Abstract
Patients with midgut neuroendocrine tumours or carcinoid syndrome often face a delayed diagnosis. This article aims to highlight the different ways in which patients with midgut neuroendocrine tumours (NETs) present, the diagnostic approach to them, the current methods of management available and future considerations.
Keywords: Cancer, Small Intestine Cancer, Diarrhoea, Liver Metastases
Introduction
Neuroendocrine tumours (NETs) are heterogeneous malignant transformations of cells of the diffuse neuroendocrine system, a collection of neuroendocrine cells scattered throughout the body, most commonly occurring in small intestine, pancreas, stomach and colorectum. Terminology can be confusing with tumours historically labelled as ‘carcinoid’ tumours, a term coined by Oberndorfer in 1907 to describe a ‘carcinoma-like’ tumour, which was considered to have less malignant potential than adenocarcinomas of the gut.1 However, the term carcinoid is nowadays limited to the syndrome associated with metastatic midgut (small intestinal) NETs.
NETs are uncommon neoplasms with an annual age-adjusted incidence of 5.25/100 000 compared with lung cancer, which is the second most common cancer in the UK (47.8/100 000) and colorectal cancer (46.6/100 000), the third most common cancer in the UK.2
The current gastroenterology curriculum (box 1) requires that UK trainees must understand the causes of (acute and) chronic diarrhoea and their management and recognise the importance of considering, and being able to identify, uncommon tumours, such as NETs that can arise from the pancreas or small intestine. Presentation can be at any age and the clinical manifestations between each patient can vary enormously. The challenge, therefore, is to achieve a diagnosis based on the available clinical, biochemical, imaging and histological evidence. This article aims to guide the reader through the initial diagnostic considerations in the approach to a patient with a NET, outlining the key tumour markers and imaging techniques and highlighting the subsequent implications in management of patients.
Box 1. Gastroenterology Curriculum 2010 Competency.
2c Intestinal disorders: abdominal pain/diarrhoea.
Understands the causes of acute and chronic diarrhoea and their management.
Understands the biochemical processes occurring within the gut lumen and at mucosal level.
Has awareness of the factors controlling these processes—in particular, the neuroendocrine influences.
Knows the range of investigations appropriate to determining the cause of the patient's diarrhoea and is aware of the range of therapeutic possibilities.
Makes a detailed clinical assessment of patients that present with either acute or chronic diarrhoea.
Shows ability to interpret results, reach a diagnosis and formulate a treatment plan.
How do patients present
NETs are characterised by a susceptibility to produce a variety of hormones, peptides and vasoactive substances, so patients can present in a number of ways. Williams and Sandler classified NETs based on their embryonic origin into
foregut (bronchial, gastric, duodenal, pancreatic)
midgut (ileal, jejunal, caecal)
hindgut (distal colonic, rectal).3
In this article, we will be concentrating on midgut NETs, which are associated with the classical carcinoid syndrome. This article does not focus on pancreatic and duodenal NETs that can either be non-functioning or can secrete one of a number of hormones producing rare syndromes, for example, gastrinoma, somatostatinoma and VIPoma causing diarrhoea and insulinoma, which can cause recurrent hypoglycaemia.
Patients with midgut NETs can develop symptoms from
primary effects of the tumour
enlarging metastases
secretion of hormones.
The most common presenting symptom in midgut NETs is intermittent crampy abdominal pain.4 This can be due to the mechanical effect of the intraluminal tumour or due to secondary desmoplastic reaction from mesenteric lymph node involvement. Desmoplasia results in tethering and kinking of the small bowel, which may lead to bowel obstruction (manifesting as abdominal pain, nausea and vomiting) or mesenteric ischaemia.
Even small midgut NETs can metastasise and the most common distant metastatic sites are liver, mesentery and peritoneum. Liver metastases can cause derangement in liver function tests and if large, can cause right upper quadrant abdominal pain from liver capsule stretch.
The classical carcinoid syndrome was first described by Thorson et al5 in 1954 who linked metastatic tumour of the small intestine with a collection of unusual signs and symptoms including bronchospasm (25%), diarrhoea (80%), flushing (80%) and right-sided valvular heart disease (10%–30%). Flushing usually involves the face, neck and chest, and may be brought on by alcohol, exercise, stress and certain trigger foods.
Serotonin (or 5-hydroxytryptamine) is the principal hormone responsible for the carcinoid syndrome. Derived from the amino acid tryptophan, it is enzymatically inactivated in the liver into 5-hydroxyindoleacetic acid (5-HIAA), a urinary metabolite that can be measured clinically. Therefore, the carcinoid syndrome occurs primarily in patients with liver (or lung) metastases from a midgut primary that secretes serotonin directly into the systemic circulation.
In addition to serotonin, there are other vasoactive substances, such as prostaglandins, histamines and tachykinins (kallikrein and substance P), that also contribute to the development of carcinoid syndrome.6 Significant releases of such vasoactive substances during surgery can precipitate a ‘carcinoid crisis’, which is characterised by severe hypotension. Administration of somatostatin analogues presurgery can reduce the risk of such occurrences and intraoperatively can treat the crisis.7
Carcinoid heart disease typically occurs in patients with chronically elevated levels of circulating serotonin from liver metastases.8 Direct exposure of serotonin to the right side of the heart causes deposition of fibrotic tissue on right-sided heart valves, leading to tricuspid regurgitation and pulmonary stenosis. The European Neuroendocrine Tumour Society (ENETS) guidelines advocate that echocardiograms should be performed on all patients with carcinoid syndrome but measuring n-terminal proBNP (brain natriuretic peptide) can also be helpful in screening for carcinoid heart disease.9
Classification
The classification of NETs has evolved considerably over the years to reflect the fact that NETs are heterogeneous in terms of tumour biology. In 2007, the ENETS published guidelines that incorporated the prognostic stratification of gastroenteropancreatic neuroendocrine tumours (GEP-NETs) to allow a better stage-adjusted treatment of the patients based on tumour-node-metastasis classification and grade.10 11
The WHO Classification of GEP-NETs was also updated in 2010 to separate well-differentiated tumours into low grade (G1) or intermediate grade (G2) depending on proliferative rate (mitotic count or Ki-67 proliferation index) and distinguishes them from poorly differentiated/high grade (G3) neuroendocrine carcinomas (table 1).12 These categories have prognostic value, but there is debate as to the degree of agreement between mitotic count, Ki-67 index and differentiation.13 Compared with pancreatic NETs, the majority of midgut NETs are low grade as opposed to intermediate or high grade.
Table 1.
WHO classification of gastroenteropancreatic neuroendocrine tumours 2010
| Differentiation | Grade | Criteria |
|---|---|---|
| Well differentiated | Low | <2 mitoses/10 HPF and ≤2% Ki-67 index |
| Intermediate | 2–20 mitoses/10 HPF or 3%–20% Ki-67 index | |
| Poorly differentiated | High | >20 mitoses/10 HPF or >20% Ki-67 index |
HPF, high power field.
Investigation
There are a number of different types of investigation involved in the diagnostic approach to a patient with a (midgut) NET.
Biochemical markers
Twenty-four-hour urinary 5-HIAA is specific for serotonin-producing NETs and is, therefore, useful in midgut NETs with a sensitivity of 70%–73% and specificity of 79%–98%.11 It is usually collected in a bottle containing glacial acetic acid, which acts as a preservative. False positives can be seen in patients with malabsorption syndromes, for example, coeliac disease or who have eaten tryptophan-rich foods like avocados and kiwis. Thus, a strict diet is required to be adhered to when evaluating 5-HIAA.14
Chromogranin A (CgA) does not rely on serotonin secretion so is a more sensitive and broadly applicable tumour marker for NETs than urinary 5HIAA, but it is less specific. Increases in CgA in patients with metastatic NETs have been shown to correlate with shorter survival.15 CgA should be used with caution as a diagnostic marker in patients with renal failure, liver cirrhosis, hyperthyroidism, hyperparathyroidism, inflammatory bowel disease and in those taking proton pump inhibitors as CgA levels can be raised in these situations. It is recommended that patients fast for the blood test as levels may fluctuate with meals. There are no significant differences in measuring plasma or serum levels although there are different assays, so normal ranges may vary when comparing results.
Cross-sectional imaging
Triple-phase CT and MRI are able to reveal the primary and metastatic lesions in 30%–70% and >90% of NETs, respectively. CT is useful for identifying small bowel NETs that are located at the root of the mesentery and exhibit a characteristic circumferential pattern of desmoplastic fibrosis. MRI has a high sensitivity for detecting liver metastases.
Molecular imaging
Molecular imaging has become extremely useful in the assessment of malignant tumours. Indium-111-diethylentriamine penta-acetic acid-octreotide (OctreoScan), which is based on the expression of somatostatin receptors (SSTR), especially subtypes 2 and 5, in 70%–90% of GEP-NETs, is often still the first choice with an overall sensitivity of approximately 80%–90%.16 More recently, labelling of positron emission tomography (PET) isotopes, such as 68Ga, to somatostatin analogues has led to the development of 68Ga-DOTATOC and 68Ga-DOTATATE PET scans. 68Ga-labelled somatostatin analogues have several advantages compared with OctreoScan. These include shorter imaging time (2 vs24–48 h), reduced radiation dose (0.0167 lmSv/MBq 0.054 mSv/MBq), higher affinity of DOTA-peptides to SSR-2 and better sensitivity and resolution of PET cameras. The latter two advantages seem to result in the identification of additional tumour lesions. The more commonly used 2-fluoro-2-deoxy-D-glucose-PET is more sensitive in NETs or other cancers with higher proliferation index so can be used in combination with 68Ga-labelled somatostatin analogues to distinguish synchronous cancers.17
Endoscopy
Upper and lower gastrointestinal endoscopy remain useful adjuncts for the diagnosis of NETs. Colonoscopy has been credited with early detection of rectal NETs leading to improved survival rates as it allows visualisation, sampling and, potentially, treatment of the lesion. Video capsule endoscopy can be a useful diagnostic modality with a diagnostic yield of 45% for identification of primary small bowel NETs.18 Double balloon enteroscopy allows localisation, tissue sampling and possible treatment of mid small bowel lesions. Endoscopic ultrasound provides a useful adjunct to CT/MRI in staging NETs and for examining extraluminal structures, particularly the pancreas.
Treatment options
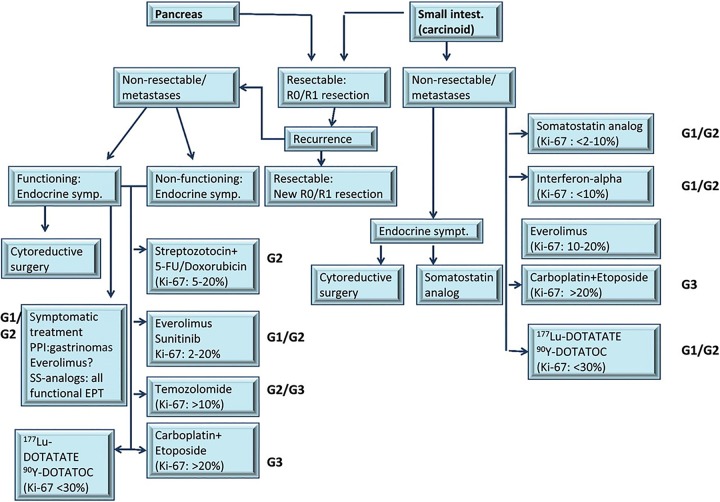
The UK and Ireland Neuroendocrine Tumour Society and British Society of Gastroenterology recommend that multidisciplinary teams (MDTs) at referral centres should give guidance on the definitive management of patients with all varieties of NETs (figure 1).14
Figure 1.
Algorithm for the treatment of neuroendocrine tumour (NETs) taken from European Society for Medical Oncology guidelines.30
Local options in controlling tumour growth
Surgical measures:
Resection of liver metastases can be considered in the absence of diffuse bilobar involvement, compromised liver function or extrahepatic metastases but the majority recur.
Resection of the primary in small bowel NETs can be considered where they are associated with desmoplasia and intermittent bowel obstruction.
Liver transplantation has been attempted in small series of patients with metastatic disease confined to the liver but the majority have recurrent disease.
Valve replacement for patients with symptomatic carcinoid heart disease is beneficial but associated with relatively high perioperative morbidity.
Preoperative administration of octreotide can reduce the risk of carcinoid crisis and is definitely recommended for patients with a history of carcinoid syndrome needing surgical procedures.
Non-surgical liver-directed measures:
Hepatic artery embolisation works on the principle that hepatic tumours derive most of their blood supply from the hepatic artery, whereas healthy hepatocytes derive most of their blood supply from the portal vein. It involves the infusion of microparticles into the hepatic artery through an angiography catheter (transarterial embolisation) or in conjunction with chemotherapy (transarterial chemoembolisation) and prolongs survival in biochemically responsive patients.19
Radiofrequency ablation, either percutaneously or laparoscopically, can be considered in patients with small liver metastases.
Systemic therapies for controlling symptoms and tumour growth
Somatostatin analogues such as octreotide are highly effective in controlling the symptoms associated with midgut NETs, VIPomas and glucagonomas. Monthly long-acting injections of octreotide LAR or lanreotide autogel are typically started after a brief trial of short-acting octreotide, with gradual dose escalation to optimise symptom control. Patients can use additional short-acting octreotide for breakthrough symptoms. The therapeutic levels of long-acting somatostatin analogues are not reached until 10–14 days after initiation so patients can sometimes be on short-acting octreotide during this interim period. Side effects occur in one-third of patients—nausea, abdominal discomfort, bloating, diarrhoea and fat malabsorption during the first weeks of therapy, after which time, symptoms tend to subside. Use of pancreatic enzyme supplements, like Creon, can ameliorate symptoms associated with pancreatic insufficiency. The PROMID trial, which involved 85 patients with locally inoperable or metastatic midgut NETs randomly assigned to receive treatment with either octreotide or placebo, showed that the median time to tumour progression was significantly longer with octreotide compared with placebo (14.3 vs 6 months) suggesting an antitumour effect.20 Therefore, patients who do not have carcinoid syndrome but who have octreotide-avid disease (as determined by somatostatin receptor scintigraphy) may also benefit from somatostatin analogues. The CLARINET study involved 204 patients with metastatic or locally advanced inoperable sporadic non-functioning gastroenteropancreatic NETs (approximately 45% pancreas, 35% midgut) who were randomised to receive lanreotide at 120 mg or placebo every 4 weeks for 96 weeks or until progression or death. The study met its primary endpoint, significantly improving progression-free survival at 2 years from 33% with placebo to 65% with lanreotide.21
Peptide receptor radionuclide therapy (PRRT) is considered in patients with inoperable metastatic NET who have octreotide-avid disease on molecular imaging and have progressed despite somatostatin analogues. This involves the injection of radiopeptides—made from a combination of octreotide with a radionuclide such as indium 111 (111In), yttrium 90 (90Y) 22 or lutetium 177 (177Lu)—that will bind to NET cells that exhibit SSTR and emit radiation to kill them. After the initial cycle, patients who show symptomatic improvement and tumour stabilisation/regression can have further cycles of treatment (renal function permitting). The median progression-free survival is more than 40 months with PRRT.23 Long-term side effects include renal impairment and pancytopenia.
Interferon α (IFN-α), either alone or in combination with somatostatin analogues, has been shown to reduce the effects of hormonal hypersecretion and induce tumour stabilisation,24 but its side effect profile (fatigue, depression, myelosuppression and alteration of thyroid function) has limited its more widespread acceptance as a treatment of metastatic NETs.
Molecular targeted agents, such as everolimus (mammalian target of rapamycin inhibitor) and sunitinib (tyrosine kinase inhibitor), can be considered in patients with progressing advanced pancreatic NET. In contrast to pancreatic NETs, the benefit of molecularly targeted therapy for midgut tumours is less well established although the RADIANT 2 trial demonstrated everolimus plus octreotide LAR, compared with placebo plus octreotide LAR, improved progression-free survival in patients with advanced NETs associated with carcinoid syndrome.25
Compared with pancreatic NETs, there is less of a role for chemotherapy in midgut NETs. However, two options are a streptozocin-based combination or a temozolomide-containing regimen in patients with intermediate or higher grade tumours where other therapies have failed or are contraindicated.26 For patients with poorly differentiated NETs, systemic chemotherapy with a platinum-based combination regimen (analogous to that used for small cell lung cancer) is recommended.
Future considerations
There are numerous treatment modalities available for patients with midgut NETs and most are expensive but with an expanding evidence base. It is hoped that the future will bring more randomised controlled trials directly comparing different treatments so management algorithms can be streamlined. There are currently trials looking into 177Lu-DOTA0-Tyr3-Octreotate plus best supportive care (30 mg octreotide LAR) compared with treatment with high-dose (60 mg) octreotide LAR in patients with inoperable, somatostatin receptor positive, histologically proven midgut carcinoid tumours in the UK. Telotristat etiprate has been shown in phase II trials to be well tolerated and effective in reducing bowel movements and serotonin production and improving patients’ symptoms with results of an international phase III trial awaited.27 Following on from its promise in treating pancreatic NETs, there are trials looking into the use of everolimus and sunitinib in midgut NETs.28 29 Also, more studies comparing the different radiopeptides in PRRT will help to define the most appropriate diagnostic imaging modality for patients with NETs.
Conclusion
Although midgut NETs are uncommon, the incidence and prevalence of NETs are increasing. They can, but do not necessarily always, present with carcinoid syndrome symptoms. Diagnosis depends on a combination of biochemical testing and appropriate cross-sectional/molecular imaging. Owing to the rarity of NETs, not all clinicians and local hospitals will have the full expertise to deal with patients with NETs. Therefore, it is paramount that all NET cases are discussed and managed by an MDT or a regional cancer network group that includes gastroenterologists, endocrinologists, oncologists, surgeons, radiologists, nuclear medicine specialists and pathologists.
Footnotes
Contributors: VTFC conceived the article, performed a literature review, manuscript writing and final approval of manuscript. MSK conceived the article, manuscript writing and final approval of manuscript.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Oberndorfer S. Karzinoide tumoren des dünndarms. Frankf Z Pathol 1907;1:426–32. [Google Scholar]
- 2.Cancer Research UK, UK Cancer Incidence (2010) by Country Summary, December 2012.
- 3.Williams ED, Sandler M. The classification of carcinoid tumours. Lancet 1963;1:238–9. [DOI] [PubMed] [Google Scholar]
- 4.Kulke MH, Mayer RJ. Carcinoid tumors. N Engl J Med 1999;340:858–68. [DOI] [PubMed] [Google Scholar]
- 5.Thorson A, Biorck G, Bjorkman G, et al. Malignant carcinoid of the small intestine with metastases to the liver, valvular disease of the right side of the heart (pulmonary stenosis and tricuspid regurgitation without septal defects), peripheral vasomotor symptoms, bronchoconstriction, and an unusual type of cyanosis; a clinical and pathologic syndrome. Am Heart J 1954;47:795–817. [DOI] [PubMed] [Google Scholar]
- 6.Vinik AI, Silva MP, Woltering EA, et al. Biochemical testing for neuroendocrine tumors. Pancreas 2009;38:876–89. [DOI] [PubMed] [Google Scholar]
- 7.Kvols LK, Martin JK, Marsh HM, et al. Rapid reversal of carcinoid crisis with a somatostatin analogue. N Engl J Med 1985;313:1229–30. [DOI] [PubMed] [Google Scholar]
- 8.Robiolio PA, Rigolin VH, Wilson JS, et al. Carcinoid heart disease. Correlation of high serotonin levels with valvular abnormalities detected by cardiac catheterization and echocardiography. Circulation 1995;92:790–5. [DOI] [PubMed] [Google Scholar]
- 9.Pape UF, Perren A, Niederle B, et al. ENETS Consensus Guidelines for the management of patients with neuroendocrine neoplasms from the jejuno-ileum and the appendix including goblet cell carcinomas. Neuroendocrinology 2012;95:135–56. [DOI] [PubMed] [Google Scholar]
- 10.Rindi G, Klöppel G, Ahlman H, et al. TNM staging of foregut (neuro)endocrine tumors: a consensus proposal including a grading system. Virchows Archiv 2006;449:395–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rindi G, Klöppel G, Couvelard A, et al. TNM staging of midgut and hindgut (neuro)endocrine tumors: a consensus proposal including a grading system. Virchows Archiv 2007;451:757–62. [DOI] [PubMed] [Google Scholar]
- 12.Klimstra DS, Modlin IR, Coppola D, et al. The pathologic classification of neuroendocrine tumors: a review of nomenclature, grading, and staging systems. Pancreas 2010;39:707–12. [DOI] [PubMed] [Google Scholar]
- 13.Khan MS, Luong TV, Watkins J, et al. A comparison of Ki-67 and mitotic count as prognostic markers for metastatic pancreatic and midgut neuroendocrine neoplasms. Br J Cancer 2013;108:1838–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ramage JK, Ahmed A, Ardill J, et al. Guidelines for the management of gastroenteropancreatic neuroendocrine (including carcinoid) tumours (NETs). Gut 2012;61:6–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khan MS, Caplin ME. The use of biomarkers in neuroendocrine tumours. Frontline Gastroenterology 2013;4:175–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kwekkeboom SJ, Krenning EP, Scheidhauer K, et al. ENETS consensus guidelines for the standards of care in neuroendocrine tumors: somatostatin receptor imaging with 111In-pentetreotide. Neuroendocrinology 2009;90:184–9. [DOI] [PubMed] [Google Scholar]
- 17.Kayani I, Bomanji JB, Groves A, et al. Functional imaging of neuroendocrine tumors with combined PET/CT using68Ga-DOTATATE (DOTA-DPhe1, Tyr3-octreotate) and18F-FDG. Cancer 2008;112:2447–55. [DOI] [PubMed] [Google Scholar]
- 18.van Tuyl SA, van Noorden JT, Timmer R, et al. Detection of small-bowel neuroendocrine tumors by video capsule endoscopy. Gastrointest Endosc 2006;64:66–72. [DOI] [PubMed] [Google Scholar]
- 19.Swärd C, Johanson V, Nieveen van Dijkum E, et al. Prolonged survival after hepatic artery embolization in patients with midgut carcinoid syndrome. Br J Surg 2009;96:517–21. [DOI] [PubMed] [Google Scholar]
- 20.Rinke A, Müller HH, Schade-Brittinger C, et al. ; PROMID Study Group. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J Clin Oncol 2009;27:4656–63. [DOI] [PubMed] [Google Scholar]
- 21.Caplin ME, Pavel M, Ćwikła J, et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med 2014;371:224–33. [DOI] [PubMed] [Google Scholar]
- 22.Imhof A, Brunner P, Marincek N, et al. Response, survival, and long-term toxicity after therapy with the radiolabeled somatostatin analogue [90Y-DOTA]-TOC in metastasized neuroendocrine cancers. J Clin Oncol 2011;29:2416. [DOI] [PubMed] [Google Scholar]
- 23.Kam BL, Teunissen JJ, Krenning EP, et al. Lutetium-labelled peptides for therapy of neuroendocrine tumours. Eur J Nucl Med Mol Imaging 2012;39(Suppl 1):S103–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Faiss S, Pape UF, Böhmig M, et al. ; International Lanreotide and Interferon Alfa Study Group. Prospective, randomized, multicenter trial on the antiproliferative effect of lanreotide, interferon alfa, and their combination for therapy of metastatic neuroendocrine gastroenteropancreatic tumors—the International Lanreotide and Interferon Alfa Study Group. J Clin Oncol 2003;21:2689. [DOI] [PubMed] [Google Scholar]
- 25.Pavel ME, Hainsworth JD, Baudin E, et al. ; RADIANT-2 Study Group. Everolimus plus octreotide long-acting repeatable for the treatment of advanced neuroendocrine tumours associated with carcinoid syndrome (RADIANT-2): a randomised, placebo-controlled, phase 3 study. Lancet 2011;378:2005. [DOI] [PubMed] [Google Scholar]
- 26.Turner NC, Strauss SJ, Sarker D, et al. Chemotherapy with 5-fluorouracil, cisplatin and streptozocin for neuroendocrine tumours. Br J Cancer 2010;102:1106–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kulke MH, O'Dorisio T, Phan A, et al. Telotristat etiprate in carcinoid syndrome not adequately controlled by octreotide. Endocr Relat Cancer Published Online First: 10 Jul 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Raymond E, Dahan L, Raoul J, et al. Sunitinib malate for the treatment of pancreatic neuroendocrine tumors. N Engl J Med 2011;364:501–13. [DOI] [PubMed] [Google Scholar]
- 29.Yao J, Shah M, Ito T, et al. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med 2011;364:514–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Öberg K, Knigge U, Kwekkeboom D, et al. Neuroendocrine gastroenteropancreatic tumours: ESMO clinical practice guidelines. Ann Oncol 2012;23(Suppl 7):vii124– 30. [DOI] [PubMed] [Google Scholar]