Abstract
The Brugada syndrome (BrS) is an arrhythmogenic disease associated with an increased risk of ventricular fibrillation and sudden cardiac death. The risk stratification and management of BrS patients, particularly of asymptomatic ones, still remains challenging. A previous history of aborted sudden cardiac death or arrhythmic syncope in the presence of spontaneous type 1 ECG pattern of BrS phenotype appear to be the most reliable predictors of future arrhythmic events. Several other ECG parameters have been proposed for risk stratification. Among these ECG markers, QRS-fragmentation appears very promising. Although the value of electrophysiological study still remains controversial, it appears to add important information on risk stratification, particularly when incorporated in multiparametric scores in combination with other known risk factors. The present review article provides an update on the pathophysiology, risk stratification and management of patients with BrS.
Keywords: Brugada Syndrome, Risk Stratification, Electrophysiological Study, Sudden Cardiac Death
Introduction
Brugada syndrome (BrS) is an inherited arrhythmogenic disorder characterized by an elevated ST-segment and J-point in the right precordial leads of an electrocardiogram (ECG) in the absence of structural heart disease, and it may cause sudden cardiac death due to ventricular fibrillation (VF).[1] Currently, BrS is diagnosed using criteria from the second consensus report, which was released in 2005.[2] According to the report, the new diagnostic criteria require typical ECG changes in one precordial lead.
Since BrS was described in 1992, a tremendous number of BrS cases have been reported,up to 1–5/10,000 worldwide.[3-4] Mastuo et al. investigated 4,788 subjects (1,956 men and 2,832 women) who were < 50 years old in 1958 and had undergone biennial health examinations, including electrocardiography, through 1999. The prevalence and incidence of the BrS ECG pattern were 146.2 in 100,000 persons and 14.2 persons per 100,000 person-years, respectively.[5] The average age at presentation of BrS was 45 ±10.5 years, with a peak at 30-40 years of age, and the incidence was nine times higher among men than women.
The implantation of cardiovertor defibrillator (ICD) is the only reliable therapeutic modality to prevent sudden cardiac death from cardiac arrest (CA).[6-8] ICD is clearly indicated for those with prior CAof VF. However, for asymptomatic patients with BrS, a risk stratification is needed. This article reviews the current status of risk stratification for BrS and management of the patients.
History Of CA
BrS patients with a history of CA carry the highest risk for recurrence of CA (Figure-1), and implanting ICD is considered a necessary precaution.[6-8]
Figure 1: The averaged annual rate of arrhythmic events in Brugada syndrome (BrS) from the literature.
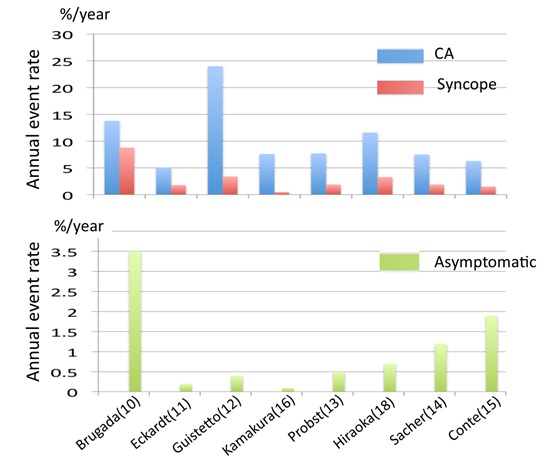
Upper column. The annual event rates of BrS patients with prior cardiac arrest (CA) (blue) and those with syncope (red). Lower column. The event rates of pateints with asymptomatic BrS. Sacher and Conte are providing the event-rates after ICD implantation. The numericals in the parenthesis is the reference number in the text.
In the first report by Brugada et al.[9] in 1998, VF recurred in 34% of symptomatic patients with previous CA or syncope during a follow-up period of 34 months with 12 % recurrence per year. In their subsequent report in 2002,[10] 12 (62%) out of 71 patients who presented with CA developed new arrhythmic events during a mean follow-up period of 54 months (13.8% per year). In the study of Eckhardt et al.,[11] the arrhythmic event rates of patients with aborted sudden death was lower: 5.1% per year. The risk of recurrent VF among patients presenting with CA can be estimated as 10% at 4 years,[12,13] and >40% at 7 years.[14-15] The mean time from presentation to VF recurrence was 1.5-2 years,[15-16] but late recurrence (>5 years after the initial event) was not rare. Similar event rates were observed in studies from Japan: 8.4 % to 11.6% per year.[16-18]
VF storms defined as ≥ 3 separate VF episodes within 24 hours have occured before and after ICD implantation in up to 24 % of the patients with appropriate ICD shocks.[15,16,19] In the series with the longest follow-up ≥5 years for 75% of the patients,[20] VF storms occurred in 12 % of those initially presenting with CA. Of the 22 men with BrS who presented with VF storms, 12 patients (54.5%) suffered VF recurrences at 21 ± 24 months after the first arrhythmic storms whereas only 1 (5.9 %) out of 17 patients with a history of a single VF episode suffered VF recurrence.[19] Spontaneous type I ECG patterns and J waves were found in 77.3% and 36.4 % of patients with VF storms vs. 28.2 % (P < 0.0001) and 9.1 % (P=0.0007) in age- and sex-matched controls of BrS patients without VF storms, respectively. Patients with ES are at risk of VF storm recurrence.[15,16,19]
Patients with a personal history of aborted sudden death have a substantial risk for recurrence of arrhythmic events and the implantation of ICD is indicated as Class I.[06-8]
Syncope
Arrhythmic (or malignant) syncope is suspected in the absence of prodromes and specific triggering circumstances when a brief loss of consciousness occurs with a rapid return. Sacher et al.[20] defined syncope based on a clinical impression as “probably arrhythmic,” “probably vagal,” or “syncope of unclear mechanism” in 40%, 30%, and 30% of patients, respectivel, including 57 BrS patients. VF occurred during follow-up in 22% of the patients with presumed arrhythmic syncope but in none of the other patients.
In another study of 118 patients with syncope,[21] 12% of those presumed to have arrhythmic syncope, but none of those with “non-arrhythmic syncope”, developed VF during the follow-up period 4.5 years. Take et al.[22] studied 84 patients with type 1 electrocardiograms and syncope (41 patients with prodrome and 43 patients without prodrome), and followed the patients for 48 ± 48 months. Syncope due to VF recurred in 13 patients among patients with unexplained syncope and was more frequent in the non-prodromal group than in the prodromal group. Blurred vision (hazard ratio [HR] 0.20) was negatively associated with VF occurrence and abnormal respiration (HR 2.18) or fragmented QRS (HR 2.39) was positively associated with VF occurrence.
Vagal syncope can occur in patients with BrS with concomitant accentuation of the ECG pattern in BrS.[23] A detailed clinical history at the time of syncope is essential to distinguish benign syncope from malignant syncope.
Priori et al. analyzed risks of cardiac events in 200 patients withy BrS;130 probands and 70 affected family members, and observed that the association between syncope and spontaneous ST-segment elevation was the strongest risk for cardiac events,[24] and this was confirmed by other workers: a risk for recurrence of arrhythmic events that ranges from 2.6-6.4% with an annual rate of 1.4-4.0 % per year as shown in Figure-1.[11,12,16-19,25-29] Some investigators propose syncope in patients with spontaneous type 1 ECG or fragmented QRS is a predictor of arrhythmic events,[24-27] whereas others do not believe there is enough evidence to support the connection denied by others.[30-31]
In BrS, ICD implantation can be considered useful in patients with a history of syncope judged to be likely caused by ventricular arrhythmias.[8]
ECG Markers
A diagnosis of BrS is confirmed by the presence of a type 1 pattern, which is a coved-type ST elevation (≥ 2 mm) descending slowly and emerging into a negative T with little or no isoelectric separation, in ≥ 1 precordial leads (V1 to V3) at the 4th, 3rd, 2nd intercostal spaces, either spontaneously or following administration of sodium channel agents.[2] In addition to its diagnostic value, some ECG markers have been studied as risks for arrhythmic events in asymptomatic BrS.
Spontaneous Type 1 ECG Pattern
In the FINGER study,[13] 1,090 patients were recruited from 11 tertiary centers in 4 European countries (745 men; 72%) with a median age of 45 (35 to 55) years. The inclusion criteria consisted of a type 1 ECG present either at baseline or after drug challenge. During follow-up up of 31.9 (14 to 54.4) months, the cardiac event rate per year was 7.7% in patients with aborted CA, 1.9% in patients with syncope, and 0.5% in asymptomatic patients. The aforementioned symptoms and spontaneous type 1 ECG were predictors of arrhythmic events, whereas gender, a familial history of SCD, the inducibility of ventricular tachyarrhythmias during electrophysiological study, and the presence of an SCN5A mutation were not predictors.
Curio et al.[32] studied 64 subjects who were diagnosed with BrS from ECGs with high intercostal spaces. The mean age from the last follow-up was 42±11 years. A typical ECG pattern was recorded at baseline in 4 subjects before a drug-challenge with sodium-channel blockers. Of those 4 subjects with spontaneous abnormal ECG, 3 experienced cardiac events.
Drug-Induced Type 1 ECG Pattern
In the PRELUDE study,[26] none of the asymptomatic patients with drug-induced type I ECG developed arrhythmic events during the 3 years of follow-up, regardless of VF inducibility at EPS. Curio[32] observed that none among the 60 patients with drug-induced ECG pattern from high intercostal spaces experienced cardiac events. Thus, patients with spontaneous type I ECG consistently have twice the risk of arrhythmic events than patients who develop a type 1 ECG pattern when challenged with a sodium-channel blocker.[13,14] ICD implantation was not indicated in asymptomatic BrS patients with a drug-induced type I ECG in the expert consensus statement.[8]
Fragmented QRS
Fragmented QRS complexes (f-QRS) are defined as ≥ 4 spikes in the QRS by Morita et al.[33] or as ≥2 spikes in the QRS of V1, V2, or V3 by Priori et al.[26] Morita[33] noted that f-QRS was more frequent in patients with BrS than in controls with right bundle branch block (RBBB) (43% vs. 3%), and particularly among BrS patients with CA (85%). Its presence was associated with an increased risk of arrhythmic events. In the PRELUDE study,[26 a prospective evaluation of 308 patients without CA (including 65 with syncope and 243 with no symptoms) revealed that patients with f-QRS were associated with a 9 times higher risk for VF recurrence. f-QRS is a promising predictor for arrhythmic events,[26,33-35] but may needs a further study before it can be declared a criterion for justifying ICD implantation in asymptomatic patients with BrS.[8]
Early Repolarization Pattern (ERP)
Notch or slur at the terminal part of the QRS complex often represents early ERP. ERP was observed in 3 of the 8 patients with idiopathic VF in 1993,[36] and recently the association was confirmed by a larger study by Haissaguerre et al.[37] The dynamic characteristics of ERP were also shown in idiopathic VF patients[38] ERP can be observed in healthy individuals, and ERP with horizontal or down-sloping ST was cennected to the malignant type of ERP.[39,40]
ERP can coexist with BrS, and Sarkozy et al.[41] observed that 15% of patients with BrS had ERP in the inferolateral leads. Kamakura et al.[16] observed a similar prevalence of ERP in BrS. ERP was associated with a 4-fold increased risk of VF recurrence. Similarly, Takagi et al.[42] reported that the risk was 11 times higher in BrS when the patients had inferolateral ERP with horizontal pattern. Some researchers have suggested inferolateral ERP is a risk for VF recurrence,[16-43] but other researchers do not support this view.[44] Patients with VF storms were associated with a higher prevalence of ERP:36%.[19] During the follow-up of 22 patients presenting VF storms, 44% had recurring VF storms within the mean follow-up time of 21±24 months. When ERP is found in patients with BrS, either ERP or BrS can be a trigger of VF. Recently, we experienced a patient with BrS combined with prominent slurs, and marked and transient ERP was considered a trigger for VF storm.[45]
Other ECG Signs
A wide QRS in lead V2 (≥ 120 ms );[46] the duration of the S-wave in lead I,[47] the r-J interval in lead V2 ≥ 90 ms and the QRS width in V6 ≥ 90ms;[48] aVR sign[49] or Tpe interval[50] were found to be good predictors of VT/VF, but these factors need to be confirmed by a larger study. Complete RBBB may coexist with BrS and unmasks the ECG pattern of BrS.[51] The prevalence and prognostic significance as well as the pathophysiology of this comorbidity needs to be explored.
Late potentials in a signal-averaged ECG are often found in BrS,[52,53] but the predictive value is considered limited. An increased TWA at night was observed more frequently among Brugada patients with a history of CA,[54] but its prognostic significance was limited.[54,55]
Electrophysiological Study
VF has been induced in 68-83% of symptomatic and in 33-39% of asymptomatic patients with BrS, and earlier studies suggested that the inducibility of VF during EPS is a risk for VF occurrence during follow-up.[10-12,56-59] However, other studies showed a negative or limited value for VF induction.[08,13,14,16,26] The VF inducibility might be affected by four factors:
The site of stimulation.
The number of extrastimuli.
The coupling intervals of extrastimuli and
The use of antiarrhythmic agents.
Site Of Stimulation
When the hearts of the patients with BrS was stimulated, a bigger conduction delay occurs in the right ventricle compared to the left ventricle,[60] and a conduction delay within the ventricle begins at longer coupling intervals of premature stimuli in BrS compared to non-BrS patients.[61] These findings support the existence of electrophysiological heterogeneity within the heart of BrS, and this heterogeneity may affect the responses to electrical stimulation during EPS.
To avoid non-specific results, some workers prefer the apex of the right ventricle for stimulation. Sieira et al.[59] updated their long-term follow-up data in 273 patients with asymptomatic BrS who underwent EPS only from the RVA and were followed for up to 15 years. The positive and negative predictive values of VF induction from the RVA for foreseeing arrhythmic events were 18% and 98%, respectively. However, the association between the site of VF induction (RVA vs. RVOT) and subsequent arrhythmic events was not evident in the studies of Makimoto et al.[62] and Kamakura et al.[16]
Number Of Extrastimuli
An increase in the number of extrastimuli will increase the rate of VF inducibility, and using two extrastimuli improved the sensitivity of the test from 50% to 75% with a low positive predictive value (13%) but a good negative predictive value of PES in asymptomatic non-inducible individuals (99%).[57]
Makimoto et al.[62] reported that 2 out of 17 patients (12%) who had VF induced by 1-2 extrastimuli developed VF, but none of the 14 non-inducible patients by 3 extrastimuli or the 11 patients with no inducible arrhythmias developed VF during the 6 years of follow-up. In a pooled analysis of 1,312 patients with BrS but without CA by Sroubek et al,[28] the mean age at the electrophysiology study was 44.9±13.3 years. Of those patients, 1,034 (79%) were male, 429 (33%) presented with syncope, and 696 (53%) had a spontaneous type 1 ECG pattern. Ventricular arrhythmia was induced in 527 of 1,247 (42%) as follows: 22 with a single extrastimulus, 231 with double extrastimuli and 274 with triple extrastimuli. The individuals induced with single or double extrastimuli rather than more aggressive stimulation protocols were associated with an increased risk for CA. However, Takagi et al.[63] reported that none of the 30 patients who had VF induced by 1-2 extrastimuli developed spontaneous VF during the 3 years of follow-up. In the PRELUDE study, no differences were observed in the VF-free survival curves between the 63 patients without prior CA who had VF induced by 1-2 extrastimuli and the 245 patients who were either non-inducible or had VF induced with 3 extrastimuli.[26]
Coupling Intervals
Patients with BrS might have a shorter ventricular effective refractory period (VERP) compared to non-BrS patients.[64] The short VERP < 200 ms during basic ventricular pacing at 600 ms correlated with an increased incidence of spontaneous VF in the PRELUDE study.[26] This outcome differs from the data of Makimoto et al.[62] which showed that the VF-free survival curves of 81 patients with inducible VF were identical whether VF was induced with a coupling interval < 200 ms.
Antiarrhythmic Agents
Some antiarrhythmic agents are known to prevent VF recurrence in BrS. The study by Belhassen et al. showed that the EPS-guided selection of IA antiarrhythmic agents, which prevent VF induction, was beneficial.[65] However, such studies are not routinely performed.
Familial And Genetic Background
The inheritance of BrS occurs via an autosomal dominant mode of transmission, and 12 responsible genes have been reported thus far.[66] Either a decrease in the inward sodium or calcium current or an increase in one of the outward potassium currents has been shown to be associated with the BrS phenotype. Some mutations may develop a more severe phenotype,[67] but in many cases, there is complex interplay between mutations and polymorphisms.[68-72] No associations have been observed between a family history of sudden cardiac deaths or mutations in the SCN5A gene, and the risk of VF in larger studies. Furthermore, SCN5A mutations were found only in 30% or less of BrS patients. This low yield is a limiting factor of genetic studies in BrS.
Managements Of BrS
As acute managements of VF storms, both oral quinidine and intravenous isoproterenol are effective.[8,73-75] Quinidine blocks transient outward current and rapid delayed rectifier currents and isoproterenol augments L-type calcium current.[76]
For long-term management, ICD is the main therapy (Figure 2). In the expert consensus statements,[08] ICD implantation is considered a class IIB indication for asymptomatic patients with inducible VF. Whereas in Japan, Class IIA or Class IIB indication is determined from the number of risk factors: a history of syncope, a family history of sudden death and inducibility of VF (Class IIA for the patients with two risks factors and Class IIB for those with one risk factors.[77] However, the current recommendation of ICD is still debated.
Figure 2: Indications of ICD for patients with Brugada syndrome (BrS).
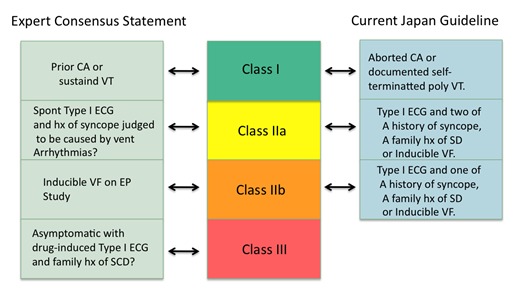
In the expert consensus statement (left) patients should have spontaneou type I ECG pattern of BrS when considering an implantation of ICD. In the Japan guideline (right), prior cardiac arrest or documentation of self-terminating polymorphic venticular tachycardia is requried for Class I indication. ICD may be recommended as Class IIA if patients have two of three risks factors, and as Class IIB if patients have one risk factor in addtion to spontaenous or drug-induced type I ECG pattern for BrS.
Quinidine is effective for prevention of VF in BrS,[65,73,74] but it may be intolerable in some patients. In a smaller number of patients, bepridil[78,79] or cilostasol[80] have been shown to be efficacious and promising. As new option, catheter ablation was shown to be effective in controlling VF storms by eliminating the VF triggering premature beats[81,82] or by modulating the arrhythmogenic substrate in the epicardial side.[83]
Conclusions
Current status of risk stratification of BrS and its managements were reviewed. For patients presenting with aborted sudden cardiac death or malignant syncope, ICD is recommended. However, risk stratification in asymptomatic BrS patients is still controversial and indication of ICD may vary from a country to another. Additional progress through the accumulation of pathophysiology data and genetic mutation data as well as clinical evidence are needed.
Disclosures
None.
References
- 1.Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J. Am. Coll. Cardiol. 1992 Nov 15;20 (6):1391–6. doi: 10.1016/0735-1097(92)90253-j. [DOI] [PubMed] [Google Scholar]
- 2.Antzelevitch Charles, Brugada Pedro, Borggrefe Martin, Brugada Josep, Brugada Ramon, Corrado Domenico, Gussak Ihor, LeMarec Herve, Nademanee Koonlawee, Perez Riera Andres Ricardo, Shimizu Wataru, Schulze-Bahr Eric, Tan Hanno, Wilde Arthur. Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation. 2005 Feb 08;111 (5):659–70. doi: 10.1161/01.CIR.0000152479.54298.51. [DOI] [PubMed] [Google Scholar]
- 3.Hermida J S, Lemoine J L, Aoun F B, Jarry G, Rey J L, Quiret J C. Prevalence of the brugada syndrome in an apparently healthy population. Am. J. Cardiol. 2000 Jul 01;86 (1):91–4. doi: 10.1016/s0002-9149(00)00835-3. [DOI] [PubMed] [Google Scholar]
- 4.Furuhashi M, Uno K, Tsuchihashi K, Nagahara D, Hyakukoku M, Ohtomo T, Satoh S, Nishimiya T, Shimamoto K. Prevalence of asymptomatic ST segment elevation in right precordial leads with right bundle branch block (Brugada-type ST shift) among the general Japanese population. Heart. 2001 Aug;86 (2):161–6. doi: 10.1136/heart.86.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matsuo K, Akahoshi M, Nakashima E, Suyama A, Seto S, Hayano M, Yano K. The prevalence, incidence and prognostic value of the Brugada-type electrocardiogram: a population-based study of four decades. J. Am. Coll. Cardiol. 2001 Sep;38 (3):765–70. doi: 10.1016/s0735-1097(01)01421-8. [DOI] [PubMed] [Google Scholar]
- 6.Zipes Douglas P, Camm A John, Borggrefe Martin, Buxton Alfred E, Chaitman Bernard, Fromer Martin, Gregoratos Gabriel, Klein George, Moss Arthur J, Myerburg Robert J, Priori Silvia G, Quinones Miguel A, Roden Dan M, Silka Michael J, Tracy Cynthia, Smith Sidney C, Jacobs Alice K, Adams Cynthia D, Antman Elliott M, Anderson Jeffrey L, Hunt Sharon A, Halperin Jonathan L, Nishimura Rick, Ornato Joseph P, Page Richard L, Riegel Barbara, Priori Silvia G, Blanc Jean-Jacques, Budaj Andrzej, Camm A John, Dean Veronica, Deckers Jaap W, Despres Catherine, Dickstein Kenneth, Lekakis John, McGregor Keith, Metra Marco, Morais Joao, Osterspey Ady, Tamargo Juan Luis, Zamorano José Luis. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death). J. Am. Coll. Cardiol. 2006 Sep 05;48 (5):e247–346. doi: 10.1016/j.jacc.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 7.Guidelines for risks and prevention of sudden cardiac death (JCS 2010): – digest version –. Circ. J. 2012;76 (2):489–507. doi: 10.1253/circj.cj-88-0022. [DOI] [PubMed] [Google Scholar]
- 8.Priori Silvia G, Wilde Arthur A, Horie Minoru, Cho Yongkeun, Behr Elijah R, Berul Charles, Blom Nico, Brugada Josep, Chiang Chern-En, Huikuri Heikki, Kannankeril Prince, Krahn Andrew, Leenhardt Antoine, Moss Arthur, Schwartz Peter J, Shimizu Wataru, Tomaselli Gordon, Tracy Cynthia. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm. 2013 Dec;10 (12):1932–63. doi: 10.1016/j.hrthm.2013.05.014. [DOI] [PubMed] [Google Scholar]
- 9.Brugada J, Brugada R, Brugada P. Right bundle-branch block and ST-segment elevation in leads V1 through V3: a marker for sudden death in patients without demonstrable structural heart disease. Circulation. 1998 Feb 10;97 (5):457–60. doi: 10.1161/01.cir.97.5.457. [DOI] [PubMed] [Google Scholar]
- 10.Brugada Josep, Brugada Ramon, Antzelevitch Charles, Towbin Jeffrey, Nademanee Koonlawee, Brugada Pedro. Long-term follow-up of individuals with the electrocardiographic pattern of right bundle-branch block and ST-segment elevation in precordial leads V1 to V3. Circulation. 2002 Jan 01;105 (1):73–8. doi: 10.1161/hc0102.101354. [DOI] [PubMed] [Google Scholar]
- 11.Eckardt Lars, Probst Vincent, Smits Jeroen P P, Bahr Eric Schulze, Wolpert Christian, Schimpf Rainer, Wichter Thomas, Boisseau Pierre, Heinecke Achim, Breithardt Günter, Borggrefe Martin, LeMarec Herve, Böcker Dirk, Wilde Arthur A M. Long-term prognosis of individuals with right precordial ST-segment-elevation Brugada syndrome. Circulation. 2005 Jan 25;111 (3):257–63. doi: 10.1161/01.CIR.0000153267.21278.8D. [DOI] [PubMed] [Google Scholar]
- 12.Giustetto Carla, Drago Stefano, Demarchi Pier Giuseppe, Dalmasso Paola, Bianchi Francesca, Masi Andrea Sibona, Carvalho Paula, Occhetta Eraldo, Rossetti Guido, Riccardi Riccardo, Bertona Roberta, Gaita Fiorenzo. Risk stratification of the patients with Brugada type electrocardiogram: a community-based prospective study. Europace. 2009 Apr;11 (4):507–13. doi: 10.1093/europace/eup006. [DOI] [PubMed] [Google Scholar]
- 13.Probst V, Veltmann C, Eckardt L, Meregalli P G, Gaita F, Tan H L, Babuty D, Sacher F, Giustetto C, Schulze-Bahr E, Borggrefe M, Haissaguerre M, Mabo P, Le Marec H, Wolpert C, Wilde A A M. Long-term prognosis of patients diagnosed with Brugada syndrome: Results from the FINGER Brugada Syndrome Registry. Circulation. 2010 Feb 09;121 (5):635–43. doi: 10.1161/CIRCULATIONAHA.109.887026. [DOI] [PubMed] [Google Scholar]
- 14.Sacher Frédéric, Probst Vincent, Maury Philippe, Babuty Dominique, Mansourati Jacques, Komatsu Yuki, Marquie Christelle, Rosa Antonio, Diallo Abou, Cassagneau Romain, Loizeau Claire, Martins Raphael, Field Michael E, Derval Nicolas, Miyazaki Shinsuke, Denis Arnaud, Nogami Akihiko, Ritter Philippe, Gourraud Jean-Baptiste, Ploux Sylvain, Rollin Anne, Zemmoura Adlane, Lamaison Dominique, Bordachar Pierre, Pierre Bertrand, Jaïs Pierre, Pasquié Jean-Luc, Hocini Mélèze, Legal François, Defaye Pascal, Boveda Serge, Iesaka Yoshito, Mabo Philippe, Haïssaguerre Michel. Outcome after implantation of a cardioverter-defibrillator in patients with Brugada syndrome: a multicenter study-part 2. Circulation. 2013 Oct 15;128 (16):1739–47. doi: 10.1161/CIRCULATIONAHA.113.001941. [DOI] [PubMed] [Google Scholar]
- 15.Conte Giulio, Sieira Juan, Ciconte Giuseppe, de Asmundis Carlo, Chierchia Gian-Battista, Baltogiannis Giannis, Di Giovanni Giacomo, La Meir Mark, Wellens Francis, Czapla Jens, Wauters Kristel, Levinstein Moises, Saitoh Yukio, Irfan Ghazala, Julià Justo, Pappaert Gudrun, Brugada Pedro. Implantable cardioverter-defibrillator therapy in Brugada syndrome: a 20-year single-center experience. J. Am. Coll. Cardiol. 2015 Mar 10;65 (9):879–88. doi: 10.1016/j.jacc.2014.12.031. [DOI] [PubMed] [Google Scholar]
- 16.Kamakura Shiro, Ohe Tohru, Nakazawa Kiyoshi, Aizawa Yoshifusa, Shimizu Akihiko, Horie Minoru, Ogawa Satoshi, Okumura Ken, Tsuchihashi Kazufumi, Sugi Kaoru, Makita Naomasa, Hagiwara Nobuhisa, Inoue Hiroshi, Atarashi Hirotsugu, Aihara Naohiko, Shimizu Wataru, Kurita Takashi, Suyama Kazuhiro, Noda Takashi, Satomi Kazuhiro, Okamura Hideo, Tomoike Hitonobu. Long-term prognosis of probands with Brugada-pattern ST-elevation in leads V1-V3. Circ Arrhythm Electrophysiol. 2009 Oct;2 (5):495–503. doi: 10.1161/CIRCEP.108.816892. [DOI] [PubMed] [Google Scholar]
- 17.Takagi M, Sekiguchi Y, Yokoyama Y, Aihar N, Aonuma K, Hiraoka M. Clinical follow-up and predictoers of cardiac events in pateitns with Brugada syndrome. Jpn J Eectrocardiol. 2012;0:5–10. [Google Scholar]
- 18.Hiraoka Masayasu, Takagi Masahiko, Yokoyama Yasuhiro, Sekiguchi Yukio, Aihara Naohiko, Aonuma Kazutaka. Prognosis and risk stratification of young adults with Brugada syndrome. J Electrocardiol. 2013 May 25;46 (4):279–83. doi: 10.1016/j.jelectrocard.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 19.Kaneko Yoshiaki, Horie Minoru, Niwano Shinichi, Kusano Kengo F, Takatsuki Seiji, Kurita Takashi, Mitsuhashi Takeshi, Nakajima Tadashi, Irie Tadanobu, Hasegawa Kanae, Noda Takashi, Kamakura Shiro, Aizawa Yoshiyasu, Yasuoka Ryobun, Torigoe Katsumi, Suzuki Hiroshi, Ohe Toru, Shimizu Akihiko, Fukuda Keiichi, Kurabayashi Masahiko, Aizawa Yoshifusa. Electrical storm in patients with brugada syndrome is associated with early repolarization. Circ Arrhythm Electrophysiol. 2014 Dec;7 (6):1122–8. doi: 10.1161/CIRCEP.114.001806. [DOI] [PubMed] [Google Scholar]
- 20.Sacher Frédéric, Arsac Florence, Wilton Stephen B, Derval Nicolas, Denis Arnaud, de Guillebon Maxime, Ramoul Khaled, Bordachar Pierre, Ritter Philippe, Hocini Mélèze, Clémenty Jacques, Jaïs Pierre, Haïssaguerre Michel. Syncope in Brugada syndrome patients: prevalence, characteristics, and outcome. Heart Rhythm. 2012 Aug;9 (8):1272–9. doi: 10.1016/j.hrthm.2012.04.013. [DOI] [PubMed] [Google Scholar]
- 21.Olde Nordkamp Louise R A, Vink Arja S, Wilde Arthur A M, de Lange Freek J, de Jong Jonas S S G, Wieling Wouter, van Dijk Nynke, Tan Hanno L. Syncope in Brugada syndrome: prevalence, clinical significance, and clues from history taking to distinguish arrhythmic from nonarrhythmic causes. Heart Rhythm. 2015 Feb;12 (2):367–75. doi: 10.1016/j.hrthm.2014.10.014. [DOI] [PubMed] [Google Scholar]
- 22.Take Yutaka, Morita Hiroshi, Toh Norihisa, Nishii Nobuhiro, Nagase Satoshi, Nakamura Kazufumi, Kusano Kengo F, Ohe Tohru, Ito Hiroshi. Identification of high-risk syncope related to ventricular fibrillation in patients with Brugada syndrome. Heart Rhythm. 2012 May;9 (5):752–9. doi: 10.1016/j.hrthm.2011.11.045. [DOI] [PubMed] [Google Scholar]
- 23.Yokokawa Miki, Okamura Hideo, Noda Takashi, Satomi Kazuhiro, Suyama Kazuhiro, Kurita Takashi, Aihara Naohiko, Kamakura Shiro, Shimizu Wataru. Neurally mediated syncope as a cause of syncope in patients with Brugada electrocardiogram. J. Cardiovasc. Electrophysiol. 2010 Feb;21 (2):186–92. doi: 10.1111/j.1540-8167.2009.01599.x. [DOI] [PubMed] [Google Scholar]
- 24.Priori Silvia G, Napolitano Carlo, Gasparini Maurizio, Pappone Carlo, Della Bella Paolo, Giordano Umberto, Bloise Raffaella, Giustetto Carla, De Nardis Roberto, Grillo Massimiliano, Ronchetti Elena, Faggiano Giovanna, Nastoli Janni. Natural history of Brugada syndrome: insights for risk stratification and management. Circulation. 2002 Mar 19;105 (11):1342–7. doi: 10.1161/hc1102.105288. [DOI] [PubMed] [Google Scholar]
- 25.Gehi Anil K, Duong Truong D, Metz Louise D, Gomes J Anthony, Mehta Davendra. Risk stratification of individuals with the Brugada electrocardiogram: a meta-analysis. J. Cardiovasc. Electrophysiol. 2006 Jun;17 (6):577–83. doi: 10.1111/j.1540-8167.2006.00455.x. [DOI] [PubMed] [Google Scholar]
- 26.Priori Silvia G, Gasparini Maurizio, Napolitano Carlo, Della Bella Paolo, Ottonelli Andrea Ghidini, Sassone Biagio, Giordano Umberto, Pappone Carlo, Mascioli Giosuè, Rossetti Guido, De Nardis Roberto, Colombo Mario. Risk stratification in Brugada syndrome: results of the PRELUDE (PRogrammed ELectrical stimUlation preDictive valuE) registry. J. Am. Coll. Cardiol. 2012 Jan 03;59 (1):37–45. doi: 10.1016/j.jacc.2011.08.064. [DOI] [PubMed] [Google Scholar]
- 27.Okamura Hideo, Kamakura Tsukasa, Morita Hiroshi, Tokioka Koji, Nakajima Ikutaro, Wada Mitsuru, Ishibashi Kohei, Miyamoto Koji, Noda Takashi, Aiba Takeshi, Nishii Nobuhiro, Nagase Satoshi, Shimizu Wataru, Yasuda Satoshi, Ogawa Hisao, Kamakura Shiro, Ito Hiroshi, Ohe Tohru, Kusano Kengo F. Risk stratification in patients with Brugada syndrome without previous cardiac arrest – prognostic value of combined risk factors. Circ. J. 2015;79 (2):310–7. doi: 10.1253/circj.CJ-14-1059. [DOI] [PubMed] [Google Scholar]
- 28.Sroubek Jakub, Probst Vincent, Mazzanti Andrea, Delise Pietro, Hevia Jesus Castro, Ohkubo Kimie, Zorzi Alessandro, Champagne Jean, Kostopoulou Anna, Yin Xiaoyan, Napolitano Carlo, Milan David J, Wilde Arthur, Sacher Frederic, Borggrefe Martin, Ellinor Patrick T, Theodorakis George, Nault Isabelle, Corrado Domenico, Watanabe Ichiro, Antzelevitch Charles, Allocca Giuseppe, Priori Silvia G, Lubitz Steven A. Programmed Ventricular Stimulation for Risk Stratification in the Brugada Syndrome: A Pooled Analysis. Circulation. 2016 Feb 16;133 (7):622–30. doi: 10.1161/CIRCULATIONAHA.115.017885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brugada Josep, Brugada Ramon, Brugada Pedro. Determinants of sudden cardiac death in individuals with the electrocardiographic pattern of Brugada syndrome and no previous cardiac arrest. Circulation. 2003 Dec 23;108 (25):3092–6. doi: 10.1161/01.CIR.0000104568.13957.4F. [DOI] [PubMed] [Google Scholar]
- 30.Sarkozy Andrea, Boussy Tim, Kourgiannides Georgios, Chierchia Gian-Battista, Richter Sergio, De Potter Tom, Geelen Peter, Wellens Francis, Spreeuwenberg Marieke Dingena, Brugada Pedro. Long-term follow-up of primary prophylactic implantable cardioverter-defibrillator therapy in Brugada syndrome. Eur. Heart J. 2007 Feb;28 (3):334–44. doi: 10.1093/eurheartj/ehl450. [DOI] [PubMed] [Google Scholar]
- 31.Dores Hélder, Reis Santos Katya, Adragão Pedro, Moscoso Costa Francisco, Galvão Santos Pedro, Carmo Pedro, Cavaco Diogo, Bello Morgado Francisco, Mendes Miguel. Long-term prognosis of patients with Brugada syndrome and an implanted cardioverter-defibrillator. Rev Port Cardiol. 2015 Jun;34 (6):395–402. doi: 10.1016/j.repc.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 32.Curcio Antonio, Mazzanti Andrea, Bloise Raffaella, Monteforte Nicola, Indolfi Ciro, Priori Silvia G, Napolitano Carlo. Clinical Presentation and Outcome of Brugada Syndrome Diagnosed With the New 2013 Criteria. J. Cardiovasc. Electrophysiol. 2016 Aug;27 (8):937–43. doi: 10.1111/jce.12997. [DOI] [PubMed] [Google Scholar]
- 33.Morita Hiroshi, Kusano Kengo F, Miura Daiji, Nagase Satoshi, Nakamura Kazufumi, Morita Shiho T, Ohe Tohru, Zipes Douglas P, Wu Jiashin. Fragmented QRS as a marker of conduction abnormality and a predictor of prognosis of Brugada syndrome. Circulation. 2008 Oct 21;118 (17):1697–704. doi: 10.1161/CIRCULATIONAHA.108.770917. [DOI] [PubMed] [Google Scholar]
- 34.Das Mithilesh K, Zipes Douglas P. Fragmented QRS: a predictor of mortality and sudden cardiac death. Heart Rhythm. 2009 Mar;6 (3 Suppl):S8–14. doi: 10.1016/j.hrthm.2008.10.019. [DOI] [PubMed] [Google Scholar]
- 35.Tokioka Koji, Kusano Kengo F, Morita Hiroshi, Miura Daiji, Nishii Nobuhiro, Nagase Satoshi, Nakamura Kazufumi, Kohno Kunihisa, Ito Hiroshi, Ohe Tohru. Electrocardiographic parameters and fatal arrhythmic events in patients with Brugada syndrome: combination of depolarization and repolarization abnormalities. J. Am. Coll. Cardiol. 2014 May 27;63 (20):2131–8. doi: 10.1016/j.jacc.2014.01.072. [DOI] [PubMed] [Google Scholar]
- 36.Aizawa Y, Tamura M, Chinushi M, Naitoh N, Uchiyama H, Kusano Y, Hosono H, Shibata A. Idiopathic ventricular fibrillation and bradycardia-dependent intraventricular block. Am. Heart J. 1993 Dec;126 (6):1473–4. doi: 10.1016/0002-8703(93)90550-s. [DOI] [PubMed] [Google Scholar]
- 37.Haïssaguerre Michel, Derval Nicolas, Sacher Frederic, Jesel Laurence, Deisenhofer Isabel, de Roy Luc, Pasquié Jean-Luc, Nogami Akihiko, Babuty Dominique, Yli-Mayry Sinikka, De Chillou Christian, Scanu Patrice, Mabo Philippe, Matsuo Seiichiro, Probst Vincent, Le Scouarnec Solena, Defaye Pascal, Schlaepfer Juerg, Rostock Thomas, Lacroix Dominique, Lamaison Dominique, Lavergne Thomas, Aizawa Yoshifusa, Englund Anders, Anselme Frederic, O'Neill Mark, Hocini Meleze, Lim Kang Teng, Knecht Sebastien, Veenhuyzen George D, Bordachar Pierre, Chauvin Michel, Jais Pierre, Coureau Gaelle, Chene Genevieve, Klein George J, Clémenty Jacques. Sudden cardiac arrest associated with early repolarization. N. Engl. J. Med. 2008 May 08;358 (19):2016–23. doi: 10.1056/NEJMoa071968. [DOI] [PubMed] [Google Scholar]
- 38.Aizawa Yoshifusa, Sato Akinori, Watanabe Hiroshi, Chinushi Masaomi, Furushima Hiroshi, Horie Minoru, Kaneko Yoshiaki, Imaizumi Tsutomu, Okubo Kimie, Watanabe Ichiro, Shinozaki Tsuyoshi, Aizawa Yoshiyasu, Fukuda Keiichi, Joo Kunitake, Haissaguerre Michel. Dynamicity of the J-wave in idiopathic ventricular fibrillation with a special reference to pause-dependent augmentation of the J-wave. J. Am. Coll. Cardiol. 2012 May 29;59 (22):1948–53. doi: 10.1016/j.jacc.2012.02.028. [DOI] [PubMed] [Google Scholar]
- 39.Tikkanen Jani T, Anttonen Olli, Junttila M Juhani, Aro Aapo L, Kerola Tuomas, Rissanen Harri A, Reunanen Antti, Huikuri Heikki V. Long-term outcome associated with early repolarization on electrocardiography. N. Engl. J. Med. 2009 Dec 24;361 (26):2529–37. doi: 10.1056/NEJMoa0907589. [DOI] [PubMed] [Google Scholar]
- 40.Adler Arnon, Rosso Raphael, Viskin Dana, Halkin Amir, Viskin Sami. What do we know about the "malignant form" of early repolarization? J. Am. Coll. Cardiol. 2013 Sep 03;62 (10):863–8. doi: 10.1016/j.jacc.2013.05.054. [DOI] [PubMed] [Google Scholar]
- 41.Sarkozy Andrea, Chierchia Gian-Battista, Paparella Gaetano, Boussy Tim, De Asmundis Carlo, Roos Marcus, Henkens Stefan, Kaufman Leonard, Buyl Ronald, Brugada Ramon, Brugada Josep, Brugada Pedro. Inferior and lateral electrocardiographic repolarization abnormalities in Brugada syndrome. Circ Arrhythm Electrophysiol. 2009 Apr;2 (2):154–61. doi: 10.1161/CIRCEP.108.795153. [DOI] [PubMed] [Google Scholar]
- 42.Takagi Masahiko, Aonuma Kazutaka, Sekiguchi Yukio, Yokoyama Yasuhiro, Aihara Naohiko, Hiraoka Masayasu. The prognostic value of early repolarization (J wave) and ST-segment morphology after J wave in Brugada syndrome: multicenter study in Japan. Heart Rhythm. 2013 Apr;10 (4):533–9. doi: 10.1016/j.hrthm.2012.12.023. [DOI] [PubMed] [Google Scholar]
- 43.Kawata Hiro, Morita Hiroshi, Yamada Yuko, Noda Takashi, Satomi Kazuhiro, Aiba Takeshi, Isobe Mitsuaki, Nagase Satoshi, Nakamura Kazufumi, Fukushima Kusano Kengo, Ito Hiroshi, Kamakura Shiro, Shimizu Wataru. Prognostic significance of early repolarization in inferolateral leads in Brugada patients with documented ventricular fibrillation: a novel risk factor for Brugada syndrome with ventricular fibrillation. Heart Rhythm. 2013 Aug;10 (8):1161–8. doi: 10.1016/j.hrthm.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 44.Sarkozy Andrea, Chierchia Gian-Battista, Paparella Gaetano, Boussy Tim, De Asmundis Carlo, Roos Marcus, Henkens Stefan, Kaufman Leonard, Buyl Ronald, Brugada Ramon, Brugada Josep, Brugada Pedro. Inferior and lateral electrocardiographic repolarization abnormalities in Brugada syndrome. Circ Arrhythm Electrophysiol. 2009 Apr;2 (2):154–61. doi: 10.1161/CIRCEP.108.795153. [DOI] [PubMed] [Google Scholar]
- 45.Raut Shruti, Parker Martyn J. Medium to long term follow up of a consecutive series of 604 Exeter Trauma Stem Hemiarthroplasties (ETS) for the treatment of displaced intracapsular femoral neck fractures. Injury. 2016 Mar;47 (3):721–4. doi: 10.1016/j.injury.2015.10.077. [DOI] [PubMed] [Google Scholar]
- 46.Junttila M Juhani, Brugada Pedro, Hong Kui, Lizotte Eric, DE Zutter Marc, Sarkozy Andrea, Brugada Josep, Benito Begona, Perkiomaki Juha S, Mäkikallio Timo H, Huikuri Heikki V, Brugada Ramon. Differences in 12-lead electrocardiogram between symptomatic and asymptomatic Brugada syndrome patients. J. Cardiovasc. Electrophysiol. 2008 Apr;19 (4):380–3. doi: 10.1111/j.1540-8167.2007.01050.x. [DOI] [PubMed] [Google Scholar]
- 47.Calò Leonardo, Giustetto Carla, Martino Annamaria, Sciarra Luigi, Cerrato Natascia, Marziali Marta, Rauzino Jessica, Carlino Giulia, de Ruvo Ermenegildo, Guerra Federico, Rebecchi Marco, Lanzillo Chiara, Anselmino Matteo, Castro Antonio, Turreni Federico, Penco Maria, Volpe Massimo, Capucci Alessandro, Gaita Fiorenzo. A New Electrocardiographic Marker of Sudden Death in Brugada Syndrome: The S-Wave in Lead I. J. Am. Coll. Cardiol. 2016 Mar 29;67 (12):1427–40. doi: 10.1016/j.jacc.2016.01.024. [DOI] [PubMed] [Google Scholar]
- 48.Takagi Masahiko, Yokoyama Yasuhiro, Aonuma Kazutaka, Aihara Naohiko, Hiraoka Masayasu. Clinical characteristics and risk stratification in symptomatic and asymptomatic patients with brugada syndrome: multicenter study in Japan. J. Cardiovasc. Electrophysiol. 2007 Dec;18 (12):1244–51. doi: 10.1111/j.1540-8167.2007.00971.x. [DOI] [PubMed] [Google Scholar]
- 49.Babai Bigi Mohamad Ali, Aslani Amir, Shahrzad Shahab. aVR sign as a risk factor for life-threatening arrhythmic events in patients with Brugada syndrome. Heart Rhythm. 2007 Aug;4 (8):1009–12. doi: 10.1016/j.hrthm.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 50.Maury Philippe, Sacher Frederic, Gourraud Jean-Baptiste, Pasquié Jean-Luc, Raczka Franck, Bongard Vanina, Duparc Alexandre, Mondoly Pierre, Sadron Marie, Chatel Stephanie, Derval Nicolas, Denis Arnaud, Cardin Christelle, Davy Jean-Marc, Hocini Meleze, Jaïs Pierre, Jesel Laurence, Carrié Didier, Galinier Michel, Haïssaguerre Michel, Probst Vincent, Rollin Anne. Increased Tpeak-Tend interval is highly and independently related to arrhythmic events in Brugada syndrome. Heart Rhythm. 2015 Dec;12 (12):2469–76. doi: 10.1016/j.hrthm.2015.07.029. [DOI] [PubMed] [Google Scholar]
- 51.Aizawa Yoshiyasu, Takatsuki Seiji, Sano Motoaki, Kimura Takehiro, Nishiyama Nobuhiro, Fukumoto Kotaro, Tanimoto Yoko, Tanimoto Kojiro, Murata Mitsushige, Komatsu Takashi, Mitamura Hideo, Ogawa Satoshi, Funazaki Toshikazu, Sato Masahito, Aizawa Yoshifusa, Fukuda Keiichi. Brugada syndrome behind complete right bundle-branch block. Circulation. 2013 Sep 03;128 (10):1048–54. doi: 10.1161/CIRCULATIONAHA.113.003472. [DOI] [PubMed] [Google Scholar]
- 52.Ikeda Takanori, Takami Mitsuaki, Sugi Kaoru, Mizusawa Yuka, Sakurada Harumizu, Yoshino Hideaki. Noninvasive risk stratification of subjects with a Brugada-type electrocardiogram and no history of cardiac arrest. Ann Noninvasive Electrocardiol. 2005 Oct;10 (4):396–403. doi: 10.1111/j.1542-474X.2005.00055.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yoshioka Koichiro, Amino Mari, Zareba Wojciech, Shima Makiyoshi, Matsuzaki Atsushi, Fujii Toshiharu, Kanda Shigetaka, Deguchi Yoshiaki, Kobayashi Yoshinori, Ikari Yuji, Kodama Itsuo, Tanabe Teruhisa. Identification of high-risk Brugada syndrome patients by combined analysis of late potential and T-wave amplitude variability on ambulatory electrocardiograms. Circ. J. 2013;77 (3):610–8. doi: 10.1253/circj.cj-12-0932. [DOI] [PubMed] [Google Scholar]
- 54.Sakamoto Shogo, Takagi Masahiko, Tatsumi Hiroaki, Doi Atsushi, Sugioka Kenichi, Hanatani Akihisa, Yoshiyama Minoru. Utility of T-wave alternans during night time as a predictor for ventricular fibrillation in patients with Brugada syndrome. Heart Vessels. 2016 Jun;31 (6):947–56. doi: 10.1007/s00380-015-0692-y. [DOI] [PubMed] [Google Scholar]
- 55.Uchimura-Makita Yuko, Nakano Yukiko, Tokuyama Takehito, Fujiwara Mai, Watanabe Yoshikazu, Sairaku Akinori, Kawazoe Hiroshi, Matsumura Hiroya, Oda Nozomu, Ikanaga Hiroki, Motoda Chikaaki, Kajihara Kenta, Oda Noboru, Verrier Richard L, Kihara Yasuki. Time-domain T-wave alternans is strongly associated with a history of ventricular fibrillation in patients with Brugada syndrome. J. Cardiovasc. Electrophysiol. 2014 Sep;25 (9):1021–7. doi: 10.1111/jce.12441. [DOI] [PubMed] [Google Scholar]
- 56.Delise Pietro, Allocca Giuseppe, Marras Elena, Giustetto Carla, Gaita Fiorenzo, Sciarra Luigi, Calo Leonardo, Proclemer Alessandro, Marziali Marta, Rebellato Luca, Berton Giuseppe, Coro Leonardo, Sitta Nadir. Risk stratification in individuals with the Brugada type 1 ECG pattern without previous cardiac arrest: usefulness of a combined clinical and electrophysiologic approach. Eur. Heart J. 2011 Jan;32 (2):169–76. doi: 10.1093/eurheartj/ehq381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Brugada Pedro, Brugada Ramon, Mont Lluis, Rivero Maximo, Geelen Peter, Brugada Josep. Natural history of Brugada syndrome: the prognostic value of programmed electrical stimulation of the heart. J. Cardiovasc. Electrophysiol. 2003 May;14 (5):455–7. doi: 10.1046/j.1540-8167.2003.02517.x. [DOI] [PubMed] [Google Scholar]
- 58.Belhassen Bernard, Michowitz Yoav. Arrhythmic risk stratification by programmed ventricular stimulation in Brugada syndrome: the end of the debate? Circ Arrhythm Electrophysiol. 2015 Aug;8 (4):757–9. doi: 10.1161/CIRCEP.115.003138. [DOI] [PubMed] [Google Scholar]
- 59.Sieira Juan, Conte Giulio, Ciconte Giuseppe, de Asmundis Carlo, Chierchia Gian-Battista, Baltogiannis Giannis, Di Giovanni Giacomo, Saitoh Yukio, Irfan Ghazala, Casado-Arroyo Ruben, Juliá Justo, La Meir Mark, Wellens Francis, Wauters Kristel, Van Malderen Sophie, Pappaert Gudrun, Brugada Pedro. Prognostic value of programmed electrical stimulation in Brugada syndrome: 20 years experience. Circ Arrhythm Electrophysiol. 2015 Aug;8 (4):777–84. doi: 10.1161/CIRCEP.114.002647. [DOI] [PubMed] [Google Scholar]
- 60.Furushima Hiroshi, Chinushi Masaomi, Hirono Takashi, Sugiura Hirotaka, Watanabe Hiroshi, Komura Satoru, Washizuka Takashi, Aizawa Yoshifusa. Relationship between dominant prolongation of the filtered QRS duration in the right precordial leads and clinical characteristics in Brugada syndrome. J. Cardiovasc. Electrophysiol. 2005 Dec;16 (12):1311–7. doi: 10.1111/j.1540-8167.2005.00262.x. [DOI] [PubMed] [Google Scholar]
- 61.Furushima Hiroshi, Chinushi Masaomi, Iijima Kenichi, Izumi Daisuke, Hosaka Yukio, Aizawa Yoshifusa. Significance of early onset and progressive increase of activation delay during premature stimulation in Brugada syndrome. Circ. J. 2009 Aug;73 (8):1408–15. doi: 10.1253/circj.cj-08-1111. [DOI] [PubMed] [Google Scholar]
- 62.Makimoto Hisaki, Kamakura Shiro, Aihara Naohiko, Noda Takashi, Nakajima Ikutaro, Yokoyama Teruki, Doi Atsushi, Kawata Hiro, Yamada Yuko, Okamura Hideo, Satomi Kazuhiro, Aiba Takeshi, Shimizu Wataru. Clinical impact of the number of extrastimuli in programmed electrical stimulation in patients with Brugada type 1 electrocardiogram. Heart Rhythm. 2012 Feb;9 (2):242–8. doi: 10.1016/j.hrthm.2011.09.053. [DOI] [PubMed] [Google Scholar]
- 63.Takagi Masahiko, Yokoyama Yasuhiro, Aonuma Kazutaka, Aihara Naohiko, Hiraoka Masayasu. Clinical characteristics and risk stratification in symptomatic and asymptomatic patients with brugada syndrome: multicenter study in Japan. J. Cardiovasc. Electrophysiol. 2007 Dec;18 (12):1244–51. doi: 10.1111/j.1540-8167.2007.00971.x. [DOI] [PubMed] [Google Scholar]
- 64.Watanabe Hiroshi, Chinushi Masaomi, Sugiura Hirotaka, Washizuka Takashi, Komura Satoru, Hosaka Yukio, Furushima Hiroshi, Watanabe Hiroshi, Hayashi Junichi, Aizawa Yoshifusa. Unsuccessful internal defibrillation in Brugada syndrome: focus on refractoriness and ventricular fibrillation cycle length. J. Cardiovasc. Electrophysiol. 2005 Mar;16 (3):262–6. doi: 10.1046/j.1540-8167.2005.40579.x. [DOI] [PubMed] [Google Scholar]
- 65.Belhassen Bernard, Rahkovich Michael, Michowitz Yoav, Glick Aharon, Viskin Sami. Management of Brugada Syndrome: Thirty-Three-Year Experience Using Electrophysiologically Guided Therapy With Class 1A Antiarrhythmic Drugs. Circ Arrhythm Electrophysiol. 2015 Dec;8 (6):1393–402. doi: 10.1161/CIRCEP.115.003109. [DOI] [PubMed] [Google Scholar]
- 66.Mizusawa Yuka, Wilde Arthur A M. Brugada syndrome. Circ Arrhythm Electrophysiol. 2012 Jun 01;5 (3):606–16. doi: 10.1161/CIRCEP.111.964577. [DOI] [PubMed] [Google Scholar]
- 67.Meregalli Paola G, Tan Hanno L, Probst Vincent, Koopmann Tamara T, Tanck Michael W, Bhuiyan Zahurul A, Sacher Frederic, Kyndt Florence, Schott Jean-Jacques, Albuisson J, Mabo Philippe, Bezzina Connie R, Le Marec Herve, Wilde Arthur A M. Type of SCN5A mutation determines clinical severity and degree of conduction slowing in loss-of-function sodium channelopathies. Heart Rhythm. 2009 Mar;6 (3):341–8. doi: 10.1016/j.hrthm.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 68.Viswanathan Prakash C, Benson D Woodrow, Balser Jeffrey R. A common SCN5A polymorphism modulates the biophysical effects of an SCN5A mutation. J. Clin. Invest. 2003 Feb;111 (3):341–6. doi: 10.1172/JCI16879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Poelzing Steven, Forleo Cinzia, Samodell Melissa, Dudash Lynn, Sorrentino Sandro, Anaclerio Matteo, Troccoli Rossella, Iacoviello Massimo, Romito Roberta, Guida Pietro, Chahine Mohamed, Pitzalis Mariavittoria, Deschênes Isabelle. SCN5A polymorphism restores trafficking of a Brugada syndrome mutation on a separate gene. Circulation. 2006 Aug 01;114 (5):368–76. doi: 10.1161/CIRCULATIONAHA.105.601294. [DOI] [PubMed] [Google Scholar]
- 70.Cordeiro Jonathan M, Barajas-Martinez Hector, Hong Kui, Burashnikov Elena, Pfeiffer Ryan, Orsino Anne-Marie, Wu Yue Sheng, Hu Dan, Brugada Josep, Brugada Pedro, Antzelevitch Charles, Dumaine Robert, Brugada Ramon. Compound heterozygous mutations P336L and I1660V in the human cardiac sodium channel associated with the Brugada syndrome. Circulation. 2006 Nov 07;114 (19):2026–33. doi: 10.1161/CIRCULATIONAHA.106.627489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Núñez Lucía, Barana Adriana, Amorós Irene, de la Fuente Marta González, Dolz-Gaitón Pablo, Gómez Ricardo, Rodríguez-García Isabel, Mosquera Ignacio, Monserrat Lorenzo, Delpón Eva, Caballero Ricardo, Castro-Beiras Alfonso, Tamargo Juan. p.D1690N Nav1.5 rescues p.G1748D mutation gating defects in a compound heterozygous Brugada syndrome patient. Heart Rhythm. 2013 Feb;10 (2):264–72. doi: 10.1016/j.hrthm.2012.10.025. [DOI] [PubMed] [Google Scholar]
- 72.Bezzina Connie R, Barc Julien, Mizusawa Yuka, Remme Carol Ann, Gourraud Jean-Baptiste, Simonet Floriane, Verkerk Arie O, Schwartz Peter J, Crotti Lia, Dagradi Federica, Guicheney Pascale, Fressart Véronique, Leenhardt Antoine, Antzelevitch Charles, Bartkowiak Susan, Borggrefe Martin, Schimpf Rainer, Schulze-Bahr Eric, Zumhagen Sven, Behr Elijah R, Bastiaenen Rachel, Tfelt-Hansen Jacob, Olesen Morten Salling, Kääb Stefan, Beckmann Britt M, Weeke Peter, Watanabe Hiroshi, Endo Naoto, Minamino Tohru, Horie Minoru, Ohno Seiko, Hasegawa Kanae, Makita Naomasa, Nogami Akihiko, Shimizu Wataru, Aiba Takeshi, Froguel Philippe, Balkau Beverley, Lantieri Olivier, Torchio Margherita, Wiese Cornelia, Weber David, Wolswinkel Rianne, Coronel Ruben, Boukens Bas J, Bézieau Stéphane, Charpentier Eric, Chatel Stéphanie, Despres Aurore, Gros Françoise, Kyndt Florence, Lecointe Simon, Lindenbaum Pierre, Portero Vincent, Violleau Jade, Gessler Manfred, Tan Hanno L, Roden Dan M, Christoffels Vincent M, Le Marec Hervé, Wilde Arthur A, Probst Vincent, Schott Jean-Jacques, Dina Christian, Redon Richard. Common variants at SCN5A-SCN10A and HEY2 are associated with Brugada syndrome, a rare disease with high risk of sudden cardiac death. Nat. Genet. 2013 Sep;45 (9):1044–9. doi: 10.1038/ng.2712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Belhassen Bernard, Glick Aharon, Viskin Sami. Efficacy of quinidine in high-risk patients with Brugada syndrome. Circulation. 2004 Sep 28;110 (13):1731–7. doi: 10.1161/01.CIR.0000143159.30585.90. [DOI] [PubMed] [Google Scholar]
- 74.Hermida Jean-Sylvain, Denjoy Isabelle, Clerc Jérôme, Extramiana Fabrice, Jarry Geneviève, Milliez Paul, Guicheney Pascale, Di Fusco Stefania, Rey Jean-Luc, Cauchemez Bruno, Leenhardt Antoine. Hydroquinidine therapy in Brugada syndrome. J. Am. Coll. Cardiol. 2004 May 19;43 (10):1853–60. doi: 10.1016/j.jacc.2003.12.046. [DOI] [PubMed] [Google Scholar]
- 75.Watanabe Atsuyuki, Fukushima Kusano Kengo, Morita Hiroshi, Miura Daiji, Sumida Wakako, Hiramatsu Shigeki, Banba Kimikazu, Nishii Nobuhiro, Nagase Satoshi, Nakamura Kazufumi, Sakuragi Satoru, Ohe Tohru. Low-dose isoproterenol for repetitive ventricular arrhythmia in patients with Brugada syndrome. Eur. Heart J. 2006 Jul;27 (13):1579–83. doi: 10.1093/eurheartj/ehl060. [DOI] [PubMed] [Google Scholar]
- 76.Antzelevitch Charles, Yan Gan-Xin. J wave syndromes. Heart Rhythm. 2010 Apr;7 (4):549–58. doi: 10.1016/j.hrthm.2009.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Aonuma K, Atarashi H, Okumura K. JCS Joint group. Guidelines for Diagnosis and Management of Patients with Long QT Syndrome and Brugada Syndrome (JCS 2012). http://www.j-circ.or.jp/guideline/pdf/JCS2013_aonuma_d.pdf. 0;0:0–0. [Google Scholar]
- 78.Murakami Masato, Nakamura Kazufumi, Kusano Kengo F, Morita Hiroshi, Nakagawa Koji, Tanaka Masamichi, Tada Takeshi, Toh Norihisa, Nishii Nobuhiro, Nagase Satoshi, Hata Yoshiki, Kohno Kunihisa, Miura Daiji, Ohe Tohru, Ito Hiroshi. Efficacy of low-dose bepridil for prevention of ventricular fibrillation in patients with Brugada syndrome with and without SCN5A mutation. J. Cardiovasc. Pharmacol. 2010 Oct;56 (4):389–95. doi: 10.1097/FJC.0b013e3181f03c2f. [DOI] [PubMed] [Google Scholar]
- 79.Aizawa Yoshiyasu, Yamakawa Hiroyuki, Takatsuki Seiji, Katsumata Yoshinori, Nishiyama Takahiko, Kimura Takehiro, Nishiyama Nobuhiro, Fukumoto Kotaro, Tanimoto Yoko, Tanimoto Kojiro, Mitamura Hideo, Ogawa Satoshi, Fukuda Keiichi. Efficacy and safety of bepridil for prevention of ICD shocks in patients with Brugada syndrome and idiopathic ventricular fibrillation. Int. J. Cardiol. 2013 Oct 12;168 (5):5083–5. doi: 10.1016/j.ijcard.2013.07.187. [DOI] [PubMed] [Google Scholar]
- 80.Tsuchiya Takeshi, Ashikaga Keiichi, Honda Toshihiro, Arita Makoto. Prevention of ventricular fibrillation by cilostazol, an oral phosphodiesterase inhibitor, in a patient with Brugada syndrome. J. Cardiovasc. Electrophysiol. 2002 Jul;13 (7):698–701. doi: 10.1046/j.1540-8167.2002.00698.x. [DOI] [PubMed] [Google Scholar]
- 81.Haïssaguerre Michel, Extramiana Fabrice, Hocini Mélèze, Cauchemez Bruno, Jaïs Pierre, Cabrera Jose Angel, Farré Jerónimo, Farre Gerónimo, Leenhardt Antoine, Sanders Prashanthan, Scavée Christophe, Hsu Li-Fern, Weerasooriya Rukshen, Shah Dipen C, Frank Robert, Maury Philippe, Delay Marc, Garrigue Stéphane, Clémenty Jacques. Mapping and ablation of ventricular fibrillation associated with long-QT and Brugada syndromes. Circulation. 2003 Aug 26;108 (8):925–8. doi: 10.1161/01.CIR.0000088781.99943.95. [DOI] [PubMed] [Google Scholar]
- 82.Darmon Jean-Philippe, Bettouche Salah, Deswardt Philippe, Tiger Fabrice, Ricard Philippe, Bernasconi François, Saoudi Nadir. Radiofrequency ablation of ventricular fibrillation and multiple right and left atrial tachycardia in a patient with Brugada syndrome. J Interv Card Electrophysiol. 2004 Dec;11 (3):205–9. doi: 10.1023/B:JICE.0000048571.19462.54. [DOI] [PubMed] [Google Scholar]
- 83.Nademanee Koonlawee, Veerakul Gumpanart, Chandanamattha Pakorn, Chaothawee Lertlak, Ariyachaipanich Aekarach, Jirasirirojanakorn Kriengkrai, Likittanasombat Khanchit, Bhuripanyo Kiertijai, Ngarmukos Tachapong. Prevention of ventricular fibrillation episodes in Brugada syndrome by catheter ablation over the anterior right ventricular outflow tract epicardium. Circulation. 2011 Mar 29;123 (12):1270–9. doi: 10.1161/CIRCULATIONAHA.110.972612. [DOI] [PubMed] [Google Scholar]


