Abstract
Objective
To elicit expert views to define the aims, optimal design, format and function of an inflammatory bowel disease (IBD) multidisciplinary team (MDT) with the overall purpose of enhancing the quality of MDT-driven care within an IBD service provision.
Design
This study was a multicentre, prospective, qualitative study using a standard semistructured interview methodology.
Participants
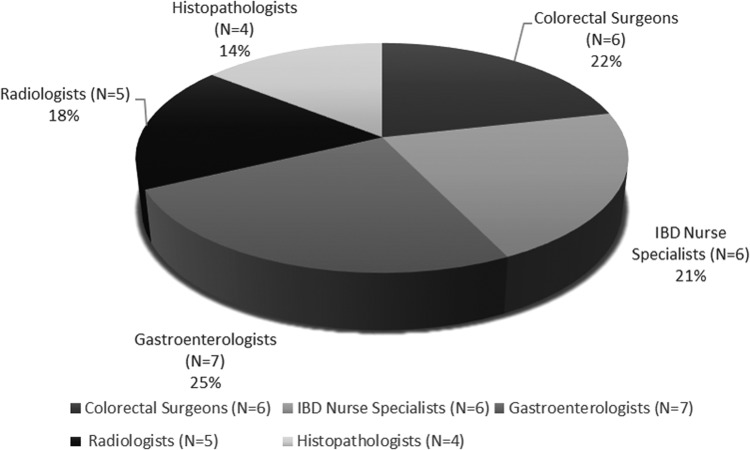
A multidisciplinary sample of 28 semistructured interviews of which there are six consultant colorectal surgeons, six IBD nurse specialists, seven consultant gastroenterologists, five consultant radiologists and four consultant histopathologists.
Setting
Participants were recruited from 10 hospitals, which were a mixture of community hospitals and specialist IBD centres between June and October 2013.
Results
Experts argued that the main goal of MDT-driven IBD care is to improve patient outcomes via sharing collective expertise in a formalised manner. Themes regarding the necessary requirements for an IBD MDT to occur included good attendance, proactive contribution, a need to define core members and appropriate and functional computer facilities. Emergent themes regarding the logistics of an effective IBD MDT included an eligibility criterion for case selection and discussion and appropriate scheduling. Themes regarding the overall design of the IBD MDT included a ‘hub-and-spoke’ model versus a ‘single-centre’ model.
Conclusions
Defining key elements for an optimal design format for the IBD MDT is necessary to ensure quality of care and reduce variation in care standards. This study has produced a set of expert-based standards that can be used to structure the IBD MDT. These standards now require larger scale validation and consensus prior to becoming a practical guideline for the management of IBD care.
Keywords: IBD, IBD CLINICAL, IBD SURGERY, HEALTH SERVICE RESEARCH
Introduction
Inflammatory bowel disease (IBD) service provision and care is being analysed as part of a general drive to reduce variation in standards of healthcare and to improve the quality of services that patients receive.1–3 Variability across institutions in 30-day reoperation rates following colorectal resection was identified in the UK. A diagnosis of IBD was demonstrated as an independent risk factor for higher reoperation rates.4 Heterogeneity in opinion between gastroenterologists, colorectal surgeons (CSs) and patients exists in treatment algorithms for IBD.5 6 The lack of clear guided standards in the setting of complex IBD may result in clinical decisions being made from an intuitive mix of probability judgements, experience and sometimes bias, combined with implicit judgements on the importance of possible outcomes. While attempts are made to elicit patient preferences in relation to the latter, the success of such patient-centred algorithms has yet to be proven.
The reason for differences in opinion between clinicians is yet to be determined, however, there is need for consensus and standardisation in the setting of IBD and related services. Closer and more focused monitoring of existing services can help steer healthcare provision and guide commissioning of clinical services to generate greater efficiency, productivity, economy and ultimately better service at patient level by initiating targeted change.4 Some UK-based centres are moving into this direction—via the introduction of multidisciplinary teams (MDTs) to manage patients with IBD. The concept of MDT-driven care has been widely implemented for the clinical decision-making and management of complex diseases, like cancer,7 cardiac disease,8 stroke and neurological rehabilitation9 and diabetes.10 The basic premise of MDT-driven care is to involve all key professional groups in the consideration of complex patients and/or diagnostic dilemmas to create a clear care plan. It is a forum where clinical cases can be discussed among a variety of healthcare professionals and care recommendations are made. The implementation of MDT-driven care has demonstrated an improvement in survival across various specialties.11–14 Efforts are being made to standardise the organisational structure and design of MDT-driven care into further improve this effect.15
MDT-driven care is now being introduced into IBD centres.16 The UK National IBD Audit demonstrated that 75% of participating institutions undertake a weekly MDT meeting for patients with IBD.1 2 European centres have also demonstrated variability in MDT-driven care.17 There is, however, little evidence of its efficacy in this context, and currently, there is no guidance on how this intervention may be standardised and used effectively.1–3 Variability in the workings of the cancer MDT has been demonstrated and protocols for the structure of this meeting are being designed and implemented.8 Providing a standardised framework for the IBD MDT meeting may enhance its capacity to establish effective quality improvement.
The aim of this study was to (1) explore attitudes towards the IBD MDT across a multidisciplinary sample of healthcare professionals, (2) identify expert views as to what the purpose or aims of the IBD MDT should be and (3) highlight logistical considerations when designing the IBD MDT to meet these aims.
Methodology
Design
This was a prospective, qualitative study using a standard semistructured interview methodology. The qualitative approach was deliberately chosen as it offers detailed information from individual participants and is well suited to explore complex and potentially controversial issues, from which hypotheses and interventions can be generated and tested further.18 19 The protocol for the study was reviewed by a Research Ethics Committee in London, UK, and approval was given prior to data collection (Research Ethics Committee reference: 13YH 0175).
Research materials and procedure
Interviews were carried out using a standardised and piloted semistructured interview protocol delivered by two trained interviewers of clinical background (PM and JR). To ensure credibility, transferability, dependability and confirmability appropriate to qualitative research, the following established measures were employed: (1) use of a standardised interview protocol and clearly defined coding framework; (2) training of the interviewer before interviews and (3) transparency of process and ‘member checking’ (ie, checking with participants that the extracted themes from their interviews matched what they actually meant) to ensure that accurate findings had been extracted from the interviews.19–22 The interview protocol explored key themes encompassing key elements for an effective IBD MDT, including an understanding of the role and purpose of the IBD MDT, structural inputs required for an effective IBD MDT meeting, logistical considerations for an effective IBD MDT meeting and what the overall design of an effective IBD MDT should entail.
Interviews lasted 20 min on average (range 3–40 min). All interviews were audiotaped and transcribed verbatim. Each interview was coded independently by two members of the research team with backgrounds in surgery (PM) and gastroenterology (JR).
Participants
The multidisciplinary sample included consultant colorectal surgeons (CSs), consultant gastroenterologists (CGs), consultant gastrointestinal (GI) histopathologists (CPs), consultant GI radiologists (CRs) and IBD nurse specialists (NSs), and were recruited from two separate regions in the UK (the Southwest region and London), across multiple institutions. Participation was voluntary, and informed consent was obtained from all participants prior to data collection. Anonymity was ensured throughout the study. The sample size was determined on the basis of the ‘saturation’ of the themes that emerge from participant interviews: that is, when similar themes are being extracted, the sample was deemed adequate.23 This is a standard sample size estimator used in this type of qualitative research.18
Data analysis
The standard recommended analytical techniques were used for analysis of the qualitative data that emerged from the study.18 All interviews were audiotaped and transcribed verbatim. Transcripts were cross-checked with the original recordings to ensure accuracy. Each transcript was subsequently analysed for content to identify emergent themes by a coder (JR). Emergent themes were reviewed by a second member of the research team (PM) who was blind to the theme extraction process, and key themes were tabulated. To establish confirmability in accordance with qualitative research, all themes were finally reviewed by a senior member of the research team (NS) with a background in psychology and patient safety.20
Results
Thematic saturation was achieved after 28 semistructured interviews (six CSs, six IBD NSs, seven CGs, five CR and four CPs, figure 1). Individual interviews took place face to face (n=12) and via telephone (n=16) between June and October 2013. Participants were recruited from 10 hospitals, which were a mixture of community hospitals and specialist IBD centres. In the Southwest, 15 participants were interviewed: two CSs, six CGs, three IBD NS, two CRs and two CPs. In the London region, 12 participants were interviewed: three CSs, one CG, three IBD NSs, three CRs and two CPs.
Figure 1.
Pie chart demonstrating relative proportion of specialists within the multidisciplinary sample—there were six consultant surgeons, six inflammatory bowel disease (IBD) nurse specialists, seven consultant gastroenterologists, five consultant radiologists and four consultant pathologists.
Twenty responding experts were regular attenders to an IBD MDT within their institution. These comprised six IBD NSs, seven CGs, two CPs, two CRs and three CSs. Seven experts described a variable attendance to the IBD MDT. They consisted of two CSs, three CRs and two CPs. There was one consultant CS who did not attend an IBD MDT.
Online supplementary tables S1–S4 summarise the main findings for each question in the interview protocol (ie, the themes extracted), the number of participants who mentioned each theme and relevant illustrative quotations. The code letter suffixed to each quotation refers to consultant CS, CG, CR, CP and IBD NS.
Role and purpose of the IBD MDT
Online supplementary table S1 describes the information for the role and purpose of the IBD MDT.
Role
Fifteen participants, across all healthcare disciplines (one CS, four CGs, three CPs, three CRs and four IBD NSs), thought there was a role for MDT-driven care in IBD. Perceived reasons for this included a recognition of IBD being a complex disease (n=11) and decision-making not being straightforward (n=10). One participant thought that there was no role for the MDT meeting in the care of patients with IBD because ‘resources, time and money are a huge issue; on that basis it's very difficult in my mind to justify MDTs’ (CS2). The interview was discontinued at 3 min as further discussions relating to IBD MDT structure, format and function was not appropriate.
Purpose
Twenty-one participants thought that the purpose of the IBD MDT is to share collective experience and expertise. In addition, the IBD MDT should aim to provide a consensus on decision-making (n=17) and improve patient outcome (n=15). Twelve respondents felt that an additional purpose should be in the setting of clinical governance. In particular, one CS stated: ‘it protects everyone that's involved…it’s easier to say, ‘The team decision was’ …I think that's an important role that people forget from the MDT…’ (CS4).
Structural inputs for an effective IBD MDT
Online supplementary table S2 details the necessary requirement for an effective IBD MDT to occur.
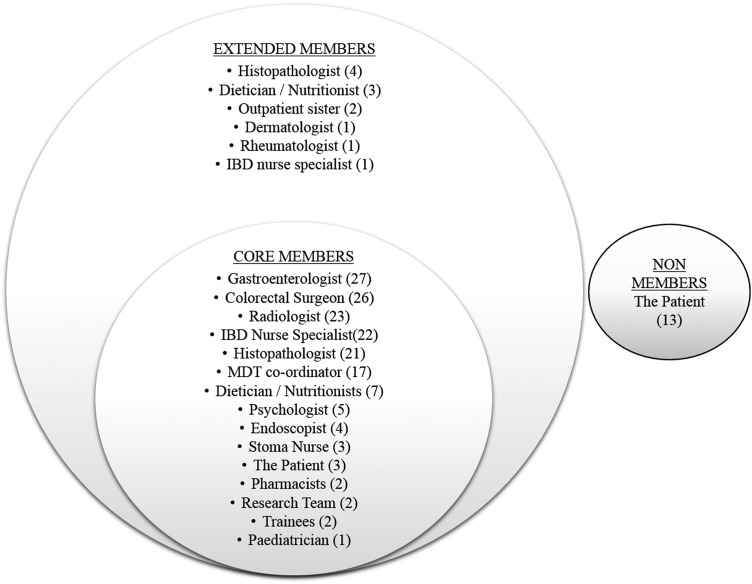
Core and extended members of the IBD MDT
Eighteen participants perceived that ensuring a good attendance is considered an important requirement for an effective IBD MDT to occur. Three participants (one CG, one CR and one IBD NS) perceived the attendance of a CS was sporadic. Further definitions of who should be core (regular attenders to the IBD MDT with contractual IBD MDT responsibilities), extended (attender invited by core members to the IBD MDT) and non-members (people who are not invited to attend the IBD MDT) were asked (figure 2). There was heterogeneity in opinion as to the presence of a histopathologist, dietician and patient as core members of the IBD MDT. It was further suggested that to ensure attendance by those deemed core members, presence should be protected time and apart of the job plan ‘it lacks the pathology input because formally we are not scheduled to go. It's not part of our job plan to attend this meeting so it is only on a voluntary basis’ (CP1).
Figure 2.
Perceived responses (and number of respondents) as to who should be core members, extended members and non-members of the inflammatory bowel disease (IBD) multidisciplinary team (MDT).
Thirteen participants perceived that the patient themselves should not be core members of the IBD MDT and three participants felt that the patient should be core members of the IBD MDT. ‘…the level of discussion and the pace at which decisions are made… if a patient was there it would just slow things down too much…(it) feels uncomfortable saying that because patients should be involved in their decision…you can involve the patient in the decision without them being there at the time of the MDT’ (CS7).
Ensuring multidisciplinary contribution
Twenty-two participants perceived that multidisciplinary contribution was a necessary requirement for an effective IBD MDT. One respondent stated that ‘you're dealing with a lot of personalities’ (NS4). Thirteen participants suggested that a means to facilitate multidisciplinary contribution within the IBD MDT is for the presence of a chair person: ‘…a clear chairperson, who leads the discussion…’ (CP2) and ‘…alternating the chairperson so that it moves from one consultant to the next…’ (NS4).
Logistical considerations for an effective IBD MDT
Online supplementary table S3 demonstrates logistical considerations deemed relevant by the participants.
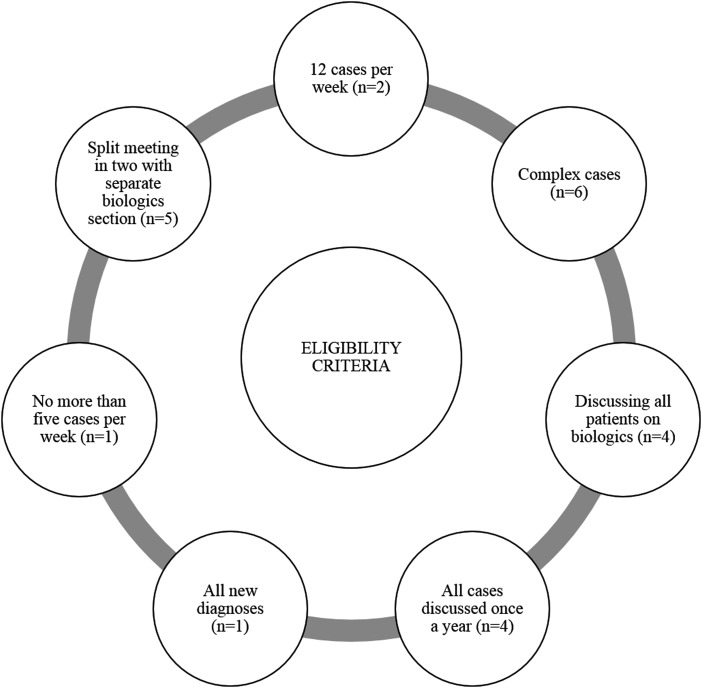
Eligibility criteria for case discussion
Nineteen participants agreed that there must be an eligibility criterion applied for case selection and discussion—‘in some places it might be that they can discuss all of their IBD cases; in others it might have to be selected to the higher risk ones, you know, such as the surgical ones and the non-surgical ones’ (CS6). Figure 3 demonstrates respondent considerations as to how cases can be selected for discussion in the IBD MDT. High-ranking elements included complex cases only (n=6) and separating patients on biologics into another ‘biologics meeting’ (n=5). Other suggested elements to an eligibility criterion included: all IBD cases to be discussed at least once a year (n=4), all new IBD diagnoses (n=1), no more than five cases (n=1) or 12 (n=2) cases to be discussed per MDT session or all patients to be started on biological therapies (n=4).
Figure 3.
Respondent suggestions as to how best to protocol case selection for the inflammatory bowel disease (IBD) multidisciplinary team (MDT)—application of an eligibility criterion for cases to be discussed in the IBD MDT.
Scheduling
The majority of participants (n=10) reported that the duration of the IBD MDT should be no longer than 1 h, however, it was stated by one participant that: ‘It depends on the volume of the cases that go through your institution. If you only have one or two cases a week, a half an hour IBD MDT would be quite adequate…If you have to discuss 10 or 15 cases, you might need a two hour MDT…’ (CS4).
The majority of participants (n=16) also reported that the IBD MDT should be scheduled for once a week. One participant reported the added benefit this would bring: ‘… if there are any inpatients that need to be discussed…two weeks is too far apart’. However, the same participant also stated: ‘…if you're a small unit, or a small hospital… an hour once a week…there may be no patients to discuss, or one or two patients to discuss…’ (CG7).
Overall design of an effective IBD MDT
Online supplementary table S4 discusses elements to consider in the overall design of the IBD MDT.
Seven participants favoured a hub-and-spoke model, where multiple smaller units were linked into a centralised IBD unit via teleconference capabilities. Concerns were raised as to the resources and constraints this may place on the central unit, and suggested: ‘…some happy medium … it may be that two hospitals would be okay’ (CS6). Medicolegal concerns were also raised to this model: ’…we've had cases where consultants from elsewhere have provided us with clinical details (of) a patient that we've never seen…and we're meant to be making decisions about what happens to them… I get quite nervous about that’ (NS4). The majority of participants (n=10) favoured a single-centre model, where each institution holds their own IBD MDT.
Discussion
The study reveals some of the key elements and requirement for an effective IBD MDT as perceived by expert healthcare providers currently involved in IBD care. Overall, there was a positive perception of the role of the MDT in IBD care among all participants within the multidisciplinary group, however, a range of potential elements to consider for good MDT working were mentioned.
First, the need for good attendance was described as a necessity for the establishment of an effective IBD MDT, in order to facilitate effective decision-making. From our participants, CSs, CRs and CPs admitted to being variable or non-attenders to the IBD MDT. Frustrations were also raised by CGs with the variable attendance of certain specialists, particularly CSs, and the impact this has on shared decision-making. The respective experts were also viewed as core members of the IBD MDT (figure 2). Non-attendance of key members is a barrier to effective decision-making in the IBD MDT setting.24 25 Recommendations made by the participants to ensure attendance included making the IBD MDT part of the job plan and ensuring that it is protected time.
Second, there was a requirement for multidisciplinary contribution for an effective IBD MDT to occur. Studies in UK cancer MDTs, which have been implemented for almost 20 years, have shown contributions from physicians outweigh those from nurses26 and an overall bias of the MDT towards the biological side of cancer at the expense of the psychosocial circumstances of the patient—which are often left to the surgeon who sees the patient in clinic to manage alone. The presence of different personalities within the IBD MDT was viewed as source of varying contribution. A means to improve this was by introducing an alternating formal chair person who can lead discussions and ensure multidisciplinary contribution. A recommendation that was consistent with a previous UK-based study that found the role of the chair can rotate between team members with adequate chairing skill.27
An emergent theme that arose was the need for a selection process to limit the demands on the IBD MDT. Numerous suggestions were made, including discussing no more than five patients in one session, splitting the meeting so those on biological therapy are discussed separately, or discussing only ‘complex’ IBD cases, with complex IBD defined by one participant as those requiring surgery.
Viewpoints on the scheduling of the IBD MDT varied considerably. Many believed that appropriate scheduling should depend on and be decided by core members within the institution to maximise attendance. Most participants agreed however that having a meeting once a week was sufficient and lasting no longer than 1 h. Scheduling the meeting once a week had the added benefit of discussing inpatient or urgent cases, however, in institutions attending to a smaller volume of patients with IBD, weekly meetings may not have the necessary number of cases discussed to use the time. These institutions may benefit with having the IBD MDT combined with other MDTs. Most participants, however, agree that the IBD MDT should be solely for the discussion of patients with IBD. In such cases, a ‘hub-and-spoke’ model would also benefit smaller institutions.
The above findings are subject to the limitations of this study. First, expert opinions from the participants may not be fully generalisable to other IBD experts, especially considering that IBD MDTs are being increasingly recognised across multiple European and North American institutions. Despite this, interviews have occurred across five mainstream IBD groups, and a wide geographical area within the UK was covered, involving multiple institutions including district general hospitals as well as teaching hospitals. Second, the duration of the interviews was short and lacks ‘prolonged engagement’ which is a recognised criterion to ensure credibility in qualitative research.20 Third, the process of member checking while considered a good practice by some, it does carry the potential risks of changing the spontaneous response offered during the interview process28 (although this was not observed in this study, as none of the participants edited or amended their prior responses when member checking was carried out). Despite these limitations, the use of semistructured interviews was appropriate to meet the aims of the study. Evidence provided from the findings of this study will be validated through Delphi consensus.
MDT-driven care is arising intuitively within the setting of IBD. There is, however, much variation in the conduct of the MDT, impeding its effectiveness in the delivery of a high-quality care. In order to standardise cancer care, measures were introduced to improve care provision with the overall purpose of ensuring high-quality care. Such measures included interventions to support clinical decision-making through the cancer MDT meeting.7 Variability in the workings of the cancer MDT has been demonstrated and protocols for the structure of this meeting have been devised and implemented.29 A recognition that the MDT is an acceptable model by which to deliver safe and high-quality cancer care has been established, and a requirement of organisational support was necessary to ensure the delivery of the MDT. Furthermore, the need of a locally agreed minimum data set on each patient has been recognised as a logistical necessity for the cancer MDT.30 Interestingly, these elements did not transpire as an emergent theme within this study—but on the other hand, these important considerations were not specifically addressed in the interview protocol. Such elements deserve further investigation. Evidence has supported improved outcomes following the implementation of these measures in general.11 13 31 32 Providing a standardised framework for the IBD MDT will enhance its capacity to establish effective quality improvement, better outcomes and patient experience in IBD care. Lessons already learnt from the standardisation of the cancer MDT can be implemented into the setting of the IBD MDT so as to avoid repetition of error, and progress towards a swift delivery of MDT-driven care within IBD.
In conclusion, the MDT meeting is widely employed by institutions throughout the UK in the care of patients with IBD. This study explores, in depth, some of the issues that surround requirements and logistics for an effective IBD MDT to occur. Emergent themes include the need for good attendance by core members, coordinated multidisciplinary contribution with an alternating chair person, appropriate case selection and scheduling. Defining key elements for the optimal design format for the IBD MDT is necessary to ensure quality of care and reduce variation in care standards. This study demonstrates the methodology used for construction of provisional standards for the IBD MDT through interviews from a multidisciplinary group. Selection and adjustments of these standards through expert consensus are required to validate measures.
Key messages.
What is already known about this subject?
Variability exists in IBD service provision across institutions nationally. MDT driven care is arising intuitively within IBD care, but there is a lack of clear evidence for this practice and a lack of consistency in its implementation in the setting of complex IBD.
What are the new findings?
Participants perceived the purpose of the IBD MDT should be to provide a consensus on decision-making and improve patient outcome. There is a need to define the role of specialists as ‘core’ and ‘extended’ members of the IBD MDT to ensure attendance and proactive contribution. An eligibility criteria was perceived to be necessary for case selection and discussion in the IBD MDT.
How might this impact on clinical practice in the foreseeable future?
This study has elicited provisional standards for the IBD MDT through interviews from a multidisciplinary group. Selection and adjustment of these standards though expert consensus are required to validate measures, which will help the IBD MDT establish effective quality improvement and improved outcomes.
Supplementary Material
Footnotes
Contributors: PM, CE, JG, NS and OF contributed to the planning of this study. PM, SA, JR contributed to the conduct of the study. PM, NS, JG, AH, JW and OF contributed to the reporting of the work.
Funding: PM, OF, CE and NS are affiliated with the Health Services Award funded by Crohn's and Colitis UK (IBDHS/13/1) Crohn's and Colitis UK. SA, NS (until January 2015) and JG are affiliated with the Imperial NIHR Grant: RDPSC 79560 UK. NS is currently funded by the NIHR Collaboration for Leadership in Applied Health Research and Care South London at King’s College Hospital NHS Foundation Trust. CE is affiliated with the Jean Brown Memorial Fund, which is a component of the South Devon Healthcare Charitable Fund (Registered charity number 1052232).
Competing interests: NS and JG delivers teaching and consultancy-based work on evaluating and improving MDT effectiveness and team processes for hospitals in the UK and internationally.
Ethics approval: NRES Committee Yorkshire & The Humber–Humber Bridge.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Group TUIAS. UK IBD Audit 2nd Round (2008) Report—Executive Summary of the National Results for the Organisation & Process of Adult IBD Care in the UK. 2009.
- 2.Group TUIAS. UK IBD Audit 2006—Executive Summary of the National Results for the Organisation & Process of IBD Care in the UK 2007.
- 3.Group ISW. Quality care: service standards for the healthcare of people who have Inflammatory Bowel Disease (IBD). IBD Standards Group, 2009. [Google Scholar]
- 4.Burns EM, Bottle A, Aylin P, et al. . Variation in reoperation after colorectal surgery in England as an indicator of surgical performance: retrospective analysis of Hospital Episode Statistics. BMJ 2011;343:d4836 doi:10.1136/bmj.d4836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Byrne CM, Solomon MJ, Young JM, et al. . Patient preferences between surgical and medical treatment in Crohn's disease. Dis Colon Rectum 2007;50:586–97. doi:10.1007/s10350-006-0847-0 [DOI] [PubMed] [Google Scholar]
- 6.Shariff U, Narula H, Speake W, et al. . Terminal ileal Crohn's disease: conservative surgeon and aggressive physician? Colorectal Dis 2009;11:522–3. doi:10.1111/j.1463-1318.2009.01820.x [DOI] [PubMed] [Google Scholar]
- 7.Haward RA. The Calman-Hine report: a personal retrospective on the UK's first comprehensive policy on cancer services. Lancet Oncol 2006;7:336–46. doi:10.1016/S1470-2045(06)70659-3 [DOI] [PubMed] [Google Scholar]
- 8.NHS. National service framework for coronary heart disease. UK: Department of Health, 2000. [Google Scholar]
- 9.NHS. National service framework for older people. Department of Health, 2001. [Google Scholar]
- 10.NHS. National service framework for diabetes: standards. UK: Department of Health, 2001. [Google Scholar]
- 11.Kersten C. Does in-house availability of multidisciplinary teams increase survival in upper gastrointestinal-cancer? World J Gastrointest Oncol 2013;5:60 doi:10.4251/wjgo.v5.i3.60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kesson EM, Allardice GM, George WD, et al. . Effects of multidisciplinary team working on breast cancer survival: retrospective, comparative, interventional cohort study of 13 722 women. BMJ 2012;344(apr26 1):e2718–e. doi:10.1136/bmj.e2718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eaker S. Regional differences in breast cancer survival despite common guidelines. Cancer Epidemiol Biomarkers Prev 2005;14:2914–8. doi:10.1158/1055-9965.EPI-05-0317 [DOI] [PubMed] [Google Scholar]
- 14.Gomella LG, Lin J, Hoffman-Censits J, et al. . Enhancing prostate cancer care through the multidisciplinary clinic approach: a 15-year experience. J Oncol Practice 2010;6:e5–10. doi:10.1200/JOP.2010.000071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Taylor C, Ramirez A-J. Defining the characteristics of effective MDT working in cancer care. BMJ Support Palliat Care 2011;1(Suppl 1):A23 doi:10.1136/bmjspcare-2011-000105.61 [Google Scholar]
- 16.Panes J, O'Connor M, Peyrin-Biroulet L, et al. . Improving quality of care in inflammatory bowel disease: what changes can be made today? J Crohns Colitis 2014;8:919–26. doi:10.1016/j.crohns.2014.02.022 [DOI] [PubMed] [Google Scholar]
- 17.Cassinotti A, Keshav S, Ardizzone S, et al. . IBD care in Europe: a comparative audit of the inpatient management of Crohn's disease and ulcerative colitis using the national UK IBD audit tool. J Crohns Colitis 2009;3:291–301. doi:10.1016/j.crohns.2009.08.002 [DOI] [PubMed] [Google Scholar]
- 18.Pope C, Ziebland S, Mays N. Analysing qualitative data. Bmj 2000;320:114–16. doi:10.1136/bmj.320.7227.114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Britten N. Qualitative Research: Qualitative interviews in medical research. BMJ 1995;311:251–3. doi:10.1136/bmj.311.6999.251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lincoln YS, Guba EG. Naturalistic Inquiry. SAGE Publications, 1985. [Google Scholar]
- 21.Mays N, Pope C. Qualitative research: Rigour and qualitative research. Bmj 1995;311:109–12. doi:10.1136/bmj.311.6997.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mays N, Pope C. Assessing quality in qualitative research. Bmj 2000;320:50–2. doi:10.1136/bmj.320.7226.50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kneebone R, Fry H. Principles and methods in qualitative research. In: Athanasiou T, Debas H, Darzi A, eds. Key topics in surgical research and methodology. Berlin, Heidelberg: Springer, 2010:243–53. [Google Scholar]
- 24.Jalil R, Ahmed M, Green JS, et al. . Factors that can make an impact on decision-making and decision implementation in cancer multidisciplinary teams: an interview study of the provider perspective. Int J Surg 2013;11:389–94. doi:10.1016/j.ijsu.2013.02.026 [DOI] [PubMed] [Google Scholar]
- 25.Lamb BW, Brown KF, Nagpal K, et al. . Quality of care management decisions by multidisciplinary cancer teams: a systematic review. Ann Surg Oncol 2011;18:2116–25. doi:10.1245/s10434-011-1675-6 [DOI] [PubMed] [Google Scholar]
- 26.Lamb BW, Sevdalis N, Mostafid H, et al. . Quality improvement in multidisciplinary cancer teams: an investigation of teamwork and clinical decision-making and cross-validation of assessments. Ann Surg Oncol 2011;18:3535–43. doi:10.1245/s10434-011-1773-5 [DOI] [PubMed] [Google Scholar]
- 27.Lamb B, Payne H, Vincent C, et al. . The role of oncologists in multidisciplinary cancer teams in the UK: an untapped resource for team leadership? J Eval Clin Pract 2011;17:1200–6. doi:10.1111/j.1365-2753.2010.01507.x [DOI] [PubMed] [Google Scholar]
- 28.Hagens V, Dobrow MJ, Chafe R. Interviewee transcript review: assessing the impact on qualitative research. BMC Med Res Methodol 2009;9:47 doi:10.1186/1471-2288-9-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lamb BW, Sevdalis N, Vincent C, et al. . Development and evaluation of a checklist to support decision making in cancer multidisciplinary team meetings: MDT-QuIC. Ann Surg Oncol 2012;19:1759–65. doi:10.1245/s10434-011-2187-0 [DOI] [PubMed] [Google Scholar]
- 30.Team NCA. The Characteristics of an Effective Multidisciplinary Team (MDT). Service NH; http://www.nhsiq.nhs.uk2010 [Google Scholar]
- 31.Morris E, Haward RA, Gilthorpe MS, et al. . The impact of the Calman-Hine report on the processes and outcomes of care for Yorkshire's colorectal cancer patients. Br J Cancer 2006;95: 979–85. doi:10.1038/sj.bjc.6603372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stephens MR, Lewis WG, Brewster AE, et al. . Multidisciplinary team management is associated with improved outcomes after surgery for esophageal cancer. Dis Esophagus 2006;19: 164–71. doi:10.1111/j.1442-2050.2006.00559.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.