Abstract
We evaluated the long-term clinical results of acute complete acromioclavicular dislocations treated by reconstruction of the acromioclavicular and coracoclavicular ligament using trapezius muscle fascia. Open reduction and internal fixation was performed using the clavicular hook plate in 12 patients with acute complete acromioclavicular joint dislocation, and the acromioclavicular and coracoclavicular ligaments were reconstructed using trapezius muscle fascia. Radiographic evaluations were conducted postoperatively. We evaluated the functional results with constant scoring system and radiological results at the final follow-up visit. The mean Constant score at the final follow-up visit was 91.67 (range, 81 to 100). The results were excellent in eight patients (66.7%) and good in four patients (33.3%). Three patients with scores from 80 to 90 had mild pain during activity, but this did not affect the range of motion of the shoulder. All patients have returned to their preoperative work without any limitations. Compared with the contralateral side, radiography showed anatomical reposition in the vertical plane in all cases. The hook-plate fixation with ligament reconstruction was successful in treating AC dislocations. The acromioclavicular and coracoclavicular ligament were reconstructed by trapezius muscle fascia that keep the distal clavicle stable both vertically and horizontally after type III injuries.
Keywords: Acromioclavicular joint, dislocation, fixation, ligament
1 Introduction
Although surgical treatment has been proposed for acromioclavicular (AC) joint dislocation since before the antiseptic era, the most effective therapy for this injury remains ambiguous. AC joint dislocation can occur through direct or indirect injury mechanisms. Several methods for restoring AC joint dislocations have been reported, including: AC joint pins or screw fixation, using a hook plate or Wolter’s crook plate, coracoclavicular (CC) fixation, using a CC screw or anchor suture polydioxanonsulphate (PDS) bands, Dacron or Mersilene suture fixation and tension band wire fixation.
In the 1960s, Tossy et al. offered three grades of AC joint injuries, according to the extent of displacement of the clavicular end relative to the acromion [1]. Tossy grade III injuries are the most traumatic and severe, with substantial breakdown of the soft tissues around the AC joint. Early operation is recommended for these injuries. However, the results of the internal fixation of acute Tossy grade III AC joint injuries are usually unsatisfactory because the AC and CC ligaments have been completely torn, and it is difficult to suture the retracted ends of the ligaments. Complications from such repairs include subacromial ulceration, perforation, and recurrent AC joint dislocation after plate removal, and even rupture as a result of the clavicular hook plate. Torn AC and CC ligaments need be reconstructed correctly to maintain long-term joint stability.
Different open and arthroscopic surgical techniques are available for the reconstruction of ruptured ligaments. One such technique involves transferring the coracoacromial ligament to the distal part of the clavicle, and suturing the ligament with absorbable or nonabsorbable sutures. Weaver first described the use of the native coracoacromial ligament to reestablish AC joint stability [2]. Morrison et al. used an arthroscopically assisted technique with a semi-tendinosus allograft to reconstruct the AC joint [3]. The results, although good, were not entirely satisfactory, as the reconstructed ligament connected the clavicle and acromion so firmly that rotational movement was restricted between the clavicle and scapula during humeral motion.
To explore a new method for reconstructing the AC ligament and to prevent recurrent AC joint dislocation after removal of the clavicular hook plate, the AC and CC ligaments were reconstructed using the trapezius muscle fascia, and the AC joint was then fixed with a hook plate. The aim of this study was to estimate the long-term clinical results of this method in 12 patients with acute Tossy grade III AC joint dislocation, and to observe any fascial metaplasia.
2 Methods
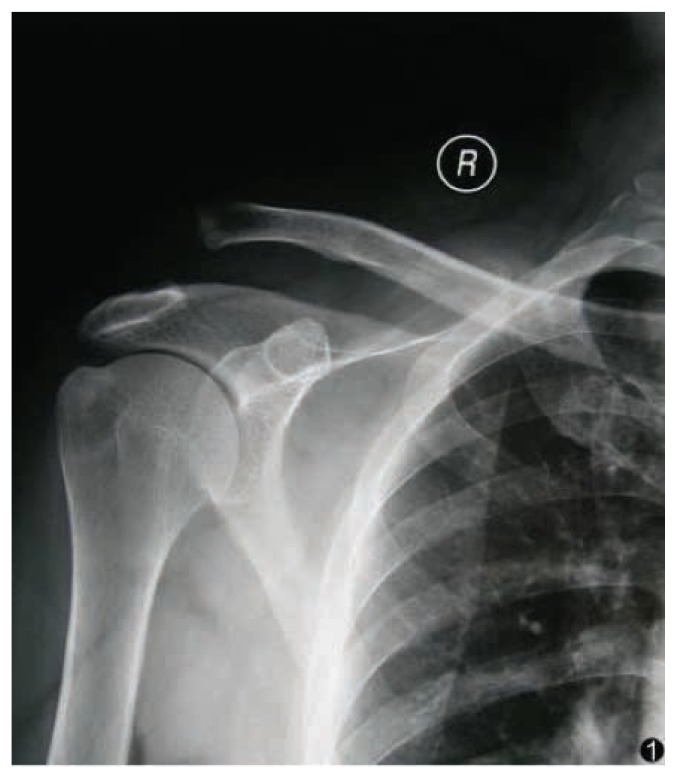
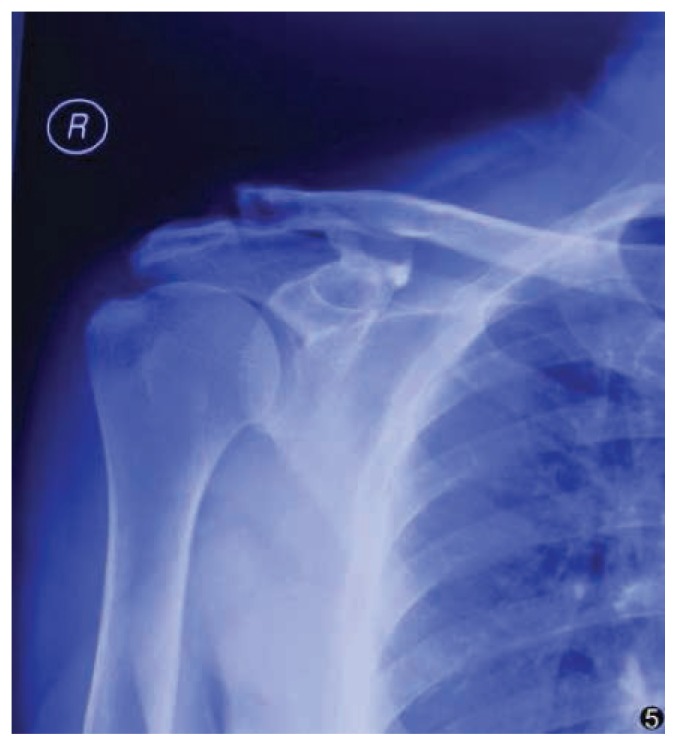
Between August 2008 and May 2012, 12 patients with acute complete AC joint dislocations (8 males, 4 females; mean age 36.08 years; range, 19 to 59 years) were recruited to this study. According to the typical history of shoulder injuries, radiograph results, and Tossy classification, [1] all patients were confirmed as having Tossy grade III injuries (Fig. 1). Table 1 shows the demographic data, follow-up duration, and mechanism of injury for each patient.
Figure 1.
A 55-year-old man fell from a motorcycle. A preoperative radiograph of his shoulder showed a complete acromioclavicular joint dislocation (Tossy grade III).
Table 1.
Detailed data of 12 patients with acute type III AC joint dislocations.
| Case | Age (years) | Sex | Injured Side | Dominant Shoulder | Mechanism | Duration of follow-up (months) | Constant score | Functional results | Time interval before surgery (days) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 19 | M | R | R | T | 16 | 100 | Excellent | 1 |
| 2 | 33 | M | L | R | Fa | 24 | 91 | Excellent | 3 |
| 3 | 25 | F | R | R | T | 18 | 95 | Excellent | 2 |
| 4 | 41 | M | R | R | T | 20 | 91 | Excellent | 4 |
| 5 | 20 | M | R | R | T | 19 | 99 | Good | 1 |
| 6 | 55 | M | R | R | Fa | 38 | 86 | Good | 5 |
| 7 | 42 | M | R | R | T | 17 | 83 | Excellent | 3 |
| 8 | 38 | M | L | L | T | 27 | 92 | Excellent | 2 |
| 9 | 59 | F | R | R | Fa | 19 | 81 | Good | 8 |
| 10 | 41 | F | R | R | T | 31 | 93 | Good | 2 |
| 11 | 26 | M | L | R | T | 25 | 98 | Excellent | 3 |
| 12 | 34 | F | R | R | T | 20 | 91 | Excellent | 2 |
| Mean | 36.08±12.65 | 22.83±6.26 | 91.67±6.02 | 3±1.95 |
M, male; F, female; L, left; R, right; Fa, falling accident; T, traffic accident
2.1 Surgical techniques
Under nerve block anesthesia, the affected shoulder was elevated using a single sand bag. During operation, the patient was in a semi-seated position. The operative fields were prepared and draped as usual. A longitudinal skin incision of 7–8 cm was made to expose the AC joint, the lateral aspect of the acromion, and the coracoid process. The dislocated AC joint was exposed after the subcutaneous incision. The coracoid process and the torn CC ligament were exposed simultaneously. The intra-articular meniscus was removed if damaged.
After open reduction of the AC joint, the lateral end of the plate was inserted deeply to the acromion and levered down on the clavicle to reduce the joint. It was secured to the clavicle with cortical or lock screws, depending on the condition of the bone. The trapezius was exposed using sharp dissection. A flap was designed on the trapezius muscle fascia to have turn points on the acromion. The length of the trapezius muscle fascia flap was the distance from the acromion to the coracoacromial ligament plus 3 cm. The extra 3 cm of fascia would be inserted in the gap between the clavicle and coracoid, and the broken ends of the coracoclavicular ligament were sutured using it. The maximum size of the flap was 12 × 3 × 1 cm.
Dissection proceeded from the distal to proximal direction to free the flap from the trapezius muscle. During flap dissection, several minor pedicles were encountered that radiated from the trapezius. These pedicles were carefully ligated and dissected, to allow sufficient flap mobility. The dissection was stopped at about 2 cm proximal to the acromion. During dissection, the major pedicle did not need to be skeletonized. For a sufficient rotation arc of the flap, the muscle could be freed from its origin for added mobility. The muscle flap was carefully handled with delicate instruments. It was rotated to the clavicle and coracoid, taking care not to stretch or kink the major pedicle.
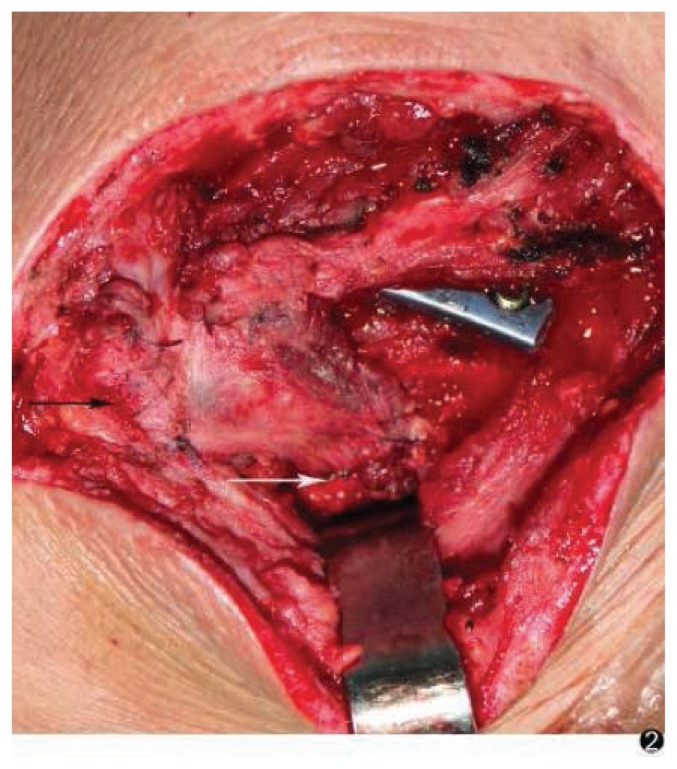
Sections of redundant muscle fascia were sampled for staining with hematoxylin and eosin postoperatively. The flap covered the AC joint, and the free part of the flap filled the space between the ruptured CC ligaments. It was sutured to the ligament with 2.0 vicryl sutures. The anterior, superior, and posterior AC ligaments were all repaired and sutured to the flap with 2.0 vicryl sutures (Fig. 2). The wound was irrigated, a 1/8-inch hemovac drain was inserted, and the wound was closed in layers.
Figure 2.
The AC ligament (black arrow) and CC ligament (white arrow) were reconstructed using trapezius muscle fascia.
2.2 Postoperative management
Postoperatively, an arm sling was used for 3 weeks. Pendulum shoulder exercises were started from the fourth postoperative day. Vigorous exercises and heavy lifting were forbidden for 6 weeks after surgery. Contact sports were forbidden for 3 months postoperatively. After this period, patients were encouraged to strengthen the shoulder joint by functional exercises, including passive pendulum exercises and active “crawling up the wall” exercises, to avoid joint stiffness and heterotopic ossification. Every 4 to 6 weeks after surgery, patients returned to the outpatient clinic for clinical and radiographic follow-up for 12 months. The most recent radiographic films and functional evaluations were used for analysis. Plate removal was performed after approximately 6 months under nerve block anesthesia.
All patients received clinical follow-up, as assessed by clinical results and radiographic follow-ups. Functional results were evaluated at the last follow-up visit by using the Constant scoring system [4]. The Constant score combines subjective symptom scores (35%), which assess pain and vocational activities, and objective scores (65%), which measure range of motion and shoulder strength. The score values range from 0 to 100, with higher scores indicating better shoulder function.
Radiographic evaluations were routinely conducted every 3 weeks until 6 months postoperatively. We used the method described by Pavlik et al. to evaluate the vertical distance between the inferior border of the acromion and the clavicle compared to the contralateral side; differences were measured in millimeters (<2 mm, anatomical reposition; 2–4 mm, slight loss of reduction; 4–8 mm, partial loss of reduction; >8 mm, total loss of reduction) [5].
Ethical approval
The research related to human use has been complied with all the relevant national regulations, institutional policies and in accordance the tenets of the Helsinki Declaration, and has been approved by the authors’ institutional review board or equivalent committee.
Informed consent
Informed consent has been obtained from all individuals included in this study.
3 Results
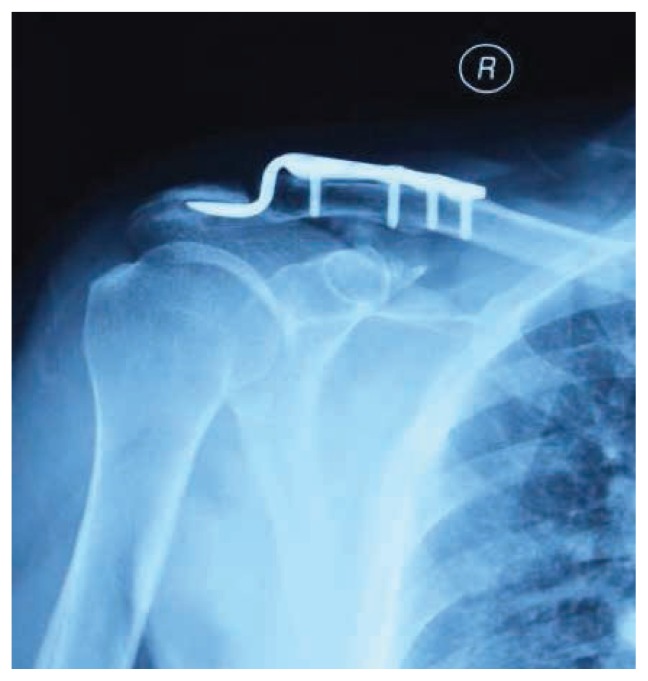
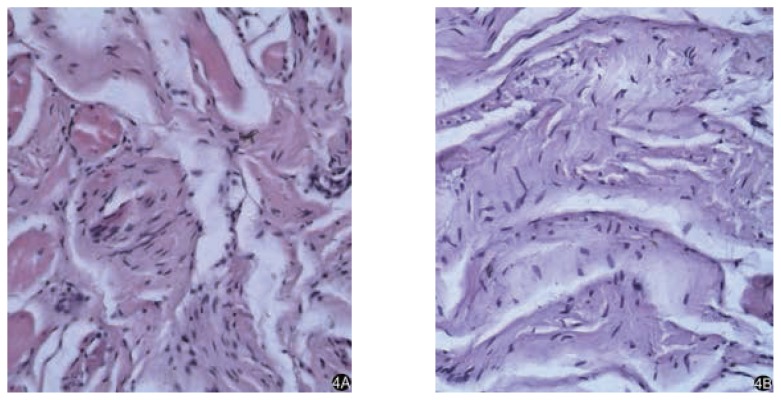
All CC ligaments were torn within the mid-section and at the sides of the coracoid process. The reduction of the AC joint was immobilized by a clavicular hook plate (Fig. 3). The AC and CC ligaments were reconstructed using a trapezius muscle fascia flap. Follow-up times ranged from 16 to 38 months (mean, 22.83 ± 6.26 months). Muscle fascia samples stained with hematoxylin and eosin showed striated muscle cells (Fig. 4A). Six months after surgery, repeat muscle fascia sampled during the second operation showed numerous fibroblast cells (Fig. 4B).
Figure 3.
Postoperative radiograph of the same patient showed an ideal reduction of the acromioclavicular joint and correct position of the hook plate.
Figure 4.
A) Muscle fascia sampled in the first operating stained with hematoxylin and eosin was showed striated muscle cell (original magnification ×200). B) Fascia flap is turning into a ligament-like structure (original magnification ×200).
In the final stages of follow-up, the average Constant score was 91.67 ± 6.02 (range, 81 to 100). Nine patients scored above 90, and three scored between 80 and 90 (Table 1). The mean score for the uninjured shoulder was not significantly different (94.12 ± 7.15; range, 92–100; p = 0.512). There were no signs of recurrent joint dislocation (Fig. 5). All patients have now returned to their preoperative work without any limitations (Fig. 6A), and no patient showed a decrease of muscle strength (Fig. 6B).
Figure 5.
Thirty-eight months postoperatively, a radiograph of the same patient demonstrated the ideal reduction of acromioclavicular joint.
Figure 6.
Thirty-eight months postoperatively, the motion of the acromioclavicular joint is normal (A), and the function of the trapezius muscle is not affected (B).
The difference between the inferior border of the acromion and the clavicle compared to the contralateral side was 1.645 ± 0.37 mm. Five patients (41.7%) experienced mild pain during activities postoperatively. The symptoms of shoulder pain and soreness were exacerbated by wet and cold weather. No other complications were observed.
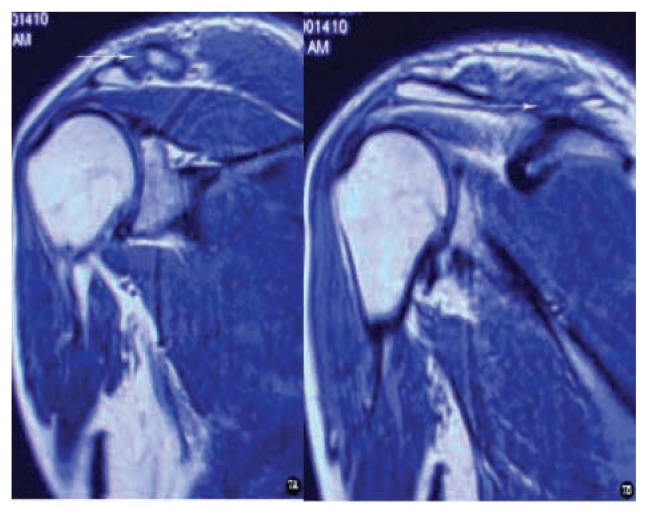
Thirty-eight months after surgery, MRI imaging showed progressive healing of the reconstructed AC (Fig. 7A, white arrow) and CC (Fig. 7B, white arrow) ligaments. Signals at the tendon-bone boundary zone were similar to those of normal structures.
Figure 7.
Thirty-eight months after surgery, MRI imaging showed progressive healing of the reconstructed acromioclavicular (A, white arrow) and coracoclavicular (B, white arrow) ligaments.
4 Discussion
In a Tossy grade III AC joint injury, the AC joint is completely dislocated, and the AC and CC ligaments are ruptured. These injuries often arise from high-energy impacts caused by traffic accidents. Early surgical treatment is strongly recommended to stabilize the AC joint and promote restoration of the ligaments [6–10]. Suggested surgical techniques mainly include direct fixation using metal plates across the AC joint or indirect approaches that involve suturing the ligament to stabilize the AC joint. There are many methods for the fixation of AC joint dislocations. Transarticular AC fixations with K-wires or screws are commonly used [11]. One of the most popular methods of fixation is pin fixation using either smooth or threaded Kirschner wires after a closed or open reduction. K-wire migration, which is relatively rare, can have serious complications, and this surgical method has been abandoned [12,13].
Fixation between the clavicle and coracoid using a screw has been reported [14]. Drawbacks of this approach include the technical difficulty of screw placement and the high rates of failure and complications; additionally, secondary procedures are necessary to remove the screw [15,16]. Because of the long lever arm of the screw between the clavicle and scapula, this fixation method is weak in terms of the resistance of anteroposterior translation and the sagittal plane rotation of the AC joint. Loosening usually occurs between the screw and the bone interface in the scapula. Furthermore, a Bosworth screw may break when the shoulder is mobilized early and the screw then has to be removed [18].
The clavicle hook plate is a convenient device that has been commonly used in Europe [18].We used an AO plate, which is either right- or left-sided. The plate is designed so that it is placed on the superior part of the clavicle. The hook of the plate is passed below the acromion posterior to the AC joint, thus not interfering with the joint. This plate has previously been used in the management of AC joint dislocation. 9 The main concern using the hook-plate is subacromial impingement. Other described complications are widening of the hook hole in the acromion, calcification, and diastasis or recurrent dislocation of the AC joint after plate removal [19,20]. If the clavicular hook plate is placed for a long time, then complications are more likely. Healing of the AC and CC ligaments can share the subacromial pressure from the hook of plate. Therefore, the combination of ligaments reconstructed with hook-plate fixation has to prevent subacromial impingement. The hook plate design simply provides superior stability of the AC joint. The provided fixation is not sufficient to allow the torn AC and CC ligaments to heal in their normal anatomical positions. The weak mechanical strength of the healed AC joint stabilizers may lead to the development of short- or long-term complications, including distal clavicle erosion or fracture, coracoid fractures, aseptic foreign body reactions, infections, and AC joint instability [21].
From anatomical and biomechanical points of view, both static and dynamic stabilizers are very important for AC joint stability and function. The AC and CC ligaments are the key to maintaining stability. To stabilize the lateral clavicle and AC joint, some authors have recommended surgical techniques that employ various suture materials or autograft/allograft tissues to reconstruct the CC ligament [22]. The use of the native coracoacromial ligament to reestablish AC joint stability was first described in 1972 by Weaver [2]. Then, Morrison et al. and Baumgarten et al. used an arthroscopic-assisted technique with a semi-tendinosus allograft to reconstruct the AC joint [3,23]. However, the rotational movement between the clavicle and the scapula during motion of the humerus is restricted with these surgical techniques, particularly with abduction and forward flexion of the shoulder, as it connects the clavicle and acromion so firmly [24].
In cases of Tossy grade III AC dislocation, the AC and CC ligaments are ruptured, and the ends of the ligament retract, which makes suturing difficult. Although we provide strong fixation with this technique, when the AC joint is reduced, the scarring in the AC and CC ligaments weaken their strength. This situation is the main reason for subacromial ulceration, perforation, and even rupturing caused by clavicular hook plate fixation. Furthermore, AC joint dislocation can recur after the plate is removed.
From this study, which had a mean follow-up duration of 22.83 months, no recurrent dislocations occurred, and the function of the trapezius muscle was not affected. The disadvantage of this method is that a second procedure is necessary to remove the plate. Future studies will assess the long-term clinical effects of this fixation and reconstruction technique for AC joint dislocation. Moreover, the molecular mechanisms of the fascial metaplasia need to be further studied.
5 Conclusion
The AC and CC ligaments were reconstructed using trapezius muscle fascia, and the joint space was maintained in the normal position by a clavicular hook plate, which maintained the reconstruction of the ligament healing without tension. After the internal fixation of the AC joint was removed, the normal AC joint was maintained by the tendinous healing of the ligaments as detected histologically. These results showed that when muscle fascia grafting was used, muscle cells differentiate into fibroblasts in some situations. The use of a trapezius muscle fascia flap for ligament reconstruction avoids the need for expensive allogenic tendon transplantations, with associated allogeneic responses and donor site morbidity. Although only a partial fascial flap of the trapezius muscle was used, muscle function did not appear to be affected.
Footnotes
Conflict of interest statement: Authors state no conflict of interest
References
- 1.Tossy JD, Mead NC, Sigmond HM. Acromioclavicular separations: useful and practical classification for treatment. Clin Orthop Relat Res. 1963;28:111–119. [PubMed] [Google Scholar]
- 2.Weaver JK, Dunn HK. Treatment of acromioclavicular injuries, especially complete acromioclavicular separation. J Bone Joint Surg Am. 1972;54:1187–1194. [PubMed] [Google Scholar]
- 3.Morrison DS, Lemos MJ. Acromioclavicular separation reconstruction using synthetic loop augmentation. Am J Sports Med. 1995;23:105–110. doi: 10.1177/036354659502300118. [DOI] [PubMed] [Google Scholar]
- 4.Kirkley A, Griffin S. Scoring systems for the functional assessment of the shoulder. Arthroscopy. 2003;10:1109–1120. doi: 10.1016/j.arthro.2003.10.030. [DOI] [PubMed] [Google Scholar]
- 5.Pavlik A, Csepai D, Hidas P. Surgical treatment of chronic acromiocla-vicular joint dislocation by modified Weaver-Dunn procedure. Knee Surg Sports Traumatol Arthrosc. 2001;5:307–312. doi: 10.1007/s001670100222. [DOI] [PubMed] [Google Scholar]
- 6.Bontempo NA, Mazzocca AD. Biomechanics and treatment of acromioclavicular and sternoclavicular joint injuries. Br J Sports Med. 2010;44:361–9. doi: 10.1136/bjsm.2009.059295. [DOI] [PubMed] [Google Scholar]
- 7.Chillemi C, Franceschini V, Giudici LD. Epidemiology of isolated acromioclavicular joint dislocation. Emerg Med Int. 2013:171609. doi: 10.1155/2013/171609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tomlinson DP, David W, Altchek, Davila J, et al. A modified technique of arthroscopically assisted AC joint reconstruction and preliminary results. Clinical orthopaedics and related research. 2008;466:639–645. doi: 10.1007/s11999-007-0085-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jiang C, Wang M, Rong G. Proximally based conjoined tendon transfer for coracoclavicular reconstruction in the treatment of acromioclavicular dislocation. J Bone Joint Surg Am. 2007;11:2408–2412. doi: 10.2106/JBJS.F.01586. [DOI] [PubMed] [Google Scholar]
- 10.John A, Johansen PW, Grutter E, McFarland G, et al. Acromioclavicular joint injuries, indications for treatment and treatment options. Journal of Shoulder and Elbow Surgery. 2011;20:70–82. doi: 10.1016/j.jse.2010.10.030. [DOI] [PubMed] [Google Scholar]
- 11.Virtanen KJ, Remes VM, Ilkka T, Tulikoura1 A, et al. Surgical treatment of Rockwood grade-V acromioclavicular joint dislocations 50 patients followed for 15–22 years. Acta Orthopaedica. 2013;2:191–195. doi: 10.3109/17453674.2013.775046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hegemann S, Kleining R, Schindler HG, Holthusen H. Kirschner wire migrationin the contralateral lung after osteosynthesis of a clavicular fracture. Unfallchirurg. 2005;108:991–993. doi: 10.1007/s00113-005-0946-8. [DOI] [PubMed] [Google Scholar]
- 13.Regel JP, Pospiech J, Aalders TA, Ruchholtz S. Intraspinal migration of a Kirschner wire 3 months after clavicular fracture fixation. Neurosurg Rev. 2002;25:110–112. doi: 10.1007/s101430100186. [DOI] [PubMed] [Google Scholar]
- 14.Bosworth BM. Acromioclavicular dislocation; end-results of screw suspension treatment. Ann Surg. 1948;1:98–111. doi: 10.1097/00000658-194801000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Galatz LM, Williams GR. Acromioclavicular joint injuries. In: Bucholz RW, Heckman JD, Brown CC, editors. Rockwood and Green’s Fractures in Adults. 6nd ed. Vol. 2. Philadelphia: Lippincott Williams & Wilkins; 2006. pp. 1331–1364. [Google Scholar]
- 16.Mazzocca AD, Sellards R, Garretson R, et al. Injuries to the acromioclavicular joint in adults and children. In: DeLee JC, Drez D Jr, Miller MD, editors. DeLee & Drez’s Orthopaedic Sports Medicine: Principles and Practice. 2nd ed. Vol. 1. Philadelphia: Saunders; 2003. pp. 912–934. [Google Scholar]
- 17.Baumgarten KM, Altchek DW, Cordasco FA. Arthroscopically assisted acromioclavicular joint reconstruction. Arthroscopy. 2006;2:228, 228. doi: 10.1016/j.arthro.2005.12.026. [DOI] [PubMed] [Google Scholar]
- 18.Qingjun L, Miao J, Lin B, Guo Z. Clinical effect of acute complete acromioclavicular joint dislocation treated with micro-movable and anatomical acromioclavicular plate. International journal of medical sciences. 2012;9:725–729. doi: 10.7150/ijms.4726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Henkel T, Oetiker R, Hackenburch W. Treatment of fresh Tossy III acromioclavicular joint dislocation by ligament suture and temporary fixation with the clavicular hooked plate. Swiss Surg. 1997;3:160–166. [PubMed] [Google Scholar]
- 20.Sim E, Schwarz N, Hocker K, et al. Repair of complete acromioclavicular separations using the acromioclavicular-hook plate. Clin Orthop. 1995;314:134–142. [PubMed] [Google Scholar]
- 21.Hessmann M, Gotzen L, Gehling H. Acromioclavicular reconstruction augmented with polydioxanonsulphate bands. Am J Sports Med. 1995;23:552–556. doi: 10.1177/036354659502300506. [DOI] [PubMed] [Google Scholar]
- 22.Shewy MTE, Azizi HE. Suture repair using loop technique in cases of acute complete acromioclavicular joint dislocation. J Orthop Traumatol. 2011;1:29–35. doi: 10.1007/s10195-011-0130-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Habernek H, Schmid I, Walch G. Management of acromioclavicular joint dislocation with the wolter hookplate, One year follow-up of 35 cases. Unfallchirurgie. 1993;19:33–39. doi: 10.1007/BF02588225. [DOI] [PubMed] [Google Scholar]
- 24.Duan X, Zhang H, Zhang H, et al. Treatment of coracoid process fractures associated with acromioclavicular dislocation using clavicular hook plate and coracoid screws. J Shoulder Elbow Surg. 2010;2:22–25. doi: 10.1016/j.jse.2009.09.004. [DOI] [PubMed] [Google Scholar]