Abstract
Chimeric major histocompatibility complex (MHC) molecules supplemented with T cell receptor (TCR) signaling motifs function as activation receptors and can redirect gene-modified T cells against pathogenic CD8 T cells. We have shown that β2 microglobulin (β2m) operates as a universal signaling component of MHC-I molecules when fused with the CD3-ζ chain. Linking the H-2Kd-binding insulin B chain peptide insulin B chain, amino acids 15–23 (InsB15–23) to the N terminus of β2m/CD3-ζ, redirected polyclonal CD8 T cells against pathogenic CD8 T cells in a peptide-specific manner in the non-obese diabetic (NOD) mouse. Here, we describe mRNA electroporation for delivering peptide/β2m/CD3-ζ genes to a reporter T cell line and purified primary mouse CD8 T cells. The peptide/β2m/CD3-ζ products paired with endogenous MHC-I chains and transmitted strong activation signals upon MHC-I cross-linking. The reporter T cell line transfected with InsB15–23/β2m/CD3-ζ mRNA was activated by an InsB15–23-H-2Kd-specific CD8 T cell hybrid only when the transfected T cells expressed H-2Kd. Primary NOD CD8 T cells expressing either InsB15–23/β2m/CD3-ζ or islet-specific glucose-6-phosphatase catalytic subunit-related protein, amino acids 206–214 (IGRP206–214)/β2m/CD3-ζ killed their respective autoreactive CD8 T cell targets in vitro. Furthermore, transfer of primary CD8 T cells transfected with InsB15–23/β2m/CD3-ζ mRNA significantly reduced insulitis and protected NOD mice from diabetes. Our results demonstrate that mRNA encoding chimeric MHC-I receptors can redirect effector CD8 against diabetogenic CD8 T cells, offering a new approach for the treatment of type 1 diabetes.
Keywords: immunotherapy, mRNA, CD8 T cells, type 1 diabetes, NOD mice
Fishman et al. report a new mRNA-based strategy for redirecting polyclonal CD8 T cells against autoreactive CD8 T cells that cause type 1 diabetes and potentially other autoimmune diseases. Such redirected CD8 T cells activated and killed insulin-specific CD8 T cells in vitro and protected NOD mice from developing diabetes in vivo.
Introduction
Type 1 diabetes (T1D) is a T cell-mediated autoimmune disease in which both CD4 and CD8 T cells (CTLs) target insulin-producing islet β cells. In human T1D, islet-specific CTLs have been identified and histology shows CTLs in the islets, whereas in the non-obese diabetic (NOD) mouse, CTLs are implicated in the initial stages as well as in progression of disease.1, 2, 3, 4, 5, 6 Selective immunotargeting of diabetogenic CTLs is therefore a promising avenue for immunotherapy of T1D.
The CD3-ζ chain is an essential signaling component of the T cell receptor (TCR) complex. T cells genetically redirected through major histocompatibility complex (MHC)-I heavy (α) chains fused with CD3-ζ and supplemented with a peptide of choice can target peptide-specific CD8 T cells, initially achieved through the expression of MHC-Iα/CD3-ζ fusion proteins. For example, T cells expressing chimeric H-2Kb/CD3-ζ and pulsed with a distinct peptide exhibited efficient cytolysis of antigen-specific cytotoxic CTL precursors.7 Furthermore, transgenic T cells of a unique memory phenotype expressing an H-2Dd/CD3-ζ construct potently vetoed responses to H-2Dd in vitro.8 The addition of a cognate H-2Dd peptide endowed these transgenic cells with cytolytic activity against an antigen-specific T cell hybridoma. The polymorphic MHC-I heavy chain is non-covalently associated with an invariant, non-MHC-encoded β2 microglobulin (β2m) light chain, not anchored to the plasma membrane. We have shown that β2m can serve as a versatile molecular scaffold for chimeric MHC-I/CD3-ζ T cell activation receptors.9 A single β2m/CD3-ζ-based expression cassette enables covalent linking of any pre-selected peptide to the N terminus of β2m, so as to redirect T cells at autoreactive CD8 T cells of a given specificity.
A number of cloned diabetogenic CTLs from the NOD mouse target identified antigens. Proinsulin is a major target antigen for diabetogenic CTLs, both in the NOD mouse10 and in humans.11, 12, 13, 14, 15, 16, 17 G9C8 is a highly pathogenic CTL clone that recognizes insulin B chain, amino acids 15–23 (InsB15–23) in the context of H-2Kd in the NOD mouse,10, 18 and the cells are a predominant population in the early CD8 T cell infiltrate detected as early as 4 weeks of age.10, 19 Later, CD8 T cells reactive against an H-2Kd-binding peptide from islet-specific glucose-6-phosphatase catalytic subunit-related protein, amino acids 206–214 (IGRP206–214)20, 21, 22, 23 become dominant. A third islet-reactive, pathogenic NOD CTL, although initially thought to be specific to a dystrophia myotonica kinase, amino acids 138–146 (DMK138–146) peptide, is actually reactive to insulin.23, 24, 25 Interestingly, the relative distribution in the infiltrate of T cells varies considerably among individual mice, defining a unique immunological signature.20, 21, 22, 23 CD8 T cells reactive to glutamic acid decarboxylase (GAD65)—especially GAD65, amino acids 546–554 (GAD65546–554)—have also been identified in the NOD mouse.26, 27
Immune responses to proinsulin are necessary for IGRP-reactive CTLs to expand28, 29 and to cause diabetes. Therefore, early immunological intervention selectively targeting dominant CTL clones may arrest β cell destruction and inhibit, or entirely prevent, the onset of disease. As a proof of concept, we previously generated NOD mice expressing an InsB15–23/β2m/CD3-ζ construct in CD8 T cells.30 CTLs from these mice killed InsB15–23-reactive target CD8 T cells and protected NOD SCID (severe combined immunodeficiency) mice from diabetes when co-transferred with the pathogenic T cells and significantly reduced spontaneous diabetes in wild-type NOD mice.31
Transfection of mRNA to modify primary human and mouse T cells has drawn considerable interest. Electroporation of mRNA is fast, simple, and exceptionally efficient and drives high and uniform expression under mild conditions, thereby preserving cell viability. Although transient, mRNA transfection can drive functional expression of the introduced genes up to 5–7 days and more.32, 33, 34, 35, 36 The use of mRNA entirely obviates the risk of cellular transformation and allows the co-introduction of several genes as pre-defined mixtures, which is often limited with other gene delivery vehicles.
Here we show that CD8 T cells can be reprogrammed to recognize diabetogenic T cells following the electroporation of mRNA encoding peptide/β2m/CD3-ζ and this can target autoreactive CTLs in vivo to reduce insulitis and prevent autoimmune diabetes in the NOD mouse.
Results
Assembly and Expression of Peptide/β2m/CD3-ζ Constructs in Reporter T Cells
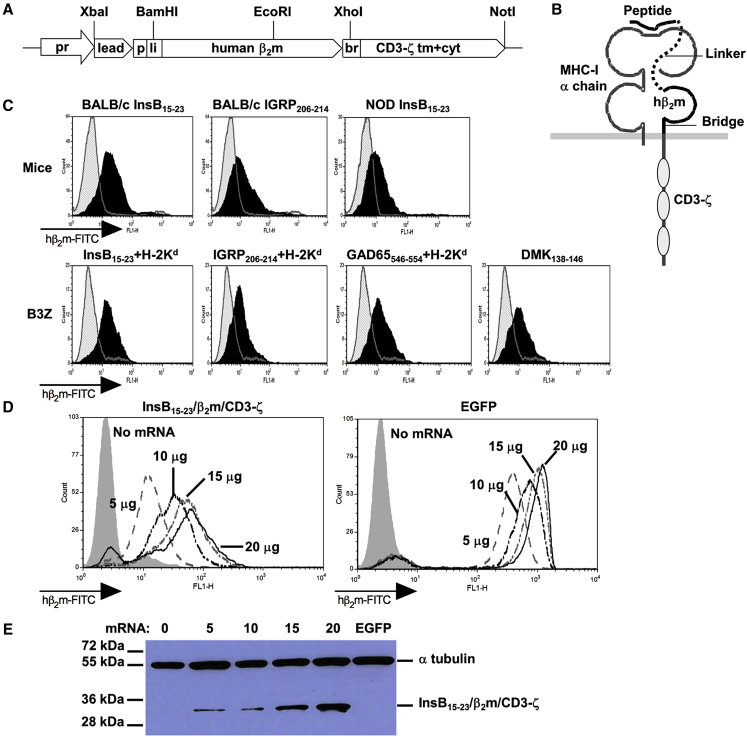
We first assembled four DNA templates for in vitro transcription of mRNA encoding peptide/β2m/CD3-ζ, incorporating InsB15–23, IGRP206–214, DMK138–146, or GAD65546–554. Figures 1A and 1B, respectively, illustrate the genetic design and the anticipated MHC-I complexes comprising the chimeric polypeptide chains. Human β2m (hβ2m), which was used throughout this study, has been shown to associate efficiently with mouse MHC-I heavy chains37, 38, 39 and is useful for detecting expression of the resulting MHC-I complexes. Flow cytometric analysis confirmed the expression of hβ2m at the cell surface of CD8 T cells purified from BALB/c and NOD mice and the reporter B3Z T cell hybridoma following mRNA transfection (Figure 1C). This expression was reproducible over many experiments. We then evaluated the effect of the amount of InsB15–23/β2m/CD3-ζ mRNA used for electroporation and level of expression in B3Z cells. Indeed, both flow cytometry and western blot analyses for hβ2m (Figures 1D and 1E) revealed dose-dependent expression, which was not accompanied by a reduction in cell viability at the higher mRNA concentrations (not shown). Western blot analysis, which was performed under reduced conditions, revealed a band of approximately 33 kDa, in accordance with the calculated molecular weight of the InsB15–23/β2m/CD3-ζ polypeptide product.
Figure 1.
Gene, Product and Expression of Peptide/β2m/CD3-ζ
(A) Genetic design. Selected restriction sites are shown. br, bridge; lead, leader peptide; li, linker; p, peptide; pr, promoter; tm+cyt, transmembrane and cytoplasmic domain. (B) Scheme of an intact, surface MHC-I complex comprising the chimeric peptide/β2m/CD3-ζ chain. (C) Flow cytometric analysis for surface expression. Splenic CD8 T cells of BALB/c and NOD mice (upper panel) and B3Z cells (lower panel) were transfected with 10 μg mRNA encoding the indicated constructs. mRNA encoding H-2Kd was added to enable presentation of the respective peptides. Cells were stained with anti-human β2m and detected with FITC-conjugated donkey anti-mouse IgG. Staining of non-transfected cells is presented by the gray histograms. (D) Flow cytometric analysis of B3Z cells electroporated with different amounts of mRNA (in micrograms), no mRNA, or EGFP mRNA and analyzed using anti-human β2m mAb purified from the supernatant of hybridoma HB149. (E) Western blot analysis performed under reduced conditions with cell lysates of B3Z cells transfected with the same mRNA as in (D), with detection using rabbit anti-human β2m polyclonal antibodies (Abs).
Function of Peptide/β2m/CD3-ζ Constructs in Reporter T Cells
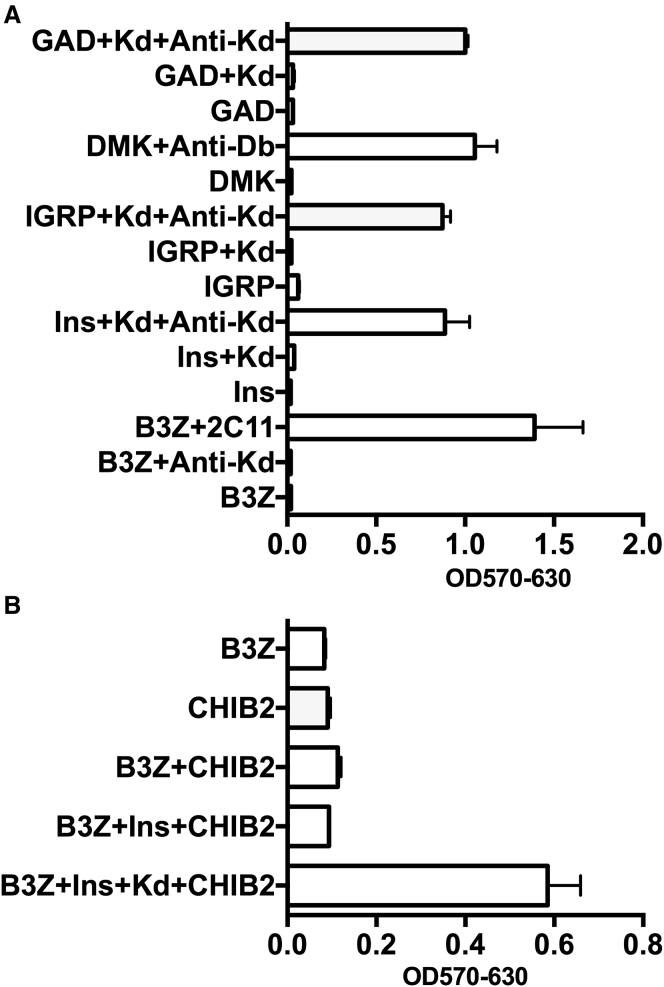
We tested whether the new MHC-I complexes expressed at the cell surface can indeed function as T cell activation receptors. To this end, we transfected B3Z reporter cells with mRNA encoding each of four peptide/β2m/CD3-ζ polypeptides, with or without mRNA encoding the full-length H-2Kd heavy chain. The B3Z cells endogenously express the MHC-I H-2Db, but not the H-2Kd necessary for antigen presentation of some of the transfected peptides in the NOD mouse, necessitating the transfection of the appropriate MHC-I complex in addition to the peptide/β2m/CD3-ζ. The four peptides were derived from previously identified autoantigens in diabetes in the NOD mouse, which express the MHC-I H-2Kd and H-2Db. These were insulin B chain, amino acids 15–23 (InsB15–23), islet-specific glucose-6-phosphatase catalytic subunit-related protein, amino acids 206–214 (IGRP206–214), and glutamic acid decarboxylase, amino acids 546–554 (GAD65546–554), which are presented by MHC-I H-2Kd. Dystrophia myotonica kinase, amino acids 138–146 (DMK138–146), binds H-2Db, which is naturally expressed by B3Z cells. Transfected cells were then incubated in the presence or absence of immobilized antibodies against the respective MHC-I heavy chain and T cell activation was monitored by a reporter assay (Figure 2A). Clearly, this experiment indicates that the polypeptide products functionally paired with exogenous (H-2Kd) or endogenous (H-2Db) heavy chains at the plasma membrane and, when triggered by the anti-MHC-I antibody binding and hence cross-linking MHC-I, potent activation signals were transmitted. These signals were comparable in magnitude to those produced by similarly cross-linking the endogenous TCR expressed by B3Z cells as shown by the response seen with anti-CD3 antibody 2C11. We then assessed the ability of InsB15–23β2m/CD3-ζ expressed by B3Z to mediate peptide-specific T cell activation in target T cells expressing an anti-InsB15–23-H-2Kd TCR. To this end, we used the CHIB2 T cell hybridoma, which expresses the αβTCR of the diabetogenic G9C8 CD8 T cell clone that recognizes the insulin B chain peptide, amino acids 15–23. We observed construct-mediated recognition upon co-culture of the two cells (Figure 2B) only when B3Z expressed both InsB15–23/β2m/CD3-ζ and H-2Kd. As both cells express the same nuclear factor of activated T cells (NFAT)-lacZ reporter gene, this assay does not discriminate between the two. However, it coincides with our previous work31 showing two-way T cell activation mediated by the G9C8 TCR and the InsB15–23/β2m/CD3-ζ construct, as the G9TCR recognizes the construct and the triggering of the construct activates the transfected cell. Here we recapitulate this notion also for exogenous mRNA-driven expression.
Figure 2.
CD8 T Cell-Targeting Genes Are Functionally Expressed in a Reporter T Cell Hybridoma following mRNA Transfection
(A) B3Z hybridoma cells, endogenously expressing MHC H-2Db, were used as reporter T cell hybridomas expressing the immunotherapeutic targeting constructs that encompassed peptides from four autoantigens important in diabetes: GAD, DMK, IGRP, and insulin. GAD, IGRP, and insulin peptides require presentation by MHC H-2Kd, which is not endogenously expressed by B3Z cells. Thus, the B3Z cells were transfected with 10 μg of each of the indicated mRNAs with or without H-2Kd mRNA. The peptide from DMK is presented by H-2Db, endogenously expressed by the B3Z. The peptide/β2m/CD3-ζ polypeptides pair with exogenous H-2Kd (GAD, IGRP, and insulin) or endogenous H-2Db (DMK) heavy chains and transmit T cell activation signals upon MHC-I cross-linking by plate-bound anti-Kd or anti-Db. The assay was performed by incubating the transfected cells overnight in 96-well plates coated with anti-Kd or anti-Db. Cell lysates were prepared and subjected to a CPRG colorimetric assay. When these indicator T cells expressing the targeting construct were triggered, either by binding to an anti-Kd or anti-Db antibody, a color change was seen in the lysates. The negative controls were cells with transfected construct, but no stimulation with anti-Kd or anti-Db antibody, or in the case of GAD, IGRP, and insulin peptides, no exogenous MHC construct. The positive control is shown as B3Z stimulated by anti-CD3 antibody, 2C11, indicating that when the B3Z cells are triggered through their own endogenous TCR, they are able to effect the color change, which is a positive control for the cell activation. (B) The B3Z cells were transfected with the InsB15–23 peptide construct with or without H-2Kd. The cells were co-incubated overnight in triplicate in a 96-well plate, the cells were lysed, and the lysate was analyzed by the CPRG colorimetric assay. The B3Z cells transfected with the InsB15–23 peptide construct together with H-2Kd can be recognized by the CHIB2 cells and this recognition stimulates activation of the B3Z cells, indicated by the color change. The error bars represent SD of the mean from triplicate experiments.
Functional Expression of Peptide/β2m/CD3-ζ in NOD CD8 T Cells
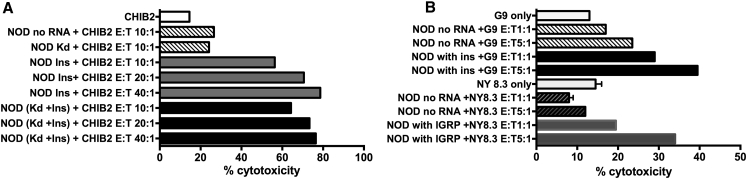
We went on to test whether polyclonal NOD CD8 T cells can be endowed with the ability to kill diabetogenic T cells following electroporation with peptide/β2m/CD3-ζ mRNA. In the experiment presented in Figure 3A, we employed CHIB2 T cell hybridomas as target cells. Polyclonal CD8 T cells transfected to express InsB15–23/β2m/CD3-ζ (effectors) were incubated with CHIB2 (targets) at three different effector-to-target (E:T) ratios and dose-dependent killing of the target CHIB2 cells was observed. We previously showed that expression of the peptide/β2m/anchor configuration resulted in exceptionally high occupancy of the restricting MHC-I product by the linked peptide.9, 40 To supplement the endogenous H-2Kd in the polyclonal NOD CD8 T cells, we tested the addition of mRNA encoding H-2Kd heavy chains. Figure 3A illustrates that the transfected polyclonal CD8 T cells have acquired the ability to kill the target CHIB2 cells and overexpression of H-2Kd had no discernible effect on the killing activity. Example flow cytometric plots are shown in Figure S1. Figure 3B presents the results of a similar cell cytotoxicity assay, showing that NOD CD8 T cells transfected with InsB15–23/β2m/CD3-ζ or IGRP206–214/β2m/CD3-ζ mRNA, respectively, kill target T cells expressing insulin-reactive G9C8 or IGRP-reactive NY8.3 TCRs purified from the corresponding TCR transgenic NOD mice. Example flow cytometric plots from Figure 3 are shown in Figure S1.
Figure 3.
Peptide/β2m/CD3-ζ mRNA Redirects NOD CD8 T Cells to Kill Insulin Reactive CHIB2 T-Hybridoma Cells and Insulin Peptide-Specific CD8 T Cells
(A) Effector cells transfected with InsB15–23/β2m/CD3-ζ mRNA (NOD Ins; shown in gray filled bars) or InsB15–23/β2m/CD3-ζ mRNA together with additional H-2Kd [NOD (Kd+Ins)]; shown in the black filled bars) were co-incubated for 24 hr with PKH26-labeled target CHIB2 cells at effector target ratios of 10:1, 20:1, and 40:1. TO-PRO-3 was added to the cells and the percentage of lysed target CHIB2 cells was determined by flow cytometric analysis. As controls (shown in the top three bars), target CHIB2 cells alone (white open bars), effector cells electroporated in the absence of mRNA (NOD no RNA; light hatched bars), or effector cells electroporated with mRNA encoding only the MHC (NOD Kd) but not the peptide (dark hatched bars) were each incubated with target cells. (B) Effector cells transfected with InsB15–23/β2m/CD3-ζ mRNA (NOD with ins; shown in filled black bars) or IGRP/β2m/CD3-ζ mRNA (NOD with IGRP; shown in filled gray bars) were co-incubated for 24 hr with PKH26-labeled target InsB15–23-reactive G9 or IGRP206–214-reactive NY8.3 CD8 T cells, respectively, at effector-to-target (E:T) ratios of 1:1 or 5:1, in duplicate. As controls, the same target cells were incubated with cells electroporated in the absence of mRNA (NOD no RNA), as shown in light hatched bars or dark hatched bars, respectively. TO-PRO-3 was added to the cells and the percentage of lysed cells was determined by flow cytometric analysis. Controls showing target G9 T cells or NY8.3 T cells are shown in the open bars. The graph shown is representative of nine similar experiments. The error bars represent SD of the mean.
CD8 T Cells Redirected to Kill Insulin-Reactive CD8 T Cells Reduce Diabetes
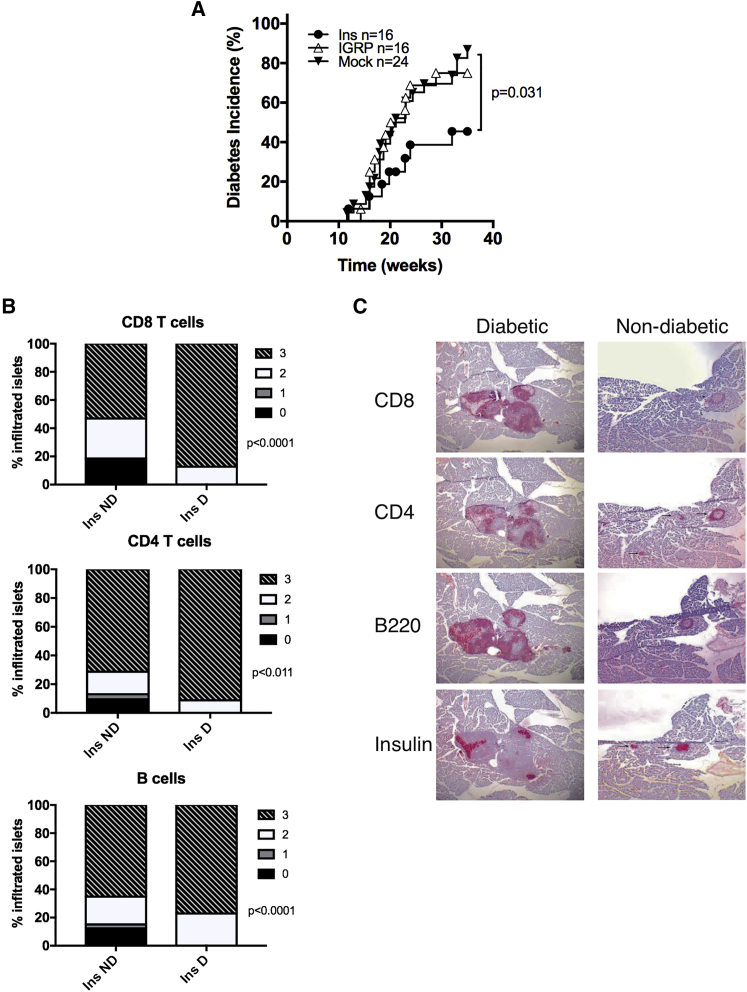
Having shown that the redirected CD8 T cells were able to kill insulin-reactive or IRGP-reactive T cells in vitro, we then tested the effect of the redirected CD8 T cells on the incidence of diabetes in vivo. CD8 T cells transfected with either InsB15–23/β2m/CD3-ζ or IGRP206–214/β2m/CD3-ζ mRNA were adoptively transferred into 5- to 6-week-old female NOD mice in a single transfer. These mice were tested weekly for glycosuria and diabetes was confirmed by a blood glucose reading of >13.9 mmol/L. The mice were euthanized either when they became diabetic or at 35 weeks if they were non-diabetic. We observed a significant reduction in the incidence of diabetes when the cells were transfected with the InsB15–23/β2m/CD3-ζ mRNA construct but not with the IGRP206–214/β2m/CD3-ζ mRNA construct, as shown in Figure 4A. Furthermore, there was a clear reduction in insulitis, the infiltration of lymphocytes, in the non-diabetic mice, compared with the insulitis in diabetic mice, with significant differences in composition of the infiltration of CD4 and CD8 T cells as well as B cells (Figures 4B and 4C).
Figure 4.
Insulitis and Diabetes in NOD Mice following Transfer of mRNA-Transfected Cells
Female NOD mice were transferred with 107 NOD CD8 T cells that had been transfected with InsB15–23/β2m/CD3-ζ mRNA (Ins; n = 16), IGRP206–214/β2m/CD3-ζ mRNA (IGRP; n = 16), or control cells electroporated but without mRNA (Mock; n = 24). The mice were screened weekly for glycosuria and following two consecutive positive readings, diabetes was confirmed by a blood glucose reading of >13.9 mmol/L. (A) Incidence of diabetes is shown with data that were analyzed by log-rank survival statistics, comparing the Ins group with the Mock group (p = 0.031). (B) Insulitis scores either when the mice developed diabetes or for the non-diabetic mice at 35 weeks of age are shown. We examined 80–115 islets from at least three mice in each group. The sections were stained with anti-CD8 (top), anti-CD4 (middle), and anti-B220 for B cells (bottom). Scoring for insulitis was as follows: 0, no insulitis; 1, peri-insulitis; 2, less than 50% infiltration; and 3, more than 50% infiltration. Data were analyzed by the χ2 test. (C) Examples of the insulitis are shown, with separate staining for CD8 and CD4 T cells, B cells (B220), and insulin, all stained in red, in a diabetic mouse and a non-diabetic mouse. Magnification is 100×.
Discussion
In this study, we have shown that mRNA constructs encoding autoantigenic peptide/β2m/CD3-ζ can be used to transfect both T cell hybrids as well as polyclonal T cells and redirect these T cells against autoreactive pathogenic CTLs. This means of selectively targeting antigen-specific cells is a modification of the successful chimeric antigen receptor (CAR) strategy adopted for tumor adoptive cell therapy41 and could be used in adoptive cell therapy in type 1 diabetes. There is good expression of the constructs and we have shown that functionally, the redirected targeting cells are recognized specifically by autoreactive CD8 T cells. The autoreactive CD8 T cells are selectively removed, as illustrated by the in vitro assays. We have also shown that peptide/β2m/CD3-ζ can target specific autoreactive CD8 T cells in vivo and reduce the incidence of autoimmune diabetes.
The simultaneous immunotargeting of a number of dominant autoreactive CD8 T cell clones by the peptide/β2m/CD3-ζ constructs can be attained either by the co-transfection of the same polyclonal CD8 T cells with a combination of mRNAs encoding the respective peptide/β2m/CD3-ζ polypeptides or the co-administration of a mixture of T cell transfectants, each of which expresses a different peptide/β2m/CD3-ζ mRNA. In the current study, we have demonstrated the functional expression of the different mRNA species, each co-transfected (when needed) with mRNA encoding the H-2Kd heavy chain (Figure 2A). In this experiment, the activation of transfectants by MHC-I cross-linking required the functional expression and pairing of the polypeptide products of both mRNA encoding MHC-I as well as the peptide/β2m/CD3-ζ. Nevertheless, it was almost as powerful as cellular activation triggered by TCR cross-linking under exactly the same conditions. In an accompanying study,42 we recently showed that mRNA encoding peptide/MHC-II/CD3-ζ can be similarly used to efficiently redirect T cells against pathogenic CD4 T cells in a peptide-specific manner. Likewise, in that study, T cell activation through the chimeric MHC-II molecules, which also required co-expression and pairing of the two products, was comparable to TCR-mediated activation. The current achievement complements our arsenal of genetic immunotargeting devices against both CD4 and CD8 islet-reactive T cells in the NOD mouse.
The demonstration that redirected polyclonal NOD CD8 T cells kill autoreactive CD8 T cells (Figure 3) recapitulates our previous findings31 in which the insulin-reactive CD8 T cells were killed by pre-activated T cells that expressed InsB15–23/β2m/CD3-ζ as a transgene. However, while those transgenic experiments illustrated the principle that CD8 T cells could be effectively redirected to kill antigen-specific targets, this procedure would not be translatable for immunotherapy in humans. In the current study, the strategy brings the procedure a step nearer to translation, in that we have shown that primary cells can be readily transfected with the mRNA construct and can kill insulin-reactive targets in a similar manner.
When the InsB15–23/β2m/CD3-ζ or IGRP206–214/β2m/CD3-ζ mRNA-transfected cells were transferred to young NOD female mice, protection from diabetes was only seen when the cells targeted InsB15–23-reactive T cells. The injection was done at a time (5–6 weeks of age) when insulin-reactive cells are detected in the pancreatic lymph nodes in a higher proportion than at later time points. In contrast, IGRP-reactive T cells tend to rise later on, so that injecting the cells at this young age may be more likely to target insulin-reactive T cells.10, 19 In principle, cell transfer aiming at immunotargeting T cells of both autoreactivities can be carried out at different time points, so that the earlier transfer targets insulin-reactive T cells and the later one targets IGRP-reactive cells. The current study demonstrates proof of principle and further studies will be carried out in the future to optimize timing of injections, including injections at later time points and whether more than one adoptive cell transfer may be required.
To our knowledge, this work is the first demonstration that mRNA-transfected T cells expressing chimeric MHC complexes can selectively immunotarget pathogenic T cells in vivo and inhibit or reduce the incidence of autoimmune diabetes. We are also evaluating the similar reprogramming of regulatory T cells in an ongoing study, hypothesizing that the targeting of a narrow population of autoreactive CD8 or CD4 T cell clones may suffice for eliciting a broad tolerizing effect.
Materials and Methods
DNA Vectors and Plasmids
The pGEMT vector for direct cloning of PCR products was from Promega. Template DNA for in vitro transcription of mRNA was cloned into the pGEM4Z/GFP/A64 vector,43 a kind gift from Dr. E. Gilboa (University of Miami) following the removal of the GFP insert (pGEM4Z/A64).
Assembly of Genetic Constructs
All PCR products were sub-cloned and their DNA sequence was confirmed prior to insertion in expression vectors. For cloning of the four constructs encoding peptide/human β2m/mouse CD3-ζ, we used essentially the same cloning strategy we described previously.9 The gene segment encoding the full leader sequence of human β2m, the antigenic peptide, and the N-terminal part of the linker was amplified from a hβ2m cDNA clone (prepared from Jurkat cells) with the forward primer 5′-GGG TCT AGA GCC GAG ATG TCT CGC TCC GTG-3′ and one of the following reverse primers: 5′-CGC GGA TCC GCC ACC TCC CAC ACG CTC CCC ACA CAC CAG GTA GAG AGC CTC AAG GCC AGA AAG-3′ for the InsB15–23 variant peptide G9V (LYLVCGERV44), 5′-CGC GGA TCC GCC ACC TCC AAG AAA AAC ATT AGT TTT AAG ATA AAC AGC ATA CAA GCC GGT CAG-3′ for IGRP206–214 (VYLKTNVFL), 5′-CGC GGA TCC GCC ACC TCC AAC TTT ATC ACC AAG AGG TTG ATA AGA AGC ATA CAA GCC GGT CAG-3′ for GAD65546–554 (SYQPLGDKV), and 5-CGC GGA TCC GCC ACC TCC AAG ATA AAG ATA ATT TTC ATC TTG AAA AGC ATA CAA GCC GGT CAG-3′ for DMK138–146 (FQDENYLYL). The resulting XbaI/BamHI fragment and a BamHI/EcoRI fragment encoding the hβ2m/CD3-ζ portion of the chimeric polypeptide9 were inserted into pGEM4Z/A64.
Cell Lines
B3Z45 is an ovalbumin (OVA)257–264-specific, H-2Kb-restricted CTL hybridoma and was a kind gift from Dr. N. Shastri (University of California, Berkeley). CHIB2 is an InsB15–23-specific hybrid of the G9C8 T cell clone with the BW5147 thymoma expressing CD8, H-2Kd-restricted T cell hybridoma.10 Both B3Z and CHIB2 harbor the nuclear factor of activated T cells-lacZ inducible reporter gene.46
In Vitro Transcription and Electroporation of mRNA
Template DNA cloned in pGEM4Z/A64 was prepared with the EndoFree Plasmid Maxi Kit (Promega) and linearized using the SpeI restriction site positioned at the 3′ end of the poly(A) tract of the vector. In vitro transcription was conducted in a 20-μL reaction mix at 37°C using the T7 mScript Standard mRNA Production System (CellScript) to generate 5′-capped in vitro-transcribed mRNA. Cells were washed twice with OptiMEM medium (Gibco) and re-suspended in 200 μL OptiMEM containing the required amount of in vitro-transcribed mRNA (10–20 μg in most experiments). Electroporation was performed with Gene Pulser Xcell (Bio-Rad Laboratories) in 2-mm cuvettes using a square wave pulse (1 millisecond, 300 V) for the experiments with cell lines, or with BTX Harvard Apparatus ECM830 (1 millisecond, 300 V) for the primary cells.
Mice
NOD mice, originally from the NOD/CaJ colony at Yale University, and G9 TCR transgenic mice47 have been bred at Cardiff University for 5 years. NY8.3 TCR transgenic mice48 were purchased from Jackson Laboratory. These mice were housed in microisolators at the specific pathogen-free facility at Cardiff University. BALB/c mice were maintained at the animal facility of the Bar-Ilan University Faculty of Medicine. All procedures were performed in accordance with protocols approved by the UK Home Office and the Israeli National Committee Institutional Animal Care and Use Committee.
Antibodies and Reagents
Anti-H-2Kd monoclonal antibody (mAb) (clone SF1-1.1) was from Pharmingen and anti-H-2Db mAb was purified from the supernatant of the 28-14-8 hybridoma. 2C11 is a hamster mAb specific to mouse CD3ε. mAb against hβ2m (clone BM-63) was from Sigma. Rabbit polyclonal antibodies against hβ2m were from Dako. Hamster mAb to mouse CD3ζ (clone H146-968) was from Santa Cruz Biotechnology. Horseradish peroxidase (HRP)-conjugated goat antibodies against rabbit IgG were from Jackson Laboratory. Rabbit antibodies against hamster IgG and fluorescein isothiocyanate (FITC)-conjugated goat anti-mouse IgG and FITC-conjugated donkey anti-mouse IgG were from Sigma and Jackson Laboratory, respectively. HRP-conjugated rabbit antibodies against hamster IgG were from Sigma. Biotinylated rat anti-mouse CD4 (clone GK1.5) was purchased from Biolegend. Biotinylated rat anti-mouse CD8a (clone 53-6.7) and rat anti-mouse B220 (clone RA3-6B2) were from BD Pharmingen and biotinylated mouse anti-insulin antibody (ICBTACLS) was from eBioscience.
Flow Cytometry
One million cultured cells or primary cells harvested from the spleen of mice were used. Single cell suspensions were either stained with the respective monoclonal antibodies in a direct staining procedure or, for indirect staining, the cells were incubated with the primary antibody for 1 hr and then washed before further incubation with fluorophore-labeled secondary antibody at 4°C. Cells were washed twice, re-suspended in 1 mL cold PBS, and analyzed by a FACSCalibur or FACSCanto system (Becton Dickinson). Data were analyzed by FCS Express (version 4; De Novo Software) or FlowJo (version 7.6.5; Tree Star) software.
Chlorophenol Red β-D-Galactopyranoside Assay
B3Z transfected cells were incubated in plates coated with immobilized MHC-I antibody or with CHIB2 hybridoma cells overnight. The culture medium was removed and 100 μL lysis buffer (9 mM MgCl2, 0.125% NP-40, and 0.3 mM chlorophenol red β-D-galactopyranoside [CPRG] in PBS) was added to each well. One to 24 hr post-lysis, the optical density (OD) of each well was measured using an ELISA reader (at 570 nm, with 630 nm as reference).
Immunoblot Analysis
Protein samples were boiled for 3 minutes, separated on a 10% non-reducing SDS polyacrylamide gel at 50 mA, and transferred onto a nitrocellulose membrane. The membrane was blocked with milk buffer (0.3 g Na2HPO4, 2.19 g NaCl, 25 mL water, and 225 mL 1% low-fat milk) overnight at 4°C and 1 hr at room temperature, washed twice with PBS, and incubated for 2 hr with the primary antibody. The membrane was then washed six times for 6 min with PBS, incubated for 1 hr with the secondary peroxidase-conjugated antibody, washed six times for 6 min with TPBS (PBS with 0.05% Tween 20), washed six times for 6 min with PBS, and then developed using an ECL (enhanced chemiluminescence) kit (Pierce-Thermo Fisher Scientific) and X-ray film 100NIF (Fuji).
Cytotoxicity Assay
CD8 T cells were isolated from the spleen of 5- to 6-week-old NOD mice and separated by negative selection (MACS; Miltenyi Biotec). The purified CD8 T cells were then activated and expanded by stimulation using plate-bound anti-CD3 and anti-CD28 antibodies, interleukin (IL)-2 and IL-7 as previously described.49 The activated CD8 T cells were transfected with mRNA encoding InsB15–23/β2m/CD3-ζ or IGRP206–214/β2m/CD3-ζ. These cells were the effector cells of the assay. G9 and NY8.3 TCR transgenic CD8+ T cells were purified by negative selection (MACS; Miltenyi Biotec) from the spleens of G9 and NY8.3 transgenic mice, respectively. Activated mRNA-transfected T cells (effectors) were incubated with purified G9 or NY8.3 T cells (targets), labeled with PKH-26 (Sigma), at an effector-to-target ratio of 1:1 and 5:1 for 16 hr at 37°C. To detect cell death, TO-PRO-3 iodide (Thermo Fisher Scientific) was added immediately prior to flow cytometric analysis. Single PKH-26+TO-PRO-3+ cells were gated, and cytotoxicity was expressed as the percentage of dead cells/total targets.31 Activated CD8 T cells with no transfected mRNA served as controls for the effector T cells.
Adoptive Transfer
NOD CD8 T cells were isolated, activated, expanded, and transfected with mRNA as described for the cytotoxicity assay. As a control, CD8+ T cells were subjected to the electroporation procedure but with no added mRNA (mock transfection). Transfected cells (peptide/β2m/CD3-ζ construct and mock-transfected) were adoptively transferred into 6-week-old NOD mice recipients by injection into the tail vein (6–10 × 106 cells per mouse).
Diagnosis of Diabetes
Mice were screened weekly for glycosuria (Diastix; Bayer) and, following two consecutive positive readings, diabetes was confirmed by a blood glucose reading of >13.9 mmol/L.
Histology
The pancreas was fixed in paraformaldehyde lysine periodate buffer overnight and then infused with 10% sucrose followed by 20% sucrose, as previously described.31 The pancreas was then embedded in OCT and snap frozen for immunohistochemistry. Frozen sections of 10-μm thickness were cut and stained with rat anti-mouse CD4, CD8, B220, and anti-insulin antibodies and detected with streptavidin-alkaline phosphatase and a Vector Red AP substrate kit (Vector Laboratories). The sections were counter-stained with hematoxylin. Insulitis was assessed from at least three mice per group and 80–115 islets were scored. Scoring for insulitis is shown in the legend for Figure 4.
Statistical Analysis
Log-rank analysis was carried out for the adoptive transfer experiments. The χ2 test was performed for the analysis of insulitis. For all tests, p < 0.05 was considered statistically significant.
Author Contributions
G.G. and F.S.W. conceived and designed the study. S.F., M.D.L., L.K.S., E.D.L., D.K., J.D., and D.Z. performed experiments. A.M., N.K., G.G., and F.S.W. supervised the study. S.F., G.G., and F.S.W. wrote the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
Acknowledgments
This work was supported by grants from the European Foundation for the Study of Diabetes (EFSD) and Diabetes UK (14/0005003).
Footnotes
Supplemental Information includes one figure and can be found with this article online at http://dx.doi.org/10.1016/j.ymthe.2016.12.007.
Supplemental Information
References
- 1.Liblau R.S., Wong F.S., Mars L.T., Santamaria P. Autoreactive CD8 T cells in organ-specific autoimmunity: emerging targets for therapeutic intervention. Immunity. 2002;17:1–6. doi: 10.1016/s1074-7613(02)00338-2. [DOI] [PubMed] [Google Scholar]
- 2.DiLorenzo T.P., Serreze D.V. The good turned ugly: immunopathogenic basis for diabetogenic CD8+ T cells in NOD mice. Immunol. Rev. 2005;204:250–263. doi: 10.1111/j.0105-2896.2005.00244.x. [DOI] [PubMed] [Google Scholar]
- 3.Tsai S., Shameli A., Santamaria P. CD8+ T cells in type 1 diabetes. Adv. Immunol. 2008;100:79–124. doi: 10.1016/S0065-2776(08)00804-3. [DOI] [PubMed] [Google Scholar]
- 4.Faustman D.L., Davis M. The primacy of CD8 T lymphocytes in type 1 diabetes and implications for therapies. J. Mol. Med. (Berl.) 2009;87:1173–1178. doi: 10.1007/s00109-009-0516-6. [DOI] [PubMed] [Google Scholar]
- 5.Willcox A., Richardson S.J., Bone A.J., Foulis A.K., Morgan N.G. Analysis of islet inflammation in human type 1 diabetes. Clin. Exp. Immunol. 2009;155:173–181. doi: 10.1111/j.1365-2249.2008.03860.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coppieters K.T., Dotta F., Amirian N., Campbell P.D., Kay T.W.H., Atkinson M.A., Roep B.O., von Herrath M.G. Demonstration of islet-autoreactive CD8 T cells in insulitic lesions from recent onset and long-term type 1 diabetes patients. J. Exp. Med. 2012;209:51–60. doi: 10.1084/jem.20111187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nguyen P., Geiger T.L. Antigen-specific targeting of CD8+ T cells with receptor-modified T lymphocytes. Gene Ther. 2003;10:594–604. doi: 10.1038/sj.gt.3301932. [DOI] [PubMed] [Google Scholar]
- 8.McFarland H.I., Hansal S.A., Morris D.I., McVicar D.W., Love P.E., Rosenberg A.S. Signaling through MHC in transgenic mice generates a population of memory phenotype cytolytic cells that lack TCR. Blood. 2003;101:4520–4528. doi: 10.1182/blood-2002-10-3265. [DOI] [PubMed] [Google Scholar]
- 9.Margalit A., Fishman S., Berko D., Engberg J., Gross G. Chimeric beta2 microglobulin/CD3zeta polypeptides expressed in T cells convert MHC class I peptide ligands into T cell activation receptors: a potential tool for specific targeting of pathogenic CD8(+) T cells. Int. Immunol. 2003;15:1379–1387. doi: 10.1093/intimm/dxg136. [DOI] [PubMed] [Google Scholar]
- 10.Wong F.S., Karttunen J., Dumont C., Wen L., Visintin I., Pilip I.M., Shastri N., Pamer E.G., Janeway C.A., Jr. Identification of an MHC class I-restricted autoantigen in type 1 diabetes by screening an organ-specific cDNA library. Nat. Med. 1999;5:1026–1031. doi: 10.1038/12465. [DOI] [PubMed] [Google Scholar]
- 11.Pinkse G.G., Tysma O.H., Bergen C.A., Kester M.G., Ossendorp F., van Veelen P.A., Keymeulen B., Pipeleers D., Drijfhout J.W., Roep B.O. Autoreactive CD8 T cells associated with beta cell destruction in type 1 diabetes. Proc. Natl. Acad. Sci. USA. 2005;102:18425–18430. doi: 10.1073/pnas.0508621102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hassainya Y., Garcia-Pons F., Kratzer R., Lindo V., Greer F., Lemonnier F.A., Niedermann G., van Endert P.M. Identification of naturally processed HLA-A2--restricted proinsulin epitopes by reverse immunology. Diabetes. 2005;54:2053–2059. doi: 10.2337/diabetes.54.7.2053. [DOI] [PubMed] [Google Scholar]
- 13.Toma A., Haddouk S., Briand J.P., Camoin L., Gahery H., Connan F., Dubois-Laforgue D., Caillat-Zucman S., Guillet J.G., Carel J.C. Recognition of a subregion of human proinsulin by class I-restricted T cells in type 1 diabetic patients. Proc. Natl. Acad. Sci. USA. 2005;102:10581–10586. doi: 10.1073/pnas.0504230102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mallone R., Martinuzzi E., Blancou P., Novelli G., Afonso G., Dolz M., Bruno G., Chaillous L., Chatenoud L., Bach J.M., van Endert P. CD8+ T-cell responses identify beta-cell autoimmunity in human type 1 diabetes. Diabetes. 2007;56:613–621. doi: 10.2337/db06-1419. [DOI] [PubMed] [Google Scholar]
- 15.Jarchum I., Baker J.C., Yamada T., Takaki T., Marron M.P., Serreze D.V., DiLorenzo T.P. In vivo cytotoxicity of insulin-specific CD8+ T-cells in HLA-A*0201 transgenic NOD mice. Diabetes. 2007;56:2551–2560. doi: 10.2337/db07-0332. [DOI] [PubMed] [Google Scholar]
- 16.Baker C., Petrich de Marquesini L.G., Bishop A.J., Hedges A.J., Dayan C.M., Wong F.S. Human CD8 responses to a complete epitope set from preproinsulin: implications for approaches to epitope discovery. J. Clin. Immunol. 2008;28:350–360. doi: 10.1007/s10875-008-9177-4. [DOI] [PubMed] [Google Scholar]
- 17.Skowera A., Ellis R.J., Varela-Calviño R., Arif S., Huang G.C., Van-Krinks C., Zaremba A., Rackham C., Allen J.S., Tree T.I. CTLs are targeted to kill beta cells in patients with type 1 diabetes through recognition of a glucose-regulated preproinsulin epitope. J. Clin. Invest. 2008;118:3390–3402. doi: 10.1172/JCI35449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wong F.S., Visintin I., Wen L., Flavell R.A., Janeway C.A., Jr. CD8 T cell clones from young nonobese diabetic (NOD) islets can transfer rapid onset of diabetes in NOD mice in the absence of CD4 cells. J. Exp. Med. 1996;183:67–76. doi: 10.1084/jem.183.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Trudeau J.D., Kelly-Smith C., Verchere C.B., Elliott J.F., Dutz J.P., Finegood D.T., Santamaria P., Tan R. Prediction of spontaneous autoimmune diabetes in NOD mice by quantification of autoreactive T cells in peripheral blood. J. Clin. Invest. 2003;111:217–223. doi: 10.1172/JCI16409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anderson B., Park B.J., Verdaguer J., Amrani A., Santamaria P. Prevalent CD8(+) T cell response against one peptide/MHC complex in autoimmune diabetes. Proc. Natl. Acad. Sci. USA. 1999;96:9311–9316. doi: 10.1073/pnas.96.16.9311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Amrani A., Verdaguer J., Serra P., Tafuro S., Tan R., Santamaria P. Progression of autoimmune diabetes driven by avidity maturation of a T-cell population. Nature. 2000;406:739–742. doi: 10.1038/35021081. [DOI] [PubMed] [Google Scholar]
- 22.Lieberman S.M., Evans A.M., Han B., Takaki T., Vinnitskaya Y., Caldwell J.A., Serreze D.V., Shabanowitz J., Hunt D.F., Nathenson S.G. Identification of the beta cell antigen targeted by a prevalent population of pathogenic CD8+ T cells in autoimmune diabetes. Proc. Natl. Acad. Sci. USA. 2003;100:8384–8388. doi: 10.1073/pnas.0932778100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lieberman S.M., Takaki T., Han B., Santamaria P., Serreze D.V., DiLorenzo T.P. Individual nonobese diabetic mice exhibit unique patterns of CD8+ T cell reactivity to three islet antigens, including the newly identified widely expressed dystrophia myotonica kinase. J. Immunol. 2004;173:6727–6734. doi: 10.4049/jimmunol.173.11.6727. [DOI] [PubMed] [Google Scholar]
- 24.Graser R.T., DiLorenzo T.P., Wang F., Christianson G.J., Chapman H.D., Roopenian D.C., Nathenson S.G., Serreze D.V. Identification of a CD8 T cell that can independently mediate autoimmune diabetes development in the complete absence of CD4 T cell helper functions. J. Immunol. 2000;164:3913–3918. doi: 10.4049/jimmunol.164.7.3913. [DOI] [PubMed] [Google Scholar]
- 25.Lamont D., Mukherjee G., Kumar P.R., Samanta D., McPhee C.G., Kay T.W.H., Almo S.C., DiLorenzo T.P., Serreze D.V. Compensatory mechanisms allow undersized anchor-deficient class I MHC ligands to mediate pathogenic autoreactive T cell responses. J. Immunol. 2014;193:2135–2146. doi: 10.4049/jimmunol.1400997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Quinn A., McInerney M.F., Sercarz E.E. MHC class I-restricted determinants on the glutamic acid decarboxylase 65 molecule induce spontaneous CTL activity. J. Immunol. 2001;167:1748–1757. doi: 10.4049/jimmunol.167.3.1748. [DOI] [PubMed] [Google Scholar]
- 27.Busick R.Y., Aguilera C., Quinn A. Dominant CTL-inducing epitopes on GAD65 are adjacent to or overlap with dominant Th-inducing epitopes. Clin. Immunol. 2007;122:298–311. doi: 10.1016/j.clim.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 28.Krishnamurthy B., Dudek N.L., McKenzie M.D., Purcell A.W., Brooks A.G., Gellert S., Colman P.G., Harrison L.C., Lew A.M., Thomas H.E., Kay T.W. Responses against islet antigens in NOD mice are prevented by tolerance to proinsulin but not IGRP. J. Clin. Invest. 2006;116:3258–3265. doi: 10.1172/JCI29602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krishnamurthy B., Mariana L., Gellert S.A., Colman P.G., Harrison L.C., Lew A.M., Santamaria P., Thomas H.E., Kay T.W. Autoimmunity to both proinsulin and IGRP is required for diabetes in nonobese diabetic 8.3 TCR transgenic mice. J. Immunol. 2008;180:4458–4464. doi: 10.4049/jimmunol.180.7.4458. [DOI] [PubMed] [Google Scholar]
- 30.Scott G.S., Fishman S., Margalit A., Siew L.K., Chapman S., Wen L., Gross G., Wong F.S. Developing a novel model system to target insulin-reactive CD8 T cells. Ann. N Y Acad. Sci. 2008;1150:54–58. doi: 10.1196/annals.1447.040. [DOI] [PubMed] [Google Scholar]
- 31.Scott G.S., Fishman S., Khai Siew L., Margalit A., Chapman S., Chervonsky A.V., Wen L., Gross G., Wong F.S. Immunotargeting of insulin reactive CD8 T cells to prevent diabetes. J. Autoimmun. 2010;35:390–397. doi: 10.1016/j.jaut.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 32.Holtkamp S., Kreiter S., Selmi A., Simon P., Koslowski M., Huber C., Türeci O., Sahin U. Modification of antigen-encoding RNA increases stability, translational efficacy, and T-cell stimulatory capacity of dendritic cells. Blood. 2006;108:4009–4017. doi: 10.1182/blood-2006-04-015024. [DOI] [PubMed] [Google Scholar]
- 33.Birkholz K., Hombach A., Krug C., Reuter S., Kershaw M., Kämpgen E., Schuler G., Abken H., Schaft N., Dörrie J. Transfer of mRNA encoding recombinant immunoreceptors reprograms CD4+ and CD8+ T cells for use in the adoptive immunotherapy of cancer. Gene Ther. 2009;16:596–604. doi: 10.1038/gt.2008.189. [DOI] [PubMed] [Google Scholar]
- 34.Zhao Y., Moon E., Carpenito C., Paulos C.M., Liu X., Brennan A.L., Chew A., Carroll R.G., Scholler J., Levine B.L. Multiple injections of electroporated autologous T cells expressing a chimeric antigen receptor mediate regression of human disseminated tumor. Cancer Res. 2010;70:9053–9061. doi: 10.1158/0008-5472.CAN-10-2880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pato A., Eisenberg G., Machlenkin A., Margalit A., Cafri G., Frankenburg S., Merims S., Peretz T., Lotem M., Gross G. Messenger RNA encoding constitutively active Toll-like receptor 4 enhances effector functions of human T cells. Clin. Exp. Immunol. 2015;182:220–229. doi: 10.1111/cei.12688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weinstein-Marom H., Pato A., Levin N., Susid K., Itzhaki O., Besser M.J., Peretz T., Margalit A., Lotem M., Gross G. Membrane-attached cytokines expressed by mRNA electroporation act as potent T-cell adjuvants. J. Immunother. 2016;39:60–70. doi: 10.1097/CJI.0000000000000109. [DOI] [PubMed] [Google Scholar]
- 37.Schmidt W., Festenstein H., Ward P.J., Sanderson A.R. Interspecies exchange of beta 2-microglobulin and associated MHC and differentiation antigens. Immunogenetics. 1981;13:483–491. doi: 10.1007/BF00343716. [DOI] [PubMed] [Google Scholar]
- 38.Pedersen L.O., Stryhn A., Holter T.L., Etzerodt M., Gerwien J., Nissen M.H., Thøgersen H.C., Buus S. The interaction of beta 2-microglobulin (beta 2m) with mouse class I major histocompatibility antigens and its ability to support peptide binding. A comparison of human and mouse beta 2m. Eur. J. Immunol. 1995;25:1609–1616. doi: 10.1002/eji.1830250621. [DOI] [PubMed] [Google Scholar]
- 39.Berko D., Carmi Y., Cafri G., Ben-Zaken S., Sheikhet H.M., Tzehoval E., Eisenbach L., Margalit A., Gross G. Membrane-anchored beta 2-microglobulin stabilizes a highly receptive state of MHC class I molecules. J. Immunol. 2005;174:2116–2123. doi: 10.4049/jimmunol.174.4.2116. [DOI] [PubMed] [Google Scholar]
- 40.Margalit A., Sheikhet H.M., Carmi Y., Berko D., Tzehoval E., Eisenbach L., Gross G. Induction of antitumor immunity by CTL epitopes genetically linked to membrane-anchored beta2-microglobulin. J. Immunol. 2006;176:217–224. doi: 10.4049/jimmunol.176.1.217. [DOI] [PubMed] [Google Scholar]
- 41.Gross G., Eshhar Z. Therapeutic potential of T cell chimeric antigen receptors (CARs) in cancer treatment: counteracting off-tumor toxicities for safe CAR T cell therapy. Annu. Rev. Pharmacol. Toxicol. 2016;56:59–83. doi: 10.1146/annurev-pharmtox-010814-124844. [DOI] [PubMed] [Google Scholar]
- 42.Perez S., Fishman S., Bordowitz A., Margalit A., Wong F.S., Gross G. Selective immunotargeting of diabetogenic CD4 T cells by genetically redirected T cells. Immunology. 2014;143:609–617. doi: 10.1111/imm.12340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Boczkowski D., Nair S.K., Nam J.H., Lyerly H.K., Gilboa E. Induction of tumor immunity and cytotoxic T lymphocyte responses using dendritic cells transfected with messenger RNA amplified from tumor cells. Cancer Res. 2000;60:1028–1034. [PubMed] [Google Scholar]
- 44.Wong F.S., Moustakas A.K., Wen L., Papadopoulos G.K., Janeway C.A., Jr. Analysis of structure and function relationships of an autoantigenic peptide of insulin bound to H-2K(d) that stimulates CD8 T cells in insulin-dependent diabetes mellitus. Proc. Natl. Acad. Sci. USA. 2002;99:5551–5556. doi: 10.1073/pnas.072037299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Karttunen J., Sanderson S., Shastri N. Detection of rare antigen-presenting cells by the lacZ T-cell activation assay suggests an expression cloning strategy for T-cell antigens. Proc. Natl. Acad. Sci. USA. 1992;89:6020–6024. doi: 10.1073/pnas.89.13.6020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Karttunen J., Shastri N. Measurement of ligand-induced activation in single viable T cells using the lacZ reporter gene. Proc. Natl. Acad. Sci. USA. 1991;88:3972–3976. doi: 10.1073/pnas.88.9.3972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wong F.S., Siew L.K., Scott G., Thomas I.J., Chapman S., Viret C., Wen L. Activation of insulin-reactive CD8 T-cells for development of autoimmune diabetes. Diabetes. 2009;58:1156–1164. doi: 10.2337/db08-0800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Verdaguer J., Schmidt D., Amrani A., Anderson B., Averill N., Santamaria P. Spontaneous autoimmune diabetes in monoclonal T cell nonobese diabetic mice. J. Exp. Med. 1997;186:1663–1676. doi: 10.1084/jem.186.10.1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lewis M.D., de Leenheer E., Fishman S., Siew L.K., Gross G., Wong F.S. A reproducible method for the expansion of mouse CD8+ T lymphocytes. J. Immunol. Methods. 2015;417:134–138. doi: 10.1016/j.jim.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.