Abstract
Kounis syndrome is the concurrence of coronary spasm, acute myocardial infarction or stent thrombosis, with allergic reactions in the setting of mast-cell and platelet activation. In this report Kounis syndrome manifesting as stent thrombosis with left ventricular thrombus formation was triggered by a food-induced allergic reaction. The allergic reaction to food was confirmed by oral rice pudding ingredients challenge test while skin tests were inconclusive. To our knowledge, this is first report of early stent thrombosis secondary to food allergic reaction in a 70-year-old man patient who was found to have left ventricular thrombus and undiagnosed hypertrophic cardiomyopathy.
Keywords: Allergic myocardial infarction, Allergic reaction, Kounis syndrome, Stent thrombosis
Core tip: Kounis syndrome highlights, the role of anaphylactic mediated acute coronary syndromes complicating stent thrombosis in the era of invasive treatment of coronary artery disease. Drugs, stings, bites, contrast material, atopic diathesis and even food ingestion could be the culprits. Managing the complex pathophysiology of this condition is a challenging issue, especially in the emergency setting, that requires rapid treatment decisions. The role of detailed past history and of preventive anti-allergic medication in high risk patients with anaphylactic reactions should be considered in randomized studies.
INTRODUCTION
Kounis syndrome is a variety of acute coronary syndromes triggered by the release of inflammatory mediators following an allergic insult[1]. Stent thrombosis is a rare, but serious, complication that is strongly associated with severe morbidity and mortality. Stent thrombosis associated with allergic mediated inflammatory reaction has been described as a serious manifestation of Kounis syndrome[2-4]. Several reports exist in the medical literature on patients with coronary stent implantation who developed stent thrombosis, concurrently with an allergic reaction manifesting as Kounis syndrome. Such reactions had been triggered by non anionic contrast material iopromide, flavonate-propyphenazone, non steroidal anti-inflammatory agent acemetacine, insect stings, snake bite and clopidogrel, the drug that is given itself to prevent stent thrombosis[5-10]. In the following report we describe a patient who suffered early stent thrombosis with left ventricular thrombus formation triggered by an allergic reaction following food consumption. To the best of our knowledge, this is the first case of early stent thrombosis associated with food-induced allergy reaction.
CASE REPORT
A 70-year-old man smoker with a previous history of a transient ischemic attack, was referred to the emergency department of our hospital because of a pain to the left shoulder and arm that had started 4 d ago and was unresponsive to analgesics.
Upon admission, the electrocardiogram showed anteroseptal ST elevation myocardial infarction (Figure 1A) and transthoracic echocardiography revealed left ventricular hypertrophy, that was more pronounced at the interventricular septum, compatible with hypertrophic cardiomyopathy. Additional findings were an apical aneurysm, and moderate attenuation of systolic function. High sensitivity troponin I was elevated to 11037 ng/L. The patient was transferred to the coronary care unit and the next day coronary angiography revealed left anterior descending artery occlusion at the mid-level (Figure 1B). Subsequently, he was submitted to balloon angioplasty with placement of a drug-eluting stent (Resolute Integrity, 3 mm × 18 mm, Figure 1C). The patient remained asymptomatic and was discharged under optimal medical treatment including aspirin, clopidogrel, simvastatin, metoprolol, furosemide, lisinopril and eplerenone.
Figure 1.
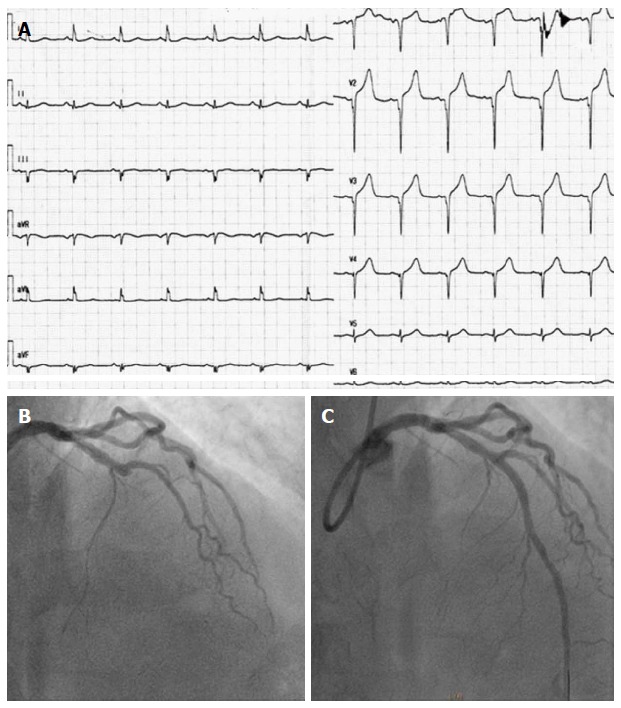
First presentation with acute coronary syndrome. A: Electrocardiograph upon admission; B: Coronary angiography showing critical stenosis in left anterior descending; C: After implantation of resolute integrity drug-eluting stent.
Four days later and about 20 min after taking his evening medication that was metoprolol and simvastatin and during ingestion of Greek rice pudding made of sheep milk, rice and sugar, the patient started gradually to develop lip swelling and itching followed by erythematous rash in all over his body. Within, approximately, 15 min he complained of chest pain and discomfort spreading to the left shoulder and arm. He was immediately transferred to the emergency department of our hospital. On arrival, the patient was covered in all his body with rash accompanied by itching and angioedema of the lips. The electrocardiogram showed ST elevation in V1-V4 leads (Figure 2A). Hydrocortisone and dimetindene maleate was given intravenously together with oral desloratadine and he was transferred to the catheterization laboratory, where coronary angiography revealed stent thrombosis with left anterior descending coronary artery occlusion (Figure 2B). The patient underwent thrombus aspiration that was followed by an additional stent placement (stent in stent procedure, drug eluting stent 3 mm × 16 mm, Figure 2C). However, mild chest pain remained for about 2 h and was attributed to “no reflow” phenomenon. Transthoracic echocardiography revealed, apart from hypertrophic cardiomyopathy with asymmetrical septal hypertrophy, also thrombus formation in an apical aneurysm (Figure 2E and F) necessitating heparin infusion. Contrast-echocardiography with Sonovue-Sulfur hexafluoride microbubbles revealed sessile apical thrombus (Figure 2F). Tryptase was elevated confirming an allergic reaction. The patient had an uneventful recovery and was scheduled for discharge after an allergology investigation.
Figure 2.
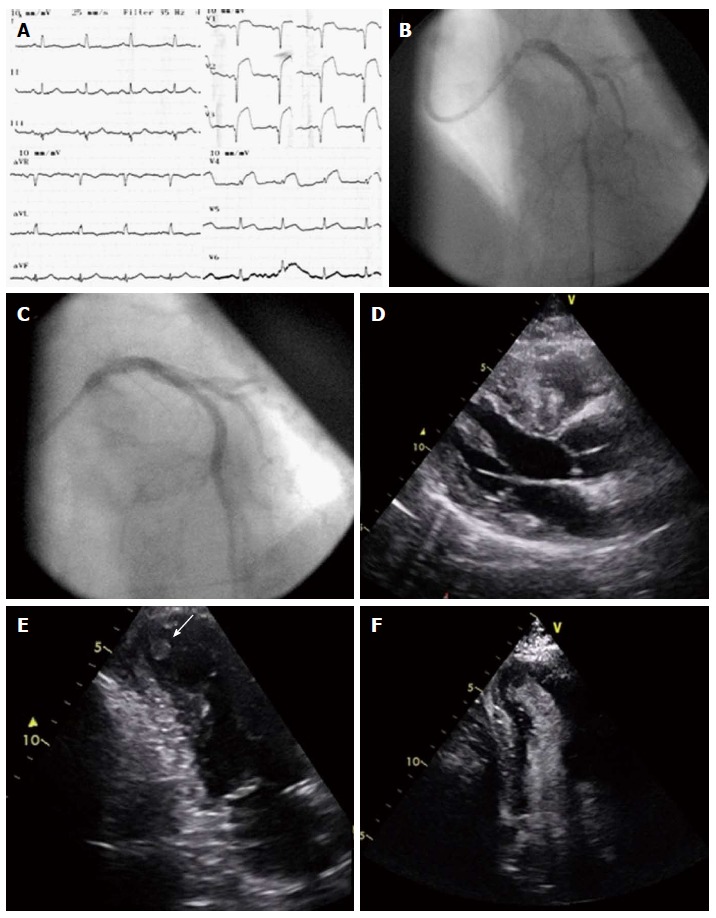
Kounis syndrome following rice pudding consumption. A: Electrocardiograph upon admission; B: Coronary angiography showing stent thrombosis; C: After implantation of drug-eluting stent (stent in stent); D: Parasternal long axis view showing excessive hypertrophy of the septum; E: Thrombus in aneurysmatic apex, apical 2-chamber view; F: Contrast derived image, with thrombus in the apex, apical 2-chamber view.
Oral food challenge test
In order to identify what had triggered the allergic reaction, skin prick tests were performed, under strict hemodynamic monitoring, for simvastatin and metoprolol that were the drugs the patient was taking after the first episode, and were inconclusive. Subsequently, it was decided to proceed to an oral food challenge test, again under strict hemodynamic monitoring, using the rice putting ingredients that were sheep milk, rice and sugar according to the protocol described previously[11]. Following an initial amount of 0.6 g of sheep milk given slowly and 15 min after swallowing of 5 g of sheep milk the patient suddenly felt unwell, dizzy, started sweating, developed urticarial rash and complained of severe dyspnea. Soon after, he became disorientated and sleepy. On examination, he was pale with bronchospasm accompanied by hypoxemia (SpO2 82%), and sinus tachycardia (110/60 mmHg, 125 bpm), feeling itchy but without electrocardiographic changes. He was immediately treated with 250 mg hydrocortisone intravenously, 4 mg dimetindene maleate intravenously and 5 mg desloratadine orally with improvement in signs and symptoms. He gradually became stable and asymptomatic. Blood examinations, 10 min after onset of symptoms were performed for troponin, IgE antibodies and tryptase. Troponin was not increased, eosinophils were 70/μL, but IgE levels were increased to > 1000 IU/mL (normal values: 1-183 IU/mL). We did not proceed to challenge the patient with rice or sugar on ethical grounds, while the patient recalled that he was apprehended to sheep milk in the past.
He had an uncomplicated hospital follow-up and was discharged with the advice neither to eat rice pudding nor to drink sheep’s milk again.
DISCUSSION
Acute myocardial infarction after a prolonged allergic reaction was firstly described in 1950[12]. However, a detailed description of the allergic angina syndrome progressing to acute myocardial infarction was described in 1991 by Kounis et al[13]. Three variants of Kounis syndrome have been described so far[14]: Type I that includes patients with normal coronary arteries in whom the acute release of inflammatory mediators can induce coronary artery spasm that could progress to acute myocardial infarction. Type II that includes patients with culprit and quiescent atheromatous disease in whom the acute release of inflammatory mediators may induce plaque erosion or rupture manifesting as acute myocardial infarction. The type III variant includes coronary artery stent thrombosis in the setting of allergic or hypersensitivity and anaphylactic or anaphylactoid insults. In this type, the thrombus is infiltrated by eosinophils and/or mast cells.
The patient was found to have a previously undiagnosed hypertrophic cardiomyopathy with septal hypertrophy and apical thrombus formation. Coexisting of hypertrophic cardiomyopathy with coronary spasm is not frequent and clinical characteristics in patients with both diseases have not been clarified yet. However, in a study of 36 patients with hypertrophic cardiomyopathy challenged with acetylcholine provocation test coronary vasospasm was induced in 10 (28%). The conclusion was that coronary vasospasm appears to play a significant role in the etiology of myocardial ischemia in patients with hypertrophic cardiomyopathy and smoking, as in our patient, might be a major risk factor for coexistence of coronary vasospasm[15].
The apical thrombus formation could be attributed to pre-existing ischemic disease with aneurysmal dilatation of the apex. However, the activation of the thrombotic path during Kounis syndrome may have played an additional role. Indeed, platelet surface membrane contains, not only the well known receptors for thromboxane, adenosine diphosphate, IIb/IIIa but additional receptors for multiple exogenous agonists which contribute to platelet activation. These include receptors for thrombin, serotonin, epinephrine collagen, platelet activating factor and histamine[16]. Additionally, a subset of platelets bear in their surface high and low affinity FCγRI, FCγRII, FCεRI and FRεRII IgE receptors[17] that are activated during hypersensitivity responses.
The anaphylactic reaction was confirmed during hospitalization with oral food consumption test and it was found that the patient was allergic to sheep milk. Tryptase levels were not elevated and this might be due to blood sample collection soon after the onset of symptoms, and according to tryptase kinetics these levels are found to elevate later[18]. Immunoglobulin E antibodies were highly elevated that explains the IgE-mediated allergic reaction. In a study comparing cow milk allergy with sheep and goat milk allergy, it was found that the latter affects older children and appears at a later age. In sheep or goat milk allergic patients, the IgE antibodies recognize the caseins but not the whey proteins. Moreover, IgE specificity and affinity was high to sheep-goat milk and lower to cow milk caseins despite their marked sequence homology[19].
Both physicians and susceptible individuals should be aware that high risk patients and patients with predisposition to allergies, especially allergy to sheep or goat milk require strict avoidance of such milk and milk derived products as reactions could be severe and life threatening. Vigorous anti-allergic medication and standardized treatment protocol is mandatory in order to prevent allergic insults and catastrophic cardiovascular adverse events.
COMMENTS
Case characteristics
A 70-year-old man with coronary artery disease who suffered early stent thrombosis with left ventricular thrombus formation triggered by a food-induced (sheep milk in rice pudding) allergic reaction and was found by oral food challenge test to be sensitized to sheep milk.
Clinical diagnosis
Clinical diagnosis Kounis syndrome, complicating early stent thrombosis following Greek rice pudding consumption, in a patient with coronary artery disease and hypertrophic cardiomyopathy.
Differential diagnosis
Acute coronary syndrome and anaphylactic shock. Both of them are the two sides of the same coin when investigating the complex pathophysiology of Kounis syndrome.
Laboratory diagnosis
Increased cardiac enzymes, IgE antibodies and tryptase levels.
Imaging diagnosis
Coronary angiography revealed stent thrombosis completely occluding left anterior descending artery. Echocardiography demonstrated left ventricular hypertrophy compatible with hypertrophic cardiomyopathy, an apical aneurysm and moderate attenuation of systolic function with thrombus formation in the apical aneurysm.
Pathological diagnosis
In the acute setting of the coronary syndrome, no thrombus was kept for pathological analysis.
Treatment
The patient underwent balloon angioplasty with placement of a drug-eluting stent in the acute setting of the stent thrombosis. In the second allergic reaction, during the allergic skin tests and the oral food challenge test, he was treated with hydrocortisone, dimetindene maleate and desloratadine with improvement in signs and symptoms of the allergic reaction.
Related reports
To our knowledge, this is the first report of Kounis syndrome with the clinical manifestation of early stent thrombosis after food allergic reaction.
Experience and lessons
Kounis syndrome is “a new twist on an old disease”, which is frequently misdiagnosed. The early diagnosis could improve patients’ outcome and prognosis, while original randomized studies could investigate the role of preventive anti-allergic medication in high risk patients with anaphylactic reactions.
Peer-review
This manuscript is well-written and an interesting case report with addressing type III Kounis syndrome (anaphylactic reaction) induced by food allergy.
Footnotes
Institutional review board statement: This case report conforms to the ethical standards of our institution.
Informed consent statement: The patient involved in this study gave his verbal informed consent authorizing use of his protected health information.
Conflict-of-interest statement: All the authors have no conflicts of interests to declare.
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: Greece
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
Peer-review started: October 11, 2016
First decision: November 10, 2016
Article in press: January 14, 2017
P- Reviewer: Hoshi T, Kettering K, Liu T, Vermeersch P S- Editor: Song XX L- Editor: A E- Editor: Wu HL
References
- 1.Nikolaidis LA, Kounis NG, Gradman AH. Allergic angina and allergic myocardial infarction: a new twist on an old syndrome. Can J Cardiol. 2002;18:508–511. [PubMed] [Google Scholar]
- 2.Biteker M. A new classification of Kounis syndrome. Int J Cardiol. 2010;145:553. doi: 10.1016/j.ijcard.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 3.Chen JP, Hou D, Pendyala L, Goudevenos JA, Kounis NG. Drug-eluting stent thrombosis: the Kounis hypersensitivity-associated acute coronary syndrome revisited. JACC Cardiovasc Interv. 2009;2:583–593. doi: 10.1016/j.jcin.2009.04.017. [DOI] [PubMed] [Google Scholar]
- 4.Venturini E, Magni L, Kounis NG. Drug eluting stent-induced Kounis syndrome. Int J Cardiol. 2011;146:e16–e19. doi: 10.1016/j.ijcard.2008.12.190. [DOI] [PubMed] [Google Scholar]
- 5.Kogias JS, Papadakis EX, Tsatiris CG, Hahalis G, Kounis GN, Mazarakis A, Batsolaki M, Gouvelou-Deligianni GV, Kounis NG. Kounis syndrome: a manifestation of drug-eluting stent thrombosis associated with allergic reaction to contrast material. Int J Cardiol. 2010;139:206–209. doi: 10.1016/j.ijcard.2008.08.026. [DOI] [PubMed] [Google Scholar]
- 6.Patanè S, Marte F, Di Bella G, Chiofalo S, Currò A, Coglitore S. Acute myocardial infarction and Kounis syndrome. Int J Cardiol. 2009;134:e45–e46. doi: 10.1016/j.ijcard.2007.12.075. [DOI] [PubMed] [Google Scholar]
- 7.Greif M, Pohl T, Oversohl N, Reithmann C, Steinbeck G, Becker A. Acute stent thrombosis in a sirolimus eluting stent after wasp sting causing acute myocardial infarction: a case report. Cases J. 2009;2:780. doi: 10.4076/1757-1626-2-7800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akyel A, Murat SN, Cay S, Kurtul A, Ocek AH, Cankurt T. Late drug eluting stent thrombosis due to acemetacine: type III Kounis syndrome: Kounis syndrome due to acemetacine. Int J Cardiol. 2012;155:461–462. doi: 10.1016/j.ijcard.2011.12.032. [DOI] [PubMed] [Google Scholar]
- 9.Karabay CY, Can MM, Tanboğa IH, Ahmet G, Bitigen A, Serebruany V. Recurrent acute stent thrombosis due to allergic reaction secondary to clopidogrel therapy. Am J Ther. 2011;18:e119–e122. doi: 10.1097/MJT.0b013e3181cdb98c. [DOI] [PubMed] [Google Scholar]
- 10.Kounis NG, Soufras GD. Coronary stent thrombosis: beware of an allergic reaction and of Kounis syndrome. Indian Heart J. 2014;66:153–155. doi: 10.1016/j.ihj.2013.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wainstein BK, Saad RA. Repeat oral food challenges in peanut and tree nut allergic children with a history of mild/moderate reactions. Asia Pac Allergy. 2015;5:170–176. doi: 10.5415/apallergy.2015.5.3.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pfister CW, Plice SG. Acute myocardial infarction during a prolonged allergic reaction to penicillin. Am Heart J. 1950;40:945–947. doi: 10.1016/0002-8703(50)90191-8. [DOI] [PubMed] [Google Scholar]
- 13.Kounis NG, Zavras GM. Histamine-induced coronary artery spasm: the concept of allergic angina. Br J Clin Pract. 1991;45:121–128. [PubMed] [Google Scholar]
- 14.Kounis NG, Mazarakis A, Tsigkas G, Giannopoulos S, Goudevenos J. Kounis syndrome: a new twist on an old disease. Future Cardiol. 2011;7:805–824. doi: 10.2217/fca.11.63. [DOI] [PubMed] [Google Scholar]
- 15.Kodama K, Hamada M, Kazatani Y, Matsuzaki K, Murakami E, Shigematsu Y, Hiwada K. Clinical characteristics in Japanese patients with coexistent hypertrophic cardiomyopathy and coronary vasospasm. Angiology. 1998;49:849–855. doi: 10.1177/000331979804900909. [DOI] [PubMed] [Google Scholar]
- 16.Shah BH, Lashari I, Rana S, Saeed O, Rasheed H, Arshad Saeed S. Synergistic interaction of adrenaline and histamine in human platelet aggregation is mediated through activation of phospholipase, map kinase and cyclo-oxygenase pathways. Pharmacol Res. 2000;42:479–483. doi: 10.1006/phrs.2000.0721. [DOI] [PubMed] [Google Scholar]
- 17.Hasegawa S, Pawankar R, Suzuki K, Nakahata T, Furukawa S, Okumura K, Ra C. Functional expression of the high affinity receptor for IgE (FcepsilonRI) in human platelets and its’ intracellular expression in human megakaryocytes. Blood. 1999;93:2543–2551. [PubMed] [Google Scholar]
- 18.Kounis NG. Serum tryptase levels and Kounis syndrome. Int J Cardiol. 2007;114:407–408. doi: 10.1016/j.ijcard.2005.11.088. [DOI] [PubMed] [Google Scholar]
- 19.Ah-Leung S, Bernard H, Bidat E, Paty E, Rancé F, Scheinmann P, Wal JM. Allergy to goat and sheep milk without allergy to cow’s milk. Allergy. 2006;61:1358–1365. doi: 10.1111/j.1398-9995.2006.01193.x. [DOI] [PubMed] [Google Scholar]


