy Paul, Guerra Peter G, Deyell Marc W, Rivard Lena, Macle Laurent, Thibault Bernard, Talajic Mario, Roy Denis, Dubuc Marc. Efficacy and safety of cryoballoon ablation for atrial fibrillation: a systematic review of published studies. Heart Rhythm. 2011 Sep;8 (9):1444–51. doi: 10.1016/j.hrthm.2011.03.050. [DOI] [PubMed] [Google Scholar]