Abstract
Purpose:
The purpose of this study is to compare the outcomes following femtosecond laser-assisted deep anterior lamellar keratoplasty (DALK) with 75% of stromal dissection (predescemetic group) and femtosecond laser-assisted DALK using big-bubble technique with total stromal resection (descemetic group) for the treatment of keratoconus.
Subjects and Methods:
Twenty eyes of 17 patients with keratoconus were studied. There were 10 eyes of 9 patients in predescemetic group and 10 eyes of 8 patients in descemetic group. The postoperative best-corrected visual acuity (BCVA), manifest refraction, keratometry, endothelial cell density (ECD), and central corneal thickness (CCT) were analyzed.
Results:
All surgeries were performed uneventfully. At 1 year after surgery, the BCVA, corneal astigmatism, keratometry, CCT, and ECD between two groups were not statistically significant (all P > 0.05). However, the mean manifest refraction was −9.43 ± 7.44 diopter (D) and −1.03 ± 1.13D in predescemetic and descemetic groups, respectively, which was statistically significant between two groups (P < 0.05).
Conclusions:
The results of BCVA and corneal astigmatism, keratometry, ECD, and CCT were comparable between two groups. However, the mean postoperative manifest refraction was lower in descemetic group.
Keywords: Descemetic lamellar keratoplasty, femtosecond laser-assisted, keratoconus, predescemetic lamellar keratoplasty
Deep anterior lamellar keratoplasty (DALK) is a lamellar transplantation technique, which can be used to treat keratoconus without affecting the endothelium.[1] There are two types of DALK: Predescemetic with 75% of stromal dissection and descemetic with total stromal resection using big-bubble technique with preserving the recipient's endothelium and decreasing the risk of immunologic rejection.[1,2] The visual outcomes are comparable between DALK and penetrating keratoplasty (PKP);[3] of note, DALK surgeries have superiority over PKP in maintaining of eyeball integrity, reducing the dosages and duration in postoperative steroid therapy, and lower incidence of graft rejection and acute and chronic endothelial cell loss.[4,5]
Several manual techniques have been used to separate the plane between deep stroma and Descemet's membrane (DM). The significant topographical irregularities in the lamellar interface and poor visual acuity in some patients were resulted from DALK procedure with manually separating technique.[6] A femtosecond laser-assisted keratoplasty procedure has been developed to produce bladeless, precise, and predefine lamellar cuts with minimal tissue injury. Here, we report the clinical results following femtosecond laser-assisted DALK with 75% of stromal dissection (predescemetic group) and using big-bubble technique with total stromal resection (descemetic group) for the treatment of moderate to advanced keratoconus by 500-kHz VisuMax femtosecond laser (Carl Zeiss Meditec AG, Jena, Germany).
Subjects and Methods
All patients have signed the informed consent. The study was approved by the Medical Ethics Committee of Jinling Hospital and adhered to the tenets of the Declaration of Helsinki. All patients have >280 µm of corneal thickness. None of the patients had any other coexisting ocular disease. All donor tissues were obtained within 12 h after enucleated eyeballs from healthy young adults with accidental death without any disease. Twenty eyes of 17 patients, who are with moderate to advanced keratoconus without acute keratoconus, the corneas were clear and there was no edema in DM, were enrolled in this study. The patients were divided into femtosecond laser-assisted DALK with 75% of stromal dissection (predescemetic group) and using big-bubble technique with total stromal resection (descemetic group). There were 10 eyes of 9 patients (8 males and 1 female) with mean age of 29.4 ± 8.8 years (range, 20–42 years) in predescemetic group and 10 eyes of 8 patients (all males) with mean age of 20.6 ± 6.4 years (range, 15–32 years) in descemetic group.
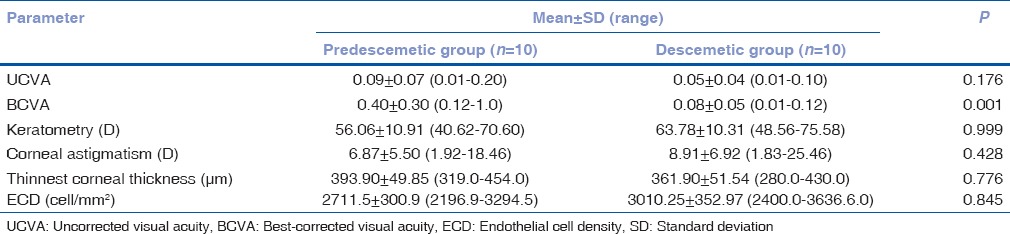
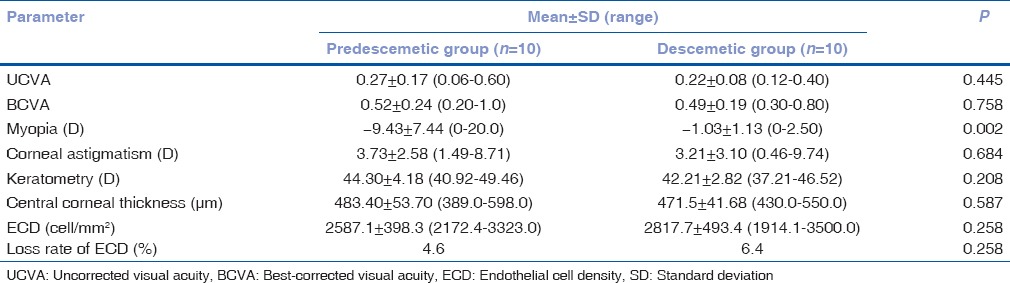
All treated eyes were examined preoperatively and postoperatively in terms of the uncorrected visual acuity (UCVA) and best-corrected visual acuity (BCVA) with the standard logarithm of the minimum angle of resolution chart. Anterior segment optical coherence tomography (OCT) (Carl Zeiss Meditec, Jena, Germany) combined with the 50-MHz ultrasound corneal pachymetry was used to measure the thinnest corneal thickness in the recipient cornea. Slit-lamp examination, endothelial cell density (ECD), corneal topography, and dilated fundus examination in dilated pupil were also evaluated. The preoperative data were shown in Table 1.
Table 1.
The preoperative data in two groups
All procedures of the two groups were performed by a sole fully qualified and highly experienced surgeon (Zhen-Ping Huang). The whole eyeball was placed in the eyeball fixation (which we previously described)[7] and received the treatment with the 500-kHz VisuMax femtosecond laser (Carl Zeiss Meditec AG, Jena, Germany).
In the predescemetic group, the mean donor lenticule thickness and diameter were 399 ± 55.27 µm (range, 300–510 µm) and 7.73 ± 0.21 mm (range, 7.3–8.0 mm), respectively; the mean recipient lenticule thickness, lenticule diameter, and residual stromal bed thickness were 309.5 ± 53.87 µm (range, 230–380 µm), 7.54 ± 0.16 mm (range, 7.3–7.8 mm), and 84.4 ± 8.67 µm (range, 74–105 µm), respectively. After femtosecond laser procedure, the patient was transferred to the operating room. The recipient corneal button was lifted, and the donor lenticule was placed on the recipient residual corneal stromal bed and sutured by continuous or 16 interrupted stitches with 10-0 nylon sutures under retrobulbar anesthesia.
In descemetic group, we use the laser settings in PKP mode for the donor and recipient to achieve the vertical side cut according to the thinnest corneal thickness. The mean diameter of lamellar was 7.52 ± 0.14 mm (range, 7.4–7.8 mm) in the donor and 7.38 ± 0.10 mm (range, 7.2–7.5 mm) in the recipient. After femtosecond laser procedure, the patient was transferred to the operating room with retrobulbar anesthesia.
A 27-gauge needle bent into 60° with a 5 ml syringe filled with air was inserted into the deep stroma. Air was then injected into the stroma to achieve a big bubble between the DM and posterior stroma. The anterior chamber paracentesis was performed to lower the intraocular pressure, and a small air bubble was injected into the anterior chamber to check the baring of DM. Then, a crescent disposable knife was used to cut the corneal stroma into half, and an ophthalmic viscosurgical device was used to refill the space and protect the DM. The residual stroma was excised by corneal scissors to expose the smoothly transparent DM. After peeling off DM and endothelium using forceps from the donor lamella, prepared by femtosecond laser, the donor lamella was placed on the host stromal bed and sutured by 16 interrupted stitches with 10-0 nylon sutures.
The antibiotics and corticosteroids of intravenous injection were used once a day for 3 days. Tobramycin dexamethasone and ofloxacin eye drops were applied six times and four times/day for 2 weeks, respectively. Fluorometholone and cyclosporine A eye drops were instilled three times/day for 3 months to prevent graft rejection.
Mean follow-up time was 1 year. Data of the last visit from each patient were recorded and selected for analysis. Statistical analysis was performed with SPSS software (Version 17, SPSS, Inc., Chicago, IL, USA). Data were calculated as mean ± standard deviation differences of BCVA, myopia, corneal astigmatism, keratometry, central corneal thickness (CCT), and ECD between two groups were analyzed using two independent samples t-test. A P < 0.05 was defined statistically significant.
Results
All procedures of twenty eyes were uneventful while one eye has encountered intraoperative DM microperforation in the predescemetic group without converted to PKP operation intraoperatively. No other intraoperative complications were detected.
The clear, smooth DM was observed intraoperatively [Fig. 1a] in the descemetic group, and the regular surface of predescemetic plane was detected in the predescemetic group [Fig. 1b]. Alignment of DM with the donor tissue was much better in the descemetic group at day 2 postoperatively [Fig. 2] compared with predescemetic group [Fig. 3].
Figure 1.
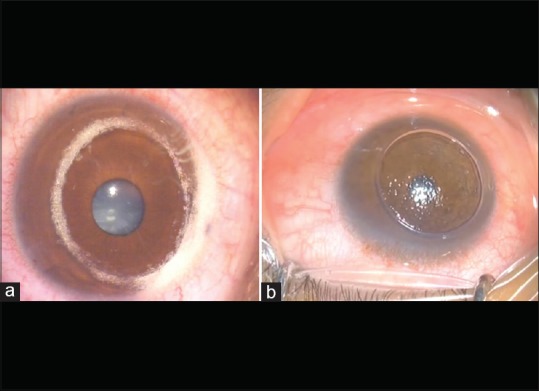
(a) The clear and smooth Descemet's membrane was observed after stromal removal in descemetic group. (b) The regular surface of predescemetic plane was detected in predescemetic group
Figure 2.
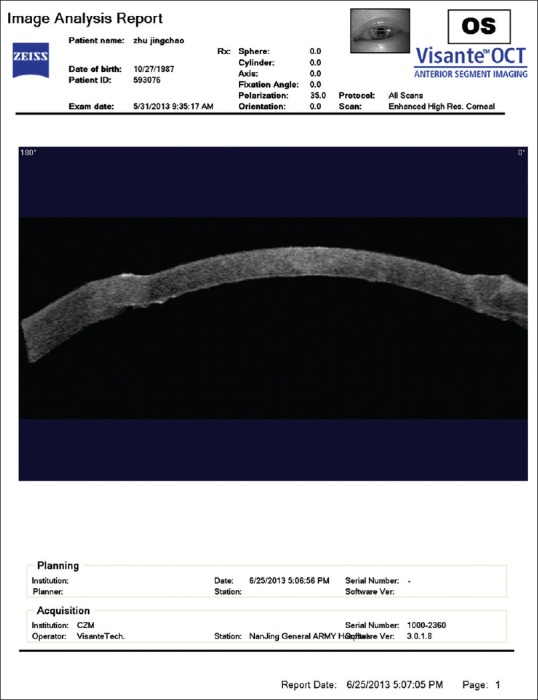
The excellent alignment of Descemet's membrane with the donor tissue was observed through anterior segment optical coherence tomography at 2 days after surgery in descemetic group
Figure 3.
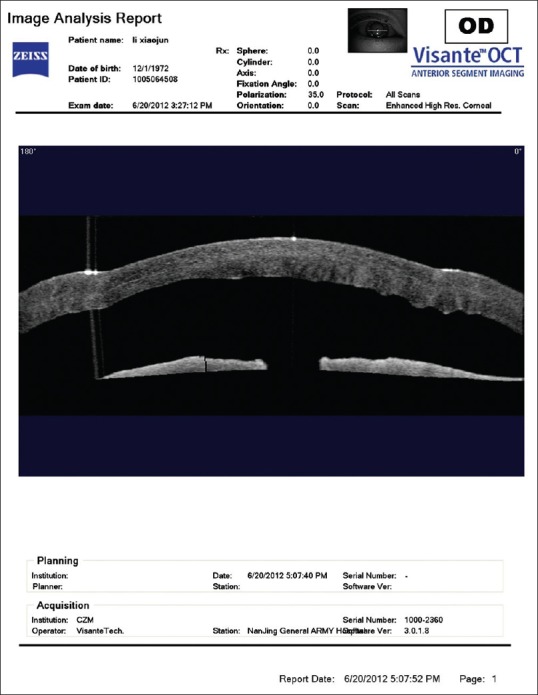
The alignment of Descemet's membrane with the donor tissue was detected through anterior segment optical coherence tomography at day 2 postoperatively in predescemetic group
The postoperative parameter between two groups was shown in Table 2. The differences of BCVA, corneal astigmatism, corneal curvature, CCT, and loss rate of ECD between two groups were not statistically significant (all P > 0. 05) while the loss rate of ECD was slightly higher in the descemetic group (6.4%) than the predescemetic group (4.6%). However, the mean postoperative myopia was −9.43 ± 7.44 diopter (D) in the predescemetic group and −1.03 ± 1.13D in the descemetic group, which was statistically significant (P = 0.002).
Table 2.
The postoperative data in two groups at the last examination
In term of postoperative complications, there was one patient with wound dehiscence in the predescemetic group, which has been resutured and one eye with stromal rejection, which has been treated with the application of topical steroids; there was one eye with high intraocular pressure postoperative induced by the application of steroid in descemetic group, which has been treated by medical therapy.
Discussion
Keratoconus is characterized by the conical shape of cornea with thinning and forward protrusion.[8] It has gained widespread acceptance that lamellar keratoplasty (LK) is necessary for the treatment of moderate to advanced keratoconus, and the acute advanced keratoconus with ruptured DM is required to be treated with PKP.[9] The important benefit from LK is that it can decrease the risk of endothelial rejection.
In the previous study, the UCVA and BCVA have been improved by the femtosecond laser-assisted predescemetic LK for the patients with moderate to advanced keratoconus.[10] As the stroma is unhealthy for the patients with keratoconus, we performed the femtosecond laser-assisted descemetic LK with big-bubble technique for the treatment of keratoconus.
DALK with big-bubble technique was first reported by Anwar and Teichmann in 2002,[4] which the 60%–80% thickness of the cornea was removed first and injected air between deep stroma and DM to separate the cornea with the advantages of shortening the surgical time, reducing the risk of perforation, and exposing the smooth surface.
In contrast to Anwar's technique, we use the 500-kHz VisuMax femtosecond laser to cut the donor and host peripheral cornea with regular and smooth incision.
Our results indicate that the differences of BCVA, corneal astigmatism, keratometry, CCT, and the loss rate of ECD between two groups are not statistically significant (all P > 0. 05) at the last follow-up. The results of postoperative BCVA are similar to results by Abdelkader and Kaufman,[11] Sarnicola et al.,[8] and Schiano-Lomoriello et al.,[12] which have indicated that no difference in BCVA between the predescemetic and descemetic groups is observed, while the visual recovery time is faster in the descemetic group. However, authors have not compared the postoperative myopia between the predescemetic and descemetic groups in their reports.
The preoperative mean thinnest corneal thickness, evaluated with ultrasound corneal pachymetry and with anterior segment OCT, was 393.90 ± 49.85 µm (range, 319.0–454.0 µm) in the predescemetic group and 361.90 ± 51.54 µm (range, 280.0–430.0 µm) in the descemetic group. The postoperative corneal mean thickness was 483.40 ± 53.70 µm (range, 389.0–598.0 µm) and 471.5 ± 41.68 µm (range, 430.0–550.0 µm) in the predescemetic group and descemetic group, respectively. Although there was no statistically significant difference in the CCT of the two groups, both groups have an improvement of thickness and restoring the corneal optical integrity and structure.
The mean postoperative myopia is −9.43 ± 7.44D (8 of 10 eyes ≥−6.0D) in the predescemetic group and −1.03 ± 1.13D (all of 10 eyes <−3D) in the descemetic group in our results, which is statistically significant (P < 0.05). The results of descemetic group are consistent with Buzzonetti et al.'s paper,[13] who have reported the mean postoperative myopia was −1.50 ± 1.70D at 12 months after surgery following the 60-kHz IntraLase femtosecond laser-assisted DALK with big-bubble technique for keratoconus.
Girard et al.[14] reported that the postoperative myopia has been decreased when the diameter of donor graft is 0.25 mm smaller than the recipient graft in PKP for keratoconus. Doyle et al.[15] stated, to some extent, the postoperative refraction could be manipulated toward acceptable ametropia with altering the size of the donor graft button, and they have demonstrated that the average of hyperopic 2.2D would resulted from decreased 0.25 mm of diameter for the graft.
Some papers have indicated that the diameter of donor graft is depending on the axial length of eyeball. If the axial length is more than 24.5 mm, the diameter of donor graft should be equal to the recipient. If not, the diameter of donor graft should be 0.25 mm larger than the recipient. In addition, when the diameter of donor grafts was smaller than the recipient or the tight sutures were used intraoperatively, there will be hyperopic diopters for the patients and vice versa. Shimmura et al.[16] have verified that the postoperative visual acuity was better in the patients with same size of the donor and recipient graft than the patients with donor graft 0.25 mm larger of than recipient for the keratoconus patients with longer axial length of eyeball.
In this study, we set the mean diameter of donor graft 0.19 mm larger than the recipient in the predescemetic and 0.14 mm larger in the descemetic group referring to Mosca et al.'s paper,[17] which they set the average diameter of donor graft 0.2 mm larger than the recipient.
Wang et al. who performed predescemetic LK and big-bubble descemetic LK for keratoconus manually, which there was no significant difference of postoperative myopic diopter between two groups (P > 0.05). It was different from our results while it was possible to be significant difference of postoperative myopic diopter between predescemetic and descemetic groups using femtosecond laser as the postoperative corneal pattern is better in the patients with total stromal resection.
Moreover, Ardjomand et al.[18] reported that the postoperative visual acuity following DALK was similar to PKP when the residual stromal thickness was <20 µm, while it would be affected in the case of >80 µm of the residual stromal thickness. In our study, the residual stromal thickness was 84.4 ± 8.67 µm in the predescemetic group and 15 µm in the descemetic group (the thickness of DM was about 10 µm and the endothelium was 5 µm); however, there was no significant difference in terms of BCVA and UCVA between two groups (P = 0.758 and 0.445, respectively).
The excellent alignment of DM with the donor tissue was noticed in the descemetic group through anterior segment OCT at early postoperative examination while there was interface observed between the recipient DM and the donor tissue in the predescemetic group.
Hence, we believe that there will be different results in different diameters of donor and recipient graft with or without femtosecond laser. In this paper, we have not evaluated the preoperative manifest refraction and axial length of eyeball in the study population, further study should include these data and increase the studied patients.
Conclusions
Our preliminary results suggest that femtosecond laser-assisted descemetic LK with big-bubble technique could be the alternative procedure to treat the patients with keratoconus rather than femtosecond laser-assisted predescemetic LK.
Financial support and sponsorship
This work was supported in part by young medical talent project grant QNRC2016905 from Jiangsu Province, China.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Tan DT, Dart JK, Holland EJ, Kinoshita S. Corneal transplantation. Lancet. 2012;379:1749–61. doi: 10.1016/S0140-6736(12)60437-1. [DOI] [PubMed] [Google Scholar]
- 2.Baradaran-Rafii A, Eslani M, Sadoughi MM, Esfandiari H, Karimian F. Anwar versus Melles deep anterior lamellar keratoplasty for keratoconus: A prospective randomized clinical trial. Ophthalmology. 2013;120:252–9. doi: 10.1016/j.ophtha.2012.07.090. [DOI] [PubMed] [Google Scholar]
- 3.Watson SL, Ramsay A, Dart JK, Bunce C, Craig E. Comparison of deep lamellar keratoplasty and penetrating keratoplasty in patients with keratoconus. Ophthalmology. 2004;111:1676–82. doi: 10.1016/j.ophtha.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 4.Anwar M, Teichmann KD. Deep lamellar keratoplasty: Surgical techniques for anterior lamellar keratoplasty with and without baring of Descemet's membrane. Cornea. 2002;21:374–83. doi: 10.1097/00003226-200205000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Fogla R, Padmanabhan P. Results of deep lamellar keratoplasty using the big-bubble technique in patients with keratoconus. Am J Ophthalmol. 2006;141:254–9. doi: 10.1016/j.ajo.2005.08.064. [DOI] [PubMed] [Google Scholar]
- 6.Soong HK, Malta JB, Mian SI, Juhasz T. Femtosecond laser-assisted lamellar keratoplasty. Arq Bras Oftalmol. 2008;71:601–6. doi: 10.1590/s0004-27492008000400028. [DOI] [PubMed] [Google Scholar]
- 7.Lu Y, Yang L, Ge Y, Chen X, Huang Z. Femtosecond laser-assisted anterior lamellar keratoplasty for the treatment of stromal corneal pathology. BMC Ophthalmol. 2015;15:15. doi: 10.1186/s12886-015-0009-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sarnicola V, Toro P, Gentile D, Hannush SB. Descemetic DALK and predescemetic DALK: Outcomes in 236 cases of keratoconus. Cornea. 2010;29:53–9. doi: 10.1097/ICO.0b013e3181a31aea. [DOI] [PubMed] [Google Scholar]
- 9.Brierly SC, Izquierdo L, Jr, Mannis MJ. Penetrating keratoplasty for keratoconus. Cornea. 2000;19:329–32. doi: 10.1097/00003226-200005000-00014. [DOI] [PubMed] [Google Scholar]
- 10.Lu Y, Shi YH, Yang LP, Ge YR, Chen XF, Wu Y, et al. Femtosecond laser-assisted deep anterior lamellar keratoplasty for keratoconus and keratectasia. Int J Ophthalmol. 2014;7:638–43. doi: 10.3980/j.issn.2222-3959.2014.04.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abdelkader A, Kaufman HE. Descemetic versus pre-descemetic lamellar keratoplasty: Clinical and confocal study. Cornea. 2011;30:1244–52. doi: 10.1097/ICO.0b013e318219bc1a. [DOI] [PubMed] [Google Scholar]
- 12.Schiano-Lomoriello D, Colabelli-Gisoldi RA, Nubile M, Oddone F, Ducoli G, Villani CM, et al. Descemetic and predescemetic DALK in keratoconus patients: A clinical and confocal perspective study. Biomed Res Int 2014. 2014:123156. doi: 10.1155/2014/123156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buzzonetti L, Laborante A, Petrocelli G. Refractive outcome of keratoconus treated by combined femtosecond laser and big-bubble deep anterior lamellar keratoplasty. J Refract Surg. 2011;27:189–94. doi: 10.3928/1081597X-20100520-01. [DOI] [PubMed] [Google Scholar]
- 14.Girard LJ, Eguez I, Esnaola N, Barnett L, Maghraby A. Effect of penetrating keratoplasty using grafts of various sizes on keratoconic myopia and astigmatism. J Cataract Refract Surg. 1988;14:541–7. doi: 10.1016/s0886-3350(88)80013-0. [DOI] [PubMed] [Google Scholar]
- 15.Doyle SJ, Harper C, Marcyniuk B, Ridgway AE. Prediction of refractive outcome in penetrating keratoplasty for keratoconus. Cornea. 1996;15:441–5. [PubMed] [Google Scholar]
- 16.Shimmura S, Ando M, Ishioka M, Shimazaki J, Tsubota K. Same-size donor corneas for myopic keratoconus. Cornea. 2004;23:345–9. doi: 10.1097/00003226-200405000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Mosca L, Fasciani R, Tamburelli C, Buzzonetti L, Guccione L, Mandarà E, et al. Femtosecond laser-assisted lamellar keratoplasty: Early results. Cornea. 2008;27:668–72. doi: 10.1097/ICO.0b013e31816736b1. [DOI] [PubMed] [Google Scholar]
- 18.Ardjomand N, Hau S, McAlister JC, Bunce C, Galaretta D, Tuft SJ, et al. Quality of vision and graft thickness in deep anterior lamellar and penetrating corneal allografts. Am J Ophthalmol. 2007;143:228–35. doi: 10.1016/j.ajo.2006.10.043. [DOI] [PubMed] [Google Scholar]


