Sir,
We report a case of ocular surface squamous neoplasia (OSSN) in-patient with non-Hodgkin's lymphoma (NHL). A 64-year-old man presented with complaints of foreign body sensation, redness, and blurring of vision in the right eye of 6 months’ duration. On ocular examination, we noted a gelatinous mass at superior limbus from 3 to 9 o’clock position extending over the cornea and sclera. Brown- and black-pigmented areas were seen over the mass [Fig. 1]. The prominent vessel was seen superiorly with few tributaries. Both eyes had visual acuity of 20/200 with cataractous lens. Intraocular pressure was 18 mmHg. Dilated fundus examination and ultrasonography of the orbit were normal in both eyes.
Figure 1.
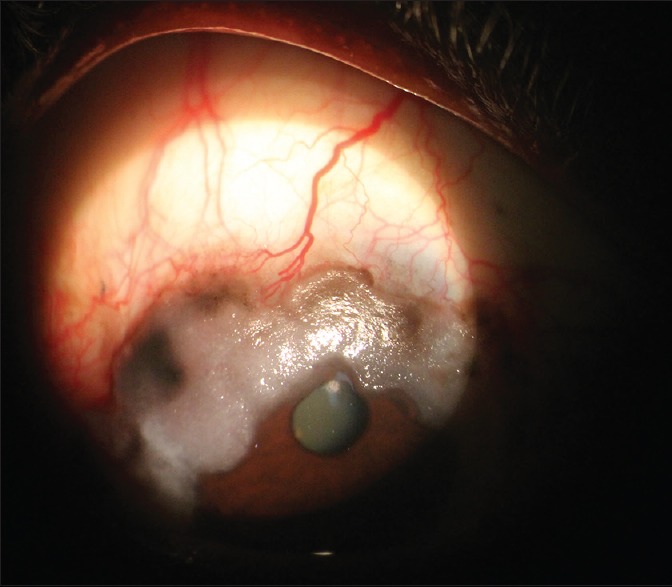
Slit lamp appearance of ocular surface squamous neoplasia: Gelatinous leukoplakic features at the superior limbus
Systemic examination revealed submandibular and cervical lymphadenopathy and hepatosplenomegaly. The left cervical lymph node biopsy was suggestive of NHL of small lymphocyte type. Bone marrow study was indicative of NHL of low grade of B-cell phenotype. He was HIV-negative. No systemic chemotherapeutic or immunosuppressive therapy was advised to the patient.
An excisional biopsy of the ocular lesion with surrounding 4-mm margin was performed under local anesthesia. Histopathological examination was suggestive of carcinoma - in situ of squamous cell variety [Fig. 2]. Postoperatively, the patient was treated for 4 weeks with topical 0.04% mitomycin-C eye drops. No recurrence was noted during 1-year follow-up.
Figure 2.
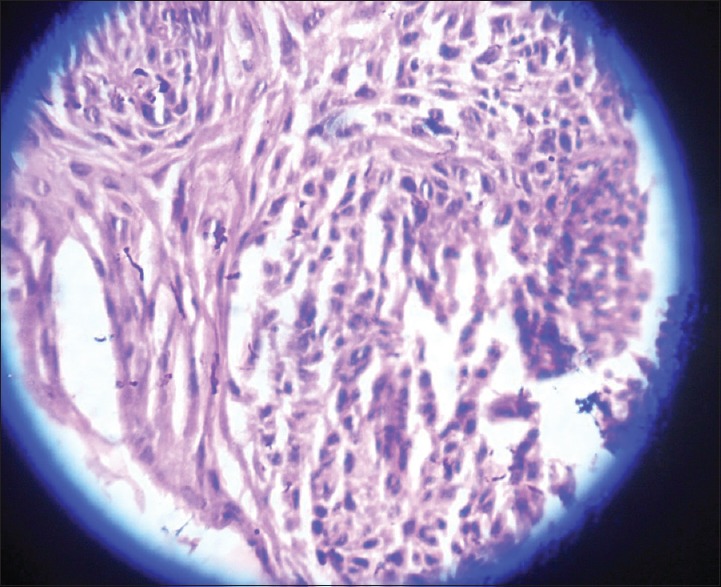
Histological appearance of ocular surface squamous neoplasia: Atypical squamous cells invading the stroma
The incidence of OSSN is strongly associated with solar ultraviolet radiation, HIV, and human papillomavirus.[1] Most lesions are noted in the interpalpebral opening. Nasal limbus is commonly affected. In our patient, the lesion was situated at the superior limbus covered by the upper lid excluding the possibility of ultraviolet light as a cause for the lesion. Other probable factors comprise of having an outdoor occupation, fair skin-iris, chemical exposure, some medications (like antimalignant drugs), chronic inflammatory diseases of eye, vitamin A deficiency, mechanical trauma (e.g., ocular prosthesis), contact lens users, and a history of actinic skin lesions. None of the factors mentioned were present in this patient.
NHL is one of the causes for an extranodal mucosa-associated lymphoid tissue.[2] However, such type lesions are generally seen hidden under the eyelid in the bulbar conjunctiva or in the fornix, rather than at the more discernible limbal site.[3] Our patient had limbal lesion and was rapidly progressive for 6 months.
Exact etiological factor leading to OSSN inpatient with NHL is not known. Immune deficiency is one of the strongest known risk factors for NHL. Grulich et al. have shown altered immunity as one of the risk factors for the development of NHL.[4] Immunosuppression impairs tumor immune surveillance allowing survival of aberrant cells.[5]
In a patient with NHL, the expected ocular surface manifestation would be a conjunctival lymphoma, but the uniqueness of this report is that the patient presented with an OSSN with no obvious risk factor or cause of immunosuppression except the lymphoma.
OSSN is currently largely ignored, as it is largely related with systemic diseases. OSSN in NHL is not known. Systemic periodic ophthalmic examination in – patient with NHL may help ensure the early diagnosis of subtle OSSN, as early stages it does not affect vision.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
I acknowledge Dr. Meena Anand Pangarkar, Associate Professor, Department of Pathology, Government Medical College, Nagpur, Maharashtra, India, for histopathology report.
References
- 1.Gichuhi S, Sagoo MS, Weiss HA, Burton MJ. Epidemiology of ocular surface squamous neoplasia in Africa. Trop Med Int Health. 2013;18:1424–43. doi: 10.1111/tmi.12203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coupland SE, Krause L, Delecluse HJ, Anagnostopoulos I, Foss HD, Hummel M, et al. Lymphoproliferative lesions of the ocular adnexa. Analysis of 112 cases. Ophthalmology. 1998;105:1430–41. doi: 10.1016/S0161-6420(98)98024-1. [DOI] [PubMed] [Google Scholar]
- 3.Shields CL, Shields JA, Carvalho C, Rundle P, Smith AF. Conjunctival lymphoid tumors: Clinical analysis of 117 cases and relationship to systemic lymphoma. Ophthalmology. 2001;108:979–84. doi: 10.1016/s0161-6420(01)00547-4. [DOI] [PubMed] [Google Scholar]
- 4.Grulich AE, Vajdic CM, Cozen W. Altered immunity as a risk factor for non-Hodgkin lymphoma. Cancer Epidemiol Biomarkers Prev. 2007;16:405–8. doi: 10.1158/1055-9965.EPI-06-1070. [DOI] [PubMed] [Google Scholar]
- 5.Gichuhi S, Ohnuma S, Sagoo MS, Burton MJ. Pathophysiology of ocular surface squamous neoplasia. Exp Eye Res. 2014;129:172–82. doi: 10.1016/j.exer.2014.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]


