Abstract
Introduction:
As in all surgeries, complications during cataract surgery are unavoidable and cause distress to the surgeon and the patient. This study was conducted to know the factors contributing to complications in our settings, to be able to counsel patients about complications and outcomes and to reduce litigations.
Materials and Methods:
The secondary data analysis was conducted using the National Eye Database from 2007 to 2014. Demographic features, ocular comorbidities, technique of surgery, grade of surgeons, types of intraoperative complications, and reasons for not obtaining good visual acuity following intraoperative complications were studied. Statistics was done using Statistical Package for Social Sciences version 20.
Results:
Out of 12,992 eyes, 6.1% had intraoperative complications. The highest rate of complications was when more trainees (medical officers [MOs] and gazetting specialists) operated. Posterior capsule rupture (PCR) was the most common complication followed by vitreous loss and zonular dehiscence. Those aged below 40 years had more complications (P < 0.05), and females had more complications. Ethnicity did not affect complications. Pseudoexfoliation was the only comorbidity causing complications (P < 0.05). Phacolytic lenses had 8.118 times the odds of getting intraoperative complications. MOs and gazetting specialists got more complications. Good outcomes were obtained in cases without complications and those operated by specialists. High astigmatism was the main reason for poorer outcomes.
Conclusion:
Intraoperative complications were caused mostly by less experienced doctors and had poorer outcomes. Age below 40 years, females, the presence of pseudoexfoliation and phacolytic lenses had more complications. PCR was the most common complication.
Keywords: Associations, cataract complications, outcomes
Cataracts and uncorrected refractive errors are the leading cause of blindness in Malaysia.[1]
The only treatment modality for cataracts is surgery.[2,3,4] As in any surgery, the occurrence of intraoperative complications is unavoidable. Complications can also subject a surgeon or hospital to litigation.
There is currently lack of study on intraoperative complications in Malaysia. We aimed to look at factors that contribute to and are associated with intraoperative complications in our setting and to recommend guidelines to minimize these complications in future. We hope that appropriate counseling of patients would also reduce complaints and legal suits in future.
Materials and Methods
We did an 8-year retrospective analysis of all patients who had intraoperative complications during cataract surgery in Melaka Hospital. Data were obtained from the National Eye Database (NED). Permission to conduct the study was granted by the Medical Research Ethics Committee.
The age, gender, and side of eye operated on were noted. The age groups were divided into <40 years, 41–50 years, 51–60 years, 71–80 years, and above 80 years.
Ocular comorbidities such as pterygium involving the cornea, corneal opacity, glaucoma, chronic uveitis, and pseudoexfoliation were noted. Lens-related complications such as phacomorphic, phacolytic, and subluxated/dislocated lenses were noted.
The type of cataract surgery done whether Lens aspiration using a Simcoe cannula, extracapsular cataract extraction (ECCE), phacoemulsification (phaco), phaco converted to ECCE or intracapsular cataract extraction (ICCE) was all noted down. Whether the surgery was done alone or in combination with other procedures such as pterygium excision, filtering surgery, vitreoretinal surgery, and penetrating keratoplasty were noted down. The grade of the surgeon doing the surgery whether specialist, gazetting specialist or medical officer (MO) was all noted down. A specialist is one who has been assessed after having passed the postgraduate examination and is found to be able to work independently. A gazetting specialist is one who has passed the postgraduate examination in ophthalmology (MS or FRCS) but has to work under the supervision of a consultant senior specialist. A MO is one who has passed MBBS and has to be supervised by a specialist during surgery.
The types of intraoperative complications such as posterior capsular rupture (PCR) without vitreous loss, PCR with vitreous loss, central corneal edema, zonular dehiscence, dropped nucleus, and suprachoroidal hemorrhage were all recorded.
We looked to see if certain demographic features and presence of ocular comorbidities resulted in more complications. We studied the relationship between types of cataract surgery, whether done alone or in combination and the grade of a surgeon operating with the occurrence of an intraoperative complication.
The best-corrected visual acuity at 6 weeks postoperatively was taken. Refractions were done by hospital-based optometrists. The visual acuity was classified into – good vision (6/6–6/12), impaired vision (6/18–6/36), and poor vision (6/60 and worse). The outcome of each of the intraoperative complications was studied.
We analyzed the reasons for not obtaining good visual acuity following intraoperative complications. These included high astigmatism, posterior capsule opacification, cystoid macular edema (CME), endophthalmitis, preexisting ocular comorbidity, corneal decompensation, intraocular lens (IOL) decentration and retinal detachment (RD).
Statistics
The data were analyzed with IBM SPSS Statistics for Windows, Version 20.0 (IBM Corp., Released 2011, Armonk, NY, USA). Global Chi-square and Fisher's exact tests were used to determine the possible relation between two categorical variables. Logistic regression test was performed to determine the strongest factors between the categorical data. P < 0.05 was considered statistically significant.
Results
A total of 12,992 eyes underwent cataract surgery from 2007 to 2014 with 6.1% registering intraoperative complications. Some had >1 intraoperative complication during surgery as shown in Table 1. Due to some missing data, only available data were analyzed in various sections of the study.
Table 1.
Total intraoperative complications from 2007 to 2014
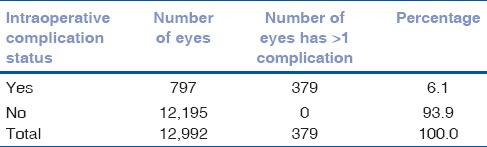
Fig. 1 shows the trend of intraoperative complications from the year 2007 to 2014. The highest number of intraoperative complications was recorded in 2013 (18.3%) followed by 13.9% in 2014, The lowest number of intraoperative complications was recorded in 2012 (9.2%).
Figure 1.
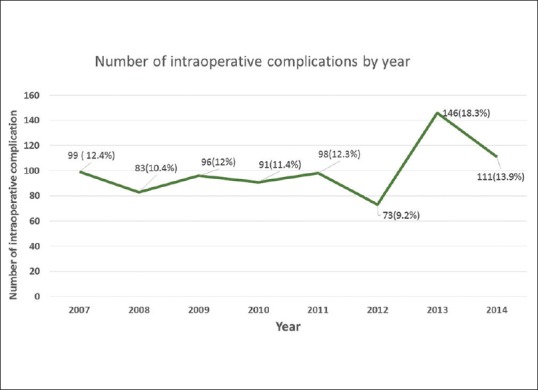
Trend of Intraoperative complications (2007–2014)
Fig. 2 shows that there was a drop in the number of MOs and gazetting specialist handling cataract surgery in 2012 (n = 190) with the number doubling in 2013 (n = 366).
Figure 2.
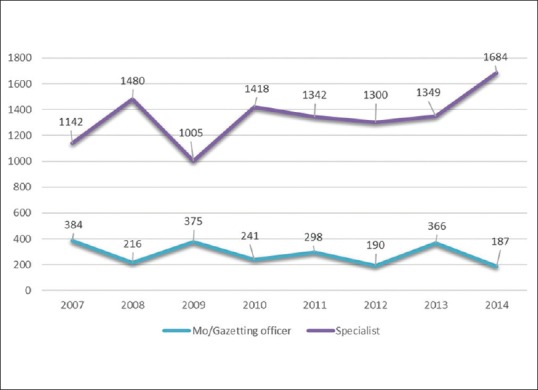
Number of medical officers/gazetting specialist and Specialists handling cataract surgery
As seen in Fig. 3, PCR was the main cause of intraoperative complications from 2007 to 2014 with the highest number of cases recorded in 2013 (114 cases). A large number of cases of vitreous loss and zonular dehiscence were also seen from 2007 to 2014. Fewer cases of dropped nucleus, suprachoroidal hemorrhage, and corneal edema occurred during cataract surgery.
Figure 3.
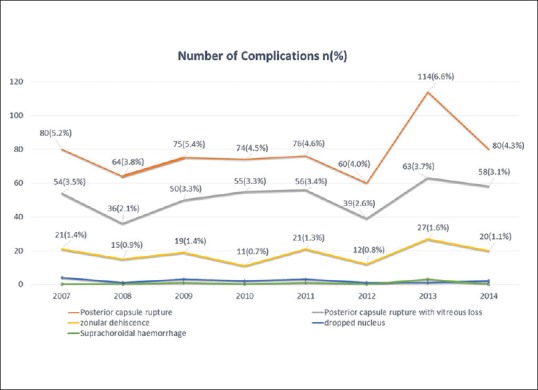
Types of intraoperative complications by year
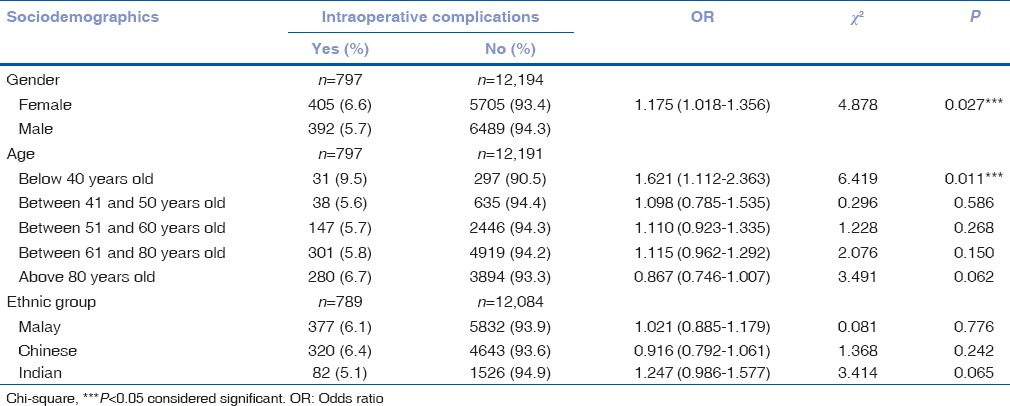
Table 2 shows that gender (P < 0.05) and age below 40 years old (P < 0.05) were significantly associated with intraoperative complications while ethnicity was not significantly associated with intraoperative complications (P > 0.05). Females (6.6%) had more intraoperative complications compared to males (5.7%). The highest percentage of intraoperative complications was seen in those aged below 40 years (9.5%) followed by those above 80 years old (6.7%).
Table 2.
Association between sociodemographic status and intraoperative complications
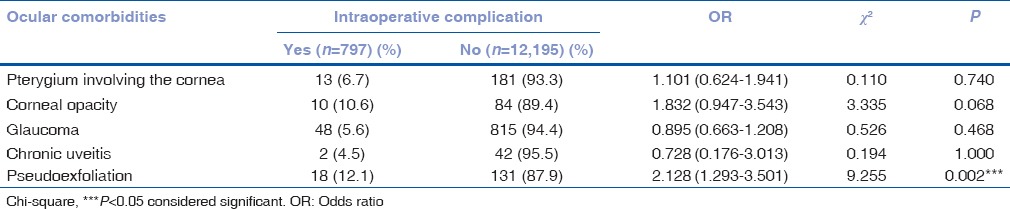
Pseudoexfoliation was the only ocular comorbidity significantly associated with intraoperative complications (P < 0.05) and accounted for 12.1% of complications from 2007 to 2014 [Table 3].
Table 3.
Association between sociodemographic status and intraoperative complications
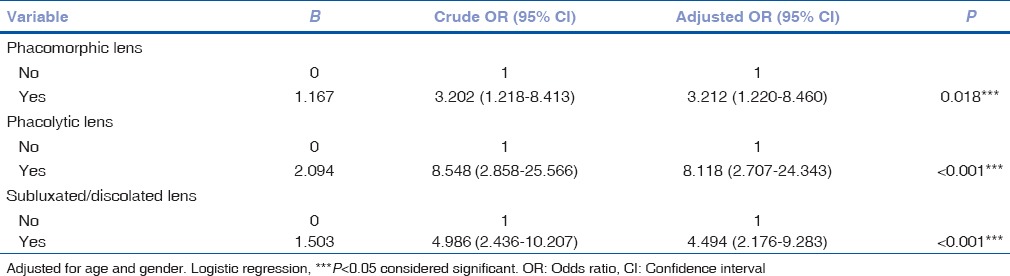
When adjusted for age group and gender, phacolytic lens, phacomorphic lens, and subluxated lens were noted to have odds of 8.118, 4.494, and 3.212 respectively of acquiring intraoperative complications as compared to other lens (P < 0.05) [Table 4].
Table 4.
Association between lens and intraoperative complication by logistic regression
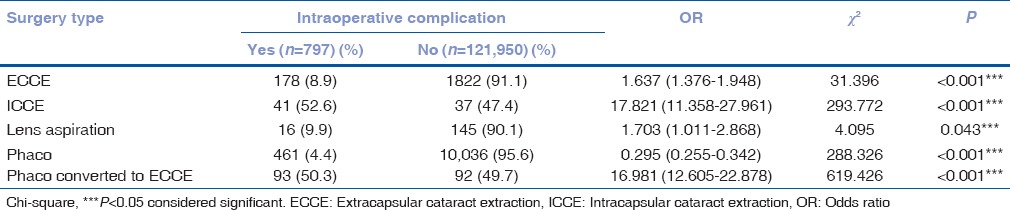
All types of surgery were significantly associated with intraoperative complications (P < 0.05) [Table 5]. ICCE (52.6%) and phaco converted to ECCE (50.3%) were the most common techniques of cataract surgeries that caused intraoperative complications followed by lens aspiration (9.9%), ECCE (58.9%), and phaco (4.4%) as shown in Table 5.
Table 5.
The association between type of cataract surgery and intraoperative complication
Surgeon grade was significantly associated with intraoperative complications. MOs (11.7%) had more intraoperative complications compared to gazetting specialists (10.1%) and specialist (5.1%) as seen in Table 6.
Table 6.
The association between grade of surgeon and intraoperative complication

Intraoperative complications were significantly associated with visual outcomes as shown in Table 7. More patients who had intraoperative complications got impaired/poor vision outcome (12.4%). Patients with intraoperative complication had 3.3 times likelihood of having impaired/poor vision outcome compared to patients without intraoperative complication (3.033, 2.554–3.601).
Table 7.
The association between intraoperative complication and visual outcome
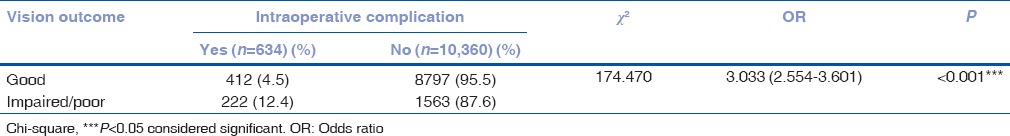
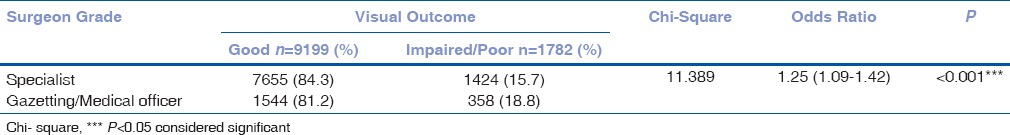
Table 8 shows that there was a significant association between surgeon grade and visual outcomes. It was noted that patients who were operated upon by specialists had 1.25 odds of having good visual outcome as compared to patients who were operated on by gazetting/MOs (P < 0.001).
Table 8.
The Association between grade of surgeon and visual outcome among cases with intraoperative complications
Reasons for not obtaining good acuity were analyzed after excluding the cases with preexisting ocular comorbidities. Fig. 4 shows that high astigmatism (4.9%) was the main reason for not obtaining good visual acuity after surgery. The other reasons were CME (1.3%), corneal decompensation (0.6%), posterior capsular opacity (0.6%), RD (0.3%), infective endophthalmitis (0.1%), and IOL decentration/discolation (0.1%).
Figure 4.
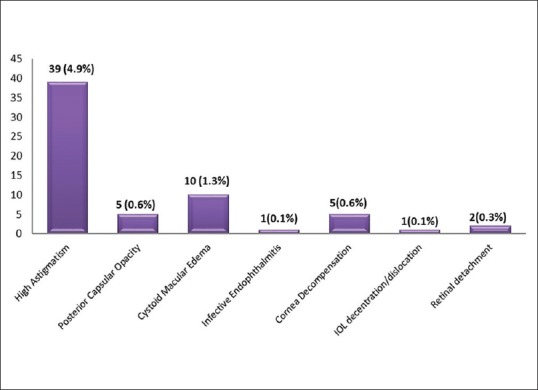
Reasons for not obtaining good visual acuity among patients with intraoperative complications
Discussion
In this retrospective study of the NED, we focused on the intra- and post-operative complications of cataract surgery over 8 years in a Malaysian tertiary hospital. Out of 12,992 eyes undergoing cataract surgery, only 6.1% had a variety of intraoperative complications, some of which had >1 complication. Other centers recorded fewer complications of 1.4%,[2] 1.9%,[3] but higher rates than ours were also found (8.5%).[4]
There was a drop in complications in 2012 followed by a rapid rise in 2013 after which it got back to almost to the usual rate of complications. This trend of complications was seen in the three major types of complications, namely, PCR, vitreous loss, and zonular dehiscence. Throughout the 8 years, the pattern of complications correlated with the increase and decrease in the number gazetting specialists and MOs.
Females and extremes of ages (below 40 years and above 80 years) had more complications. Females and those above 70 were found to have more complications in other studies too.[2] Complications were not affected by ethnicity.
Pseudoexfoliation was the only ocular comorbidity associated with intraoperative complications. Cataract complications were also higher in cases with pseudoexfoliation in northeast of Spain.[5] Other studies do not show an association between the presence of pseudoexfoliation and intraoperative complications.[6] Thanigasalam et al. and Sufi found no correlation was found between PCR and the presence of PXM during phacoemulsification.[7,8] Pterygium involving the cornea, corneal opacity, glaucoma, and chronic uveitis were not associated with intraoperative complications in our study. Pterygium and corneal opacities extending to the visual axis may hamper the view for capsulorhexis and phacoemulsification, but this did not cause an increase in complications. Patients with glaucoma can have raised intraocular pressures if not controlled. Uveitis associated with posterior synechiae and small pupils are also a challenge for the surgeon.
Any sort of abnormal lens status, be it phacomorphic, phacolytic, subluxated, or dislocated lenses, is a nightmare for a cataract surgeon. Phacolytic lenses had the highest rate of complications followed by subluxated/dislocated lenses and least of all were the phacomorphic lenses. A point to note is that, after adjusting for age and abnormal status of lenses, we found that men had a higher rate of the odds of getting an intraoperative complication. No significant intraoperative complications were noted during surgery for 74 eyes with phacomorphic lenses.[9] ECCE or ICCE are the preferred technique for cataract extraction of subluxated lenses in our center. No significant difference in intraoperative complications was found between phaco and manual small incision surgery for subluxated lenses.[10] We should have perhaps used devices such as capsular tension rings which have been shown to reduce complications for subluxated lenses.[11,12] Most studies describe the postoperative outcomes of abnormal lens status but not about the intraoperative complications.
We found that all types of cataract surgeries had complications but the highest was for phaco convert to ECCE and the least was for phaco. Phaco convert to ECCE are cases where phaco was commenced, but at some point during the procedure, the surgeon had noticed some abnormality that could lead to further problems. These include a tear or extension of the anterior capsule, a cataract which is found to be hard, a lens which is not stable or even recognition of vitreous in the anterior chamber.
Other studies have also found that the type of cataract surgery was also associated with complications.[13] However, there are also studies that found no association between the occurrences of intraoperative complications with the type of cataract surgery done.[14,15] Phaco had the least complications in a number of studies.[16,17,18]
MOs had more complications compared to the gazetting specialists who in turn had more complications than the specialists. Complicated cases in our hospital are done by specialists. This shows that more experienced surgeons who had done more cases had fewer complications. This fact is supported by several other studies as well.[15,19,20] Vitreous loss, dropped nucleus, PCR rates all dropped with increased experience as more cases were done by the same surgeon.[21] Other studies have disproved this concept as they found that experience of the surgeon did not affect the occurrence of complications.[13,17]
The data did not have the point of occurrence of the intraoperative complication. This would have been interesting to see if there was a variation in the point at which complications occurred or were recognized. One study showed that consultants got PCR during cortex removal and specialists got it more during segment removal.[22]
After excluding eyes with preexisting comorbidities, we found that the occurrence of intraoperative complications was detrimental to vision as they resulted in impaired and poor vision. In our study, the grade of the surgeon operating also affected the visual outcomes among the complicated cases. Specialists got good outcomes compared to the gazetting specialists and MOs. The main reasons for the poorer outcomes were high astigmatism, CME, and corneal decompensation. For some patients, the reasons for poor vision were not known. Ocular computed tomography was not available to diagnose subclinical conditions of poor visual outcomes. Most patients with PCR had a favorable visual outcome with meticulous vitrectomy and insertion of a foldable IOL to prevent astigmatism.[23] In a 5-year audit of PCR, age >65 years, dropped nuclei, and postoperative retinal, corneal, and IOL complications were found to cause poor outcomes.[24] Poor visual outcomes following vitreous loss were associated with poor preoperative vision, age-related macular degeneration, CME, and anterior PPV for nuclear fragment loss.[25]
Conclusion
This study involves a large series of patients utilizing the national database. However, the results reflect the practice in only one center and do not reflect the practice patterns and outcomes of the entire nation. Future research should be done using multicenter data.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank the Director General of Health for granting permission to publish the study. We thank the Director of CRC Dr. Goh PP and Coordinator of NED Teng KM for providing the data.
References
- 1.Zainal M, Ismail SM, Ropilah AR, Elias H, Arumugam G, Alias D, et al. Prevalence of blindness and low vision in Malaysian population: Results from the National Eye Survey 1996. Br J Ophthalmol. 2002;86:951–6. doi: 10.1136/bjo.86.9.951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Matta S, Park J, Shantha GP, Khanna RC, Rao GN. Cataract surgery visual outcomes and associated risk factors in secondary level eye care centers of L V Prasad Eye Institute, India. PLoS One. 2016;11:e0144853. doi: 10.1371/journal.pone.0144853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Venkatesh R, Muralikrishnan R, Balent LC, Prakash SK, Prajna NV. Outcomes of high volume cataract surgeries in a developing country. Br J Ophthalmol. 2005;89:1079–83. doi: 10.1136/bjo.2004.063479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lam DS, Congdon NG, Rao SK, Fan H, Liu Y, Zhang L, et al. Visual outcomes and astigmatism after sutureless, manual cataract extraction in rural China: Study of cataract outcomes and up-take of services (SCOUTS) in the caring is hip project, report 1. Arch Ophthalmol. 2007;125:1539–44. doi: 10.1001/archopht.125.11.eeb70013. [DOI] [PubMed] [Google Scholar]
- 5.Romero-Aroca P, Masip-Serra R, Martínez-Salcedo I, Salvat-Serra M, Fernández-Ballart J, Bautista-Pérez A. High prevalence of pseudoexfoliation syndrome and its complications in Tarragona in Northeast Spain. Eur J Ophthalmol. 2011;21:580–8. doi: 10.5301/EJO.2011.6254. [DOI] [PubMed] [Google Scholar]
- 6.Dwivedi NR, Dubey AK, Shankar PR. Intraoperative and immediate postoperative outcomes of cataract surgery using phacoemulsification in eyes with and without pseudoexfoliation syndrome. J Clin Diagn Res. 2014;8:VC01–5. doi: 10.7860/JCDR/2014/10004.5277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thanigasalam T, Sahoo S, Kyaw Soe HH. Posterior capsule rupture during phacoemulsification among patients with pseudoexfoliation-is there a correlation? Malays J Med Sci. 2014;21:51–3. [PMC free article] [PubMed] [Google Scholar]
- 8.Sufi AR, Singh T, Mufti AA, Rather MH. Outcome of phacoemulsification in patients with and without pseudoexfoliation syndrome in Kashmir. BMC Ophthalmol. 2012;12:13. doi: 10.1186/1471-2415-12-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ramakrishanan R, Maheshwari D, Kader MA, Singh R, Pawar N, Bharathi MJ. Visual prognosis, intraocular pressure control and complications in phacomorphic glaucoma following manual small incision cataract surgery. Indian J Ophthalmol. 2010;58:303–6. doi: 10.4103/0301-4738.64136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goel R, Kamal S, Kumar S, Kishore J, Malik KP, Angmo Bodh S, et al. Feasibility and complications between phacoemulsification and manual small incision surgery in subluxated cataract. J Ophthalmol 2012. 2012:205139. doi: 10.1155/2012/205139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vasavada V, Vasavada VA, Hoffman RO, Spencer TS, Kumar RV, Crandall AS. Intraoperative performance and postoperative outcomes of endocapsular ring implantation in pediatric eyes. J Cataract Refract Surg. 2008;34:1499–508. doi: 10.1016/j.jcrs.2008.04.044. [DOI] [PubMed] [Google Scholar]
- 12.Praveen MR, Vasavada AR, Singh R. Phacoemulsification in subluxated cataract. Indian J Ophthalmol. 2003;51:147–54. [PubMed] [Google Scholar]
- 13.Thanigasalam T, Reddy SC, Chinna K. The Temerloh hospital cataract complications study: Factors associated with, types and outcomes of cataract surgery complications. Int J Ophthalmol. 2014;8:1367–72. [Google Scholar]
- 14.Thevi T, Reddy SC, Shantakumar C. Outcome of phacoemulsification and extracapsular cataract extraction: A study in a district hospital in Malaysia. Malays Fam Physician. 2014;9:41–7. [PMC free article] [PubMed] [Google Scholar]
- 15.Haripriya A, Chang DF, Reena M, Shekhar M. Complication rates of phacoemulsification and manual small-incision cataract surgery at Aravind Eye Hospital. J Cataract Refract Surg. 2012;38:1360–9. doi: 10.1016/j.jcrs.2012.04.025. [DOI] [PubMed] [Google Scholar]
- 16.Hashemi H, Alipour F, Rezvan F, Khabazkhoob M, Alaeddini F, Fotouhi A. Intraoperative complications of cataract surgeries in Iran: 2000-2005 Iranian cataract surgery survey. Iran J Ophthalmol. 2011;23:3–10. [Google Scholar]
- 17.Thanigasalam T, Reddy SC, Zaki RA. Factors Associated with complications and postoperative visual outcomes of cataract surgery; a study of 1,632 cases. J Ophthalmic Vis Res. 2015;10:375–84. doi: 10.4103/2008-322X.158892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hashemi H, Khabazkhoob M, Rezvan F, Etemad K, Gilasi H, Asgari S, et al. Complications of cataract surgery in Iran: Trend from 2006 to 2010. Ophthalmic Epidemiol. 2016;23:46–52. doi: 10.3109/09286586.2015.1083037. [DOI] [PubMed] [Google Scholar]
- 19.Artzén D, Lundström M, Behndig A, Stenevi U, Lydahl E, Montan P. Capsule complication during cataract surgery: Case-control study of preoperative and intraoperative risk factors: Swedish Capsule Rupture Study Group Report 2. J Cataract Refract Surg. 2009;35:1688–93. doi: 10.1016/j.jcrs.2009.05.026. [DOI] [PubMed] [Google Scholar]
- 20.Chen M, Lamattina KC, Patrianakos T, Dwarakanathan S. Complication rate of posterior capsule rupture with vitreous loss during phacoemulsification at a Hawaiian cataract surgical center: A clinical audit. Clin Ophthalmol. 2014;8:375–8. doi: 10.2147/OPTH.S57736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martin KR, Burton RL. The phacoemulsification learning curve: Per-operative complications in the first 3000 cases of an experienced surgeon. Eye (Lond) 2000;14(Pt 2):190–5. doi: 10.1038/eye.2000.52. [DOI] [PubMed] [Google Scholar]
- 22.Thanigasalam T, Sahoo S, Ali MM. Posterior capsule rupture with/without vitreous loss during phacoemulsification in a Hospital in Malaysia. Asia Pac J Ophthalmol (Phila) 2015;4:166–70. doi: 10.1097/APO.0000000000000056. [DOI] [PubMed] [Google Scholar]
- 23.Trinavarat A, Neerucha V. Visual outcome after cataract surgery complicated by posterior capsule rupture. J Med Assoc Thai. 2012;95(Suppl 4):S30–5. [PubMed] [Google Scholar]
- 24.Ti SE, Yang YN, Lang SS, Chee SP. A 5-year audit of cataract surgery outcomes after posterior capsule rupture and risk factors affecting visual acuity. Am J Ophthalmol. 2014;157:180–5.e1. doi: 10.1016/j.ajo.2013.08.022. [DOI] [PubMed] [Google Scholar]
- 25.Konstantopoulos A, Yadegarfar G, Madhusudhana K, Canning C, Luff A, Anderson D, et al. Prognostic factors that determine visual outcome following cataract surgery complicated by vitreous loss. Eur J Ophthalmol. 2009;19:247–53. doi: 10.1177/112067210901900212. [DOI] [PubMed] [Google Scholar]


