This population-based study followed 134 hospitals over 7 years to examine the evolution in the diagnosis and treatment patterns of PDA.
Abstract
OBJECTIVE:
To examine yearly trends of patent ductus arteriosus (PDA) diagnosis and treatment in very low birth weight infants.
METHODS:
In this retrospective cohort study of very low birth weight infants (<1500 g) between 2008 and 2014 across 134 California hospitals, we evaluated PDA diagnosis and treatment by year of birth. Infants were either inborn or transferred in within 2 days after delivery and had no congenital abnormalities. Intervention levels for treatment administered to achieve ductal closure were categorized as none, pharmacologic (indomethacin or ibuprofen), both pharmacologic intervention and surgical ligation, or ligation only. Multivariable logistic regression was used to assess risk factors for PDA diagnosis and treatment.
RESULTS:
PDA was diagnosed in 42.8% (12 002/28 025) of infants, with a decrease in incidence from 49.2% of 4205 infants born in 2008 to 38.5% of 4001 infants born in 2014. Pharmacologic and/or surgical treatment was given to 30.5% of patients. Between 2008 and 2014, the annual rate of infants who received pharmacologic intervention (30.5% vs 15.7%) or both pharmacologic intervention and surgical ligation (6.9% vs 2.9%) decreased whereas infants who were not treated (60.5% vs 78.3%) or received primary ligation (2.2% vs 3.0%) increased.
CONCLUSIONS:
There is an increasing trend toward not treating patients diagnosed with PDA compared with more intensive treatments: pharmacologic intervention or both pharmacologic intervention and surgical ligation. Possible directions for future study include the impact of these trends on hospital-based and long-term outcomes.
What’s Known on This Subject:
Optimal hospital management of patent ductus arteriosus for preterm infants still remains uncertain despite several decades of research.
What This Study Adds:
In this large, population-based cohort, there has been a recent dramatic decrease in both pharmacologic and surgical treatment of patent ductus arteriosus.
Patent ductus arteriosus (PDA) is associated with serious morbidities, such as necrotizing enterocolitis, intraventricular hemorrhage, bronchopulmonary dysplasia, as well as mortality in preterm infants.1–4 Pharmacologic intervention, either indomethacin or ibuprofen, is commonly administered to attempt to close the ductus.5,6 Surgical ligation is usually reserved for critically ill patients requiring extensive respiratory support when medical treatment has failed or was contraindicated.5,7,8 However, in observational studies, these interventions have also been associated with an increased risk of morbidities, including bronchopulmonary dysplasia and neurodevelopmental impairment.9–13
PDA management falls on a spectrum ranging between what might be considered conservative to more intensive management. Conservative management often includes no pharmacologic intervention and relies on time and strategies to allow the ductus to close spontaneously. More intensive treatments include pharmacologic intervention, both pharmacologic intervention followed by surgical ligation if the ductus remains patent, or primary surgical ligation.
Although pharmacologic and surgical interventions have been used for several decades,14,15 recent studies show wide variation in hospital practices.6,16 This variation is likely due to uncertainty about the natural history of PDA, lack of clear evidence of a causal relationship between PDA severity and adverse outcomes to guide management, as well as reports of adverse short- and long-term effects from treatment.8,10,11,13,17–24 Fueling this uncertainty is that the PDA can spontaneously close without treatment in most premature infants, even after discharge.25–27 Furthermore, newer studies report that there is no association between mortality and conservative PDA management.28,29
This study was designed to identify potential shifts in practices over the past decade, a time of increasing uncertainty about optimal PDA management. Characterizing practice patterns provides a foundation for assessing relationships between therapies and their long-term health impacts, as well as targeting areas for quality improvement initiatives.
Methods
Design
In this retrospective cohort study, we used clinical admissions and discharge data from 104 404 live-birth infants born between January 1, 2008 and December 31, 2014 that were prospectively collected from hospitals in the California Perinatal Quality Care Collaborative (CPQCC), a consortium of >90% of the NICUs throughout California.30 CPQCC collects clinical data in a prospective fashion for infants born at 136 member hospitals by using the standard definitions developed by the Vermont Oxford Network.31
Sample
Although CPQCC currently collects data on 136 member hospitals, our study included between 127 hospitals in 2008 and 134 hospitals in 2014 that had eligible patients over the study period. We included infants with birth weights of <1500 g who were either inborn or outborn and transferred to a CPQCC NICU within 2 days of delivery. We excluded infants who died in the delivery room and had major congenital abnormalities.
Data
Because some patients were cared for in >1 CPQCC hospital, we combined multiple records of a single patient to obtain their PDA diagnosis and cumulative treatment data. This strategy allowed us to follow a patient’s course across several sites of care until the initial discharge from the hospital.
Primary Outcomes
Definition of PDA
For the primary outcome of PDA diagnosis, we classified patients with a PDA diagnosis as “yes/no” if they had PDA by CPQCC definition, if they received indomethacin or ibuprofen treatment of PDA, or if they had PDA ligation. Between 2008 and 2010, CPQCC and the Vermont Oxford Network defined a PDA diagnosis as either having echocardiogram evidence of PDA with documentation of left to right ductal shunting, or the presence of at least 1 of the following: (1) left to right PDA shunt documented by continuous murmur, (2) hyperdynamic precordium, (3) bounding pulses, (4) wide pulse pressure, (5) congestive heart failure, (6) increase in pulmonary vasculature or cardiomegaly by chest radiograph, or (7) increase in oxygen requirement. In 2011, the Vermont Oxford Network (and CPQCC) revised its definition of PDA diagnosis into 2 tiers: either a left to right shunt or a bidirectional ductal shunt on Doppler echo or a systolic or continuous murmur in addition to ≥2 of the following: (1) hyperdynamic precordium, (2) bounding pulses, (3) wide pulse pressure, or (4) pulmonary vascular congestion, cardiomegaly, or both. In 2012, CPQCC applied a different definition of PDA to include patients who received treatment for PDA or who were diagnosed with PDA via echocardiographic or clinical diagnosis.
Treatment Levels for PDA
We categorized infants with a PDA diagnosis into 4 distinct groups based on the level of treatment intervention: (1) no intervention: if there was no record of receiving either pharmacologic treatment (indomethacin or ibuprofen) or surgical ligation, patients were categorized into this least intensive treatment group; (2) pharmacologic intervention: patients receiving indomethacin or ibuprofen to either prevent or treat PDA were included in the second treatment group; (3) pharmacologic and surgical intervention: if a hospital administered a pharmacologic treatment and then ligated, patients were included in the third group; and (4) surgical ligation without pharmacologic therapy, which was classified as the most intensive treatment group. Infants may have received treatment without confirming ductal significance on echocardiography.
Covariates
We were interested in the following maternal and neonatal characteristics: birth weight, gestational age (GA), small for GA (birth weight ≤10th percentile), multiple gestation, Apgar score at 5 minutes, race/ethnicity, sex, admission status (inborn or outborn), received prenatal care, mode of delivery, surfactant administration, and either had or did not have respiratory distress syndrome.
Statistical Analysis
We used the two-tailed t test and χ2 test to compare differences between groups of patients with and without a PDA diagnosis as well as patients with and without a treated PDA on the maternal and neonatal clinical factors listed above. Annual diagnosis and treatment trends were tested by using the Cochran-Armitage trend test. Adjusted odds ratios (OR) and 95% confidence intervals (CI) were estimated for each risk factor. We divided infants into 2 birth weight groups, (1) infants weighing 1000 to 1499 g at birth and (2) infants born with an extremely low birth weight (<1000 g), to assess independent risk factors and compare whether treatment intervention levels varied over time stratified by birth weight group.
Multivariable logistic regression analysis using backward elimination with an exit criterion of P < .05 was used to assess the independent risk factors listed above in addition to birth year for the group with PDA versus the group without. Similarly, we examined the same risk factors between the group receiving treatment for PDA versus the group not receiving treatment in our second model. We conducted the same analyses stratified by time period to see if there were differences in risk factors between the periods when PDA diagnostic criteria differed, 2008 to 2010 and 2012 to 2014.
The Stanford Institutional Review Board reviewed this study. Statistical analyses were conducted by using SAS version 9.3 (SAS Institute, Inc, Cary, NC).
Results
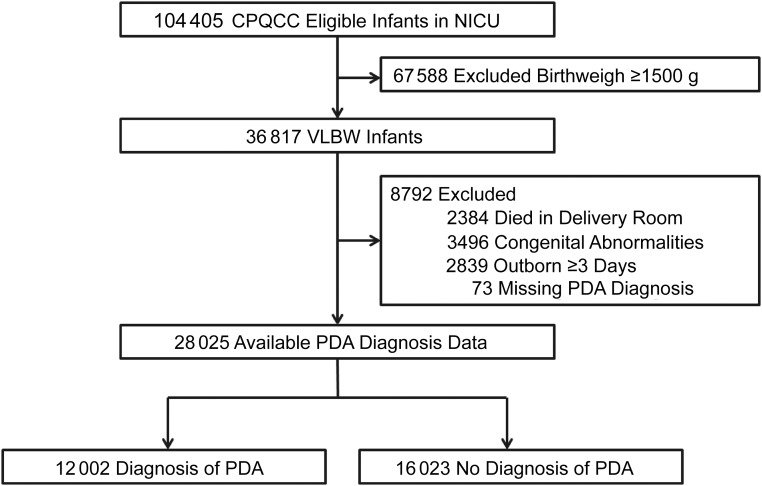
This study included 36 817 very low birth weight (VLBW) infants cared for by 134 CPQCC hospitals over the 7-year study period. After excluding patients who died in the delivery room, had congenital abnormalities, were not transferred within 2 days, or who had missing PDA diagnosis data (Fig 1), 28 025 VLBW infants remained; 42.8% (12 002/28 025) of infants were diagnosed with PDA and 57.2% (16 023/28 025) did not receive a diagnosis. Treatment for PDA, which includes either pharmacologic intervention, surgical ligation, or both, was given to 30.5% of patients.
FIGURE 1.
Flowchart of study population across 134 California hospitals, 2008 to 2014.
Diagnosis Trends
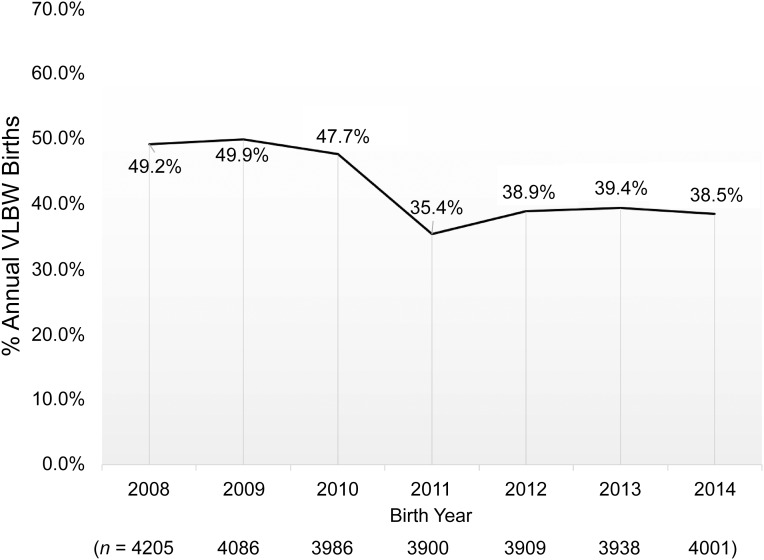
Approximately half of the 4205 VLBW infants born in 2008 were diagnosed with PDA (Fig 2). Although the number of VLBW infants born each year has remained relatively stable in the study population, the rate of infants receiving a PDA diagnosis decreased over the study period, beginning from 49.2% in 2008 to 38.5% in 2014 (Cochran-Armitage trend test Z = 15.08, P < .0001). Infants were more likely to receive a diagnosis if they had the following clinical characteristics: a lower GA, Apgar score at 5 minutes <7, respiratory distress syndrome, or if they received surfactant. They were also more likely to be extremely low birth weight (<1000 g), normal for GA, Hispanic, a boy, outborn, and delivered vaginally (Table 1).
FIGURE 2.
Incidence of PDA in VLBW infants (<1500 g) across 134 California hospitals, 2008 to 2014 (N = 28 025).
TABLE 1.
Clinical Characteristics of VLBW infants (<1500 g) With and Without a PDA Diagnosis in 134 California Hospitals, 2008 to 2014 (N = 28 025)
| Risk Factor | PDA Diagnosis (n = 12 002) | No PDA Diagnosis (n = 16 023) | OR | 95% CI | P |
|---|---|---|---|---|---|
| GA (wk), mean (SD) | 26.7 (2.3) | 29.5 (2.7) | 2.82 | 2.76–2.88 | <.0001 |
| Birth weight, g | |||||
| 1000–1499 | 39.1% | 78.0% | 0.18 | 0.17–0.19 | <.0001 |
| <1000 | 60.9% | 22.1% | 5.50 | 5.22–5.79 | <.0001 |
| Small for GA | 14.1% | 38.9% | 0.26 | 0.24–0.27 | <.0001 |
| 5-min Apgar score | |||||
| 0–3 | 7.8% | 4.5% | 2.08 | 1.88–2.30 | <.0001 |
| 4–6 | 22.1% | 11.0% | 2.43 | 2.28–2.60 | <.0001 |
| 7–10 | 70.2% | 84.5% | Reference | Reference | Reference |
| Race | |||||
| Non-Hispanic white | 25.4% | 27.5% | 0.90 | 0.85–0.95 | <.0001 |
| African American | 13.2% | 14.2% | 0.92 | 0.86–0.99 | .02 |
| Hispanic | 47.3% | 43.1% | 1.18 | 1.13–1.24 | <.0001 |
| Native American | 0.3% | 0.3% | 1.16 | 0.75–1.78 | .52 |
| Asian American | 11.7% | 12.5% | 0.93 | 0.87–1.00 | .05 |
| Sex | |||||
| Boy | 53.1% | 50.3% | 1.12 | 1.07–1.17 | <.0001 |
| Admission status | |||||
| Outborn | 18.3% | 9.95% | 2.03 | 1.89–2.17 | <.0001 |
| Surfactant use | 82.8% | 40.3% | 7.14 | 6.75–7.56 | <.0001 |
| Respiratory distress syndrome | 87.4% | 54.9% | 5.73 | 5.38–6.10 | <.0001 |
| No prenatal care | 3.9% | 3.4% | 1.13 | 0.99–1.27 | .07 |
| Multiple gestation | 27.1% | 27.3% | 0.99 | 0.94–1.05 | .77 |
| Cesarean delivery | 72.9% | 75.0% | 0.90 | 0.85–0.95 | <.0001 |
The following independent risk factors derived from multivariable logistic regression were associated with higher odds of receiving a PDA diagnosis: Hispanic ethnicity (OR, 1.10; 95% CI, 1.03–1.18), Asian American race (OR, 1.19; 95% CI, 1.09–1.31), multiple gestation (OR, 1.20; 95% CI, 1.13–1.28), outborn (OR, 1.78; 95% CI, 1.64–1.93), and cesarean delivery (OR, 1.39; 95% CI, 1.30–1.48). Lower odds for receiving a PDA diagnosis were associated with older GA (OR, 0.64; 95% CI, 0.63–0.65 for 1-week GA increase), small for GA (OR, 0.88; 95% CI, 0.82–0.95), African American race (OR, 0.88; 95% CI, 0.80–0.96), no prenatal care (OR, 0.83; 95% CI, 0.71–0.97), and receiving an Apgar score at 5 minutes between 0 and 3 (OR, 0.58; 95% CI, 0.51–0.66). Infants born in 2014 were associated with decreased odds for receiving a diagnosis compared with those born in 2008 (OR, 0.57; 95% CI, 0.52–0.63).
Between the earlier epoch, 2008 to 2010, and the later epoch, 2012 to 2014, when PDA diagnostic criteria changed, the risk factors between infants receiving a PDA diagnosis and infants who did not remained relatively constant with the exception of race/ethnicity (Table 2). We found that Hispanic infants had higher odds of receiving a diagnosis compared with white infants in the later epoch (OR, 1.14; 95% CI, 1.03–1.27) compared with no association for race/ethnicity in receiving a diagnosis during the earlier epoch (OR, 1.04; 95% CI, 0.94–1.15). African American infants had lower odds of receiving a diagnosis during the earlier epoch compared with white infants (OR, 0.84; 95% CI, 0.73–0.97). We found no association in race/ethnicity for receiving a diagnosis during the later epoch (OR, 0.96; 95% CI, 0.83–1.11).
TABLE 2.
Independent Risk Factors of VLBW Infants (<1500 g) Diagnosed With PDA in 134 California Hospitals From Multivariable Logistic Regression, Stratified by PDA Definition Changes Between 2008 and 2014 (N = 28 025)
| Risk Factor | Received Diagnosis Using 2008–2010 PDA Definition (n = 12 277) | Received Diagnosis Using 2012-2014 PDA Definition (n = 11 848) | ||||
|---|---|---|---|---|---|---|
| Adjusted OR | 95% CI | P | Adjusted OR | 95% CI | P | |
| GA, wk | 0.64 | 0.62–0.65 | <.0001 | 0.64 | 0.62–0.65 | <.0001 |
| Small for GA | 0.86 | 0.77–0.96 | .009 | 0.86 | 0.76–0.97 | .01 |
| 5-min Apgar score | ||||||
| 0–3 | 0.54 | 0.45–0.65 | <.0001 | 0.56 | 0.46–0.67 | <.0001 |
| 4–6 | 1.02 | 0.90–1.15 | .81 | 1.12 | 1.00–1.26 | .06 |
| 7–10 | Reference | Reference | Reference | Reference | Reference | Reference |
| Race | ||||||
| Non-Hispanic white | Reference | Reference | Reference | Reference | Reference | Reference |
| African American | 0.84 | 0.73–0.97 | .02 | 0.96 | 0.83–1.11 | .59 |
| Hispanic | 1.04 | 0.94–1.15 | .44 | 1.14 | 1.03–1.27 | .01 |
| Native American | 1.58 | 0.73–3.43 | .25 | 1.05 | 0.48–2.31 | .91 |
| Asian American | 1.24 | 1.07–1.44 | .004 | 1.17 | 1.02–1.36 | .03 |
| Sex | ||||||
| Boy | 0.97 | 0.89–1.05 | .41 | 1.02 | 0.93–1.11 | .73 |
| Admission status | ||||||
| Outborn | 1.89 | 1.67–2.14 | <.0001 | 1.67 | 1.46–1.90 | <.0001 |
| No prenatal care | 0.88 | 0.69–1.10 | .27 | 0.82 | 0.66–1.02 | .08 |
| Multiple gestation | 1.21 | 1.10–1.34 | <.0001 | 1.19 | 1.07–1.31 | .001 |
| Cesarean delivery | 1.51 | 1.36–1.67 | <.0001 | 1.32 | 1.19–1.46 | <.0001 |
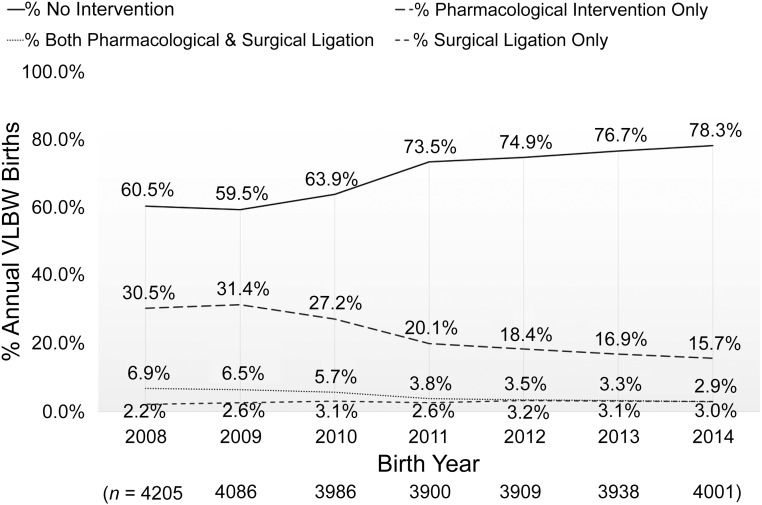
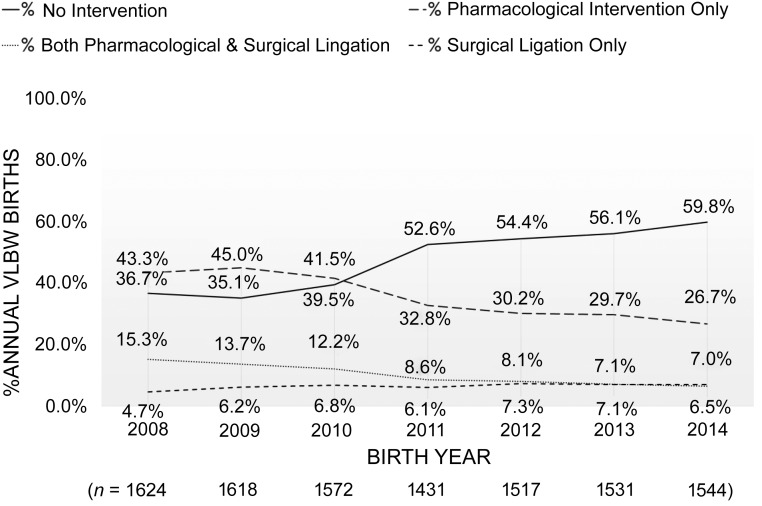
Treatment Trends
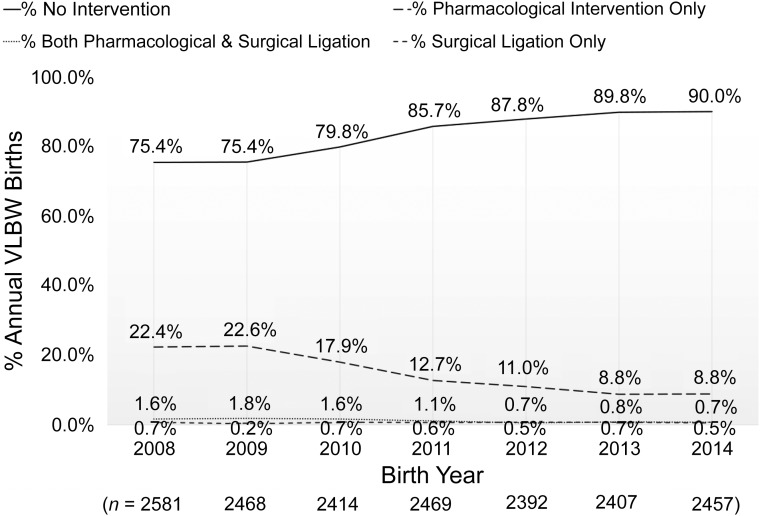
We observed considerable changes in PDA management between 2008 and 2014 for VLBW infants (Fig 3). The percentage of infants who did not receive treatment for PDA increased from 60.5% of VLBW infants in 2008 to 78.3% in 2014 (Cochran-Armitage trend test Z = 25.87, P < .0001). Over this period, the rate of infants who received pharmacologic intervention decreased from 30.5% to 15.7% of patients. The percentage of patients receiving both pharmacologic intervention and surgical ligation decreased from 6.9% to 2.9%, whereas the percentage of VLBW infants who underwent primary surgical ligation increased from 2.2% to 3.0%. We observed similar annual trends among infants weighing 1000 to 1499 g (Fig 4) as well as among extremely low birth weight infants weighing <1000 g (Fig 5).
FIGURE 3.
Hospital management of PDA in VLBW infants weighing <1500 g across 134 California hospitals, stratified by treatment intervention level, 2008 to 2014 (N = 28 025).
FIGURE 4.
Hospital management of PDA in VLBW infants weighing 1000 to 1499 g across 134 California hospitals, stratified by treatment intervention level, 2008 to 2014 (n = 17 188).
FIGURE 5.
Hospital management of PDA in extremely low birth weight infants weighing <1000 g across 134 California hospitals, stratified by treatment intervention level, 2008 to 2014 (n = 10 837). ELBW, extremely low birth weight infants.
Patients receiving a PDA diagnosis were more likely to receive treatment for PDA if they had lower GA, a lower Apgar score at 5 minutes <7, respiratory distress syndrome, and received surfactant. They were also more likely to be extremely low birth weight (<1000 g), normal for GA, Hispanic, a boy, outborn, and delivered vaginally. In logistic regression analysis, the independent risk factors associated with higher odds of receiving treatment were Asian American race (OR, 1.28; 95% CI, 1.15–1.41), multiple gestation (OR, 1.21; 95% CI, 1.13–1.30), outborn (OR, 1.48; 95% CI, 1.36–1.61), and cesarean delivery (OR, 1.40; 95% CI, 1.31–1.51). Lower odds for receiving treatment were older GA (OR, 0.63; 95% CI, 0.62–0.64 for 1-week GA increase), small for GA (OR, 0.86; 95% CI, 0.79–0.94), African American race (OR, 0.85; 95% CI, 0.77–0.93), no prenatal care (OR, 0.79; 95% CI, 0.68–0.93), and receiving an Apgar score at 5 minutes of 0 to 3 (OR, 0.56; 95% CI, 0.49–0.63). Similar to PDA diagnosis trends, the adjusted odds of infants receiving PDA treatment in 2014 compared with infants born in 2008 also decreased annually beginning in 2010, after risk adjustment (OR, 0.33; 95% CI, 0.29–0.37).
Discussion
Although there was a relatively stable diagnosis rate from 2008 to 2010, a steep decline from 2010 to 2011, a modest increase to 2012, and a stable rate between 2012 and 2014, we found that there was a net significant decrease in PDA diagnoses for VLBW infants across California over the past decade, as well as a decreasing trend in both pharmacologic and surgical intervention for PDA. Our risk-adjusted models comparing risk factors between infants receiving a PDA diagnosis or no diagnosis and between infants receiving treatment for PDA and infants not receiving treatment support the finding of a decrease in diagnosis and more intensive treatments over a similar period. Our findings show the most recent PDA diagnosis and treatment data trends available for a large population-based study.
The diagnostic criteria for PDA were revised during the last 3 years of this study. These changes may have influenced our finding of less intensive management over time. However, we found little difference in clinical characteristics between infants who received a diagnosis between 2008 and 2010 and those who received a diagnosis between 2012 and 2014. We speculate that 1 potential factor in the observed decrease in diagnosis was the deliberate decision on the part of practitioners to not actively look for PDA using echocardiograms. The decline in diagnosis may also be due to changes in the general trends in the management of the VLBW infant. These include changes in blood pressure treatments, management of fluids and nutrition, respiratory treatments in the delivery room, noninvasive ventilation, and delayed cord clamping. Changes in clinical practice may have influenced the rates of spontaneous closure of the ductus.
Our study supports a general decreasing trend in both PDA diagnosis and treatment patterns found across different types of NICUs. The rate of infants diagnosed with PDA over the 7-year period in our study (43%) is comparable to diagnosis rates across 20 Neonatal Research Network academic centers (46%) between 2003 to 2007.32 Between 2008 and 2014, the rate of patients treated for PDA, either pharmacologically or by surgical ligation, decreased. Although there was a trend toward less ligation, overall, there was an increase in primary ligation from 2.2% in 2008 to 3.0% to 3.2% during the later epoch. Because the tendency toward earlier pharmacologic intervention decreased over time, this trend may reflect cases in which treatment was deemed necessary, but too late for pharmacologic intervention. Previous studies of treatment trends in the Pediatrix Medical Group from 32 states (1997–2004) and regional tertiary-level NICUs in Canada (2004–2008) showed hospitals favored indomethacin over conservative treatment (none or fluid restriction and/or diuretics) and ligation.6,33 These studies were conducted before a review published in 2011 by Benitz,34 which concluded that randomized controlled trials and meta-analyses had not demonstrated long-term benefits of pharmacologic intervention or ligation including that of Schmidt et al.18 Despite mounting evidence of adverse outcomes from observational studies, there was no consensus on an improved alternative to existing therapies and lack of evidence to guide management. However, the prevailing prominence of the debate regarding the uncertainty of the benefit of therapy for the PDA may have affected clinical care. We also speculate that, because an infant could have been diagnosed and treated for PDA based on clinical signs alone, a potential reason for a reduction in treatment may be that clinicians began requiring echocardiography evaluation before making a diagnosis or administering treatment. Clinicians may have found that a significant proportion of PDAs were not hemodynamically significant.
An alternative method of analyzing treatment trends would have been to consider treatment rates for only those diagnosed with PDA. However, we were concerned with the overall burden of treatment on the whole population of VLBW infants, not just those diagnosed with PDA, considering that lower incidence in later years may have been partly due to ascertainment bias. We did perform similar analyses on only infants diagnosed with PDA and found similar results, including a decreasing trend in infants receiving pharmacologic intervention and both pharmacologic intervention and surgical ligation during the study period, as well as an increasing trend in infants not receiving a treatment or undergoing primary surgical ligation (data not shown).
Limitations of this study include external influences on clinicians’ management of PDA that were not accounted for in the study. These may include variation in hospital policies influencing PDA management practices during a given year. Therapies other than pharmacologic (indomethacin or ibuprofen) or surgical interventions were not captured during data collection and could have influenced treatment trends. Factors that may have contributed to changes in diagnosis rates include changes in the use of echocardiography for screening or prophylactic indomethacin. There may have been ascertainment bias because CPQCC does not collect data on echocardiography, and, therefore, true PDA diagnosis rates may be underestimated. We also lacked specific details on how PDA was diagnosed, unit policies on treatments for infants with a hemodynamically significant PDA, and whether indomethacin was used for prophylaxis.
Previous observational studies for pharmacological intervention and surgical ligation have shown associations with adverse effects, including bronchopulmonary dysplasia, severe retinopathy of prematurity, and neurosensory impairment.13 Some studies have shown that ligation has been associated with reduced mortality.10,11 However, long-term outcomes remain uncertain due to adverse effects from therapy, higher spontaneous closure rates, and smaller ductal shunts with milder symptoms.35,36 Previous therapy trials have included infants with negligible PDAs, so if risk stratification can be improved, we may be able to identify groups of patients who would benefit from therapy.
With PDA definition changes in 2011 and 2012, differential misclassification bias could have occurred during data extraction from medical records. One of the reasons why PDA diagnosis rates decreased beginning in 2011 may be due to the narrower criteria used to define PDA compared with those used between 2008 and 2010. However, when we evaluated risk factors in the 2 time periods, 2000 to 2010 and 2012 to 2014, the clinical risk factors in receiving a diagnosis remained relatively constant between the 2 periods (Table 2).
Conclusions
There has been a recent decrease in pharmacologic intervention and both pharmacologic intervention and surgical ligation for VLBW infants diagnosed with PDA. Longitudinal surveillance of treatment patterns across NICUs and their relation to clinical outcomes may provide insights into the physiology and pathophysiology of the ductus arteriosus in VLBW infants. We aim to tie our current study findings to long-term outcomes in the future through the CPQCC-California Children’s Services High Risk Infant Follow-up Quality of Care Initiative, which collects data on outcomes at 2 years of age for eligible patients.37
Glossary
- CI
confidence interval
- CPQCC
California Perinatal Quality Care Collaborative
- GA
gestational age
- OR
odds ratio
- PDA
patent ductus arteriosus
- VLBW
very low birth weight
Footnotes
Ms Ngo contributed to the study design, conducted the initial analyses, interpreted the results, and drafted the initial manuscript; Drs Gould and Profit contributed to the study conceptualization and study design, interpreted the results, and critically reviewed the manuscript; Dr Lee conceptualized the study design, designed and supervised the analysis, interpreted the results, and critically reviewed the manuscript; and all authors approved the manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported in part by Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health grant K23HD068400. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Schena F, Francescato G, Cappelleri A, et al. . Association between hemodynamically significant patent ductus arteriosus and bronchopulmonary dysplasia. J Pediatr. 2015;166(6):1488–1492 [DOI] [PubMed] [Google Scholar]
- 2.Noori S, McCoy M, Friedlich P, et al. . Failure of ductus arteriosus closure is associated with increased mortality in preterm infants. Pediatrics. 2009;123(1). Available at: www.pediatrics.org/cgi/content/full/123/1/e138 [DOI] [PubMed] [Google Scholar]
- 3.Dollberg S, Lusky A, Reichman B. Patent ductus arteriosus, indomethacin and necrotizing enterocolitis in very low birth weight infants: a population-based study. J Pediatr Gastroenterol Nutr. 2005;40(2):184–188 [DOI] [PubMed] [Google Scholar]
- 4.Marshall DD, Kotelchuck M, Young TE, Bose CL, Kruyer L, O’Shea TM; North Carolina Neonatologists Association . Risk factors for chronic lung disease in the surfactant era: a North Carolina population-based study of very low birth weight infants. Pediatrics. 1999;104(6):1345–1350 [DOI] [PubMed] [Google Scholar]
- 5.Jain A, Shah PS. Diagnosis, evaluation, and management of patent ductus arteriosus in preterm neonates. JAMA Pediatr. 2015;169(9):863–872 [DOI] [PubMed] [Google Scholar]
- 6.Laughon M, Bose C, Clark R. Treatment strategies to prevent or close a patent ductus arteriosus in preterm infants and outcomes. J Perinatol. 2007;27(3):164–170 [DOI] [PubMed] [Google Scholar]
- 7.Weisz DE, McNamara PJ. Patent ductus arteriosus ligation and adverse outcomes: causality or bias? J Clin Neonatol. 2014;3(2):67–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bose CL, Laughon MM. Patent ductus arteriosus: lack of evidence for common treatments. Arch Dis Child Fetal Neonatal Ed. 2007;92(6):F498–F502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clyman RI. Ibuprofen and patent ductus arteriosus. N Engl J Med. 2000;343(10):728–730 [DOI] [PubMed] [Google Scholar]
- 10.Weisz DE, More K, McNamara PJ, Shah PS. PDA ligation and health outcomes: a meta-analysis. Pediatrics. 2014;133(4). Available at: www.pediatrics.org/cgi/content/full/133/4/e1024 [DOI] [PubMed] [Google Scholar]
- 11.Madan JC, Kendrick D, Hagadorn JI, Frantz ID III; National Institute of Child Health and Human Development Neonatal Research Network . Patent ductus arteriosus therapy: impact on neonatal and 18-month outcome. Pediatrics. 2009;123(2):674–681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clyman R, Cassady G, Kirklin JK, Collins M, Philips JB III. The role of patent ductus arteriosus ligation in bronchopulmonary dysplasia: reexamining a randomized controlled trial. J Pediatr. 2009;154(6):873–876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kabra NS, Schmidt B, Roberts RS, Doyle LW, Papile L, Fanaroff A; Trial of Indomethacin Prophylaxis in Preterms (TIPP) Investigators . Neurosensory impairment after surgical closure of patent ductus arteriosus in extremely low birth weight infants: results from the Trial of Indomethacin Prophylaxis in Preterms. J Pediatr. 2007;150(3):229–234 [DOI] [PubMed] [Google Scholar]
- 14.Heymann MA, Rudolph AM, Silverman NH. Closure of the ductus arteriosus in premature infants by inhibition of prostaglandin synthesis. N Engl J Med. 1976;295(10):530–533 [DOI] [PubMed] [Google Scholar]
- 15.Edmunds LH Jr, Gregory GA, Heymann MA, Kitterman JA, Rudolph AM, Tooley WH. Surgical closure of the ductus arteriosus in premature infants. Circulation. 1973;48(4):856–863 [DOI] [PubMed] [Google Scholar]
- 16.Lee HC, Durand DJ, Danielsen B, Dueñas GV, Powers RJ. Hospital variation in medical and surgical treatment of patent ductus arteriosus. Am J Perinatol. 2015;32(4):379–386 [DOI] [PubMed] [Google Scholar]
- 17.Benitz WE; Committee on Fetus and Newborn, American Academy of Pediatrics . Patent ductus arteriosus in preterm infants. Pediatrics. 2016;137(1):e20153730 [DOI] [PubMed] [Google Scholar]
- 18.Schmidt B, Davis P, Moddemann D, et al. ; Trial of Indomethacin Prophylaxis in Preterms Investigators . Long-term effects of indomethacin prophylaxis in extremely-low-birth-weight infants. N Engl J Med. 2001;344(26):1966–1972 [DOI] [PubMed] [Google Scholar]
- 19.Mitra S, Rønnestad A, Holmstrøm H. Management of patent ductus arteriosus in preterm infants--where do we stand? Congenit Heart Dis. 2013;8(6):500–512 [DOI] [PubMed] [Google Scholar]
- 20.Schmidt B, Roberts RS, Fanaroff A, et al. ; TIPP Investigators . Indomethacin prophylaxis, patent ductus arteriosus, and the risk of bronchopulmonary dysplasia: further analyses from the Trial of Indomethacin Prophylaxis in Preterms (TIPP). J Pediatr. 2006;148(6):730–734 [DOI] [PubMed] [Google Scholar]
- 21.Malviya MN, Ohlsson A, Shah SS. Surgical versus medical treatment with cyclooxygenase inhibitors for symptomatic patent ductus arteriosus in preterm infants. Cochrane Database Syst Rev. 2013;(3):CD003951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hamrick SEG, Hansmann G. Patent ductus arteriosus of the preterm infant. Pediatrics. 2010;125(5):1020–1030 [DOI] [PubMed] [Google Scholar]
- 23.Mondal T, Chaudhuri D, Li B, Shivananda S, Dutta S. Prophylactic indomethacin worsens short-term respiratory outcomes in extremely low-birth-weight infants. Am J Perinatol. 2014;31(1):61–67 [DOI] [PubMed] [Google Scholar]
- 24.De Buyst J, Rakza T, Pennaforte T, Johansson A-B, Storme L. Hemodynamic effects of fluid restriction in preterm infants with significant patent ductus arteriosus. J Pediatr. 2012;161(3):404–408 [DOI] [PubMed] [Google Scholar]
- 25.Nemerofsky SL, Parravicini E, Bateman D, Kleinman C, Polin RA, Lorenz JM. The ductus arteriosus rarely requires treatment in infants > 1000 grams. Am J Perinatol. 2008;25(10):661–666 [DOI] [PubMed] [Google Scholar]
- 26.Herrman K, Bose C, Lewis K, Laughon M. Spontaneous closure of the patent ductus arteriosus in very low birth weight infants following discharge from the neonatal unit. Arch Dis Child Fetal Neonatal Ed. 2009;94(1):F48–F50 [DOI] [PubMed] [Google Scholar]
- 27.Rolland A, Shankar-Aguilera S, Diomandé D, Zupan-Simunek V, Boileau P. Natural evolution of patent ductus arteriosus in the extremely preterm infant. Arch Dis Child Fetal Neonatal Ed. 2014;100(1):F55–F58 [DOI] [PubMed] [Google Scholar]
- 28.Chock VY, Punn R, Oza A, et al. . Predictors of bronchopulmonary dysplasia or death in premature infants with a patent ductus arteriosus. Pediatr Res. 2014;75(4):570–575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kaempf JW, Wu YX, Kaempf AJ, Kaempf AM, Wang L, Grunkemeier G. What happens when the patent ductus arteriosus is treated less aggressively in very low birth weight infants? J Perinatol. 2012;32(5):344–348 [DOI] [PubMed] [Google Scholar]
- 30.Gould JB. The role of regional collaboratives: the California Perinatal Quality Care Collaborative model. Clin Perinatol. 2010;37(1):71–86 [DOI] [PubMed] [Google Scholar]
- 31.Horbar JD, Soll RF, Edwards WH. The Vermont Oxford Network: a community of practice. Clin Perinatol. 2010;37(1):29–47 [DOI] [PubMed] [Google Scholar]
- 32.Stoll BJ, Hansen NI, Bell EF, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network . Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126(3):443–456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mirea L, Sankaran K, Seshia M, et al. ; Canadian Neonatal Network . Treatment of patent ductus arteriosus and neonatal mortality/morbidities: adjustment for treatment selection bias. J Pediatr. 2012;161(4):689–694.e1 [DOI] [PubMed] [Google Scholar]
- 34.Benitz WE. Patent ductus arteriosus: to treat or not to treat? Arch Dis Child Fetal Neonatal Ed. 2012;97(2):F80–F82 [DOI] [PubMed] [Google Scholar]
- 35.Ohlsson A, Walia R, Shah SS. Ibuprofen for the treatment of patent ductus arteriosus in preterm or low birth weight (or both) infants. Cochrane Database Syst Rev. 2015;(2):CD003481. [DOI] [PubMed] [Google Scholar]
- 36.Weber SC, Weiss K, Bührer C, Hansmann G, Koehne P, Sallmon H. Natural history of patent ductus arteriosus in very low birth weight infants after discharge. J Pediatr. 2015;167(5):1149–1151 [DOI] [PubMed] [Google Scholar]
- 37.Hintz SR, Gould JB, Bennett MV, et al. . Referral of very low birth weight infants to high-risk follow-up at neonatal intensive care unit discharge varies widely across California. J Pediatr. 2015;166(2):289–295 [DOI] [PubMed] [Google Scholar]