Abstract
Prostate cancer (PCa) remains the second-leading cause of cancer-related deaths in American men with an estimated mortality of more than 26,000 in 2016 alone. Aggressive and metastatic tumors are treated with androgen deprivation therapies (ADT); however, the tumors acquire resistance and develop into lethal castration resistant prostate cancer (CRPC). With the advent of better therapeutics, the incidences of a more aggressive neuroendocrine prostate cancer (NEPC) variant continue to emerge. Although de novo occurrences of NEPC are rare, more than 25% of the therapy-resistant patients on highly potent new-generation anti-androgen therapies end up with NEPC. This, along with previous observations of an increase in the number of such NE cells in aggressive tumors, has been suggested as a mechanism of resistance development during prostate cancer progression. Dovitinib (TKI-258/CHIR-258) is a pan receptor tyrosine kinase (RTK) inhibitor that targets VEGFR, FGFR, PDGFR, and KIT. It has shown efficacy in mouse-model of PCa bone metastasis, and is presently in clinical trials for several cancers. We observed that both androgen receptor (AR) positive and AR-negative PCa cells differentiate into a NE phenotype upon treatment with Dovitinib. The NE differentiation was also observed when mice harboring PC3-xenografted tumors were systemically treated with Dovitinib. The mechanistic underpinnings of this differentiation are unclear, but seem to be supported through MAPK-, PI3K-, and Wnt-signaling pathways. Further elucidation of the differentiation process will enable the identification of alternative salvage or combination therapies to overcome the potential resistance development.
Introduction
Prostate cancer remains the second leading cause of cancer-related deaths in American men with 26,120 estimated deaths in 2015 [1]. Radical prostatectomy, with or without radiation, comprises the primary line of curative treatment. The metastatic tumors are treated with androgen-lowering agents and androgen-receptor inhibitors. However, the tumors eventually acquire resistance to such androgen deprivation therapy (ADT) and develop into lethal castration resistant prostate cancer (CRPC). The development of resistance is, in part, due to the reactivation of androgen-receptor (AR) signaling [2], which prompted the development and subsequent Food and Drug Administration (FDA) approval of enzalutamide, an improved androgen-receptor antagonist, and abiraterone, a local androgen biosynthesis blocker [3], [4]. However, not all patients respond to the new therapies, and 50% of those who respond eventually develop resistance to the new therapies within 2 years [5], [6], [7], [8]. Importantly, more than 25% of the therapy-resistant patients end up with a more aggressive and treatment resistant form of the disease neuroendocrine prostate cancer (NEPC) [9].
Neuroendocrine differentiation (NED) includes focal NED and pure NED, also known as small cell PCa. Pure NED (cancer of the NE cells) is very rare (0.5–2%) and carries very poor prognosis with the probability of survival being less than 1 year [10]. Focal NED can be classified into four sub-groups, a) adenocarcinomas with focal NE differentiation, b) Paneth-cell-like NE differentiation, c) large cell NEPC, and d) small cell NEPC [10], [11], [12]. NE cells are present in small numbers in the normal prostate and are thought to support the basal and luminal cells, during normal development and malignancy, through the secretion of various neuropeptides [13]. The number of NE cells present within the tumor has been shown to increase with disease aggressiveness [11], [13] and thus, has been purported to play a role in resistance development [14]. Indeed, prolonged androgen deprivation therapy (ADT) or radiation therapy increase NE differentiation of PCa cells [15], [16]. Moreover, stimulation with factors such as cAMP and interleukin-6 (IL-6) leads to the differentiation of PCa cells into a NE phenotype in vitro and in vivo [17], [18], [19], [20]. Studies looking at the mechanism of various ligand-induced NE differentiation processes have implicated the JAK/STAT pathway specifically through STAT3 [21], the PI3K- [22], [23], MAPK- [23], and Wnt- signaling pathways [24].
Dovitinib (TKI-258/CHIR-258) is a pan receptor tyrosine kinase (RTK) inhibitor that primarily targets fibroblast growth factor receptor (FGFR), vascular endothelial growth factor receptor (VEGFR), platelet-derived growth factor receptor (PDGFR), fms-like tyrosine kinase 3 (FLT3) and Proto-Oncogene Receptor Tyrosine Kinase (c-KIT) [25]. It has shown anti-tumor activity in pre-clinical models of several cancers and is presently in clinical trials for prostate, renal, gastrointestinal, adenoid cystic, glioblastoma, urothelial, thyroid, pancreatic, breast, and non-small lung cancers [26], [27]. Here we show that both AR-positive and AR-negative cells differentiate into a NE phenotype when treated with Dovitinib, presumably as a modality of resistance development. Elucidation of the exact mechanism will enable the identification of alternative salvage or combination therapies to overcome the resistance-development.
Material and Methods
Cell Lines and Reagents
Human prostate cancer cell lines LNCaP, CWR22Rv1, Du145 and PC3 were obtained from American Type Culture Collection (Manassas, VA, USA) and cultured in RPMI 1640 media supplemented with 10% fetal bovine serum (FBS) in the presence of penicillin (100 U/mL) and streptomycin (100 μg/mL). Media, FBS, Penicillin, Streptomycin, and 0.25% trypsin/EDTA were purchased from Gibco-Invitrogen Corporation (Carlsbad, CA, USA). Cells were maintained at 37°C in a humidified atmosphere containing 5% CO2.
Dovitinib treatment: Cells were cultured in 10-cm dish until they reached ~70–80% confluence. Thereafter, they were treated with media containing Dovitinib (SelleckChem, S2769) at 6 μM concentration. Media with drug was replaced every 3 days.
Cell Viability Assay/WST
Cell viability was assessed using the cell impermeable water-soluble tetrazolium (WST-1) assay where cellular mitochondrial dehydrogenases of living cells cleave the tetrazolium salt to form purple colored formazan. After a three-day day Dovitinib treatment, cell proliferation was determined using the WST-1 reagent (Clontech, MK400) according to the manufacturer's instructions. Absorbance was read at 440 nm and 690 nm using a SpectraMax M5 Multimode Plate Reader. Actual sample absorbance values were calculated by subtracting sodium dodecyl sulfate (SDS)-treated negative control wells (at the time of setting up experiment) to eliminate noise from dead cells. Prism6 was used to plot and calculate IC50 values. All the assays were performed three independent times in triplicates.
Fluorescence Microscopy
LNCaP and PC3 cells were cultured in 6-cm dishes with uncoated, circular-glass coverslips and treated with Dovitinib (6 μM) for 3 weeks. Cells were fixed with 4% w/v formaldehyde in phosphate buffered saline (PBS) (pH 7.4) for 1 hour at room temperature, and then washed three times with PBS. Cells were permeabilized with 0.2% w/v Triton-X-100. Cells were washed with PBS again, and blocked in PBS containing 1% w/v bovine serum albumin (BSA) (1 hour at room temperature). Primary antibodies, anti-chromogranin A + B and anti-synaptophysin (kind gift from Dr. Michael Donovan, Department of Pathology, Icahn School of Medicine at Mount Sinai (ISMMS)), were diluted to 1:5000 and 1:200 in PBS containing 1% BSA, respectively. Cells were incubated in primary antibodies at 4°C overnight. Subsequently, the cells were washed three times in PBS containing 1% BSA (5 minutes per wash), and incubated at room temperature for 1 hour with anti-mouse immunoglobulin-G-tagged fluorescein isothiocyanate (IgG–FITC) antibody (Sigma, F0257) and anti-rabbit IgG antibody (Life Technologies, A-11008) respectively, at room temperature. Cells were washed three times using PBS with 1% BSA and mounted in antifade mounting medium with 4″,6-diamidino-2-phenylindole (DAPI) (Vector Laboratories, Burlingame, CA, USA; H-1200). Labeled cells were analyzed by Leica DM5500B fluorescence microscopy equipped with a 2-megapixel Leica monochrome camera (model DFC345FX) and Leica application suite (LAS) software.
Cell Lysate and Immunoblotting
The protein concentration of the samples was determined using a detergent-compatible bicinchoninic acid (BCA) protein assay (Quick Start Bradford Protein Assay Kit, Bio-Rad, Catalog number 5000201). The samples were diluted to the same quantity of protein (20 μg) using loading buffer (100 mM Tris–HCl pH 6.8, 2% SDS, 0.02% bromophenol blue, 20% glycerol, 2% β-mercaptoethanol), separated by SDS–polyacrylamide gel electrophoresis (PAGE) on 10% gels, and electro-transferred using a Mini Trans-Blot wet transfer system (Bio-Rad Catalog number 1703930) onto polyvinylidene fluoride (PVDF) membranes (Bio-Rad, catalog number 162–0177). Membranes were blocked in Tris-buffered saline containing 0.1% Tween-20 (TBST) and 5% non-fat milk for 1 hour. After blocking, the membranes were probed with following primary antibodies for immunodetection:mouse monoclonal anti-neuron specific enolase (NSE) [ENO2] (MRQ-55) antibody (1:5000; Ventana Medical Systems, Inc., catalog number 760–4786), rabbit monoclonal anti-phospho-AKT stain transforming (AKT) antibody (1:1000; Cell Signaling, catalog number 9614), mouse monoclonal anti-phospho-(MAPK) antibody (1:1000; Cell Signaling, catalog number 9106), rabbit polyclonal anti-(MAPK) antibody (1:1000; Cell Signaling, catalog number 9102), rabbit polyclonal anti-androgen receptor (AR) (N-20) antibody (1:1000; Santa Cruz Biotechnology, catalog number sc-816), and mouse monoclonal anti-β-actin antibody (1:1000; Santa Cruz Biotechnology, catalog number sc-47778). Membranes were incubated with primary antibodies on a rocking platform overnight at 4°C. The next day, the membrane was washed with TBST (3 times for 5 minutes each) and incubated with the following secondary antibodies for 1 hour on a rocking platform: anti-mouse IgG horseradish peroxidase (HRP)-linked antibody (1:10,000; Cell Signaling, catalog number 7076) or anti-rabbit IgG HRP-linked antibody (1:10,000; Cell Signaling, catalog number 7074). After a final step of washing, detection of antibody reactivity was performed using the Western Bright enhanced chemiluminescence (ECL) western blotting detection kit (Advansta Inc., catalog number K-12045-D50) and signals were captured using the ImageQuant LAS 4000 biomolecular imager (GE Healthcare Life Sciences).
Quantitative Real-Time PCR
Total RNA was extracted from cells using Qiagen RNAeasy kit (Qiagen catalog number 74104) and cDNA generated using the iScript cDNA Synthesis kit (Bio-Rad Laboratories, catalog number 1708891), according to the manufacturer's instructions. The cDNA were then amplified and transcripts detected using SYBR Green Supermix (Bio-Rad Laboratories, catalog number 1708880) in real-time PCR detection system (Bio-Rad CFX96, catalog number 1855196) using specific primers. Each sample was examined in triplicates and Ct values were collected for β-actin, glyceraldehyde 3-phosphate dehydrogenase (GAPDH), and the target genes during the log phase of the cycle. The levels of expression for the genes of interest were normalized to β-actin and GAPDH for each sample, and compared with the values obtained for the different samples. Each experiment was repeated at least 3 times in triplicates.
Mouse Xenograft Studies
All mice experiments were carried out at the Mount Sinai vivarium in accordance with institutional guidelines and approved by the Mount Sinai Medical Center Institutional Animal Care and Use Committee (IACUC) (protocol number 2014–0176).
PC3 cells (1 × 106 cells, 1:1 mixed with Matrigel™) (Corning, catalog number 356234) were injected subcutaneously into both flanks of 8-week-old male nude mice (Jackson laboratories, catalog number 007850) and tumors were allowed to grow without treatment. Tumor volume was measured every other day through direct measurement with calipers and calculated by the formula: 1/2(length x width2). When tumor volumes reached 200mm3, mice were treated with Dovitinib dissolved in saline (30 mg/kg per day), or same volume of saline for control, until the endpoint of experiment (1000 mm3) through oral gavage. At the end of the study, mice were sacrificed and tumors collected and stored at −80°C for protein extraction and Western blot analysis.
RTK Array
The screen for the presence of phosphorylated RTKs was carried out using the Human Phospho-RTK Array (R&D Systems, catalog number ARY001B) as per the manufacturer's instruction. Briefly, cells were harvested with 0.25% Trypsin–EDTA (Gibco, catalog number 25200056) and rinsed with PBS prior to lysis. Cells were solubilized in lysis buffer (1×107 cells/mL, R&D Systems with protease inhibitors, catalog number 895561) by gently rocking for 30 minutes at 4°C. Following blocking, 300 μg of proteins were added to the membranes and incubated overnight at 4°C with gentle agitation. After washing, horseradish peroxidase (HRP)-conjugated anti-phospho-tyrosine antibodies (1:2000) (supplied in the kit) were added to each membrane and incubated at room temperature for 2 hours on a gentle shaker. After another series of washes, proteins were visualized using the ECL detection reagent (Advansta Inc., catalog number K-12045-D50) and ImageQuant LAS 4000 biomolecular imager (GE Healthcare Life Sciences).
Statistical Analysis
Statistical analysis was performed using Prism6 (GraphPad Software) and Student's t test (two-tailed) was used for the comparison of differences; P values less than 0.05 were considered significant.
Results
Dovitinib is a pan RTK inhibitor targeting FGFR, VEGFR, PDGFR, and KIT [25]. To determine whether PCa cells are sensitive to Dovitinib, we tested the cytotoxicity effect of the drug on PCa cell lines LNCaP and PC3 using the WST assay. For this, cells were treated with increasing amounts of Dovitinib and the number of live cells left after 3-day treatments were quantified and IC50 curves plotted. Both the lines exhibited sensitivity to Dovitinib treatment with IC50 in the lower μM range, Supplementary Figure S1. In an effort to uncover the mechanism of resistance development, we set out to generate Dovitinib-resistant clones through the long-term treatment of PCa cell lines. However, we observed striking morphological changes in the PCa cells upon prolonged Dovitinib treatment.
Dovitinib-Treated PCa Cells Display Morphological Transformations Consistent with NE Differentiation (NED) and Express Transcripts Associated with NE Differentiation
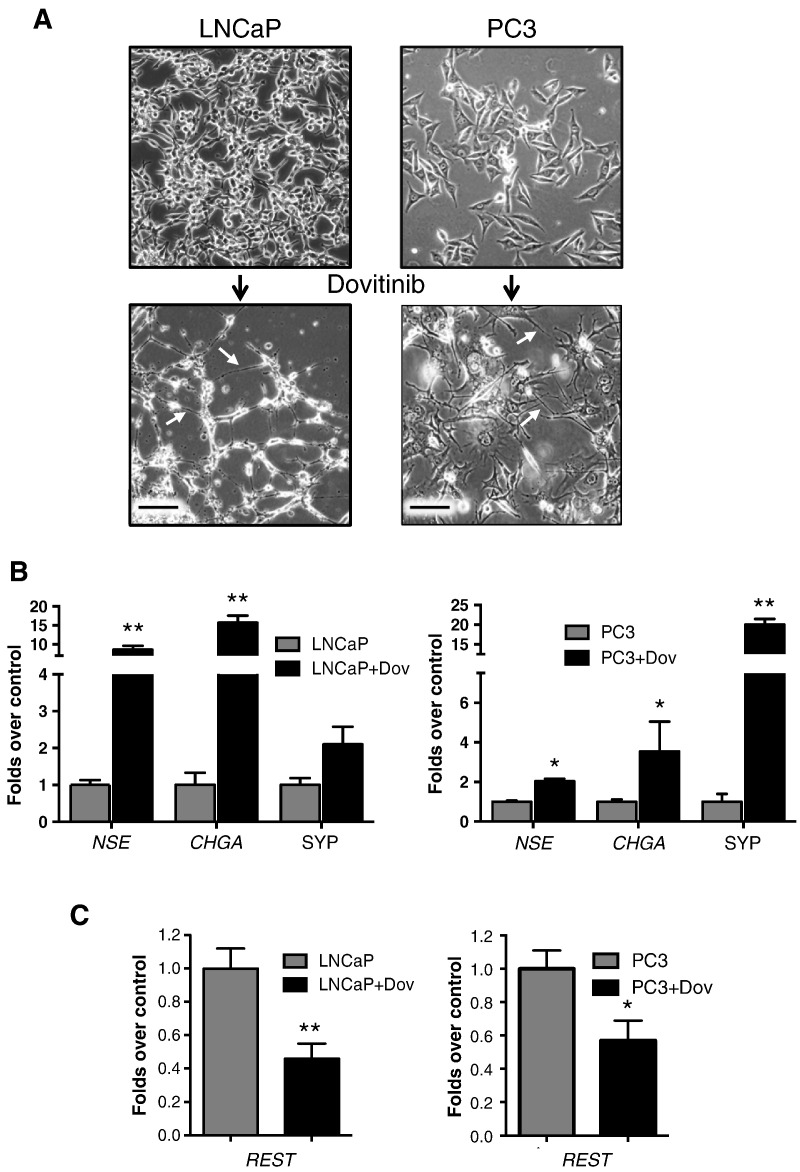
In the case of the AR-positive prostate adenocarcinoma cell line LNCaP, treatment with Dovitinib induced strong morphological alterations of reduced cell-body content and pronounced, elongated neurite-like processes, Figure 1A (left column). Phenotypically, these were consistent with previous reports of morphological alterations in LNCaP cells after anti-androgen treatment with cAMP or IL6 [15], [17], [28]. To test whether this effect extended to other PCa cell lines, we similarly treated the AR-negative CRPC cell line, PC3. Since PC3 cells have been reported to share NEPC characteristics [29], we were surprised to observe that similar to the observation in LNCaP cells, treatment of PC3 cells with Dovitinib resulted in the production of marked neurite-like processes, Figure 1A (right column). These observations were similar to previously reported outcomes of PC3 cells treated with cAMP [17]. Perhaps PC3 cells are at an intermediate stage where they are not completely terminally differentiated into the NEPC phenotype. To test whether this phenotype further extended to other PCa cell lines, we Dovitinib-treated Du145 (AR negative PCa cell line) and 22Rv1 (AR positive PCa cell line) cells with Dovitinib and looked for the formation of neurite-like structures. Upon treatment with Dovitinib, both these lines also exhibited pronounced branched neurite-like formations suggesting it to be a universal phenomenon for PCa cells lines, Supplementary Figure S2.
Figure 1.
Induction of the neuronal morphology in PCa cells upon treatment with Dovitinib and expression of NE markers. A, Representative images of LNCaP and PC3 cells treated with 6 μM Dovitinib for 3 weeks (bottom row) or not (top row). Images captured at 20× magnification using a bright-field microscope. Arrow heads point to neurite-like cellular outgrowth. Scale bar = 100 μM. B, Increased expression of NE markers upon Dovitinib treatment in LNCaP (left) and PC3 (right) cells. C. Levels of REST transcript in LNCaP (left) and PC3 (right) cells. B and C, Cells were treated with 6 μM Dovitinib for 3 weeks and the levels of mRNA of the indicated genes quantified using qRT-PCR using specific primers (See Methods). Values were normalized to GAPDH, and results plotted as fold change over control cells. Plot is representative of 3 independent experiments conducted in triplicates. (Error bars: S.E.) *P < .05, ** P < .01.
NE differentiation is characterized by the varying levels of expression of neuronal markers such as neuron specific enolase (NSE), chromogranin A (CHGA) or synaptophysin (SYP) [30], [31]. To test whether the morphological changes observed with Dovitinib treatment also resulted in the expression of the above NE markers, both LNCaP and PC3 cells were treated with Dovitinib and their cellular RNA subjected to qPCR analysis using gene-specific primers. Dovitinib treatment induced a 10-fold increase in NSE mRNA expression in LNCaP cells when compared to untreated controls, and a 5-fold increase in PC3 cells compared similarly, Figure 1B. The level of chromogranin A was observed to be around 15-fold higher in LNCaP cells treated with Dovitinib when compared with untreated control, and was more than 3-fold higher in the case of treated PC3 cells when compared to untreated PC3 controls Figure 1B (right panel). The expression of SYP was 2-fold higher in Dovitinib-treated LNCaP cells and more than 15-fold higher for Dovitinib-treated PC3 cells. Taken together, treatment of prostate cancer cells with Dovitinib led to morphological trans-differentiation accompanied by the expression of the transcripts encoded by these three widely used NE-markers.
The repressor element (RE)-1 silencing transcription factor (REST), which represses neuronal gene expression in non-neuronal tissues, has been shown to be suppressed in NEPC [32], [33], [34]. To test whether treatment of PCa cells with Dovitinib resulted in suppression of REST, we compared the level of REST transcripts in 3-week Dovitinib treated cells to control cells. As shown in Figure 1C, we observed a significant suppression of REST levels in Dovitinib treated LNCaP (Figure 1C, left) and PC3 (Figure 1C, right) cells. Taken together, the above observations suggest that treatment of PCa cells with Dovitinib induces expression of markers associated with NE differentiation and suppression of REST.
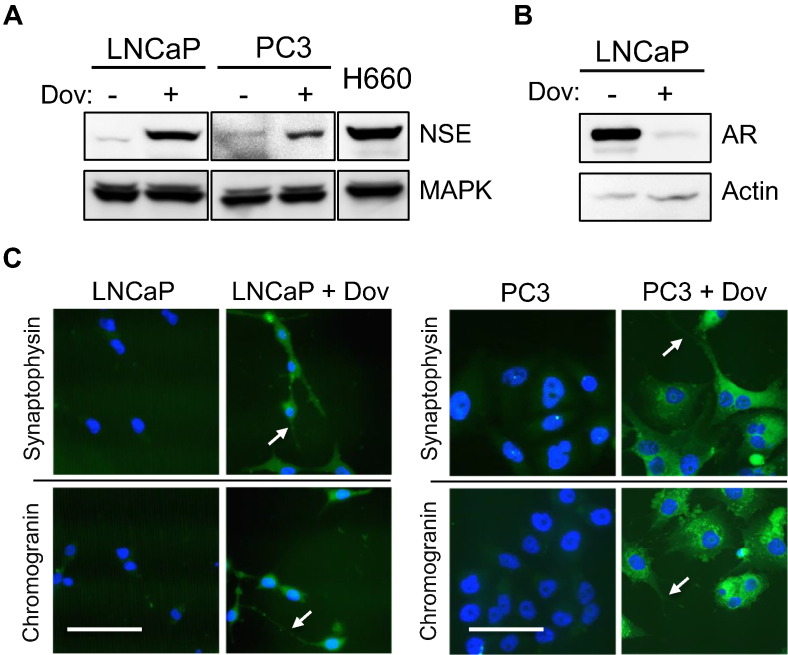
Detection of Proteins Associated with NE Differentiation Upon Dovitinib-Treatment of PCa Cells
To test whether the observed increase in mRNA expression levels resulted in protein expression, both LNCaP and PC3 cells were treated with Dovitinib and their cell-lysate subjected to western blot analysis using anti-NSE antibody. Predictably, Dovitinib treatment induced a marked increase in NSE expression in LNCaP cells when compared to untreated control. The relative increase in NSE expression was however modest in the case of PC3 cells treated similarly, Figure 2A. In vitro NEPC trans-differentiation has been shown to be associated with a loss in AR expression [20], [30]. To test whether Dovitinib-mediated NE transdifferentiation led to a similar response, lysates of 3-week Dovitinib treated AR-positive cell-line LNCaP was subjected to western blot analysis and compared with control cells. As observed in Figure 2B concomitant with increase in NSE, Dovitinib treatment of LNCaP cells led to a considerable suppression of AR expression. To test the levels of chromogranin and synaptophysin, we employed indirect immunofluorescence to detect the levels of proteins expressed by the above genes. Both PC3 and LNCaP cells were grown on coverslips and treated with Dovitinib for 3 weeks. The treated cells were then probed with anti-synaptophysin and anti-chromogranin A/B antibodies and compared with control cells. Both PC3 and LNCaP cells treated with Dovitinib displayed increased amounts of fluorescence, which suggests increased protein expression of SYP and CHGA/B, Figure 2C. Taken together, these observations strongly suggest that Dovitinib-induces NE trans-differentiation of PCa cells.
Figure 2.
Expression of proteins associated with NE differentiation A, LNCaP and PC3 cells were treated or not with 6 μM Dovitinib for 3 weeks, and their cell lysates subjected to western blot analysis using NSE antibody. MAPK was used as loading control and NCI-H660, a NEPC cell line, as positive control. B, Western blot analysis of the LNCaP lysate, treated as in B with Dovitinib, with AR antibody. Actin was used as loading control. C, Indirect immunofluorescence-based detection of chromogranin and synaptophsin in LNCaP (left) and PC3 (right) cells upon 6 μM Dovitinib treatment, using antibody against synaptophysin (top row) and chromogranin A + B (bottom row), and FITC-labeled secondary. DAPI was used to stain the nucleus (blue). Arrows point to neurites-like cellular extensions. Scale bar: 100 μM.
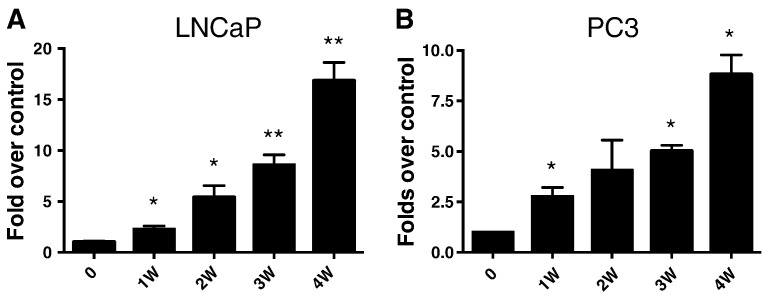
Time Course of NE Transformation with Dovitinib Treatment
Having established that PCa cells undergo NE trans-differentiation with Dovitinib treatment, we wondered how long was the treatment required for this transformation to manifest. Using both PC3 and LNCaP cells, we carried out a time-course of NE differentiation upon Dovitinib treatment. The cells were treated with Dovitinib and representative samples were harvested each week. At the end of 4 weeks, RNA was extracted and levels of NSE measured by qRT-PCR and compared to control cells. As depicted in Figure 3, expression of NSE was induced, as early as the second week of treatment, and continued through 4 weeks for both the cell lines. However, despite an increase in NSE expression in the 4-week treated samples when compared to 3-week treated samples, the cells began to look unhealthy and started to lift off the plates. Thus the time for complete transdifferentiation was taken to be around 3 weeks.
Figure 3.
Time course of NE-differentiation of prostate cancer cells treated with Dovitinib. LNCaP (Left) and PC3 (right) were treated or not with 6 μM Dovitinib in 6-well plates. Cells were harvested at each week time point and frozen. After the 4-week time point, qPCR was carried out and analyzed as in Figure 1.
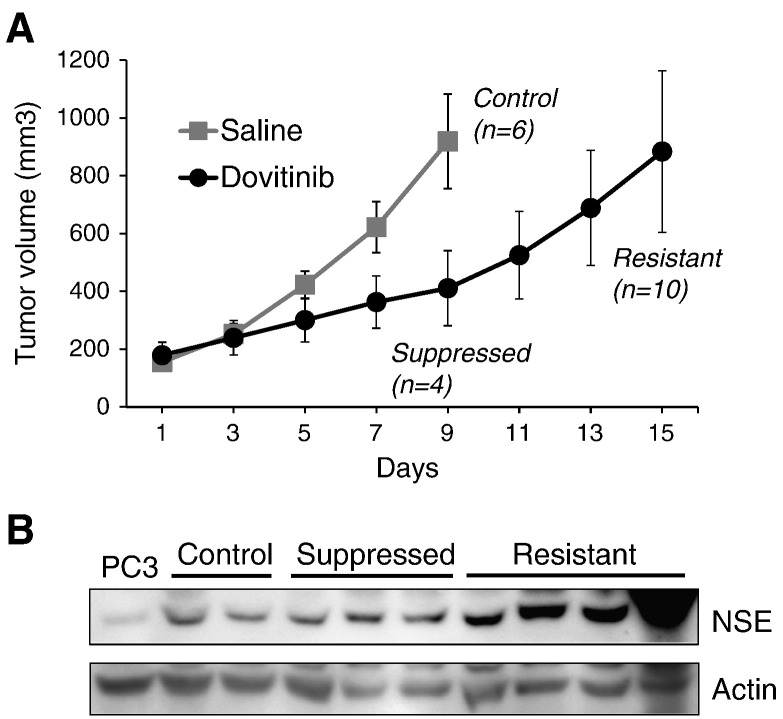
Dovitinib Induces NE Differentiation In Vivo
To test whether the NED-effect of Dovitinib extended to in vivo systems, we utilized the PC3 xenograft tumor model as it is an advanced model of CRPC and physiologically relevant in terms of therapy response leading to NEPC development. Nude mice were bilaterally injected with 1 million PC3 cells and tumors were allowed to form. When the tumors reached 200mm3 (around 2 weeks) mice were treated with 30 mg/kg Dovitinib daily and changes in tumor volume monitored. When compared to saline treated controls, which continued to grow rapidly and reached experimental end point (1000mm3), mice treated with Dovitinib had slower-growing tumors. However, after an initial lag-phase, these tumors appeared to rapidly increase their growth-rate past day-9 of treatment, reaching endpoint by Day 15, Figure 4A. To test whether tumors from Dovitinib-treated mice had increased level of neuronal markers, we carried out western blot analysis of lysates prepared from various stages of the tumorigenesis process. These included untreated saline control, suppressed (i.e. slow-growing phase) from the 1-week Dovitinib treatment and resistant phase from the 2-week Dovitinib treatment. When compared to PC3 cells, the levels of NSE were higher in all the tumor samples. Notably, there was a marked and progressive increase of NSE expression from control to suppressed and finally resistant tumors, Figure 4B. Taken together, the increased level of NSE expression suggests that the NED can be achieved with PC3 cells in vivo as observed in vitro.
Figure 4.
Induction of NE differentiation in PC3 xenografted tumors upon Dovitinib treatment. A, Nude mice were bilaterally injected with PC3 cells to induce xenograft tumor formation. When the tumors developed to around 200 mm3, mice were treated daily with 30 mg/kg Dovitinib or saline (control) through oral gavage. Changes in tumor volume were measured every day, and at around 1000 mm3, mice were sacrificed and tumors harvested. Mice were also sacrificed and tumors harvested at day 9. n = number of tumors and Error bars = S.E. B, Western blot analysis of representative samples collected at various points of tumorigenesis. Control (saline treated), suppressed (tumors from mice treated for 9 days), and resistant tumors were harvested, lysates prepared and the levels of the indicated proteins detected using neuron specific enolase, NSE antibody. Actin was used as loading control.
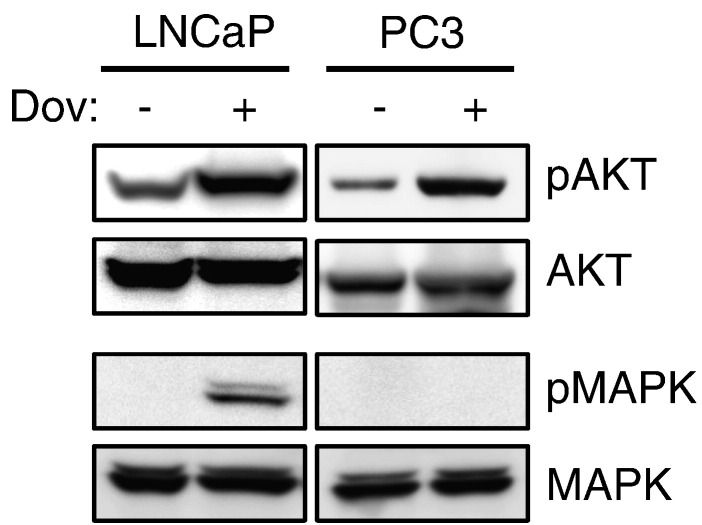
Mechanism of NE Differentiation: the Role of PI3K- and MAPK-Pathways
Previous studies have identified the PI3K-pathway to play a major role in driving prostate tumorigenesis, including NE differentiation [35], [36]. Furthermore, studies have also suggested the role of the MAPK-pathway in promoting NE differentiation [22], [37], [38]. To test whether up-regulation of the PI3K/AKT/mTOR pathway and/or MAPK-pathway played a role in the acquisition of Dovitinib-induced NED process, we probed cell lysates of Dovitinib-treated PCa cells with phospho-AKT and phospho-MAPK-specific antibodies. Both the cell lines showed increased levels of p-AKT upon Dovitinib-treatment, Figure 5, suggesting that perhaps up-regulation of the PI3K-pathway plays an important role in coordinating the differentiation process. However, when Dovitinib-treated cell lysates were tested for levels of MAPK-activation only, LNCaP cells showed a robust increase in phosphorylation of MAPK compared to controls, Figure 5. This increase in MAPK phosphorylation is consistent with a previous observation of NED of LNCaP cells in vitro [38]. It is quite conceivable that AR-positive and AR-negative cells undergo NED upon Dovitinib treatment via slightly different processes. In AR-negative cells, perhaps other factors such as Rac, Rho and cdc42, known to alter cell morphology and play a role in neuron survival, are involved [39]. Further experiments are needed to uncover the exact signaling-mechanisms driving the Dovitinib-mediated trans-differentiation process and the role of AR therein.
Figure 5.
Changes in PI3K and MAPK pathways upon Dovitinib treatment. LNCaP or PC3 cells were treated or not with 6 μM Dovitinib for 3 weeks and the cell lysates subjected to western blot analysis using phospho-AKT specific antibody to detect changes in PI3K pathway alterations. Total AKT was used as loading control (top rows). Phospho-MAPK specific antibody was used to probe for activation of MAPK pathway. Total MAPK was used as loading control (bottom rows). The same membrane was stripped after phospho-specific antibody probing and the membrane was re-probed using antibody targeting the total protein. Figure is representative of 3 independent experiments with similar results.
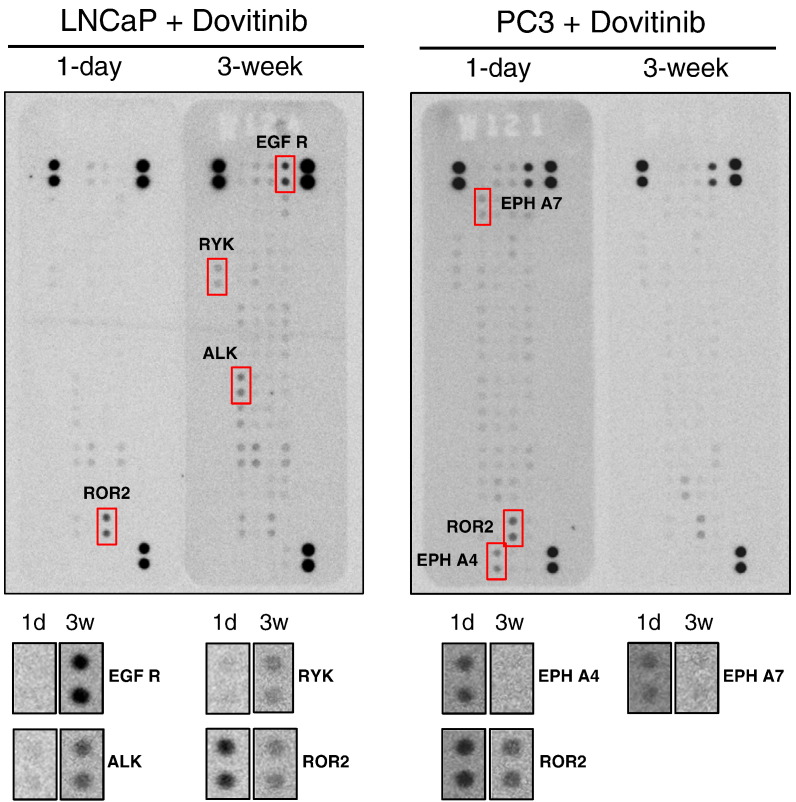
Role of Various RTKs in Dovitinib-Mediated Neuroendocrine Differentiation
Since both MAPK- and PI3K-pathway can be regulated through activated RTKs, we reasoned that perhaps the sustained treatment of the cells with the pan-RTK inhibitor Dovitinib induces a compensatory response from some of the 50 or so other RTKs, or perhaps even a re-activation or desensitization of the targeted receptors themselves. To address these possibilities we used a human RTK array that measures the amount of activated RTK in cell lysates. The lysates of 1 day (short term) and 3-week Dovitinib-treated cells, from both LNCaP and PC3, were compared to determine the differential regulation of RTK activation in the two conditions. Notably, in both the cell lines, 1-day treatment with Dovitinib displayed suppression in the phosphorylated form of its target RTKs (FGFR, VEGFR and PDGFR), Figure 6 and Supplementary Figure S3.
Figure 6.
Activation status of various RTKs during Dovitinib mediated NE differentiation of PCa cells. LNCaP (left) and PC3 (right) cells were treated with 6 μM Dovitinib for 1 day or 3 weeks, and the cell lysates subjected to analysis using the human Phospho-RTK array kit that only detects the activated or phosphorylated form of the receptor using a pan phospho-tyrosine antibody (see Methods for details). Each receptor is spotted in duplicate and 3 sets of positive controls added at three corners (top and bottom right) and 1 set of negative control on the bottom left corner (see Fig. S3 for more explanation and individual receptor locations). Epidermal growth factor receptor (EGFR), receptor-like tyrosine kinase (RYK), anaplastic lymphoma kinase (ALK), receptor tyrosine kinase like orphan receptor 2 (ROR2), Ephrin type-A receptor 4 (EPH A4), and Ephrin type-A receptor 7 (EPH A7) were identified to be differentially expressed and are shown in red-boxes below the strips.
Further analysis of the RTK strip treated with LNCaP lysates revealed a specific activation of EGFR in the 3-week Dovitinib treated cells when compared to 1-day treated cells, Figure 6 (left panel). EGFR has been shown to signal through various pathways including the MAPK-pathway [40], and EGF treatment has been demonstrated to promote neuroendocrine-like state in LNCaP cells [41]. Taken together, this adds support to role of the MAPK pathway seen previously (Figure 6) in the NED process.
Amongst other activated RTKs anaplastic lymphoma kinase (ALK) and receptor-like tyrosine kinase (RYK) were prominent. Whereas ALK is expressed specifically in the nervous system [42], RYK is part of the Wnt signaling pathway shown to influence axonal outgrowth [43], [44]. Furthermore, we also observed suppression of receptor tyrosine kinase-like orphan receptor 2 (ROR2) activation, which is also a part of the Wnt-signaling pathway, and its suppression has been shown to increase axon length [45], [46]. Thus, AKL, RYK and ROR2 perhaps act in concert to control neuron morphogenesis and regeneration [47], [48]. Taken together, the alterations in the above RTKs support the modulation of not only MAPK- and PI3K-pathways, but also the Wnt-signaling in driving the transdifferentiation of LNCaP cells upon Dovitinib treatment.
In the case of PC3 cells however, we observed a constitutively active EGFR in both the 1-day as well as the 3-week Dovitinib treated cells, which is consistent with previous reports of EGFR up-regulation in PC3 cells [49], [50]. Similar to LNCaP cells, we observed suppression of ROR2 activity upon prolonged Dovitinib treatment. Furthermore, we observed loss of Ephrin receptor activation, particularly Eph A4 (ephrin type-A receptor 4) and Eph A7 (ephrin type-A receptor 7) in the 3-week treated PC3 cells. Regulations through Ephrin receptors have been shown to guide axon elongation of neuronal cells [51], [52] and their suppression in certain contexts promotes tumorigenesis [53]. Remarkably, Eph A4 loss has been shown to promote axon regeneration [54], [55], Eph A7 suppression has been shown to help complex dendrite formations and axon elongation [56]. Taken together, they suggest the involvement of the Wnt signaling pathway and provide additional support to the differentiation of PCa cells to neuron-like cells with highly complex neurite-like processes.
Discussion and Conclusions
Treating prostate cancer remains a major challenge as around 33% of the treated patients eventually develop resistance to their drug regimen, and progress to metastatic CRPC for which there are limited treatment options [57]. Nevertheless, drug development efforts have produced more FDA-approved drugs in the last three years than in the previous 30 years [58]. However, resistance development to the newly approved therapies has impeded success [59]. Although the occurrence of de novo NEPC is rare, the development of resistance through NE differentiation, during ADT, docetaxel chemotherapy and radiation therapy, have been documented [14], [16], [59], [60], [61]. Further corroborating this, the analysis of tumors resistant to more potent AR-pathway targeted therapies (enzalutamide and abiraterone) suggests that around 39% of the resistant tumors display either pure or intermediate NEPC [62]. Thus, understanding the mechanism of resistance development through the NE trans-differentiation process is crucial towards determining alternative therapy regimens.
Therapeutically-targeting multiple receptor tyrosine kinases (RTKs) that play an important role in promoting tumor progression, such as angiogenesis and growth factor signaling, presents an attractive approach. Dovitinib (TKI-258/CHIR-258) fulfills this niche by inhibiting multiple RTKs such as FGFR, PDGFR, cKIT and FLT3, and is being evaluated in clinical trials for several cancers [27], [63].
We serendipitously observed that treatment of LNCaP cells with Dovitinib resulted in a uniform transformation of the cells to a distinct neuronal morphology. This alteration of was concomitant with expression of NE markers such as NSE, SYP and CHGA, loss of AR expression and suppression of REST.
It is challenging to address why the cancer cells differentiate into NE type during therapy and how this trans-differentiation benefits the cancer cells. Perhaps, through the acquisition of characteristics of both neuronal and endocrine cells, the cells gain the ability to withstand therapy and maintain survival signaling. Our in vitro experiments suggest that within 2 weeks of treatment, cells start to express high levels of NE marker NSE. Similarly, mice harboring PC3 xenografted tumors when treated systemically with Dovitinib showed high levels of NSE expression in the resistant tumors. The short-term nature of NED both in vitro and in vivo suggests that perhaps epigenetic regulation drives the differentiation process.
Previous studies have shown that PI3K and MAPK play a role in the differentiation process [35], [36]. Supporting these observations, Dovitinib-induced NE differentiation suggests the involvement of both PI3K and MAPK pathways. PC3 and LNCaP cells show up-regulation of PI3K signaling upon Dovitinib treatment and LNCaP cells show additional activation of MAPK. Further biochemical studies are needed to uncover the exact mechanistic links between AR and MAPK-pathway and their role in NED upon Dovitinib treatment.
Using human RTK arrays, we identified not only activation of receptors that are known to play a role in neuronal signaling, such as the various Ephrin receptors, but also those that are involved in driving MAPK- and PI3K-signaling, such as EGFR and Insulin R. We also identified RYK and ROR2, which have been shown to play a role in WNT-signaling in neuronal tissues, in line with previous reports that showed WNT signaling to promote NE differentiation of PCa cells [24], [64].
Our study for the first time demonstrates that Dovitinib-treated PCa cells develop NE phenotype, perhaps as a way of developing resistance. Analyzing the data of an ongoing clinical trial for Dovitinib in prostate cancer [27], not only in terms of survival benefit but also in terms of the number of patients developing treatment-induced NEPC, would be highly informative in making future treatment decisions. Finally, the study establishes a robust method to bring about rapid NED in vitro and could be a valuable tool to understand the biology and identify targets for therapeutic interventions.
Acknowledgements
We are thankful to the Department of Hematology and Oncology for use of their equipment and resources. We also would like to extend our thanks to the faculty of the Department of Urology for helpful discussions and suggestions. Thanks also to David Mulholland, PhD and Roseanne Wick for critical reading of the manuscript. KKY thanks Dr. Nora M Navone, MD Anderson Cancer Center for insightful discussions. The research work was supported by funds from Deane Prostate Health. Both SSY and KKY are Prostate Cancer Foundation Young Investigator Awardees.
Footnotes
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.tranon.2017.01.011.
Appendix A. Supplementary data
Fig. S1: Dovitinib IC50 curves of LNCaP (left) and PC3 (right). Both cell-lines were treated with increasing concentration of Dovitinib and viable cells left after 3-day treatment quantified using the WST method. Figures were generated using Prism 6, employing the 3-parameter dose-response curve fit. Error bars: SE.
Fig. S2: Induction of the neuronal morphology in Du145 and 22Rv1 cells upon prolonged treatment with Dovitinib. Representative images of Du145 and 22Rv1 cells treated with 6μM Dovitinib for 3 weeks (right) or not (left). Images were captured at 20x magnification using a bright-field microscope. Arrow heads point to neurite-like cellular outgrowth. Scale bar = 100μM.
Fig. S3: Status of various RTKs during NE differentiation. A. LNCaP and PC3 cells were treated with 6μM Dovitinib for 1 day or 3 weeks, and the cell lysates subjected to analysis using the human Phospho-RTK array kit (Same as Figure 6). The kit only detects the activated or phosphorylated form of the receptor (see Methods for details). Each receptor is spotted in duplicate and 3 sets of positive controls added at three corners (top and bottom right) and 1 set of negative control on the bottom left corner, all in duplicates. Ovals mark the control locations (red – positive; blue – negative). Location of various RTKs that are targeted by Dovitinib: Blue- FGFRs, Red- PDGFRs, and Green- VEGFRs. B. The placement of the various RTKs on the array. C. Guide to identify the exact location of the various receptors on the array using alphanumeric coordinates.
References
- 1.Miller KD, Siegel RL, Lin CC, Mariotto AB, Kramer JL, Rowland JH, Stein KD, Alteri R, Jemal A. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin. 2016;66(4):271–289. doi: 10.3322/caac.21349. [DOI] [PubMed] [Google Scholar]
- 2.Chen CD, Welsbie DS, Tran C, Baek SH, Chen R, Vessella R, Rosenfeld MG, Sawyers CL. Molecular determinants of resistance to antiandrogen therapy. Nat Med. 2004;10(1):33–39. doi: 10.1038/nm972. [DOI] [PubMed] [Google Scholar]
- 3.Tran C, Ouk S, Clegg NJ, Chen Y, Watson PA, Arora V, Wongvipat J, Smith-Jones PM, Yoo D, Kwon A. Development of a second-generation antiandrogen for treatment of advanced prostate cancer. Science. 2009;324(5928):787–790. doi: 10.1126/science.1168175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barrie SE, Potter GA, Goddard PM, Haynes BP, Dowsett M, Jarman M. Pharmacology of novel steroidal inhibitors of cytochrome P450(17) alpha (17 alpha-hydroxylase/C17-20 lyase) J Steroid Biochem Mol Biol. 1994 Sep;50(5–6):267–273. doi: 10.1016/0960-0760(94)90131-7. [DOI] [PubMed] [Google Scholar]
- 5.Scher HI, Beer TM, Higano CS, Anand A, Taplin M-E, Efstathiou E, Rathkopf D, Shelkey J, Yu EY, Alumkal J. Antitumour activity of MDV3100 in castration-resistant prostate cancer: a phase 1–2 study. Lancet. 2010 Apr;375(9724):1437–1446. doi: 10.1016/S0140-6736(10)60172-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Bono JS, Logothetis CJ, Molina A, Fizazi K, North S, Chu L, Chi KN, Jones RJ, Goodman OB, Saad F. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med. 2011;364(21):1995–2005. doi: 10.1056/NEJMoa1014618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scher HI, Fizazi K, Saad F, Taplin M-E, Sternberg CN, Miller K, de Wit R, Mulders P, Chi KN, Shore ND. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367(13):1187–1197. doi: 10.1056/NEJMoa1207506. [DOI] [PubMed] [Google Scholar]
- 8.Ryan CJ, Smith MR, de Bono JS, Molina A, Logothetis CJ, de Souza P, Fizazi K, Mainwaring P, Piulats JM, Ng S. Abiraterone in metastatic prostate cancer without previous chemotherapy. N Engl J Med. 2013;368(2):138–148. doi: 10.1056/NEJMoa1209096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aparicio A, Logothetis CJ, Maity SN. Understanding the lethal variant of prostate cancer: power of examining extremes. Cancer Discov. 2011;1(6):466–468. doi: 10.1158/2159-8290.CD-11-0259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nadal R, Schweizer M, Kryvenko ON, Epstein JI, Eisenberger MA. Small cell carcinoma of the prostate. Nat Rev Urol. 2014;11(4):213–219. doi: 10.1038/nrurol.2014.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.di Sant’Agnese PA, Cockett ATK. Neuroendocrine differentiation in prostatic malignancy. Cancer. 1996;78(2):357–361. doi: 10.1002/(SICI)1097-0142(19960715)78:2<357::AID-CNCR27>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 12.Parimi V, Goyal R, Poropatich K, Yang XJ. Neuroendocrine differentiation of prostate cancer: a review. Am J Clin Exp Urol. 2014;2(4):273–285. [PMC free article] [PubMed] [Google Scholar]
- 13.Abrahamsson PA. Neuroendocrine cells in tumour growth of the prostate. Endocr Relat Cancer. 1999;6(4):503–519. doi: 10.1677/erc.0.0060503. [DOI] [PubMed] [Google Scholar]
- 14.Terry S, Maillé P, Baaddi H, Kheuang L, Soyeux P, Nicolaiew N, Ceraline J, Firlej V, Beltran H, Allory Y. Cross modulation between the androgen receptor axis and protocadherin-PC in mediating neuroendocrine transdifferentiation and therapeutic resistance of prostate cancer. Neoplasia N Y N. 2013 Jul;15(7):761–772. doi: 10.1593/neo.122070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shen R, Dorai T, Szaboles M, Katz AE, Olsson CA, Buttyan R. Transdifferentiation of cultured human prostate cancer cells to a neuroendocrine cell phenotype in a hormone-depleted medium. Urol Oncol Semin Orig Investig. 1997 Mar;3(2):67–75. doi: 10.1016/s1078-1439(97)00039-2. [DOI] [PubMed] [Google Scholar]
- 16.Deng X, Liu H, Huang J, Cheng L, Keller ET, Parsons SJ, Hu C-D. Ionizing radiation induces prostate cancer neuroendocrine differentiation through Interplay of CREB and ATF2: implications for disease progression. Cancer Res. 2008;68(23):9663–9670. doi: 10.1158/0008-5472.CAN-08-2229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bang YJ, Pirnia F, Fang WG, Kang WK, Sartor O, Whitesell L, Ha MJ, Tsokos M, Sheahan MD, Nguyen P. Terminal neuroendocrine differentiation of human prostate carcinoma cells in response to increased intracellular cyclic AMP. Proc Natl Acad Sci U S A. 1994;91(12):5330–5334. doi: 10.1073/pnas.91.12.5330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mori S, Murakami-Mori K, Bonavida B. Interleukin-6 induces G1 arrest through induction of p27Kip1, a cyclin-dependent kinase inhibitor, and neuron-like morphology in LNCaP prostate tumor cells. Biochem Biophys Res Commun. 1999;257(2):609–614. doi: 10.1006/bbrc.1999.0515. [DOI] [PubMed] [Google Scholar]
- 19.Delk NA, Farach-Carson MC. Interleukin-6: a bone marrow stromal cell paracrine signal that induces neuroendocrine differentiation and modulates autophagy in bone metastatic PCa cells. Autophagy. 2012;8(4):650–663. doi: 10.4161/auto.19226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burchardt T, Burchardt M, Chen MW, Cao Y, de la Taille A, Shabsigh A, Hayek O, Dorai T, Buttyan R. Transdifferentiation of prostate cancer cells to a neuroendocrine cell phenotype in vitro and in vivo. J Urol. 1999;162(5):1800–1805. [PubMed] [Google Scholar]
- 21.Spiotto MT, Chung TDK. STAT3 mediates IL-6-induced growth inhibition in the human prostate cancer cell line LNCaP. Prostate. 2000;42(2):88–98. doi: 10.1002/(sici)1097-0045(20000201)42:2<88::aid-pros2>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 22.Gutiérrez-Cañas I, Juarranz MG, Collado B, Rodríguez-Henche N, Chiloeches A, Prieto JC, Carmena MJ. Vasoactive intestinal peptide induces neuroendocrine differentiation in the LNCaP prostate cancer cell line through PKA, ERK, and PI3K. Prostate. 2005;63(1):44–55. doi: 10.1002/pros.20173. [DOI] [PubMed] [Google Scholar]
- 23.Kim J, Adam RM, Freeman MR. Activation of the Erk mitogen-activated protein kinase pathway stimulates neuroendocrine differentiation in LNCaP cells independently of cell cycle withdrawal and STAT3 phosphorylation. Cancer Res. 2002;62(5):1549–1554. [PubMed] [Google Scholar]
- 24.Yang X, Chen M-W, Terry S, Vacherot F, Chopin DK, Bemis DL, Kitajewski J, Benson MC, Guo Y, Buttyan R. A human- and male-specific protocadherin that acts through the wnt signaling pathway to induce neuroendocrine transdifferentiation of prostate cancer cells. Cancer Res. 2005;65(12):5263–5271. doi: 10.1158/0008-5472.CAN-05-0162. [DOI] [PubMed] [Google Scholar]
- 25.Trudel S, Li ZH, Wei E, Wiesmann M, Chang H, Chen C, Reece D, Heise C, Stewart AK. CHIR-258, a novel, multitargeted tyrosine kinase inhibitor for the potential treatment of t(4;14) multiple myeloma. Blood. 2005;105(7):2941–2948. doi: 10.1182/blood-2004-10-3913. [DOI] [PubMed] [Google Scholar]
- 26.Wan X, Corn PG, Yang J, Palanisamy N, Starbuck MW, Efstathiou E, Tapia EML-N, Zurita AJ, Aparicio A, Ravoori MK. Prostate cancer cell-stromal cell crosstalk via FGFR1 mediates antitumor activity of dovitinib in bone metastases. Sci Transl Med. 2014;6(252):252ra122. doi: 10.1126/scitranslmed.3009332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dovitinib (TKI258) and abiraterone acetate in metastatic castrate-resistant prostate cancer (mCRPC) - Full Text View - ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT01994590 [Internet]. [cited 2015 Jul 1]. Available from:
- 28.Qiu Y, Robinson D, Pretlow TG, Kung HJ. Etk/Bmx, a tyrosine kinase with a pleckstrin-homology domain, is an effector of phosphatidylinositol 3’-kinase and is involved in interleukin 6-induced neuroendocrine differentiation of prostate cancer cells. Proc Natl Acad Sci U S A. 1998;95(7):3644–3649. doi: 10.1073/pnas.95.7.3644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tai S, Sun Y, Squires JM, Zhang H, Oh WK, Liang C-Z, Huang J. PC3 is a cell line characteristic of prostatic small cell carcinoma. Prostate. 2011;71(15):1668–1679. doi: 10.1002/pros.21383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yuan T-C, Veeramani S, Lin M-F. Neuroendocrine-like prostate cancer cells: neuroendocrine transdifferentiation of prostate adenocarcinoma cells. Endocr Relat Cancer. 2007;14(3):531–547. doi: 10.1677/ERC-07-0061. [DOI] [PubMed] [Google Scholar]
- 31.Terry S, Beltran H. The many faces of neuroendocrine differentiation in prostate cancer progression. Front Oncol. 2014;4 doi: 10.3389/fonc.2014.00060. [cited 2015 Jul 1];Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3971158/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang X, Coleman IM, Brown LG, True LD, Kollath L, Lucas JM, Lam H-M, Dumpit R, Corey E, Chéry L. SRRM4 Expression and the loss of REST activity may promote the emergence of the neuroendocrine phenotype in castration-resistant prostate cancer. Clin Cancer Res. 2015;21(20):4698–4708. doi: 10.1158/1078-0432.CCR-15-0157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhu Y, Liu C, Cui Y, Nadiminty N, Lou W, Gao AC. Interleukin-6 induces neuroendocrine differentiation (NED) through suppression of RE-1 silencing transcription factor (REST) Prostate. 2014 Aug;74(11):1086–1094. doi: 10.1002/pros.22819. [DOI] [PubMed] [Google Scholar]
- 34.Svensson C, Ceder J, Iglesias-Gato D, Chuan Y-C, Pang ST, Bjartell A, Martinez RM, Bott L, Helczynski L, Ulmert D. REST mediates androgen receptor actions on gene repression and predicts early recurrence of prostate cancer. Nucleic Acids Res. 2014;42(2):999–1015. doi: 10.1093/nar/gkt921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xie S, Lin H-K, Ni J, Yang L, Wang L, di Sant’Agnese PA, Chang C. Regulation of interleukin-6-mediated PI3K activation and neuroendocrine differentiation by androgen signaling in prostate cancer LNCaP cells. Prostate. 2004;60(1):61–67. doi: 10.1002/pros.20048. [DOI] [PubMed] [Google Scholar]
- 36.Shen MM, Abate-Shen C. Molecular genetics of prostate cancer: new prospects for old challenges. Genes Dev. 2010;24(18):1967–2000. doi: 10.1101/gad.1965810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Martín-Orozco RM, Almaraz-Pro C, Rodríguez-Ubreva FJ, Cortés MA, Ropero S, Colomer R, López-Ruiz P, Colás B. EGF prevents the neuroendocrine differentiation of LNCaP cells induced by serum deprivation: the modulator role of PI3K/Akt. Neoplasia N Y N. 2007;9(8):614–624. doi: 10.1593/neo.07337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pinski J, Wang Q, Quek ML, Cole A, Cooc J, Danenberg K, Danenberg PV. Genistein-induced neuroendocrine differentiation of prostate cancer cells. Prostate. 2006;66(11):1136–1143. doi: 10.1002/pros.20440. [DOI] [PubMed] [Google Scholar]
- 39.Stankiewicz TR, Linseman DA. Rho family GTPases: key players in neuronal development, neuronal survival, and neurodegeneration. Front Cell Neurosci. 2014;8:314. doi: 10.3389/fncel.2014.00314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Scaltriti M, Baselga J. The epidermal growth factor receptor pathway: a model for targeted therapy. Clin Cancer Res. 2006;12(18):5268–5272. doi: 10.1158/1078-0432.CCR-05-1554. [DOI] [PubMed] [Google Scholar]
- 41.Cortés MA, Cariaga-Martinez AE, Lobo MVT, Orozco RMM, Motiño O, Rodríguez-Ubreva FJ, Angulo J, López-Ruiz P, Colás B. EGF promotes neuroendocrine-like differentiation of prostate cancer cells in the presence of LY294002 through increased ErbB2 expression independent of the phosphatidylinositol 3-kinase-AKT pathway. Carcinogenesis. 2012;33(6):1169–1177. doi: 10.1093/carcin/bgs139. [DOI] [PubMed] [Google Scholar]
- 42.Iwahara T, Fujimoto J, Wen D, Cupples R, Bucay N, Arakawa T, Mori S, Ratzkin B, Yamamoto T. Molecular characterization of ALK, a receptor tyrosine kinase expressed specifically in the nervous system. Oncogene. 1997;14(4):439–449. doi: 10.1038/sj.onc.1200849. [DOI] [PubMed] [Google Scholar]
- 43.Clark CEJ, Nourse CC, Cooper HM. The tangled web of non-canonical Wnt signalling in neural migration. Neurosignals. 2012;20(3):202–220. doi: 10.1159/000332153. [DOI] [PubMed] [Google Scholar]
- 44.Blakely BD, Bye CR, Fernando CV, Prasad AA, Pasterkamp RJ, Macheda ML, Stacker SA, Parish CL. Ryk, a receptor regulating Wnt5a-mediated neurogenesis and axon morphogenesis of ventral midbrain dopaminergic neurons. Stem Cells Dev. 2013;22(15):2132–2144. doi: 10.1089/scd.2013.0066. [DOI] [PubMed] [Google Scholar]
- 45.Paganoni S, Ferreira A. Neurite extension in central neurons: a novel role for the receptor tyrosine kinases Ror1 and Ror2. J Cell Sci. 2005;118(Pt 2):433–446. doi: 10.1242/jcs.01622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Oishi I, Suzuki H, Onishi N, Takada R, Kani S, Ohkawara B, Koshida I, Suzuki K, Yamada G, Schwabe GC. The receptor tyrosine kinase Ror2 is involved in non-canonical Wnt5a/JNK signalling pathway. Genes Cells. 2003;8(7):645–654. doi: 10.1046/j.1365-2443.2003.00662.x. [DOI] [PubMed] [Google Scholar]
- 47.Ho H-YH, Susman MW, Bikoff JB, Ryu YK, Jonas AM, Hu L, Kuruvilla R, Greenberg ME. Wnt5a-Ror-Dishevelled signaling constitutes a core developmental pathway that controls tissue morphogenesis. Proc Natl Acad Sci U S A. 2012;109(11):4044–4051. doi: 10.1073/pnas.1200421109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hollis ER, Zou Y. Expression of the Wnt signaling system in central nervous system axon guidance and regeneration. Front Mol Neurosci. 2012;5:5. doi: 10.3389/fnmol.2012.00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sheikh SSE, Domin J, Abel P, Stamp G, Lalani E-N. Phosphorylation of both EGFR and ErbB2 is a reliable predictor of prostate cancer cell proliferation in response to EGF. Neoplasia. 2004;6(6):846–853. doi: 10.1593/neo.04379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sherwood ER, Van Dongen JL, Wood CG, Liao S, Kozlowski JM, Lee C. Epidermal growth factor receptor activation in androgen-independent but not androgen-stimulated growth of human prostatic carcinoma cells. Br J Cancer. 1998;77(6):855–861. doi: 10.1038/bjc.1998.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Egea J, Klein R. Bidirectional Eph-ephrin signaling during axon guidance. Trends Cell Biol. 2007;17(5):230–238. doi: 10.1016/j.tcb.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 52.O’Leary DD, Wilkinson DG. Eph receptors and ephrins in neural development. Curr Opin Neurobiol. 1999;9(1):65–73. doi: 10.1016/s0959-4388(99)80008-7. [DOI] [PubMed] [Google Scholar]
- 53.Pasquale EB. Eph receptors and ephrins in cancer: bidirectional signalling and beyond. Nat Rev Cancer. 2010;10(3):165–180. doi: 10.1038/nrc2806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gatto G, Morales D, Kania A, Klein R. EphA4 receptor shedding regulates spinal motor axon guidance. Curr Biol. 2014;24(20):2355–2365. doi: 10.1016/j.cub.2014.08.028. [DOI] [PubMed] [Google Scholar]
- 55.Joly S, Jordi N, Schwab ME, Pernet V. The Ephrin receptor EphA4 restricts axonal sprouting and enhances branching in the injured mouse optic nerve. Eur J Neurosci. 2014;40(7):3021–3031. doi: 10.1111/ejn.12677. [DOI] [PubMed] [Google Scholar]
- 56.Clifford MA, Athar W, Leonard CE, Russo A, Sampognaro PJ, Van der Goes M-S, Burton DA, Zhao X, Lalchandani RR, Sahin M. EphA7 signaling guides cortical dendritic development and spine maturation. Proc Natl Acad Sci U S A. 2014;111(13):4994–4999. doi: 10.1073/pnas.1323793111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yap TA, Swanton C, de Bono JS. Personalization of prostate cancer prevention and therapy: are clinically qualified biomarkers in the horizon? EPMA J. 2012;3(1):3. doi: 10.1007/s13167-011-0138-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Galsky MD, Small AC, Tsao C, Oh WK. Clinical development of novel therapeutics for castration-resistant prostate cancer: historic challenges and recent successes. CA Cancer J Clin. 2012;62(5):299–308. doi: 10.3322/caac.21141. [DOI] [PubMed] [Google Scholar]
- 59.Seruga B, Ocana A, Tannock IF. Drug resistance in metastatic castration-resistant prostate cancer. Nat Rev Clin Oncol. 2011;8(1):12–23. doi: 10.1038/nrclinonc.2010.136. [DOI] [PubMed] [Google Scholar]
- 60.Humphrey PA. Histological variants of prostatic carcinoma and their significance. Histopathology. 2012;60(1):59–74. doi: 10.1111/j.1365-2559.2011.04039.x. [DOI] [PubMed] [Google Scholar]
- 61.Jiborn T, Bjartell A, Abrahamsson P-A. Neuroendocrine differentiation in prostatic carcinoma during hormonal treatment. Urology. 1998;51(4):585–589. doi: 10.1016/s0090-4295(97)00684-5. [DOI] [PubMed] [Google Scholar]
- 62.Small EJ, Huang J, Youngren J, Sokolov A, Aggarwal RR, Thomas G, True LD, Zhang L, Foye A, Alumkal JJ. 33(Suppl. 15) 2015. Characterization of neuroendocrine prostate cancer (NEPC) in patients with metastatic castration resistant prostate cancer (mCRPC) resistant to abiraterone (Abi) or enzalutamide (Enz): Preliminary results from the SU2C/PCF/AACR West Coast Prostate Cancer Dream Team (WCDT) p. 5003. (ASCO Meet Abstr). [Google Scholar]
- 63.Porta C, Giglione P, Liguigli W, Paglino C. Dovitinib (CHIR258, TKI258): structure, development and preclinical and clinical activity. Future Oncol. 2015;11(1):39–50. doi: 10.2217/fon.14.208. [DOI] [PubMed] [Google Scholar]
- 64.Uysal-Onganer P, Kawano Y, Caro M, Walker MM, Diez S, Darrington RS, Waxman J, Kypta RM. Wnt-11 promotes neuroendocrine-like differentiation, survival and migration of prostate cancer cells. Mol Cancer. 2010;9:55. doi: 10.1186/1476-4598-9-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig. S1: Dovitinib IC50 curves of LNCaP (left) and PC3 (right). Both cell-lines were treated with increasing concentration of Dovitinib and viable cells left after 3-day treatment quantified using the WST method. Figures were generated using Prism 6, employing the 3-parameter dose-response curve fit. Error bars: SE.
Fig. S2: Induction of the neuronal morphology in Du145 and 22Rv1 cells upon prolonged treatment with Dovitinib. Representative images of Du145 and 22Rv1 cells treated with 6μM Dovitinib for 3 weeks (right) or not (left). Images were captured at 20x magnification using a bright-field microscope. Arrow heads point to neurite-like cellular outgrowth. Scale bar = 100μM.
Fig. S3: Status of various RTKs during NE differentiation. A. LNCaP and PC3 cells were treated with 6μM Dovitinib for 1 day or 3 weeks, and the cell lysates subjected to analysis using the human Phospho-RTK array kit (Same as Figure 6). The kit only detects the activated or phosphorylated form of the receptor (see Methods for details). Each receptor is spotted in duplicate and 3 sets of positive controls added at three corners (top and bottom right) and 1 set of negative control on the bottom left corner, all in duplicates. Ovals mark the control locations (red – positive; blue – negative). Location of various RTKs that are targeted by Dovitinib: Blue- FGFRs, Red- PDGFRs, and Green- VEGFRs. B. The placement of the various RTKs on the array. C. Guide to identify the exact location of the various receptors on the array using alphanumeric coordinates.