Abstract
To compare the role of 99mTc-MIBI SPECT-CT image and US in reoperation of persistent secondary hyperparathyroidism patients. A total of 8 persistent secondary hyperparathyroidism patients underwent parathyroidectomy. The sensitivity and accuracy of US and 99mTc-MIBI images before operation were determined. 9 of 14 surgical resection tissues from 8 persistent secondary hyperparathyroidism patients were confirmed to parathyroid hyperplasia. The results showed that the sensitivities were 77.8% and 100%, respectively, for US and 99mTc-MIBI SPECT-CT images. And the accuracies of US and 99mTc-MIBI dual time planar image and SPECT-CT were 50%, 78.6%, respectively. There was significantly difference between two procedures (P=0.021). The superior and inferior localization of glands were both detected by the ultrasound and scintigraphy. Two ectopic parathyroidism nodules were found by 99mTc-MIBI SPECT-CT imaging, while US provided no consistent findings. There was no significantly difference between two procedures (P=0.3). Although two cases of them were not confirmed by pathology, the iPTH of them (800 and 1429 respectively) were much higher than other four cases (<400) pg/ml. PTX is a safe and effective treatment for the patients with persistent SHPT. 99mTc-MIBI planar and SPECT-CT imaging may provide more helps for clinician’s localization the hyperparathyroidism glands accurately.
Keywords: Secondary hyperparathyroidism, Parathyroidectomy with auto transplantation, 99mTc-MIBI; SPECT-CT, Persistent hyperparathyroidism
1 Introduction
Parathyroidectomy (PTX) is the most effective treatment of refractory secondary hyperparathyroidism (SHPT), which can positively alleviate symptoms, correct the biochemical criterion and reduce the death rate [1]. However, the treatment method might lead to two problems after operation, namely persistent HPT and SHPT. To patients of the kind, PTX is still the only effective treatment method [2] and accurate localization can improve the operation efficiency. In order to prepare the pre-operation localization effect of the ultrasonography (US) and 99mTc-MIBI SPECT-CT, this paper analyzes the clinical data and the radiographic diagnosis of the eight persistent SHPT patients who underwent PTX in China-Japan Friendship Hospital. The report is as below:
2 Research objects and methods
2.1 General data and clinical manifestation
In terms of the protopathy of the eight patients, three suffered from chronic glomerulonephritis (CGN), one from IgA nephropathy (IgAN), one from systemic lupus erythematosus (SLE), two from hemadostenosis nephropathy and one is unclear. All patients have the long-term regular hemodialysis filtration (HDF) experiences. In terms of HDF frequency, one had hemofiltration five times/two weeks and seven three times/week. The general data are shown in Table. Ethical approval: The research related to human use has been complied with all the relevant national regulations, institutional policies and in accordance the tenets of the Helsinki Declaration, and has been approved by the authors’ institutional review board or equivalent committee.
Table 1.
Clinical medical history of patients (Note: NM* stands for 99mTc-MIBI SPECT-CT imaging)
| Patients | gender | age | HDF years | iPTH(pg/ml) | Interval of two PTXs (months) | The number of parathyroid gland hyperplasic nodules | |||
|---|---|---|---|---|---|---|---|---|---|
| Pre-operation PTX for the first time | Pre-operation PTX for the second time | US | NM* | Operation | |||||
| 1 | male | 44 | 8 | 1900 | 1698 | 39 | 2 | 2 | 1 |
| 2 | female | 47 | 16 | 2100 | 1918 | 24 | 2 | 2 | 1 |
| 3 | female | 16 | 11 | 1280 | 1000 | 22 | 1 | 1 | 1 |
| 4 | male | 51 | 17 | 2900 | 2255 | 12 | 1 | 1 | 1 |
| 5 | male | 54 | 18 | 2000 | 339.1 | 60 | 1 | 1 | 0 |
| 6 | male | 36 | 8 | 2300 | 2917 | 64 | 3 | 3 | 3 |
| 7 | male | 56 | 20 | 2800 | 1193 | 72 | 1 | 3 | 2 |
| 8 | female | 59 | 17 | 1000 | 714.2 | 36 | 1 | 1 | 0 |
| Total | 45.4±13.9 | 14.4±4.7 | 2035±662 | 1504±853 | 1504±854 | 12 | 14 | 9 | |
Informed consent: Informed consent has been obtained from all individuals included in this study.
2.2 Diagnostic Imaging
99mTc-MIBI imaging adopts the double detector SPECT-CT (Siemens, Symbia T2) ultra-fine resolution low energy collimator. “Plane+dissection imaging” was conducted of the patients undergoing intravenous injection of 99mTc-MIBI 740MBq after 20min and 2h respectively. At the same time, the patients’ neck underwent the PET-CT scan as usual. In the early period, there was abnormal radioactive concentration in the neck or the upper breast. The delayed imaging showed no significant fade-out. Low-density nodules were found after the integration of PET-CT, which were identified to be the parathyroid glandular tissues with the enhanced function.
American ATIHDI3000 and HPIP color diasonograph with the linear array of detectors and frequency of 7.5~12MHz were adopted. The US of the normal parathyroid glands is hard to display. The enlarged parathyroid glands are manifested as oval or fusiform and hypoechoic nodules, which are quite close to the parathyroid glands, but their envelope functions as an envelope from the parathyroid glandular tissues, thus they can detect the rich blood flow.
2.3 Statistical analysis
Conduct chi-square test with the statistical software, SPSS 17.0. It showed P<0.05, which suggested the statistical significance.
3 Results
3.1 US, 99mTc-MIBI SPECT-CT and operation pathological condition
99mTc-MIBI imaging discovered 14 parathyroid gland heterotopic nodules and US found 12. Among them, ten turned out the same in both tests and two different, in that, US suggested they were parathyroid gland heterotopic nodules while 99mTc-MIBI imaging suggested they were non-heterotopic parathyroid glandular tissues. 99mTc-MIBI imaging discovered four heterotopic heterotopic nodules (nodules in the sternocleidomastoid transplant area, substernal, esophagus parapsidal furrow and aorta ascendens), but US failed to discover them. Refer to out to be 100% (9/9), registering an accuracy rate of 78.6% (11/14); while the US sensitivity diagnosis turned out to be 78% (7/9), registering an accuracy rate of 50% (7/14). The statistical analysis showed that there were no significant differences (P=0.021) between the two. The number of the superior and inferior parathyroid glands turned out the same in both tests. 99mTc -MIBI imaging discovered two heterotopic heterotopic nodules while US did not (Refer to Example 2 for the typical image), but there existed no significant difference (P=0.3) between the two. (See Table 2 and Table 3) 99mTc-MIBI imaging can simultaneously discover the lesion beyond the parathyroid glandular tissues, such as skeleton lesion (brown tumor). (See Example 3) Example 2 Patient (See Fig. 3–5) Example 1 for the typical imaging. Example 1 Patient (See Fig. 1 and Fig. 2).
Table 2.
Comparison of the number of parathyroid glands tested by US and 99mTc-MIBI SPECT-CT imaging
| Nodules | 99mTc-MIBI SPECT-CT | US | ||
|---|---|---|---|---|
| TPR | FPR | TPR | FPR | |
| 14 | 9 | 5 | 7 | 7 |
Table 3.
Comparison of the number of superior and inferior parathyroid glands and inferior heterotopic parathyroid glands tested by US and 99mTc-MIBI SPECT-CT and verified by the pathologically
| Upper pole | inferior pole | ectopia | total | |
|---|---|---|---|---|
| US | ||||
| Positive | 6 | 1 | 0 | 7 |
| Negative | 0 | 0 | 2 | 2 |
| 99mTc-MIBI | ||||
| Positive | 6 | 1 | 2 | 9 |
| Negative | 0 | 0 | 0 | 0 |
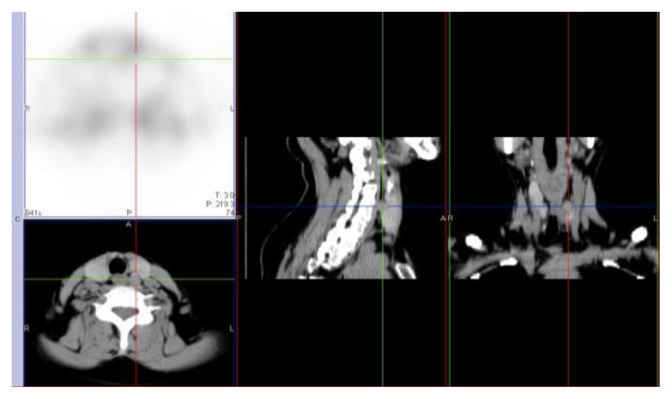
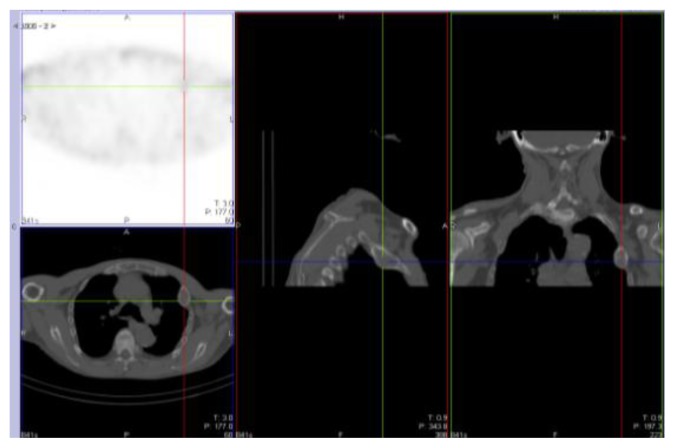
Fig. 3.
99mTc-MIBI 15min plane imaging of substernal heterotopic parathyroid glands (arrows)
Fig. 4.
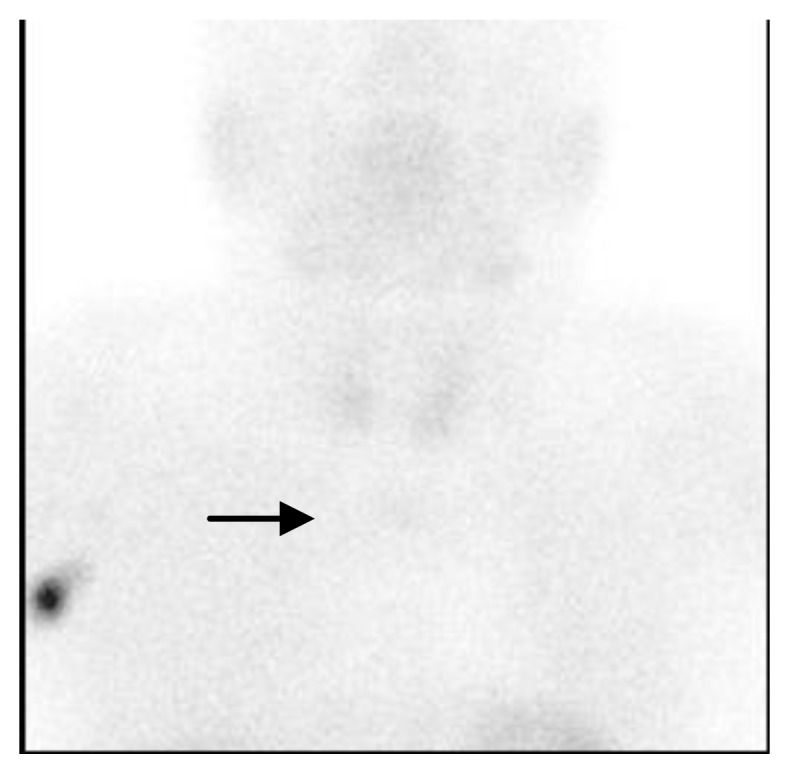
99mTc-MIBI 2h plane imaging of substernal heterotopic parathyroid glands (arrows)
Fig. 5.
99mTc-MIBI SPECT-CT image of substernal heterotopic parathyroid glands(cross) Example 3 Patient (See Fig. 6)
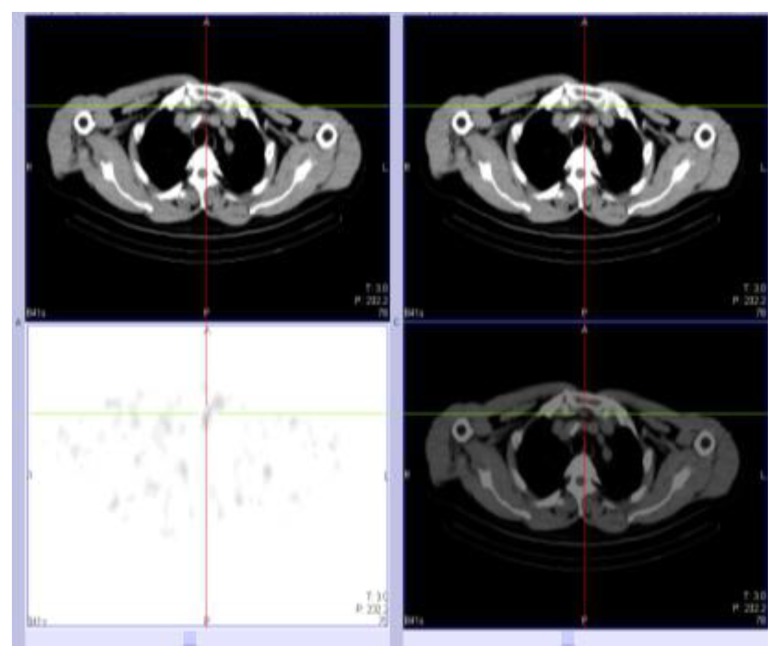
Fig. 1.
US image of parathyroid gland hyperplastic nodules in the upper rear medium of left lobe of the parathyroid gland (arrows)
Fig. 2.
99mTc-MIBI SPECT-CT image of parathyroid gland hyperplastic nodules in the upper rear medium of left lobe of the parathyroid gland (cross)
Eight patients who underwent PTX had 14 tissues removed in total. The pathological result of the other two parathyroid glandular nodules located in the esophagus parapsidal furrow and the aorta asendens failed to be obtained due to great operational difficulty. The final pathological result was: there were nine parathyroid glandular heterotopic nodules (including five nodositas hyperplasia in the neck, two adenoma hyperplasia in the neck, one parathyroid glandular transplanted nodositas in the sternocleidomastoid and one retrosternal heterotopic nodositas hyperplasia); while the remaining five tissues did not show the heterotopic parathyroid glandular tissues.
The 99mTc-MIBI SPECT-CT sensitivity diagnosis turned out to be 100% (9/9), registering an accuracy rate of 78.6% (11/14); while the US sensitivity diagnosis turned out to be 78% (7/9), registering an accuracy rate of 50% (7/14). The statistical analysis showed that there were no significant differences (P=0.021) between the two. The number of the superior and inferior parathyroid glands turned out the same in both tests. 99mTc -MIBI imaging discovered two heterotopic heterotopic nodules while US did not (Refer to Example 2 for the typical image), but there existed no significant difference (P=0.3) between the two. (See Table 2 and Table 3) 99mTc-MIBI imaging can simultaneously discover the lesion beyond the parathyroid glandular tissues, such as skeleton lesion (brown tumor). (See Example 3) Example 2 Patient (See Fig. 3–5)
3.2 Post-operation follow-up situation
The operation success rate is defined as the IPTH was reduced by >50% after the operation [3]. According to the definition, the operation of six patients was successful (the iPTH of patients 1~6 was reduced by 66.4%~100% after PTX, which averaged at 86.5%±12%), and the other two, namely 7 and 8, failed since their iPTH reduction rate was 38.6% and 10% respectively.
The post-operation follow-up of six patients (excluding patient 4 and 5) after four to 22 months showed they suffered no recurrent laryngeal nerve injury and after 1.5 to 2 years, their blood calcium and serum inorganic phosphorus were normal. The iPTH of one patient, which was 2.67 originally, was 0 four days after the operation. The iPTH of two patients who were shown to have heterotopic parathyroid glandular nodules in 99mTc -MIBI imaging, but did not remove them, was 800 pg/ml and 1429 pg/ml respectively. The iPTH of the other three patients was around 300~400 pg/ml.
4 Discussion
Persistent HPT refers to the condition in which HPT is till diagnosed by the biochemical test within six months after the PTX and the minimum value of iPTH is >100pg/ml [4]. In this research, the iPTH of eight patients rose to 339.1~2917 pg/ml respectively after 1~6 years. It is apt to judge that the eight patients suffered from persistent HPT. There are several possible reasons for that: 1) the removal in the first operation was not complete enough, thus leaving some lesion tissues; 2) there existed the heterotopic fifth or even the sixth gland; 3) the disorder of the calcium, phosphorus and activated vitamin D of the patients suffering from chronic renal failure (CRF) led to hyperphosphatemia; 4) the increase of FGF-23 factor and other factors exposed the residual or transplanted parathyroid glandular nodules to excessive stimulation after the operation, thus resulting in the hyperplasia of the parathyroid glandular tissues and the increased secretion of PHT [5]. In this research, two heterotopic parathyroid glandular tissues failed to be removed, which led to a significant increase of iPTH later. The pathological situation of one patient undergoing sternocleidomastoid auto transplantation showed the hyperplasia of the transplant, and a new heterotopic parathyroid glandular nodule appeared in the neck. Therefore, Zhang Ling et al. [6] thought that SHPT patients should take operation as soon as possible and that post-operation transplant is not advisable.
In terms of persistent HPT or SPHT, excision is still the only effective treatment method [2]. However, since patients of the kind are generally in poor health, the normal dissection layers of their neck have been destroyed by scar adhesion, reoperation is faced increasing difficulty. In this research one patient suffered from permanent HPT after the operation. Yao Li et al. [7] also thought that the difficulty of the reoperation of patients undergoing auto transplantation lies in whether the postoperative recurrence position is the residual parathyroid gland in the neck or the parathyroid gland in the auto transplantation. Therefore, it is of paramount importance to conduct accurate localization before the operation.
Now, pre-operation localization methods include US, CT, MRI, 99mTc -MIBI SPECT-CT imaging and so on, of which US is a top choice. The hyper-function parathyroid glandular nodules are manifested as hypoechoic nodules on the SU image. Most of them feature rich blood supply. A satisfying image can be obtained through the high-frequency color ultrasound [8]. However, US also has its limits: 1) its accuracy relies on the operator’s experience and the device performance; 2) the parathyroid glandular recurrent nodules, especially the convex nodules and nodules located in the dorsal part might influence the accuracy rate; and 3) it is difficult to diagnose the parathyroid gland.
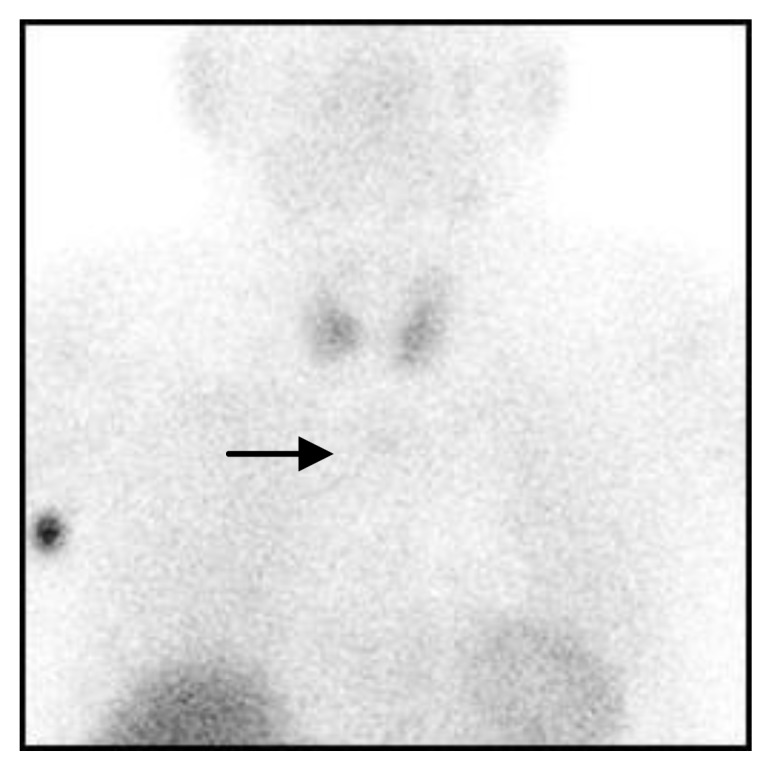
99mTc-MIBI SPECT-CT image is the blending image of function and dissection. Only parathyroid glandular tissues with reinforced functions can take in MIBI. Besides, the removal process is quite slow. PET-CT can provide a detailed dissection image for the clinicians, help operators rapidly find the parathyroid tissues with reinforced functions and shorten the operation time. 99mTc -MIBI imaging might also show the abnormal situation of other tissues, such as lesion of the parathyroid gland and changes of the skeleton system [9]. In this research, only one patient was found to have rib fibrous capsule osteitis. (See Example 3)
In this research, the sensitivity of US turned out to be 77.8%, which was in line with that described in the literatures [10], while its accuracy rate was 50%, which was a little lower than that of literatures [11]. The sensitivity of 99mTc-MIBI imaging turned out to be 100%, which was a little higher than that in the literatures, while its accuracy rate is 78.6% [10], which was a little lower than that in the literatures [11,12]. The reason for this might be the few research examples and that most literatures are plane imaging, but this paper is about plane and SPECT-CT imaging. In the future, more cases should be adopted for the analysis. Though most literatures [13,14] are of the opinion that US is a reliable way to localize the parathyroid glandular nodes, US cannot discover some heterotopic parathyroid glands. Besides, eight patients all had undergone PTX, so their anatomical structure is in a disorder, thus increasing the difficulty of US judgment. Under the circumstance, 99mTc -MIBI SPECT-CT imaging can play an important role [15]. In this research, there were four heterotopic nodules, but US failed to show that. Due to the intake of 99mTc -MIBI, they can be judged to be the hyperplastic parathyroid glandular nodules combined with CT, of which the substernal heterotopia (Example 2) and sternocleidomastoid transplant were finally proved to be parathyroid glandular hyperplasia. Though the pathological result of two heterotopic nodules diagnosed by 99mTc-MIBI SPECT-CT imaging failed to be obtained, the iPTH (>400pg/ml) of the two patients was far higher than that of the other patients (0~351), which did not register a significant reduction compared with that before the operation. In the post-operation follow-up, their iPTH reached as high as 800~1,429 pg/ml, which was also far higher than that of the other four patients.
To sum up, US and 99mTc -MIBI SPECT-CT imaging are top choices for the pre-operation localization of SHPT. Besides, 99mTc -MIBI SPECT-CT imaging can easily reveal the heterotopic parathyroid glandular tissues within the mediastinum, thus can provide more help for the pre-operation localization of SHPT.
Fig. 6.
99mTc-MIBI SPECT-CT image of the brown tumor in the second rib on the left side (cross)
Footnotes
Conflict of interest statement: Authors state no conflict of interest
References
- 1.Hamouda M, Ben Dhia N, Aloui S, et al. Surgical treatment of secondary hyperparathyroidism in patients with chronic renal failure. Nephrol Ther. 2011;7:105–110. doi: 10.1016/j.nephro.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Xiaowei W, Zhiyong C, Huagang ZHU. Progress in diagnosis and treatment of persistent and recurrent hyperparathyroidism. Anhui Medical and Pharmaceutical Journal. 2011;15:666–668. [Google Scholar]
- 3.Li Y, Ling Z, Peng LIU, et al. Therapeutic evaluation of parathyroidectomy for 89 cases with refractory secondary hyperparathyroid-ism. Chinese Journal of Blood Purification. 2009;8:431–436. [Google Scholar]
- 4.Clark OH, Duh QY, Kebebew E. Textbook of Endocrine Surgery, Second Edition. Philadelphia: Elsevier Saunders; 2005. p. 518. [Google Scholar]
- 5.Kalantar-Zadeh K, Shah A, Duong U, et al. Kidney bone disease and mortality in CKD, revisiting the ro1e of vitamin D, calcimimetics, alkaline phosphatase and minerals. Kidney Int. 2010;117:S10–2l. doi: 10.1038/ki.2010.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ling Z, Wenbo W, Li Y, et al. Total parathyroidectomy with forearm autograft in the treatment of a patient with secondary hyperparathyroidism. Chinese Journal of Blood Purification. 2011;10:277–282. [Google Scholar]
- 7.Li Y, Zhan H, Ling Z, et al. Is autotransplantation needed for SPHT patients after undergoing the whole excision of parathyroid glands? Chinese Journal of Blood Purification. 2011;10:233–235. [Google Scholar]
- 8.Chungui S, Zhiyong Y, Tianyan Z. The clinical value of ultrasonography in patients with secondary hyperparathyroidism performing maintenance hemodialysis. Chinese Medical Herald. 2011;8:87–88. [Google Scholar]
- 9.Lishi Z, Xiaojian L, Ling Z, et al. Value of dual-phase 99Tcm-MIBI scintigraphy and SPECT/CT in the localization diagnosis of secondary hyperparathyroidism. Chinese Journal of Blood Purification. 2011;10:242–245. [Google Scholar]
- 10.Wakamatsu H, Noguchi S, Yamashita H, et al. Technetium-99m-tetrofosmin for parathyroid scintigraphy: a direct comparison with (99m)Tc-MIBI, (201)T1, MRI and US. Eur J Nucl Med. 2001;28:1817–1827. doi: 10.1007/s002590100627. [DOI] [PubMed] [Google Scholar]
- 11.Ling T, Rongfu W, Li H, et al. Clinical Value of Radionuclide Parathyroid Imaging in Hyperparathyroidism. Chinese Journal of Medical Imaging Technology. 2003;19:863–865. [Google Scholar]
- 12.Binbin Z, Qian W, Yuan L. Parathyroid hormone testing and 99Tcm-MIBI imaging of hyperparathyroidism. Chinese Journal of Nuclear Medicine and Molecular Imaging. 2011;31:263–266. [Google Scholar]
- 13.Haiming L, Yong GU, Jun X, et al. Clinical effect of total parathyroidectomy with forearm autograft on uremic patients [Google Scholar]