Abstract
Echinococcus granulosus causes a zoonotic infection called cystic echinococcosis (CE) or more commonly known as hydatid disease. Although the two most common locations of hydatid cyst are liver and lung, it may also appear in other parts of the body. Clinical presentation of the hydatid disease depends on the site and size of the lesion. A retrospective study was done in Medical College and Hospital, Kolkata, from January 2012 to June 2014, to find the site of involvement, distribution, clinical features, history of contact, mode of presentation, laboratory diagnosis, and treatment modalities of the cases of hydatid cyst. The cases were identified by radiological and laboratory methods, the data were entered in Excel spreadsheet, and analysis was done. Among the 21 cases of hydatid cyst included in the study, solitary hepatic involvement was seen in 11 (52.38%), pulmonary involvement in 4 (19%), and 6 (28.71%) were in unusual locations such as liver cyst extending as retroperitoneal, omental cyst, choledochal cyst, splenic cyst, and in hepatorenal pouch. History of contact with dog was seen in 15 (71.43%). All the patients were treated with surgery and albendazole and were discharged in healthy condition. CE may be present in usual and unusual locations with a lot of variations in the clinical features. Hence, proper radiological and laboratory diagnosis is required for accurate diagnosis and appropriate management of these cases.
Keywords: Albendazole, cystic echinococcosis, hydatid cyst, liver cyst, lung cyst, surgery
INTRODUCTION
The larval stages of cestode Echinococcus granulosus cause a zoonotic infection called cystic echinococcosis (CE), commonly known as hydatid cyst. The disease is acquired by ingesting eggs, coming from the feces of definitive hosts such as dogs, wolves, and other canine animals, which harbor the adult Echinococcus worms in their intestine.[1] CE is included in the list of “neglected tropical diseases” by the World Health Organization.[2] It is a serious life-threatening neglected zoonotic disease that occurs in both developing and developed countries and is recognized as a major public health problem.[3] It is found in Africa, Europe, Asia, the Middle East, and Central and South America.[1] Echinococcal cysts are mostly located in the liver and the lung, but the disease can be detected anywhere in the body.[4] Clinical presentation of the hydatid disease depends on the site and size of the lesion.[5]
METHODS
A retrospective study was done in Medical College, Kolkata, a tertiary care hospital and teaching college in Eastern India for 2 years 6 months (January 2012–June 2014) to analyze all the cases of CE who presented in the Department of Surgery. All the cases included were confirmed as hydatid cyst by ultrasonography (USG) and computerized tomography (CT scan). The patients were operated, and the excised cysts were sent to the Department of Microbiology for laboratory analysis. The cyst fluid was centrifuged, and the deposit showed scolices confirming the diagnosis of hydatid cyst in all the cases. The patients were treated with oral albendazole (10–15 mg/kg/day) from 4 weeks before the operation and continued for 4 weeks postoperatively. The data for all the cases included were entered in Excel spreadsheet (Microsoft Office, Redmond, Washington, USA). The geometric mean and percentage were calculated.
RESULTS
A total of 21 confirmed cases of hydatid cyst were included in the study who presented to the Department of Surgery, Medical College, Kolkata, a tertiary care teaching hospital in West Bengal, during a period of 2 years 6 months. Among the included patients, 13 (61.9%) were males and 8 (38.1%) were females. The age of the patients was between 3 years and 56 years (mean = 32.43 years).
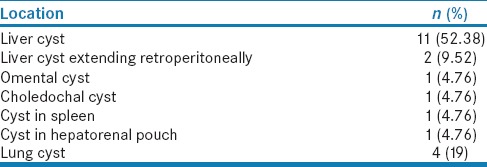
Among the included patients, solitary hepatic involvement was seen in 11 (52.38%) patients, pulmonary involvement in 4 (19%) patients, and 6 (28.71%) were in unusual locations such as liver cyst extending to retroperitoneum, omental cyst, choledochal cyst, splenic cyst, and cyst in hepatorenal pouch [Table 1].
Table 1.
The distributions of hydatid cysts according to the site of involvement
Regarding the history of contact, 15 (71.43%) cases gave a history of contact with dog, 4 (19%) cases with sheep, and in 2 (9.52%) cases, there was no definite history of contact.
Among the hydatid cyst patients, most frequently observed symptom was abdominal pain seen in 12 (57.14%) cases, especially seen in right hypochondrium and epigastrium along with left hypochondrium in a case. The most frequent clinical finding was hepatomegaly in 8 (38.1%) cases [Table 2]. Abdominal USG and CT were used for confirmation of the diagnosis [Figures 1 and 2]. Among the liver cysts, 7 were localized in the right lobe, 2 in left lobe, and 2 were located bilaterally. Communication of the cyst with the biliary tree was documented in one case.
Table 2.
Clinical features of the included cases of hydatid cyst
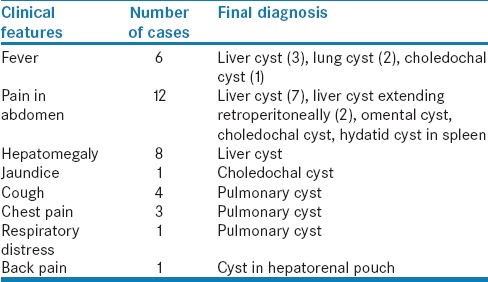
Figure 1.

Computerized tomography scan shows a large hydatid cyst with a noncalcified, high-attenuation wall in the right hepatic lobe
Figure 2.

Computerized tomographya scan shows hydatid cyst with a noncalcified wall in the spleen
Among the four cases of solitary pulmonary hydatid disease, all presented with cough, three (75%) had chest pain, two (50%) had fever, one patient had expectoration of mucopurulent sputum, and one patient had respiratory distress. There was no hemoptysis as a presenting symptom. Chest X-ray [Figure 3] and CT scan [Figure 4] were used for establishing the diagnosis in these pulmonary hydatid cysts. Involvement of lower lobes occurred in three (75%) cases and the right side was affected in three (75%) cases which was more than left side [Figure 5].
Figure 3.
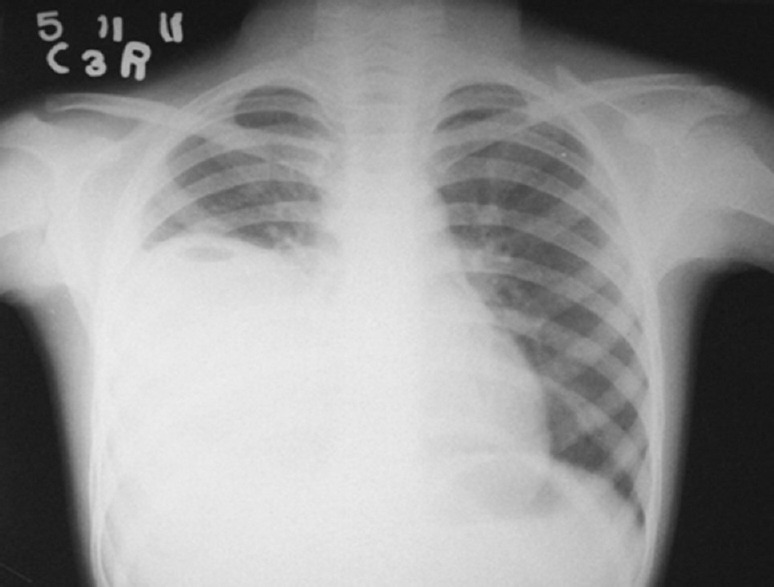
Chest X-ray showing a dense homogeneous radiopaque opacity involving the right lower zone with obliteration of costophrenic angle
Figure 4.
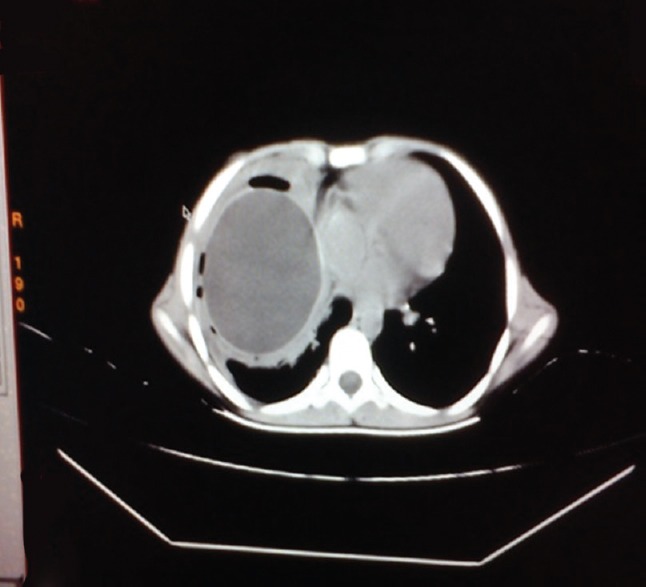
Computerized tomography scan showing a dense homogeneous mass involving the right lower zone of lung
Figure 5.

Computerized tomography scan shows a hydatid cyst with a noncalcified wall in the right lower lobe of lung (lateral view)
Regarding operative interventions of the abdominal CE, cyst excision in seven cases, partial cystectomy with omentoplasty in three cases, pericystectomy in three cases, left lateral segmentectomy in one case, right hepatectomy in one case with a huge cyst occupying the largest part of the right hepatic lobe, splenectomy was performed in one case, and cholecystectomy with T-tube drainage was done in case of cyst with biliary tree communication [Figure 6].
Figure 6.
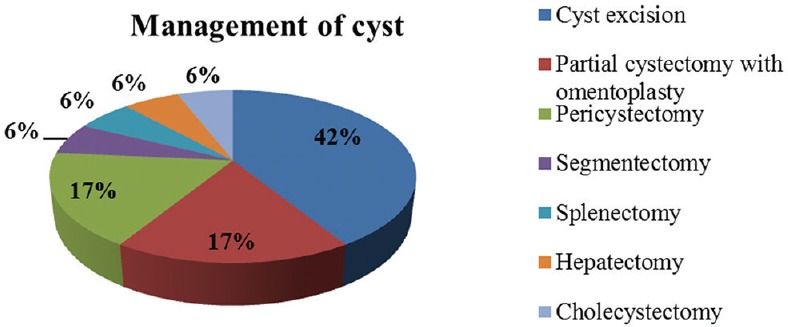
Management of the abdominal cysts
Regarding operative interventions of the pulmonary cysts, cystotomy and delivery of the cysts and partial pericystectomy with capitonnage of the residual pericyst cavity were performed on the affected side in three cases. Lobectomy was done in one case of huge cyst.
The patients were treated with oral albendazole (10–15 mg/kg/day) from 4 weeks before the operation and continued for 4 weeks postoperatively. All the patients recovered and were discharged from the hospital in healthy condition.
The fluid from the hydatid cyst after operation was examined under the microscope in the Department of Microbiology and showed brood capsule and protoscolices which confirmed CE [Figure 7]. Serologic antibody tests were not done because of their low diagnostic value compared to radiologic technique.
Figure 7.
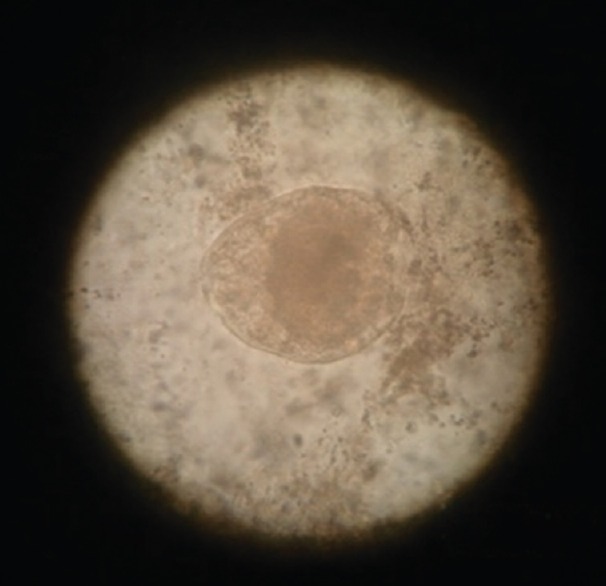
Wet mount of centrifuged hydatid cyst fluid shows scolex and hydatid sand
All the patients were followed up at an interval of 6 months for a period of 2 years. On the subsequent visits, history, physical examination, liver function tests, and USG were done. CT of the abdomen was done every year. Recurrence was seen in only one case with no mortality.
DISCUSSION
Hydatid cyst may occur at different locations. It is most commonly located in liver in 70% cases and lung (25%).[4] Primary isolated extrahepatic hydatid disease is mostly seen within the abdomen with an incidence of 6%–11%.[6] Although some patients may be asymptomatic, the clinical presentation is mostly with abdominal pain or swelling of soft tissue with respect to disease localization, i.e., spleen, pancreas, kidney, retroperitoneum, urinary bladder, ovary, bone, heart, thoracic wall, spinal column, thyroid gland, brain, and muscles.[4] We also found that the most common location of CE as solitary cysts in liver in 52.38% cases. It is common in both men and women. The risk factors for hydatid cyst include dogs living in close association with the human beings besides slaughter of livestock and unsanitary living conditions. Population at high risk of cystic echinococcosis include shepherds, butchers, slaughters, veterinarians, and all whose job requires them to work closely with animals at higher risk of the infection.[1] In this study, there was a history of association with dogs seen in 71.43% cases.
Symptoms occur due to compression of local structures or complications such as rupture and infection. The diagnosis is clear when typical radiological appearance is observed at the common sites of involvement. Complications give rise to atypical appearances.[7] Symptoms of hydatid cyst depend on the affected organ, for example, liver cysts cause jaundice, abdominal discomfort, whereas lung cysts cause cough, chest pain, and hemoptysis. In patients with hydatid cyst of the lung without concomitant liver involvement, it is postulated that the embryo after migrating through the stomach wall enters the lymphatics and passes directly to the lung by way of the thoracic duct and mediastinal lymphatics, thus avoiding the liver.[8]
Surgery is the mainstay of treatment of hydatid disease.[9] Radical surgery (total pericystectomy or partially affected organ resection), conservative surgery (open cystectomy), or simple tube drainage for infected communicating cysts are choices of surgical techniques.[5] Sterilization of the cyst cavity done by different scolicidal agents, and cetrimide solution (0.5%) provides the best protection with least complications.[10] Pre- and post-operative 1-month course of albendazole or 2 weeks of praziquantel should be considered to sterilize the cyst and decrease the chance of anaphylaxis, decrease the tension in the cyst wall, and reduce the recurrence rate postoperatively.[11] In this study, the patients were treated with surgery and albendazole with only one recurrence and no mortality.
CONCLUSION
The most common location of hydatid cyst is liver followed by lung, but it may also be located in unusual locations. Accurate diagnosis of the disease is necessary for proper management. With appropriate surgical management, hydatid disease has a good prognosis with low recurrence.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Herrador Z, Siles-Lucas M, Aparicio P, Lopez-Velez R, Gherasim A, Garate T, et al. Cystic echinococcosis epidemiology in Spain based on hospitalization records, 1997-2012. PLos Negl Trop Dis. 2016;10:e0004942. doi: 10.1371/journal.pntd.0004942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Giri S, Parija SC. A review on diagnostic and preventive aspects of cystic echinococcosis and human cysticercosis. Trop Parasitol. 2012;2:99–108. doi: 10.4103/2229-5070.105174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Biswas B, Ghosh D, Bhattacharjee R, Patra A, Basuthakur S, Basu R. One stage surgical management of hydatid cyst of lung and liver-by right thoracotomy and phrenotomy. Indian J Thorac Cardiovasc Surg, 2004;20:88–90. [Google Scholar]
- 4.Aksakal N, Kement M, Okkabaz N, Altuntas YE, Öncel M. Unusually located primary hydatid cysts. Ulus Cerrahi Derg. 2015;32:130–3. doi: 10.5152/UCD.2015.2947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ates M, Karakaplan M. Hydatid cyst in the biceps and gluteus muscles: Case report. Surg Infect (Larchmt) 2007;8:475–8. doi: 10.1089/sur.2006.040. [DOI] [PubMed] [Google Scholar]
- 6.Makni A, Jouini M, Kacem M, Safta ZB. Extra-hepatic intra-abdominal hydatid cyst: Which characteristic, compared to the hepatic location? Updates Surg. 2013;65:25–33. doi: 10.1007/s13304-012-0188-6. [DOI] [PubMed] [Google Scholar]
- 7.Malik A, Chandra R, Prasad R, Khanna G, Thukral BB. Imaging appearances of atypical hydatid cysts. Indian J Radiol Imaging. 2016;26:33–9. doi: 10.4103/0971-3026.178284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barrett NR. The anatomy and the pathology of multiple hydatid cysts in the thorax. Ann R Coll Surg Engl. 1960;26:362–79. [PMC free article] [PubMed] [Google Scholar]
- 9.Shahnazi M, Azadmehr A, Latifi R, Hajiaghaee R, Saraei M, Alipour M. In vitro protoscolicidal effects of various concentrations of Ziziphora tenuior L. extract at different exposure times. Avicenna J Phytomed. 2016;6:376–82. [PMC free article] [PubMed] [Google Scholar]
- 10.Vicidomini S, Cancrini G, Gabrielli S, Naspetti R, Bartoloni A. Muscular cystic hydatidosis: Case report. BMC Infect Dis. 2007;7:23. doi: 10.1186/1471-2334-7-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duygulu F, Karaoglu S, Erdogan N, Yildiz O. Primary hydatid cyst of the thigh: A case report of an unusual localization. Turk J Pediatr. 2006;48:256–9. [PubMed] [Google Scholar]


