Abstract
Background: Attrition in pediatric weight management negatively impacts treatment outcomes. A potentially modifiable contributor to attrition is unmet family expectations. This study aimed to evaluate the association between adolescent and parent/guardian treatment expectations and attrition.
Patients and Methods: A prospective, nonrandomized, uncontrolled, single-arm pilot trial was conducted among 12 pediatric weight management programs in the Children's Hospital Association's FOCUS on a Fitter Future collaborative. Parents/guardians and adolescents completed an expectations/goals survey at their initial visit, with categories including healthier food/drinks, physical activity/exercise, family support/behavior, and weight management goals. Attrition was assessed at 3 months.
Results: From January to August 2013, 405 parents/guardians were recruited and reported about their children (203 adolescents, 202 children <12 years). Of the 203 adolescents, 160 also self-reported. Attrition rate was 42.2% at 3 months. For adolescents, greater interest in family support/behavior skills was associated with decreased odds of attrition at 3 months [odds ratio (OR) 0.75, 95% confidence interval (CI) 0.57–0.98, p = 0.04]. The more discordant the parent/adolescent dyad responses in this category, the higher the odds of attrition at 3 months (OR 1.36, 95% CI 1.04–1.78, p = 0.02). Weight loss was an important weight management goal for both adolescents and parents. For adolescents with this goal, the median weight-loss goal was 50 pounds. Attrition was associated with adolescent weight-loss goals above the desired median (50% above the median vs. 28% below the median, p = 0.02).
Conclusions: Assessing initial expectations may help tailor treatment to meet families' needs, especially through focus on family-based change and realistic goal setting.
Clinical Trial Registration: Clinicaltrials.gov NCT01753063.
Keywords: : attrition, family-based health, obesity, pediatrics, weight management
Introduction
Obesity currently affects 17% of youth in the United States.1 With medical complications such as type 2 diabetes, elevated cholesterol, and hypertension, treatment of childhood obesity is critical. However, attrition rates from weight management programs ranging from 27% to 73% have been reported,2,3 impacting the effectiveness of available treatments. Although not consistent in the literature, patient characteristics reported to be associated with a higher rate of attrition include higher BMI, depression/low self-esteem, behavioral issues, high parental BMI, older age, and African American race.2–8 Logistical and experiential reasons for attrition, such as dissatisfaction with program staff and/or treatment focus and lack of insurance coverage, have also been reported.2,3,7,8
In 2008, the Children's Hospital Association convened a workgroup on childhood obesity treatment (FOCUS on a Fitter Future). After identifying attrition as a major barrier to program success,4 the second FOCUS on a Fitter Future workgroup (2010–2011) developed a telephone survey to better understand parental reasons for attrition. Parents of patients in 13 pediatric weight management programs were surveyed, and the survey identified family expectations that were mismatched with program goals as a factor contributing to patient attrition.5 Families explained that if logistics or program components had been adapted to their needs, they might have continued in treatment.6 When asked what components of a program they felt would be most helpful in their weight management efforts, the majority endorsed components often already provided in tertiary care pediatric weight management programs. This suggested that treatment delivery may need to be more individualized6 and that families may benefit from a review of their expectations in conjunction with program offerings at the beginning of treatment.
Few studies of patient expectations at treatment initiation for the management of pediatric chronic conditions have been described.9–11 One study, for example, reported assessment of adolescent and family expectations during an initial visit for the treatment of chronic pain, demonstrating only slight to modest agreement between parent and adolescent in 50% of the treatment-specific expectations explored. Results from this study support the importance of aligning treatment focus between the parent and adolescent during the initial pain management visit.9 Qualitative interviews with families initiating pediatric weight management found that caregivers' reasons for seeking treatment for their children were not always aligned with their perceptions of programmatic success10 and that modifiable factors, including individualizing services, were recommendations for improvement of care delivery.11 At the outset of our study, to our knowledge, no survey tools that explicitly aimed to evaluate pediatric obesity-specific treatment expectations had been evaluated and reported in the literature, although tools addressing related concepts, such as lifestyle behaviors, perceived barriers, and readiness to change, had been explored.12,13
Therefore, the third FOCUS on a Fitter Future workgroup developed and then piloted a treatment expectations and goals survey tool to be completed by parents/guardians (hereinafter referred to as parents) and adolescent patients at initial presentation for weight management. The intervention was the review of responses with clinic/program staff to inform clinical management. The tool was designed to reflect the range of patient/family preferences, and the provider could put this in the context of a clinic/program's offerings. The aims of the study were to evaluate (1) the relationship between treatment expectations at baseline and attrition over 3 months, (2) the relationship between the concordance of adolescent/parent treatment expectations and attrition over 3 months, and (3) the relationship between achievement of treatment expectations and attrition over 3 months.
Patients and Methods
This was a prospective, nonrandomized, uncontrolled, single-arm pilot trial. Participants were recruited between January 2013 and August 2013 from 12 institutions with multidisciplinary pediatric weight management programs participating in the FOCUS on a Fitter Future obesity collaborative. The institutional review boards (IRBs) of 10 participating institutions reviewed and either approved or considered this project exempt. The remaining two institutions' IRBs granted them reciprocity to follow approved protocols of two other study institutions.
Participants
Children eligible for the study were between 2 and 18 years of age and newly referred to a participating weight management clinic or program. The parent and child were required to be conversant in English or Spanish. Adolescents (children aged 12 years and older) within the recruited sample were also invited to participate unless their parent reported cognitive issues preventing completion of a survey, as might be suggested by the presence of an in-school aide >50% of the school day or participation in special education classes >50% of the school day. If more than one parent was present, it was left to the discretion of the family to choose which parent would participate.
Survey Tools and Intervention
The treatment expectations and goals survey tool was completed by the parents and participating adolescents, and the intervention was an individualized review of the responses with clinic/program staff at the initial visit to guide clinical care. A follow-up survey to assess achievement of treatment expectations, which could be completed independently of a clinical visit, was completed at 3 months.
Survey tools
Two survey versions were created for both baseline and follow-up: one for parents and the other for adolescents. A subgroup of investigators from the FOCUS on a Fitter Future workgroup led the development of the survey tool guided by the frameworks of social cognitive14 and family systems15 theories. Specifically, items were based on acquiring knowledge, behavioral skills, and the role of familial support.14,15 The investigators solicited and reviewed existing tools from member institutions that were used at initial weight management program evaluations to assess patient/parent desires for support, barriers, readiness for change, and goals. Based on this input and the quantitative and qualitative input from families obtained in the prior study,5,6 they compiled a list of the areas of support most frequently sought by families. This list was used to draft the survey tool, which was then refined with input from the broader workgroup to ensure content validity. The content of the parent and adolescent surveys was the same, but the introductory language differed, in that adolescents were addressed directly. Surveys were written at the fourth-grade level. All survey documents were translated into Spanish by certified staff from The Children's Hospital Colorado.
Each survey covered four main categories based on domains outlined by the American Academy of Pediatrics as critical for ensuring effective intervention for pediatric weight management16,17: healthier food/drinks, physical activity/exercise, family support/behavior, and weight management goals (refer to Supplementary Data for full survey; Supplementary Data are available at www.liebertpub.com/chi). Within the first three categories, topics were subcategorized into knowledge needs (e.g., “We want to know more about finding activities my child likes to do.”) and skill needs (e.g., “We want to know how to eat less junk food.”) based on a typical survey design framework of knowledge, attitudes, and practice.18 Participants were asked to rate the importance of each topic on the same five-point Likert scale from “Not at all” to “Very much” and circle the topic in each subcategory most important to them. Cronbach's alpha ≥0.8 for all seven subcategories supported the reliability and internal consistency of the survey tool for both parents (alphas 0.80–0.96) and adolescents (alphas 0.80–0.92).
For the follow-up survey, the title changed from “What Do You Want from the (clinic/program name)?” to “What Did You Learn from the (clinic/program name)?” Participants rated their learning (or progress in the case of goals) related to each topic on the same five-point Likert scale from “Not at all” to “Very much.” Participants indicated which topic helped their family the most or which change was the most important in the case of weight management goals.
Intervention
The intervention consisted of the clinic/program staff discussing participants' survey tool responses with them as part of the initial visit to guide management. A study guide was developed that outlined the basic steps for using the survey tool. However, specific strategies for survey tool use and the team members involved were individualized at each site. Expectations were conceptualized as what the parent and adolescent identified as their desired learning needs or goals.
Data Collection
Participants completed the initial survey on paper before, or during, their initial clinic/program visit. The follow-up survey was administered at 3 months (+/−2 weeks) in person on paper whenever possible. If patients did not attend follow-up appointments, sites either mailed a letter and follow-up survey to families or conducted a telephone survey using a standard script. Demographic data, including age, sex, race, ethnicity, insurance status, weight, and height at baseline, were collected from the electronic medical record. BMI percentile and BMI z-score were calculated according to CDC reference standards.19
Study data were managed using Research Electronic Data Capture (REDCap) electronic data capture tools hosted at Boston Children's Hospital.20 REDCap is a secure web-based application designed to support data capture for research studies.
Outcomes
Similar to the approach in our prior study,5 attrition or dropout was defined according to whether a patient was seen in a program or a clinic. A program was considered treatment with a defined endpoint (e.g., 12 weeks), and in such cases, dropout referred to participation in less than 25% of the required visits in the 3-month study period. A clinic was considered treatment without a defined endpoint, in which case dropout was no follow-up visit in the first 3 months after the initial baseline visit.
Predictors
Treatment expectations were summarized by first assigning the five-point (0–4), Likert scale responses with a score of 0 for “Not at all” to 4 for “Very much” and then averaging responses to the questions within each category: (1) healthier food/drink knowledge, (2) healthier food/drink skills, (3) physical activity knowledge, (4) physical activity skills, (5) family support/behavior knowledge, (6) family support/behavior skills, and (7) weight management goals. The category scores were averages of all nonmissing items from the category. If selected, the “Other” items were included in the averages. Categories were summarized separately for adolescents and parents.
Concordance of parent/adolescent expectations was calculated as the difference between parent and adolescent dyad survey responses in each category.
We also evaluated weight loss as a goal in the weight management goals category. We categorized parents and adolescents as above or below the desired median weight-loss goal for their group.
Analyses
Descriptive data are reported as mean (SD) or proportion, as appropriate. Pearson's chi-squared test was used for bivariate analyses with categorical variables. Wilcoxon rank sum test was used to explore the relationship between individual survey item responses and attrition status. Logistic regression was used to assess the relationship between baseline characteristics, including treatment expectations and concordance of parent/adolescent expectations, and attrition at 3 months. We used a parsimonious approach to modeling with planned adjustment only for predictors significant in bivariate analyses. Because there was very little between-site variation in attrition (intraclass correlations = 0.02), adjustment for site was not included in the statistical models. There were three sibling pairs in the study, but each child had a parent survey and was treated independently. Two participants were missing attrition status and were excluded from analyses. Eight parent surveys and two adolescent surveys completed at baseline had insufficient data for analysis and were excluded.
Data from the follow-up surveys are not presented due to missing data, and therefore the third study aim could not be addressed. A significance level of p < 0.05 was used in all analyses. Analyses were performed using STATA (StataCorp. 2013. Stata Statistical Software: Release 13; StataCorp LP, College Station, TX).
Results
Participants
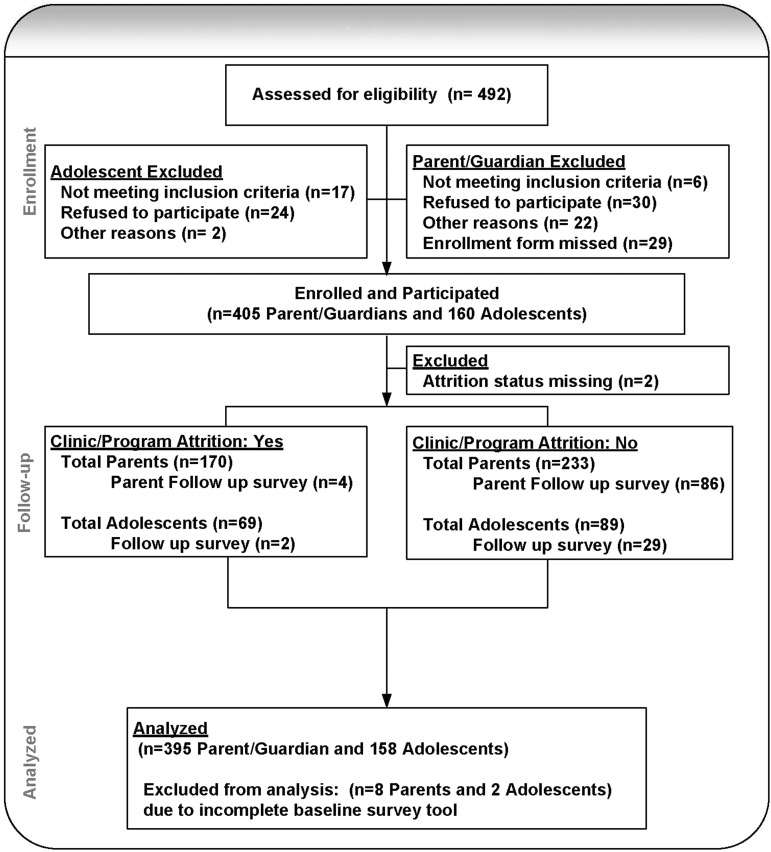
From January to August 2013, 405 parents (range 1 to 103 per site) were recruited and reported about their children (203 adolescents and 202 children <12 years) as outlined in Figure 1. Of the 203 adolescents, 160 also participated and self-reported (17 excluded, 24 declined, 2 enrolled, but did not submit surveys). Characteristics of patients are shown in Table 1. An additional 87 families were ineligible, missed, or declined to participate and did not differ from enrolled patients in age, sex, or baseline BMI z-score (data not shown).
Figure 1.
Study enrollment and retention.
Table 1.
Characteristics of Enrolled Families (N = 405)
| Mean (SD) or n (%) | |
|---|---|
| Age, years | 11.7 (3.6) |
| Body mass index percentile | 98.6 (3.1) |
| Body mass index z-score | 2.43 (0.47) |
| Female sex | 246 (60.7) |
| Race/ethnicitya | |
| Hispanic, any race | 63 (15.6) |
| White, non-Hispanic | 185 (45.7) |
| Black, non-Hispanic | 92 (22.7) |
| Asian, non-Hispanic | 4 (1.0) |
| Other/multiple race, non-Hispanic | 16 (4.0) |
| Missing race, non-Hispanic | 45 (11.1) |
| Insurance | |
| Public | 238 (58.8) |
| Private | 161 (39.8) |
| Uninsured | 2 (0.5) |
| Not sure/missing | 4 (1.0) |
Non-Hispanic categories also include those with missing ethnicity. There were 58 (14.3%) missing ethnicity and 51 (12.6%) missing race.
Attrition and Treatment Expectations
The overall attrition rate was 42.2% (170/403). Table 2 shows treatment expectations at baseline in each category. Among dyads, parent expectations were significantly higher in all categories except healthier food/drink skills and family support/behavior skills.
Table 2.
Parent/Adolescent Treatment Expectations at Baseline
| Parent | Adolescent | Parent–adolescent difference | |
|---|---|---|---|
| Categorya | Mean (SD) (n = 395) | Mean (SD) (n = 158) | Mean (SD) (n = 156)b |
| Healthier food/drink knowledge | 2.6 (1.0) | 2.2 (1.1) | 0.3 (1.1)c |
| Healthier food/drink skills | 2.6 (1.1) | 2.4 (1.1) | 0.1 (1.1) |
| Physical activity knowledge | 3.1 (1.2) | 2.7 (1.4) | 0.4 (1.2)c |
| Physical activity skills | 2.1 (1.1) | 1.6 (1.0) | 0.3 (1.2)c |
| Family support/behavior knowledge | 2.3 (1.3) | 1.6 (1.3) | 0.5 (1.4)c |
| Family support/behavior skills | 2.6 (1.1) | 2.4 (1.2) | 0.2 (1.3) |
| Weight management goals | 2.8 (1.0) | 2.4 (1.1) | 0.4 (1.2)c |
Items in all categories assessed on a five-point Likert scale from 0 to 4.
n varies with category from 140 to 156.
p < 0.001.
Table 3 shows the relationship between treatment expectations at baseline and odds of attrition at 3 months. For adolescents, greater interest in the category of family support/behavior skills was associated with significantly decreased odds of attrition at 3 months [for a one-unit increase in the Likert scale: odds ratio (OR) 0.75, 95% confidence interval (CI) 0.57–0.98, p = 0.04]. Specifically, compared with dropouts, adolescents who did not drop out indicated a significantly greater desire for help at baseline to get family “on board” with healthy eating changes (2.44 vs. 1.83, p = 0.02) and being physically active (2.48 vs. 1.80, p = 0.01). Additionally, for the same category of family support/behavior skills, the more discordant the parent/adolescent dyad treatment expectations (i.e., the greater the difference in expectations), the higher the odds of attrition at 3 months (for a one-unit difference in the Likert scale: OR 1.36, 95% CI 1.04–1.78, p = 0.02). No other categories of treatment expectations or concordance between adolescent/parent dyad responses were associated with attrition. As age, sex, insurance, and baseline BMI z-score were not predictors of attrition, they were not added to the model, so the final model was unadjusted.
Table 3.
Odds of Attrition Associated with Parent/Adolescent Treatment Expectations at Baseline
| Parent treatment expectationsa | Adolescent treatment expectationsb | Parent–adolescent dyad difference in treatment expectationsc | |
|---|---|---|---|
| Baseline survey category | OR (95% CI) | OR (95% CI) | OR (95% CI) |
| Healthier food/drink knowledge | 0.95 (0.78–1.15) | 0.82 (0.61–1.09) | 1.23 (0.91–1.68) |
| Healthier food/drink skills | 0.97 (0.81–1.17) | 0.83 (0.63–1.11) | 1.05 (0.79–1.41) |
| Physical activity knowledge | 1.00 (0.84–1.19) | 0.93 (0.74–1.17) | 0.94 (0.72–1.22) |
| Physical activity skills | 0.99 (0.83–1.20) | 0.80 (0.58–1.10) | 0.99 (0.76–1.29) |
| Family support/behavior knowledge | 0.98 (0.84–1.14) | 1.02 (0.80–1.30) | 1.01 (0.79–1.28) |
| Family support/behavior skills | 0.93 (0.78–1.12) | 0.75 (0.57–0.98)d | 1.36 (1.04–1.78)d |
| Weight management goals | 1.18 (0.96–1.45) | 0.94 (0.71–1.25) | 1.21 (0.91–1.60) |
Model n varied from 373 to 395.
Model n varied from 150 to 158.
Model n varied from 140 to 156.
p < 0.05.
CI, confidence interval; OR, odds ratio.
In the weight management goals category, weight loss was an important goal for both adolescents [n = 148, mean (SD), 3.3 (1.1)] and parents [n = 342, 3.0 (1.2)]. Among parents for whom their child's weight loss was a goal, the median weight-loss goal was 20 pounds. For adolescents with this goal, the median weight-loss goal was 50 pounds. Attrition was associated with adolescent weight-loss goals above the desired median for the group (50% above the median vs. 28% below the median, p = 0.02). There was no association between parents' weight-loss goals and attrition.
Discussion
A primary aim of this pilot was to evaluate the association between treatment expectations of parents and adolescents and the likelihood of discontinuing weight management within the first 3 months. Participants' expectations were categorized according to nutrition and physical activity health behaviors, family support/behavior, and weight management goals. We found that for adolescents, greater interest in family support/behavior skills, including items related to motivation and family engagement, was associated with decreased odds of leaving treatment. Specifically, adolescents remaining in treatment demonstrated greater interest in getting their families “on board” with eating healthier and being physically active compared with those who dropped out.
Several studies have identified predictors of attrition in pediatric obesity treatment.2,4–8,21–23 However, such programmatic- and patient-related factors, such as program location and insurance coverage, are often unchangeable, making them less than ideal targets for reducing attrition. In contrast, unmet patient expectations represent a potentially modifiable aspect of weight management programs that also influence patient retention.2,5,6,23 Skelton and Beech reported that unmet expectations for parents (48%) and children (52%) were one of the most frequently cited reasons for not returning to treatment.2 Likewise, Barlow and Ohlemeyer indicated that 37.2% of patients leaving treatment reported that the program was not what they were looking for, with some patients citing specific programmatic elements they would have preferred.23 Similarly, Hampl et al. found that 36.8% of patients reported mismatched expectations as having a moderate or high influence on their decision to discontinue treatment.5
Turer et al. recently reported that parent preferences for weight management strategies in primary care may differ depending on the accuracy of their perception of the child's weight status,24 supporting a need to assess parent perceptions of their child's weight status and treatment preferences for optimal outcomes. While our study focused on evaluation in the tertiary care setting, the survey tools could also be adapted and evaluated for use by a referring primary care provider when discussing whether a family may be ready for engagement in a tertiary care program.
Previous pediatric weight management research confirms the importance of a family-based approach to behavior change, including active parent involvement in role modeling, goal setting, and behavior monitoring.25,26 In this context, our findings may suggest that adolescents who place a high value on family support could be more likely to remain in treatment, assuming sufficient parental support exists. Our study results further support this reasoning, in that greater discordance between adolescent and parent responses for family support/behavior skills, that is, parents and youth who disagree on the importance of familial involvement, was also associated with increased odds of attrition. This underscores the importance of a shared dialogue between patient, parent, and provider regarding family-based change.27 Future research is needed to further explore the relationship between attrition and the individual components addressed in the family support/behavior survey categories, such as bullying, self-esteem, and motivation. Additional psychometric analysis of the survey tool, such as confirmatory factor analysis, may also clarify whether all scales support a unidimensional construct despite already strong support for internal consistency based on the Cronbach's alphas. A recently described trial conducted following ours, Connect for Health,28 has utilized a behavior change decision aid with health coaches for pediatric obesity management in primary care, which may further inform this line of research.
Baseline BMI z-score did not predict attrition, similar to recent findings of Pratt et al.29 However, unrealistic weight-loss goals among the adolescents were associated with higher likelihood of attrition, suggesting that setting realistic weight-loss expectations may support both improved process and outcomes in pediatric weight management.
A strength of the study was the use of a large multisite sample, allowing evaluation of patient expectations across programs with differing structures. However, the current study was not without limitations. Unfortunately, for most families who dropped out of treatment, follow-up survey data at 3 months could not be collected (Fig. 1); thus, our original aim to evaluate the relationship between the achievement of treatment expectations and attrition could not be pursued. Such an evaluation may have demonstrated some variability in the effectiveness of differing strategies used with the survey tool that warrants future investigation. In addition, our follow-up timeline was limited to 3 months by the scope of the FOCUS on a Fitter Future workgroup. While there is no consensus in the literature on a definition of attrition,3 these data may only reflect early attrition from pediatric weight management and include patients who may later return after a treatment hiatus. Furthermore, we also combined patients being evaluated in both program and clinic formats in our definition of attrition. Although we were not able to differentiate the impact of separating these groups, as our timeline was only 3 months, the definition of attrition for a program translated into at most two visits (less than 25% of the most intensive weekly visit program), which was similar to our clinic definition of attrition limited to one visit. Future research investigating the clinical utility of a treatment expectations survey and its relationship to retention should consider an expanded study timeline, administrative support to ensure follow-up with families who leave the treatment, and the impact of different formats of treatment interventions on the variability in attrition. It may also be worthwhile to assess how and whether parents and adolescents distinguish goals and responsibility for behavior change. Finally, due to missing data for race/ethnicity, we were not able to reliably assess the impact of race or ethnicity on attrition. As race/ethnicity as well as other sociodemographic variables have been associated with attrition in some studies, future research with complete data for race/ethnicity should further address this question.
Conclusions
Unmet patient expectations represent a potentially modifiable aspect of treatment for pediatric obesity. This study adds to the pediatric weight management attrition literature by describing relationships between parent and adolescent treatment expectations at the start of treatment and attrition over 3 months. Our findings demonstrate that for adolescents, greater interest in family support/behavior skills was associated with decreased odds of attrition at 3 months and those desiring greater levels of weight loss more often prematurely left the treatment. These findings support the use of a survey tool, such as the one presented here, to assess initial expectations to help tailor treatment to better meet families' needs, especially through focus on family-based change and realistic goal setting. Further study is needed to examine the impact of this tailored approach on retention.
Supplementary Material
Acknowledgments
The authors thank Stacy Biddinger MPA (Children's Hospital Association), Michelle Demeule, MS, RD, LDN (Mt. Washington Pediatric Hospital), Ihouma Eneli, MD, MS (Nationwide Children's Hospital), Cristina Fernandez, MD (Children's Hospital and Medical Center), Meg Green, MS, RD, CSP, LD (Arkansas Children's Hospital), Renee Porter, RN, MS, ND (Children's Hospital Colorado), and Patty Stephan, LMSW (Helen DeVos Children's Hospital) along with the study coordinators at each site for their assistance with this project. Portions of this study were presented in abstract form at the Society of Pediatric Psychology Annual Conference, March 27–29, 2014, Philadelphia, PA, and the Pediatric Academic Societies' 2014 Annual Meeting, May 3–6, 2014, Vancouver, BC, Canada.
The authors acknowledge the Children's Hospital Association as the primary project sponsor for FOCUS on a Fitter Future, which was also funded, in part, by the Mattel Children's Foundation. The study sponsor had no role in study design, collection or interpretation of data, the writing of the report, or the decision to submit the manuscript for publication. The sponsor hosted study group meetings and provided funding for statistical analysis. An editor supplied by the sponsor reviewed a final draft of the manuscript. The views expressed are those of the authors and do not necessarily reflect those of the Children's Hospital Association. Additional funding was provided by the New Balance Foundation Obesity Prevention Center Boston Children's Hospital. Dr. Boles was supported, in part, by NIH (NIDDK) K23DK087826.
Author Disclosure Statement
Dr. Rhodes receives research funding support from Merck. Dr. Rhodes' research with Merck is focused on type 2 diabetes mellitus and is therefore unrelated to the subject of this article. The remaining authors have no competing financial interests to disclose.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Skelton JA, Beech BM. Attrition in paediatric weight management: A review of the literature and new directions. Obes Rev 2011;12:e273–e281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dhaliwal J, Nosworthy NM, Holt NL, et al. Attrition and the management of pediatric obesity: An integrative review. Child Obes 2014;10:461–473 [DOI] [PubMed] [Google Scholar]
- 4.Hampl S, Paves H, Laubscher K, Eneli I. Patient engagement and attrition in pediatric obesity clinics and programs: Results and recommendations. Pediatrics 2011;128 Suppl 2:S59–S64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hampl S, Demeule M, Eneli I, et al. Parent perspectives on attrition from tertiary care pediatric weight management programs. Clin Pediatr (Phila) 2013;52:513–519 [DOI] [PubMed] [Google Scholar]
- 6.Sallinen Gaffka BJ, Frank M, Hampl S, et al. Parents and pediatric weight management attrition: Experiences and recommendations. Child Obes 2013;9:409–417 [DOI] [PubMed] [Google Scholar]
- 7.Cote MP, Byczkowski T, Kotagal U, et al. Service quality and attrition: An examination of a pediatric obesity program. Int J Qual Health Care 2004;16:165–173 [DOI] [PubMed] [Google Scholar]
- 8.Skelton JA, DeMattia LG, Flores G. A pediatric weight management program for high-risk populations: A preliminary analysis. Obesity (Silver Spring) 2008;16:1698–1701 [DOI] [PubMed] [Google Scholar]
- 9.Guite JW, Kim S, Chen CP, et al. Treatment expectations among adolescents with chronic musculoskeletal pain and their parents before an initial pain clinic evaluation. Clin J Pain 2014;30:17–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Giannini C, Irby MB, Skelton JA. Caregiver expectations of family-based pediatric obesity treatment. Am J Health Behav 2015;39:451–460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tremblay M, Perez AJ, Rasquinha AM, et al. Recommendations from parents to improve health services for managing pediatric obesity in Canada. Acad Pediatr 2016;16:587–593 [DOI] [PubMed] [Google Scholar]
- 12.Rhee KE, De Lago CW, Arscott-Mills T, et al. Factors associated with parental readiness to make changes for overweight children. Pediatrics 2005;116:e94–e101 [DOI] [PubMed] [Google Scholar]
- 13.Jacobson Vann JC, Finkle J, Ammerman A, et al. Use of a tool to determine perceived barriers to children's healthy eating and physical activity and relationships to health behaviors. J Pediatr Nurs 2011;26:404–415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall Inc., 1986 [Google Scholar]
- 15.Broderick BC. Understanding Family Process: Basics of Family Systems Theory. Thousand Oaks, CA: Sage Publications, 1993 [Google Scholar]
- 16.Krebs NF, Jacobson MS. Prevention of pediatric overweight and obesity. Pediatrics 2003;112:424–430 [DOI] [PubMed] [Google Scholar]
- 17.Daniels SR, Hassink SG; Committee On Nutrition. The role of the pediatrician in primary prevention of obesity. Pediatrics 2015;136:e275–e292 [DOI] [PubMed] [Google Scholar]
- 18.Macias YF, Glasauer P. Guidelines for assessing nutrition-related Knowledge, Attitudes and Practices. Available at www.fao.org/docrep/019/i3545e/i3545e00.htm accessed October30, 2016
- 19.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC Growth Charts for the United States: Methods and development. Vital Health Stat 2002;11(246):1–190 [PubMed] [Google Scholar]
- 20.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zeller M, Kirk S, Claytor R, et al. Predictors of attrition from a pediatric weight management program. J Pediatr 2004;144:466–470 [DOI] [PubMed] [Google Scholar]
- 22.Dolinsky DH, Armstrong SC, Ostbye T. Predictors of attrition from a clinical pediatric obesity treatment program. Clin Pediatr (Phila) 2012;51:1168–1174 [DOI] [PubMed] [Google Scholar]
- 23.Barlow SE, Ohlemeyer CL. Parent reasons for nonreturn to a pediatric weight management program. Clin Pediatr (Phila) 2006;45:355–360 [DOI] [PubMed] [Google Scholar]
- 24.Turer CB, Upperman C, Merchant Z, et al. Primary-care weight-management strategies: Parental priorities and preferences. Acad Pediatr 2016;16:260–266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heinberg LJ, Kutchman EM, Berger NA, et al. Parent involvement is associated with early success in obesity treatment. Clin Pediatr (Phila) 2010;49:457–465 [DOI] [PubMed] [Google Scholar]
- 26.Sharifi M, Marshall G, Goldman RE, et al. Engaging children in the development of obesity interventions: Exploring outcomes that matter most among obesity positive outliers. Patient Educ Couns 2015;98:1393–1401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wrotniak BH, Epstein LH, Paluch RA, Roemmich JN. The relationship between parent and child self-reported adherence and weight loss. Obes Res 2005;13:1089–1096 [DOI] [PubMed] [Google Scholar]
- 28.Taveras EM, Marshall R, Sharifi M, et al. Connect for Health: Design of a clinical-community childhood obesity intervention testing best practices of positive outliers. Contemp Clin Trials 2015;45(Pt B):287–295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pratt KJ, Collier DN, Walton NL, et al. Predictors of follow-up for overweight youth and parents. Fam Syst Health 2015;33:55–60 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.