Abstract
Idiopathic paroxysmal atrioventricular (AV) block poses a true diagnostic challenge. What is clear about this entity is the confusion about its definition and consequently about its etiology. According to certain sources, the diagnosis of this block requires the lack of a structural cardiac pathology that justifies the observed manifestations and an absence of electrocardiographic disorders prior to an episode. The clinical presentation of idiopathic paroxysmal AV block does not differ from that of another cardiogenic syncope or of a vasovagal syncope with a significant cardioinhibitory component. With respect to the mechanism that explains this block, it has been postulated that patients with low basal adenosine levels exhibit hyperaffinity of the A2 receptors of the AV node. Variations in plasma adenosine levels may favor episodes of paroxysmal AV block. The diagnosis of this block is complex and can require years to determine. Routine electrophysiological examination of these patients is not cost effective due to the low sensitivity and specificity of this approach. Numerous groups have supported the use of an implantable loop recorder to substantiate AV block paroxysms and assess their clinical correlations. Permanent stimulation devices are utilized to reduce syncopal recurrence.
Keywords: Atrioventricular Block Idiopathic, Syncope, Adenosine Plasma Level
Introduction
In daily clinical practice, cardiologists can encounter true diagnostic challenges. Nevertheless, this fact can be satisfying to physicians, who will be induced to investigate challenging cases to determine accurate diagnoses. The transient loss of consciousness associated with syncope represents an example of a diagnostic challenge. It is useful and necessary to classify the etiology of syncope as follows: reflex (neurally mediated) syncope, syncope due to cardiac causes, orthostatic hypotension and unexplained syncope.[1] The final category includes forms of syncope for which extensive investigation does not reveal an underlying cause; this phenomenon occurs in cases of idiopathic atrioventricular (AV) block. The definition and etiology about idiopathic paroxysmal AV block are confusing. Certain authors consider idiopathic AV block to be a new clinical entity as a cause of recurrent unexplained syncope.[2] This type of AV block is defined as a paroxysmal third-degree AV block that exhibits abrupt onset, with no other rhythm disturbances before or during the block, and occurs in patients with a normal ECG and a normal heart.[3] The clinical and electrophysiological features of this type of block differ from those of both intrinsic AV block due to AV conduction disease and extrinsic vagal AV block.
In contrast to idiopathic AV block, intrinsic AV block typically occurs in patients with underlying heart disease[4] and is frequently initiated by atrial, His or ventricular extrasystole; increased heart rate (tachycardia-dependent AV block or “phase 3 paroxysmal AV block”); or decreased heart rate (bradycardia-dependent AV block or “phase 4 paroxysmal AV block”).[5] The clinical and ECG characteristics of the patients with idiopathic AV block are shown in table 1. In a general population of patients with paroxysmal AV block these clinical and ECG conditions are present in about 30% of patients.[4]
Table 1. Patients clinical and ECG characteristics of patients with idiopathic AV block reported by Brignole et al (3). RBBB (right bundle branch block); LBBB (left bundle branch block). LAH (left anterior hemiblock.
| Characteristics | N patients 1 |
|---|---|
| Age (years) | 55 |
| Sex: male (%) Female (%) |
9 (50) 9 (50) |
| Normal ECG, no (%) | 18 (100) |
| Mean QRS duration (msec) <=120 >120 |
- |
| RBBB RBBB alone Bifascicular (RBBB+LAH) Bifascicular + long PR |
0 |
| LBBB | 0 |
| Intraventricular conduction delay | 0 |
| PR interval (msec) | - |
| Asystole duration (sec) | 9 +-7 |
| Left ventricular ejection fraction <35% (%) | 0 |
| AV block with abrupt onset | 12 (66) |
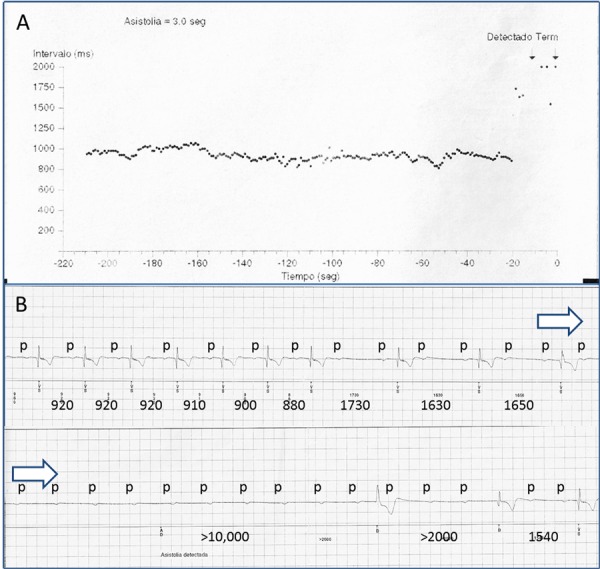
The extrinsic vagal AV block due to vagal nervous effect over the conduction system, include the gradual slowing of the sinus rate and AV conduction prolonging the PR interval (Figure 1).[6]
Figure 1. Extrinsic vagal AV block registered during implantable loop recorder monitoring in a patient without heart disease, normal ECG and recurrent syncope. A) implantable holter histogram and B)electrocardiogram. Initial sinus rhythm slowing is present, there is minimal PR interval variation in the last beat previous to 2:1 AV block, followed by complete AV block with very long pause. During AV block p-p interval shortens due to sympathetic activation. Restoration of AV conduction is without PR prolongation.
The prevalence of idiopathic AV block is unclear; however, this type of block is likely underdiagnosed due to poor recognition, its unpredictability and the typical lack of an obvious marker for AV conduction disease between episodes. The International Study on Syncope of Uncertain Etiology 2 (ISSUE 2)[7] was a prospective investigation; in this study, for subjects with an implantable loop recorder, the incidence of AV block (of type 1C according to the study’s classification system[8]) was 15% among patients with ECG-based documentation of syncope.
Diagnostic Approach To Suspected Idiopathic Paroxysmal AV Block
No specific tests exist to diagnose idiopathic paroxysmal AV block; therefore, this block should be considered in all patients who present with unexplained syncope or sudden cardiac arrest. However, before idiopathic paroxysmal AV block is diagnosed, we must exclude the possibility that the observed symptoms were caused by drug treatment (with beta blockers and/or calcium antagonists) or certain other structural cardiac diseases. In elderly, the degeneration of the His-Purkinje system and/or a degenerative valvular heart disease are the most frequent causes of AV block. Paroxysmal AV block has been reported in acute coronary syndromes caused by inferior or anterior myocardial infarctions.[9] Less frequent causes of paroxysmal AV block that we must nevertheless consider include various diseases other than Lev-Lenègre disease; immunological disorders (for instance, systemic lupus erythematosus); infections such as acute rheumatic fever and bacterial endocarditis with cardiac abscess formation; congenital defects; surgery; and sarcoidosis.[10] Finally, anecdotes have indicated that congenital disorders such as an aneurysmal membranous septum may be an exceptional cause of paroxysmal AV block[11] (Figure 2).
Figure 2. Baseline electrocardiogram, sinus bradycardia at 48 beats per minute, normal axis, PR normal, narrow QRS with no repolarization abnormality. Figure 2B: External monitoring, third-degree atrioventricular block with delay of 4320 ms and QRS escape of similar morphology to the baseline electrocardiogram. As can be seen, the paroxysmal third-degree AV block does not exhibits abrupt onset, prolonging the PR interval. So, this is not an idiopathic paroxysmal AV block. This record shows just how problematic this clinical entity.

Published by authority of the editor. Original source: Guerrero Márquez FJ, Gonzales Vargas-Machuca M, Pérez Cano B, Revello Bustos A, Marín Morgado J, Ruiz Borrell M. Aneurysmal membranous septum as an exceptional cause of paroxysmal atrioventricular block. Rev EspCardiol 2016; 69(2): 226-8. Copyright © 2016 Sociedad Española de Cardiología. Edited by Elsevier Spain, S.L. All rights reserved
In addition, to exclude structural cardiopathy, a patient’s electrocardiogram must exhibit the absence of disturbances or alterations prior to the manifestation of the AV block, such as the gradual slowing of the sinus rhythm (the PP interval) or the prolonging of the PR interval.[4,12]
To achieve a diagnosis of idiopathic paroxysmal AV block, it is necessary to perform a series of complementary tests that allow for the exclusion of other causes of syncope. A tilt table test is frequently used to assess syncope with vasovagal etiology, but this approach is not useful for reproducing an AV block due to this test’s non-specific response in cases of suspected idiopathic paroxysmal AV block.[7]
An electrophysiological study of a patient who is suspected of having idiopathic paroxysmal AV block could be considered to exclude intra-Hisian blocks that may not produce abnormalities in basal electrocardiograms.[13] However, it is well known that an electrophysiological study has limited specificity and sensitivity for detecting alterations in AV conduction.[14] Brignole et al.[3] examined 18 patients who satisfied the criteria for idiopathic paroxysmal AV block and had presented with unexplained repeated syncopal episodes. An electrophysiological study was performed, and ajmaline was administered; normal results were obtained for 12 out of the 15 patients who agreed to undergo these procedures. These data likely do not support the routine performance of an electrophysiological study in cases of suspected idiopathic paroxysmal AV block.
A useful tool in the study of recurrent syncope is an implantable loop recorder. First, this continuous electrocardiographic monitoring system enables analyses of an episode’s clinical correlations with the electrical trace at the time of the syncope and therefore allows hypotheses regarding causality. Second, this system permits assessments of whether certain previously discussed alterations occurred prior to the AV block; such determinations would enable the classification of an AV block as idiopathic. Third, the use of this system allows the adoption of a therapeutic approach based on a patient’s findings; for example, a permanent stimulation device could be implanted to prevent syncopal recurrence in cases involving the substantiation of an idiopathic paroxysmal AV block.[15] Numerous groups support the use of an implantable loop recorder[16,17,18,19] in research and in daily practice.
Permanent stimulation devices, which are not used in cases involving vasovagal syncope,[20] can be employed to prevent and avoid the recurrence of syncopal episodes in patients with idiopathic paroxysmal AV block,[3] improving morbidity. Similarly, the prognosis for these patients are not unfavorable, given the paroxysmal nature of the AV block and the low probability of degeneration into permanent forms of AV block.[3] However, no monitoring data collected over a period longer than a year exist to support this assertion.
Hypothesized Mechanism
The mechanism associated with idiopathic paroxysmal AV block is unknown. Studies have examined the role of plasma adenosine in the development of idiopathic AV block. Brignole et al.[3] considered the possibility that low plasma levels of adenosine could explain repeated syncopal episodes in the profiles of patients with idiopathic paroxysmal AV block. This statement, which lacks significant scientific evidence due to the absence of powerful supporting studies, can serve as a hypothesis regarding a possible mechanism. The aforementioned researchers examined 18 patients and observed that the only common element among these patients was a low level of plasma adenosine relative to the corresponding level in 81 healthy adults (0.33 micromole vs. 0.49 micromole). Following the intravenous administration of adenosine triphosphate (18–20 mg), a significant nodal pause was provoked in 88% of the included patients (with pauses falling between 3.3 and 25 seconds). Given these findings, Brignoleet al.developed a hypothesis involving hyperaffinity of adenosine receptors, which are found in high numbers in the AV node.[23,24] Thus, a transient increase in endogenous adenosine may be sufficient to produce an AV block in patients with low basal levels of adenosine and free or unoccupied high-affinity A1 receptors. Similar research has been conducted previously in patients with vasovagal syncope profiles;[25] although no clear and specific results were obtained, certain similarities between such patients and patients with idiopathic paroxysmal AV block may exist. Carrega et al.[26] examined adenosine receptor (A2A) levels in a group of patients who had suffered repeated syncopal episodes and had positive tilt table test results and found an elevated number of this receptor in the patients relative to healthy subjects. Subsequently, Saadjian et al.[27] examined a similar population and identified a polymorphism in the gene encoding the A2A receptor that was more common in patients who had suffered unexplained syncopal episodes than in 121 healthy subjects; this result could lead to the reorientation of hypotheses regarding these receptors’ potential role in idiopathic paroxysmal AV block.
Conclusions
Idiopathic paroxysmal AV block poses a true diagnostic challenge. Although it is true that the clinical presentation does not differ from that of another cardiogenic syncope, the diagnosis of this block requires the lack of a structural cardiac pathology that justifies the observed manifestations and an absence of electrocardiographic disorders prior to an episode. For diagnosis, it is useful the implantable loop recorder to substantiate AV block paroxysms and assess their clinical correlations.
The mechanism associated with idiopathic paroxysmal AV block is unknown. It has been postulated that patients with low basal adenosine levels exhibit hyperaffinity of the adenosine receptors of the AV node. No relevant data have been reported, so it´s necessary that more studies are needed to confirm this hypothesis.
The prognosis of idiopathic paroxysmal AV block is favorable, given the paroxysmal profile of the AV block and the low probability of degeneration into permanent forms of AV block. Permanent stimulation devices can be employed to prevent and avoid the recurrence of syncopal episodes in patients with idiopathic paroxysmal AV block.
Disclosures
None.
References
- 1.Moya Angel, Sutton Richard, Ammirati Fabrizio, Blanc Jean-Jacques, Brignole Michele, Dahm Johannes B, Deharo Jean-Claude, Gajek Jacek, Gjesdal Knut, Krahn Andrew, Massin Martial, Pepi Mauro, Pezawas Thomas, Ruiz Granell Ricardo, Sarasin Francois, Ungar Andrea, van Dijk J Gert, Walma Edmond P, Wieling Wouter. Guidelines for the diagnosis and management of syncope (version 2009). Eur. Heart J. 2009 Nov;30 (21):2631–71. doi: 10.1093/eurheartj/ehp298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mehta Niraj, Tavora Maria Zildany Pinheiro, Morillo Carlos A. Explaining the unexplained causes of syncope: are we there yet? J. Am. Coll. Cardiol. 2011 Jul 05;58 (2):174–6. doi: 10.1016/j.jacc.2011.01.039. [DOI] [PubMed] [Google Scholar]
- 3.Brignole Michele, Deharo Jean-Claude, De Roy Luc, Menozzi Carlo, Blommaert Dominique, Dabiri Lara, Ruf Jean, Guieu Regis. Syncope due to idiopathic paroxysmal atrioventricular block: long-term follow-up of a distinct form of atrioventricular block. J. Am. Coll. Cardiol. 2011 Jul 05;58 (2):167–73. doi: 10.1016/j.jacc.2010.12.045. [DOI] [PubMed] [Google Scholar]
- 4.Lee Sinjin, Wellens Hein J J, Josephson Mark E. Paroxysmal atrioventricular block. Heart Rhythm. 2009 Aug;6 (8):1229–34. doi: 10.1016/j.hrthm.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 5.El-Sherif Nabil, Jalife José. Paroxysmal atrioventricular block: are phase 3 and phase 4 block mechanisms or misnomers? Heart Rhythm. 2009 Oct;6 (10):1514–21. doi: 10.1016/j.hrthm.2009.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sud Sachin, Klein George J, Skanes Allan C, Gula Lorne J, Yee Raymond, Krahn Andrew D. Implications of mechanism of bradycardia on response to pacing in patients with unexplained syncope. Europace. 2007 May;9 (5):312–8. doi: 10.1093/europace/eum020. [DOI] [PubMed] [Google Scholar]
- 7.Brignole Michele, Sutton Richard, Menozzi Carlo, Garcia-Civera Roberto, Moya Angel, Wieling Wouter, Andresen Dietrich, Benditt David G, Grovale Nicoletta, De Santo Tiziana, Vardas Panos. Lack of correlation between the responses to tilt testing and adenosine triphosphate test and the mechanism of spontaneous neurally mediated syncope. Eur. Heart J. 2006 Sep;27 (18):2232–9. doi: 10.1093/eurheartj/ehl164. [DOI] [PubMed] [Google Scholar]
- 8.Brignole Michele, Moya Angel, Menozzi Carlo, Garcia-Civera Roberto, Sutton Richard. Proposed electrocardiographic classification of spontaneous syncope documented by an implantable loop recorder. Europace. 2005 Jan;7 (1):14–8. doi: 10.1016/j.eupc.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 9.Bortone Agustín, Albenque Jean-Paul, Marijon Eloi, Donzeau Jean-Pierre. Complete atrioventricular block and asystole in a patient with an inferior acute myocardial infarction: what is the mechanism? Heart Rhythm. 2008 Jul;5 (7):1077–9. doi: 10.1016/j.hrthm.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 10.Yahalom Malka, Roguin Nathan, Antonelli Dante, Suleiman Khaled, Turgeman Yoav. Association of heart block with uncommon disease States. Int. J. Angiol. 2013 Sep;22 (3):171–6. doi: 10.1055/s-0033-1349164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guerrero Márquez Francisco José, Gonzales Vargas-Machuca Manuel, Pérez Cano Begoña, Revello Bustos Adrián, Marín Morgado Jesús, Ruiz Borrell Mariano. Aneurysmal Membranous Septum As an Exceptional Cause of Paroxysmal Atrioventricular Block. Rev Esp Cardiol (Engl Ed) 2016 Feb;69 (2):226–8. doi: 10.1016/j.rec.2015.10.016. [DOI] [PubMed] [Google Scholar]
- 12.Zyśko Dorota, Gajek Jacek, Koźluk Edward, Mazurek Walentyna. Electrocardiographic characteristics of atrioventricular block induced by tilt testing. Europace. 2009 Feb;11 (2):225–30. doi: 10.1093/europace/eun299. [DOI] [PubMed] [Google Scholar]
- 13.Josephson M. Clinical cardiac electrophysiology: techniques and interpretations. 4 ed. Lippincott Williams and Wilkins. 2008;0:0–0. [Google Scholar]
- 14.Fujimura O, Yee R, Klein G J, Sharma A D, Boahene K A. The diagnostic sensitivity of electrophysiologic testing in patients with syncope caused by transient bradycardia. N. Engl. J. Med. 1989 Dec 21;321 (25):1703–7. doi: 10.1056/NEJM198912213212503. [DOI] [PubMed] [Google Scholar]
- 15.Sud Sachin, Klein George J, Skanes Allan C, Gula Lorne J, Yee Raymond, Krahn Andrew D. Implications of mechanism of bradycardia on response to pacing in patients with unexplained syncope. Europace. 2007 May;9 (5):312–8. doi: 10.1093/europace/eum020. [DOI] [PubMed] [Google Scholar]
- 16.Brignole M, Menozzi C, Moya A, Garcia-Civera R, Mont L, Alvarez M, Errazquin F, Beiras J, Bottoni N, Donateo P. Mechanism of syncope in patients with bundle branch block and negative electrophysiological test. Circulation. 2001 Oct 23;104 (17):2045–50. doi: 10.1161/hc4201.097837. [DOI] [PubMed] [Google Scholar]
- 17.Krahn A D, Klein G J, Yee R, Skanes A C. Randomized assessment of syncope trial: conventional diagnostic testing versus a prolonged monitoring strategy. Circulation. 2001 Jul 03;104 (1):46–51. doi: 10.1161/01.cir.104.1.46. [DOI] [PubMed] [Google Scholar]
- 18.Farwell D J, Freemantle N, Sulke A N. Use of implantable loop recorders in the diagnosis and management of syncope. Eur. Heart J. 2004 Jul;25 (14):1257–63. doi: 10.1016/j.ehj.2004.03.010. [DOI] [PubMed] [Google Scholar]
- 19.Moya A, Brignole M, Menozzi C, Garcia-Civera R, Tognarini S, Mont L, Botto G, Giada F, Cornacchia D. Mechanism of syncope in patients with isolated syncope and in patients with tilt-positive syncope. Circulation. 2001 Sep 11;104 (11):1261–7. doi: 10.1161/hc3601.095708. [DOI] [PubMed] [Google Scholar]
- 20.Raviele Antonio, Giada Franco, Menozzi Carlo, Speca Giancarlo, Orazi Serafino, Gasparini Gianni, Sutton Richard, Brignole Michele. A randomized, double-blind, placebo-controlled study of permanent cardiac pacing for the treatment of recurrent tilt-induced vasovagal syncope. The vasovagal syncope and pacing trial (SYNPACE). Eur. Heart J. 2004 Oct;25 (19):1741–8. doi: 10.1016/j.ehj.2004.06.031. [DOI] [PubMed] [Google Scholar]
- 21.Coumel P, Fabiato A, Waynberger M, Motte G, Slama R, Bouvrain Y. Bradycardia-dependent atrio-ventricular block. Report of two cases of A-V block elicited by premature beats. J Electrocardiol. 1971;4 (2):168–77. doi: 10.1016/s0022-0736(71)80010-9. [DOI] [PubMed] [Google Scholar]
- 22.Rosenbaum M B, Elizari M V, Levi R J, Nau G J. Paroxysmal atrioventricular block related to hypopolarization and spontaneous diastolic depolarization. Chest. 1973 May;63 (5):678–88. doi: 10.1378/chest.63.5.678. [DOI] [PubMed] [Google Scholar]
- 23.Shryock J C, Belardinelli L. Adenosine and adenosine receptors in the cardiovascular system: biochemistry, physiology, and pharmacology. Am. J. Cardiol. 1997 Jun 19;79 (12A):2–10. doi: 10.1016/s0002-9149(97)00256-7. [DOI] [PubMed] [Google Scholar]
- 24.Wu L, Belardinelli L, Zablocki J A, Palle V, Shryock J C. A partial agonist of the A(1)-adenosine receptor selectively slows AV conduction in guinea pig hearts. Am. J. Physiol. Heart Circ. Physiol. 2001 Jan;280 (1):H334–43. doi: 10.1152/ajpheart.2001.280.1.H334. [DOI] [PubMed] [Google Scholar]
- 25.Brignole M, Gaggioli G, Menozzi C, Gianfranchi L, Bartoletti A, Bottoni N, Lolli G, Oddone D, Del Rosso A, Pellinghelli G. Adenosine-induced atrioventricular block in patients with unexplained syncope: the diagnostic value of ATP testing. Circulation. 1997 Dec 02;96 (11):3921–7. doi: 10.1161/01.cir.96.11.3921. [DOI] [PubMed] [Google Scholar]
- 26.Carrega Louis, Saadjian Alain Y, Mercier Laurence, Zouher Ibrahim, Bergé-Lefranc Jean-Louis, Gerolami Victoria, Giaime Philippe, Sbragia Pascal, Paganelli Franck, Fenouillet Emmanuel, Lévy Samuel, Guieu Régis P. Increased expression of adenosine A2A receptors in patients with spontaneous and head-up-tilt-induced syncope. Heart Rhythm. 2007 Jul;4 (7):870–6. doi: 10.1016/j.hrthm.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 27.Saadjian Alain Y, Gerolami Victoria, Giorgi Roch, Mercier Laurence, Berge-Lefranc Jean-Louis, Paganelli Franck, Ibrahim Zouher, By Youlet, Guéant Jean Louis, Lévy Samuel, Guieu Régis P. Head-up tilt induced syncope and adenosine A2A receptor gene polymorphism. Eur. Heart J. 2009 Jun;30 (12):1510–5. doi: 10.1093/eurheartj/ehp126. [DOI] [PubMed] [Google Scholar]


