Children with asthma who both have positive family relationships and live in high greenspace areas have the best asthma outcomes.
Abstract
BACKGROUND AND OBJECTIVES:
Both the social environment and the physical environment are increasingly recognized as important to childhood diseases such as asthma. This study tested a novel hypothesis: that living in areas high in greenspace may help buffer the effects of difficult family relationships for children with asthma.
METHODS:
A total of 150 children (ages 9–17), physician-diagnosed with asthma, participated in this study. To assess difficulties in parent-child relationships, parents and children completed measures of harsh/inconsistent parenting and parental hostility. Residential greenspace was calculated by using satellite-derived Normalized Difference Vegetation Index with a buffer of 250 m around the residential address. Outcomes included both clinical and biological measures: asthma control and functional limitations, as well as airway inflammation (fractional concentration of exhaled nitric oxide) and glucocorticoid receptor expression in T-helper cells.
RESULTS:
After controlling for potential confounding variables, including family income, child demographics, and child medical variables, few main effects were found. However, interactions between residential greenspace and difficult family relationships were found for asthma control (P = .02), asthma functional limitations (P = .04), airway inflammation (P = .007), and the abundance of glucocorticoid receptor in T-helper cells (P = .05). These interactions were all in a direction such that as the quality of parent-child relationships improved, greenspace became more strongly associated with better asthma outcomes.
CONCLUSIONS:
These findings suggest synergistic effects of positive environments across the physical and social domains. Children with asthma appear to benefit the most when they both live in high greenspace areas and have positive family relationships.
What’s Known on This Subject:
Previous research has documented detrimental effects of difficult family relationships on childhood asthma, but whether living in high greenspace areas can buffer these effects of difficult family relationships for children is not known.
What This Study Adds:
This study documents the importance of considering both the social environment and the physical environment for childhood asthma. For children with asthma to benefit from greenspaces, they may also need to have positive family relationships present.
Residential greenspace has been receiving increasing attention as beneficial to mental and physical health in children and adults.1–12 One reason why greenspace might benefit health is that it has relaxing, restorative properties that can mitigate experiences of stress.13,14 If true, one might expect greenspace’s effects to be particularly beneficial to those in highly stressful environments. For children, one particularly salient type of stressful environment may be difficult relationships with parents, such as one in which there is harsh and inconsistent parenting or in which children experience hostility from their parents. In the current study, we tested this hypothesis by investigating interactions between greenspace and difficult family relationships on children’s asthma.
There is some evidence that greenspace is associated with asthma outcomes,3,15–17 although findings are mixed.18–20 One reason for this may be that social factors, such as family relationship characteristics, affect this relationship (eg, by affecting how much time children can spend outside). There is a large amount of literature linking psychological stress to asthma,21,22 with negative family relationship characteristics (such as harsh parenting) being one important stressor that is correlated with childhood asthma onset and symptoms.23–25 However, we are not aware of any previous studies that have investigated whether family relationship difficulties might moderate the effects of greenspace on childhood asthma.
We tested associations with both clinical asthma indicators as well as with asthma-relevant biological markers. We assessed a noninvasive marker of airway inflammation: the fractional concentration of exhaled nitric oxide (FeNO). FeNO levels increase as asthma control deteriorates,26 and decrease when treatment reduces airway inflammation.27 In addition, we investigated the expression of glucocorticoid receptors (GR) in T-helper cells. Glucocorticoids are transduced through receptors located inside cells (eg, T-helper lymphocytes) which coordinate immune responses that underlie airway inflammation.28 Psychosocial stress is associated with a lower responsiveness of cells to glucocorticoid’s anti-inflammatory properties.29,30 Thus, a decreased abundance of GR in T-helper cells may dampen their ability to transduce cortisol’s anti-inflammatory signals, thereby facilitating airway inflammation.
Hence, the current study considers the joint contribution of social and physical environment characteristics in childhood asthma. We tested interactions between residential greenspace and difficult family relationships (harsh/inconsistent parenting behaviors and parental hostility) in predicting (1) clinical outcomes, including asthma control and asthma functional limitations; and (2) biological markers relevant to asthma, including airway inflammation and expression of GR protein in T-helper cells among a sample of children with asthma.
Methods
Study Participants
A total of 150 children ages 9 to 17, physician-diagnosed with asthma, were recruited from Chicago and outlying suburbs/cities through 1 health care system, NorthShore University Health System, and 1 federally qualified health center, Erie Family Health Center. Mailings were sent to families about the study (14% refused to participate). Children came to the research center between 2013 and 2014 with 1 parent (88% mothers). Families were required to be fluent in English (<1% were excluded for this reason), and children had to be free of acute respiratory illness at the time of the visit and have no other chronic physical illnesses other than asthma. Children gave written assent and parents provided written consent. This study was approved by the Northwestern, NorthShore, and Erie Institutional Review Boards (see Table 1).
TABLE 1.
Descriptive Information About the Sample (n = 150)
| Mean | SD | % | |
|---|---|---|---|
| Child age | 14.12 | 2.07 | |
| Sex, % male | 57 | ||
| Ethnicity, % white | 49 | ||
| Atopic status, % yes | 82 | ||
| Asthma severity | 2.40 | 1.00 | |
| β agonist | 1.36 | 1.97 | |
| Inhaled corticosteroid | 2.40 | 2.99 | |
| Residential greenspace | 0.20 | 0.04 | |
| Harsh/inconsistent parenting | 22.52 | 2.58 | |
| Perceived parent hostility | 21.81 | 5.38 | |
| Asthma control | 20.84 | 3.54 | |
| Asthma functional limitations | 6.27 | 1.25 | |
| FeNO, ppb | 41.19 | 34.92 | |
| T-helper cell GR expression | 62.68 | 17.26 |
β agonist and inhaled corticosteroid use refers to the number of days in the past week that medication has been taken. Asthma severity is rated on a 4-point scale (1–4). Greenspace ranges from −1 to 1. Harsh/inconsistent parenting ranges from 11 to 44. Parent hostility ranges from 14 to 56. Asthma control ranges from 5 to 25. Asthma functional limitations range from 1 to 7 (higher numbers indicate fewer limitations). T-helper cell GR expression refers to the mean fluorescence intensity of glucocorticoid receptors in T-helper cells.
Measures
Greenspace
We used the satellite-derived Normalized Difference Vegetation Index to assess a continuous measure of greenness across study regions. The Normalized Difference Vegetation Index ranges from −1 to 1 (where 1 indicates a fully green space) based on land surface reflectance of visible (red) and near infrared parts of spectrum.31 All images with less than 10% cloud cover from Landsat 8 Operational Land Imager and Thermal Infrared Sensor were downloaded from January 1, 2013 to November 1, 2014, for the Chicago region to obtain a minimum of 2 measurements per season. We used ESRI ArcGIS Desktop (Release 10.1, Esri, Redlands, CA) to process relevant maps (see Supplemental Information).
Average greenness values in each season were extracted for buffers of 250-m radii around each study participant’s home address, and then averaged across the year. We conceptualized both greenspace and family environments as exerting cumulative effects over time on asthma, and hence this measure provides an indicator of long-term greenness exposure, independent of the time of year in which children participated in the study. Measures of greenspace have been found to be stable over multiple years.17 The buffer area that was used is similar to that recommended by the World Health Organization,32 has been used in previous studies,12,33–35 corresponds to other assessments of residential greenness,36 and is thought to reflect greenness directly accessible to each home (∼5-minutes’ walking distance along walkable roads or pathways from a study participant’s home).32
Difficult Family Relationships
Parents completed a questionnaire about parenting practices.37 Eleven items assessed the frequency of harsh and inconsistent parenting behaviors (eg, telling child to get out of the house when the child does something wrong, disciplining one time but not another for the same offense) on a 4-point scale (ranging from “never” to “always”), creating a range of scores from 11 to 44. Higher scores indicate more harsh/inconsistent parenting.
Children completed a questionnaire about parent hostility (in a separate room from parents).37 Fourteen items assessed the frequency of hostility (eg, parent yelling, criticizing, or insulting them) on the same 4-point scale as described previously, creating a range of scores from 14 to 56. Children completed the questionnaire about their mother (given that not all children had a father present). Higher scores indicate greater parent hostility.
Both measures are considered trait (long-term) measures, have been used in numerous previous studies, have established reliability, and have demonstrated validity in being associated with mental and physical health outcomes.38–40
Asthma Control Test
Parents completed the Asthma Control test,41 a 5-item questionnaire with established reliability and validity that assesses asthma symptoms, use of rescue medications, and the effects of asthma on daily functioning over the previous 4 weeks. Higher numbers indicate more well-controlled asthma.
Asthma Functional Limitations
Parents completed the Pediatric Asthma Caregiver Quality of Life Questionnaire,42 which contains a scale assessing functional limitations (eg, child’s asthma caused the family to change their plans). This measure has established reliability and validity,42 and higher scores indicate fewer asthma-related limitations.
Airway Inflammation
FeNO was measured via an electrochemical analyzer according to American Thoracic Society guidelines using the NIOX system (Aerocrine AB, Solna, Sweden). No caffeine, food, or exercise was allowed for 1 hour before the start of testing.
T-Helper Cell Expression of GR Protein
Blood was collected in sodium heparin vacutainers. After red blood cells had been lysed and removed, the cell suspension was incubated with 10% normal human serum for 15 minutes to reduce nonspecific binding. Cells were stained with mouse, anti-human CD3 and CD4 antibodies (PE and APC, respectively; BD Biosciences, San Jose, CA) to identify T-helper cells. After the cells had been fixed and permeabilized, they were stained for intracellular GR with a mouse, anti-human antibody (fluorescein isothiocyanate; AbD Serotec, Hercules, CA), similar to previous studies.43 Data were acquired by using a Guava 6HT2L (Millipore, Billerica, MA) and analyzed with FlowJo (Tree Star Inc, Ashland, OR). The T-helper cell population was gated based on scatter profiles and color signal quadrants. Within this gate, mean fluorescence intensity was calculated as the average fluorescein isothiocyanate event signal, which corresponds to the abundance of GR protein in the T-helper population.
Covariates
Covariates included family socioeconomic status (family income), season of visit, demographic characteristics of the child (age, sex, ethnicity coded as white or other), and medical variables, including asthma severity (mild intermittent, mild persistent, moderate, severe), atopic status (ImmunoCAP Phadiatop, Portage, MI; yes/no), inhaled corticosteroid use, and β agonist use (number of times in the past week for both). To identify the unique effects of greenness and family relationships, medical variables that might have their own associations with, and hence confound associations of greenness or family relationships with outcomes such as asthma control, were included as covariates.
Statistical Analyses
In preliminary analyses, we conducted correlations of covariates with asthma variables. In the primary analyses, we conducted hierarchical multiple regression analyses according to the recommendations of Aiken and West,44 in which asthma measures were predicted from (1) covariates described previously, (2) main effects of greenspace and family relationships, and (3) the interaction between greenspace and family relationships. Interaction coefficients can be interpreted such that positive coefficients mean that at high levels of one variable, there is a positive association between the second variable and the outcome variable. Predictor variables were centered before analyses. We also included figures for illustrative purposes. Because both greenspace and family relationships are continuous variables, these figures are created with estimated regression lines plotted at ±1 SD of these variables.
Results
Preliminary Analyses
Greenspace and difficult family relationships were not associated with each other (r = 0.01, P = .87, and r = −0.10, P = .24 for harsh/inconsistent parenting and parent hostility, respectively). Associations of asthma variables with covariates were as follows: asthma control scores were inversely associated with asthma severity (r = −0.52, P < .001), number of days of β agonist use (r = −0.41, P < .001), and ethnicity, such that white children had better asthma control (t = 3.19, P = .002). More asthma functional limitations (lower scores) were associated with higher asthma severity (r = −0.33, P < .001), higher number of days of β agonist use (r = −0.32, P < .001), and ethnicity, such that white children had fewer asthma limitations (t = 5.10, P < .001). FeNO was associated with atopic status, such that those with positive atopic status had higher FeNO scores (t = 3.82, P < .001) and with ethnicity, such that white children had lower FeNO scores (t = 2.24, P = .03). T-helper cell expression of GR was associated with child age (r = 0.22, P = .01), and with sex, such that girls had a greater abundance of GR (t = 1.96, P = .05).
Greenspace, Family Relationships, and Children’s Clinical Asthma Profiles
See Tables 2 and 3 for details of all regression results.
TABLE 2.
Regression Analyses of Greenspace and Children’s Report of Parent Hostility Predicting Child Asthma Outcomes
| β | 95% Confidence Interval | P | |
|---|---|---|---|
| Asthma control | |||
| Age | 0.06 | −0.12 to 0.34 | .35 |
| Sex | −0.07 | −1.45 to 0.46 | .31 |
| Ethnicity | 0.11 | −0.30 to 1.80 | .16 |
| Family income | 0.09 | −0.11 to 0.40 | .27 |
| Severity | −0.41 | −1.96 to −0.93 | <.001 |
| Inhaled corticosteroid use | 0.04 | −0.11 to 0.21 | .55 |
| β agonist use | −0.30 | −0.78 to −0.30 | <.001 |
| Atopic status | 0.13 | −0.07 to 2.47 | .06 |
| Season of visit | 0.00 | −0.50 to 0.52 | .97 |
| Greenspace | 0.05 | −9.05 to 17.46 | .53 |
| Parent hostility | −0.11 | −0.16 to 0.02 | .12 |
| Greenspace × Parent hostility | 0.03 | −2.28 to 3.34 | .71 |
| Asthma functional limitations | |||
| Age | 0.14 | 0.01 to 0.17 | .04 |
| Sex | 0.04 | −0.24 to 0.45 | .55 |
| Ethnicity | 0.20 | 0.13 to 0.89 | .009 |
| Family income | 0.33 | 0.10 to 0.28 | <.001 |
| Severity | −0.13 | −0.35 to 0.02 | .07 |
| Inhaled corticosteroid use | −0.05 | −0.08 to 0.04 | .48 |
| β agonist use | −0.26 | −0.25 to −0.08 | <.001 |
| Atopic status | 0.07 | −0.24 to 0.67 | .35 |
| Season of visit | 0.01 | −0.17 to 0.20 | .86 |
| Greenspace | 0.02 | −4.27 to 5.27 | .84 |
| Parent hostility | −0.08 | −0.05 to 0.01 | .24 |
| Greenspace × Parent hostility | −0.14 | −2.04 to −0.05 | .04 |
| T-helper cell GR expression | |||
| Age | 0.18 | 0.11 to 2.85 | .03 |
| Sex | 0.19 | 0.76 to 12.28 | .03 |
| Ethnicity | −0.16 | −11.80 to 1.14 | .11 |
| Family income | 0.08 | −0.92 to 2.10 | .44 |
| Severity | −0.18 | −6.16 to −0.00 | .05 |
| Inhaled corticosteroid use | 0.00 | −0.971 to 1.00 | .98 |
| β agonist use | 0.08 | −0.77 to 2.14 | .35 |
| Atopic status | 0.03 | −6.55 to 9.25 | .74 |
| Season of visit | −0.01 | −3.15 to 2.89 | .93 |
| Greenspace | 0.06 | −52.56 to 108.84 | .49 |
| Parent hostility | 0.21 | 0.14 to 1.21 | .01 |
| Greenspace × Parent hostility | −0.11 | −28.32 to 5.55 | .19 |
| FeNO | |||
| Age | −0.08 | −4.06 to 1.31 | .31 |
| Sex | −0.07 | −16.18 to 6.47 | .40 |
| Ethnicity | −0.13 | −21.35 to 3.55 | .16 |
| Family income | −0.01 | −3.19 to 2.83 | .91 |
| Severity | −0.01 | −6.60 to 5.59 | .87 |
| Inhaled corticosteroid use | −0.15 | −3.67 to 0.20 | .08 |
| β agonist use | 0.17 | 0.11 to 5.88 | .04 |
| Atopic status | 0.25 | 8.27 to 38.41 | .003 |
| Season of visit | 0.02 | −5.20 to 6.86 | .79 |
| Greenspace | −0.01 | −168.89 to 145.76 | .89 |
| Parent hostility | 0.02 | −0.90 to 1.21 | .77 |
| Greenspace × Parent hostility | 0.22 | 12.88 to 77.91 | .007 |
β data are standardized coefficients; 95% confidence interval is around the unstandardized β coefficient. Regression analyses were conducted in a stepwise fashion. Thus, the coefficients for all variables except the interaction term represent the main effect of that variable (with no interaction term included). The coefficients for interaction terms represent the interaction effect with main effects of all covariates and independent variables included. Ethnicity is coded as white or other. Inhaled corticosteroid and β agonist use refer to the number of days in the past week that participants took that medication. T-helper cell GR expression refers to the mean fluorescence intensity of glucocorticoid receptors in T-helper cells.
TABLE 3.
Regression Analyses of Greenspace and Harsh and Inconsistent Parenting Practices Predicting Child Asthma Outcomes
| β | 95% Confidence Interval | P | |
|---|---|---|---|
| Asthma control | |||
| Age | 0.05 | −0.15 to 0.31 | .50 |
| Sex | −0.06 | −1.40 to 0.53 | .37 |
| Ethnicity | 0.11 | −0.26 to 1.86 | .14 |
| Family income | 0.10 | −0.09 to 0.42 | .20 |
| Severity | −0.41 | −1.98 to −0.93 | <.001 |
| Inhaled corticosteroid use | 0.05 | −0.11 to 0.22 | .51 |
| β agonist use | −0.31 | −0.80 to −0.31 | <.001 |
| Atopic status | 0.12 | −0.19 to 2.37 | .09 |
| Season of visit | 0.01 | −0.47 to 0.55 | .88 |
| Greenspace | 0.05 | −8.72 to 18.04 | .49 |
| Parenting | −0.02 | −0.21 to 0.163 | .82 |
| Greenspace × Harsh/inconsistent parenting | −0.15 | −9.44 to −0.73 | .02 |
| Asthma functional limitations | |||
| Age | 0.12 | −0.01 to 0.15 | .08 |
| Sex | 0.04 | −0.25 to 0.43 | .59 |
| Ethnicity | 0.21 | 0.15 to 0.89 | .007 |
| Family income | 0.34 | 0.11 to 0.29 | <.001 |
| Severity | −0.12 | −0.33 to 0.04 | .11 |
| Inhaled corticosteroid use | −0.07 | −0.09 to 0.03 | .31 |
| β agonist use | −0.27 | −0.26 to −0.08 | <.001 |
| Atopic status | 0.07 | −0.22 to 0.68 | .31 |
| Season of visit | 0.03 | −0.14 to 0.22 | .69 |
| Greenspace | 0.03 | −3.85 to 5.60 | .72 |
| Parenting | −0.14 | −0.14 to −0.01 | .04 |
| Greenspace × Harsh/inconsistent parenting | −0.06 | −2.21 to 0.92 | .42 |
| T-helper cell GR expression | |||
| Age | 0.20 | 0.24 to 3.02 | .02 |
| Sex | 0.17 | −0.01 to 11.73 | .05 |
| Ethnicity | −0.18 | −12.66 to 0.51 | .07 |
| Family income | 0.05 | −1.14 to 1.92 | .62 |
| Severity | −0.16 | −5.89 to 0.42 | .09 |
| Inhaled corticosteroid use | −0.04 | −1.23 to 0.82 | .69 |
| β agonist use | 0.10 | −0.62 to 2.33 | .25 |
| Atopic status | 0.05 | −5.58 to 10.53 | .54 |
| Season of visit | −0.01 | −3.30 to 2.88 | .89 |
| Greenspace | 0.06 | −55.05 to 109.65 | .51 |
| Parenting | −0.08 | −1.67 to 0.56 | .33 |
| Greenspace × Harsh/inconsistent parenting | −0.17 | −53.10 to −0.22 | .05 |
| FeNO | |||
| Age | −0.07 | −3.91 to 1.41 | .36 |
| Sex | −0.07 | −15.98 to 6.65 | .42 |
| Ethnicity | −0.13 | −21.37 to 3.45 | .16 |
| Family income | −0.01 | −3.19 to 2.78 | .89 |
| Severity | −0.02 | −6.84 to 5.41 | .82 |
| Inhaled corticosteroid use | −0.14 | −3.59 to 0.33 | .10 |
| β agonist use | 0.17 | 0.16 to 5.89 | .04 |
| Atopic status | 0.25 | 8.04 to 38.07 | .003 |
| Season of visit | 0.02 | −5.40 to 6.64 | .84 |
| Greenspace | −0.02 | −172.18 to 142.29 | .85 |
| Parenting | 0.06 | −1.43 to 2.91 | .50 |
| Greenspace × Harsh/inconsistent parenting | −0.09 | −80.81 to 23.00 | .27 |
β data are standardized coefficients; 95% confidence interval is around the unstandardized β coefficient. Regression analyses were conducted in a stepwise fashion. Thus, the coefficients for all variables except the interaction term represent the main effect of that variable (with no interaction term included). The coefficients for interaction terms represent the interaction effect with main effects of all covariates and independent variables included. Ethnicity is coded as white or other. Inhaled corticosteroid and β agonist use refer to the number of days in the past week that participants took that medication. T-helper cell GR expression refers to the mean fluorescence intensity of glucocorticoid receptors in T-helper cells.
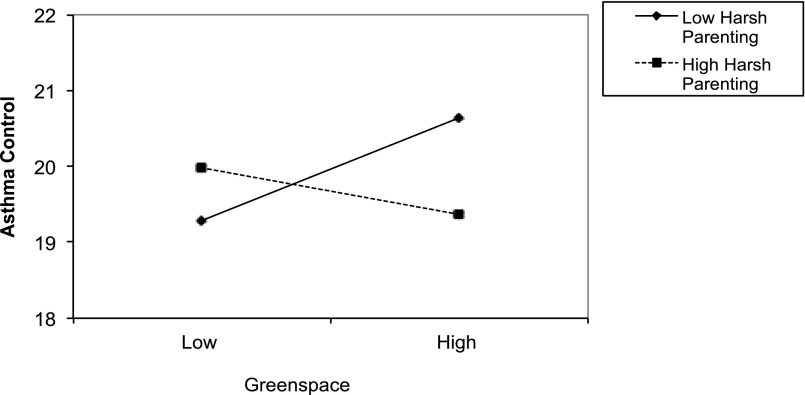
Asthma Control
There were no main effects of either greenspace or harsh/inconsistent parenting on asthma control; however, there was a significant interaction between greenspace and harsh and inconsistent parenting predicting child asthma control (β = −.15, P = .02). For illustrative purposes, we depict this interaction in Fig 1, which illustrates that as the extent of harsh/inconsistent parenting decreases, the effect of greenspace becomes more positive such that more greenspace is associated with better asthma control.
FIGURE 1.
Interaction of greenspace by harsh/inconsistent parenting predicting Asthma Control Test scores in children. Graph reflects estimated regression lines drawn from −1 SD to +1 SD of the greenspace variable. Low and high on harsh/inconsistent parenting also refers to ±1 SD.
Asthma Functional Limitations
There were no main effects of either greenspace or parent hostility on asthma functional limitations; however, there was a significant interaction between greenspace and perceived parental hostility on asthma functional limitations (β = −.14, P = .04). This interaction operated in the same way as for asthma control, whereby as parental hostility decreased, more greenspace became associated with fewer asthma functional limitations (higher scores).
Greenspace, Family Relationships, and Children’s Biological Profiles
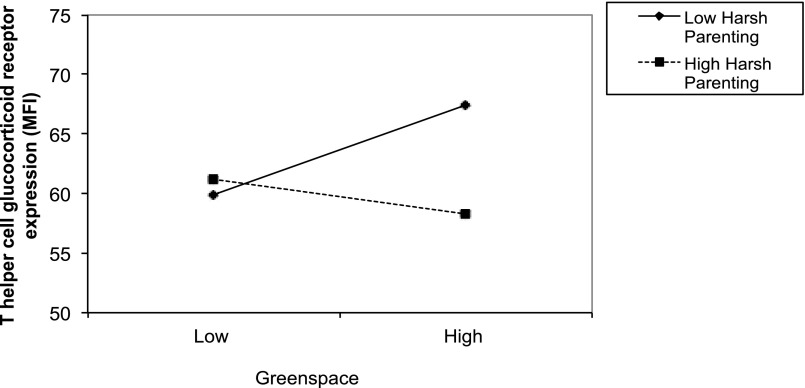
T-Helper Cell Expression of GR Protein
There were no main effects of either greenspace or harsh/inconsistent parenting on expression of GR; however, there was a significant interaction between greenspace and harsh/inconsistent parenting in predicting the expression of GR in children’s T-helper cells (β = −.17, P = .05). For illustrative purposes, we depict the interaction in Fig 2. This figure reveals that as harsh/inconsistent parenting decreases, the relationship between greenspace and GR expression becomes more positive; that is, more greenspace is associated with a greater abundance of GR protein in children’s T-helper cells.
FIGURE 2.
Interaction of greenspace by harsh/inconsistent parenting predicting T-helper cell expression (CD3+CD4+) of GR protein, as measured by mean fluorescence intensity (MFI) in children. Graph reflects estimated regression lines drawn from −1 SD to +1 SD of the greenspace variable. Low and high on harsh/inconsistent parenting also refers to ±1 SD.
FeNO
There were no significant main effects of either greenspace or children’s perceptions of parent hostility on FeNO scores. There was a significant interaction between greenspace and children’s perceptions of parent hostility in predicting airway inflammation (β = .22, P = .007). See Table 2 for details of regression results. Consistent with the other interaction patterns, as parental hostility decreased, more greenspace became associated with lower airway inflammation.
Discussion
This study tested the role that difficult family relationships and residential greenspace play in childhood asthma. Although the study is correlational and hence we cannot draw conclusions about causality, we documented a number of interactions across both clinical and biological asthma measures. These interactions were all in a direction suggesting that as family environments become less negative, greenspace has more beneficial links to clinical outcomes, such as asthma control, and to disease-relevant biological processes, such as airway inflammation, in children. These findings could not be explained by family socioeconomic status, child demographic characteristics, or child medical variables, such as atopic status. Rather, they highlight the utility for pediatricians of considering the social environment in conjunction with the physical environment when trying to understand complex diseases such as childhood asthma.45
Previous research has explored interactions between physical and social environments with respect to factors such as neighborhood air pollution,46–48 but none has conducted such tests with respect to greenspace. A focus on positive neighborhood qualities may help with future intervention approaches to promoting children’s health, and consistent with this idea, there is an emerging literature on factors that predict positive interactions with neighborhood greenspaces.49 In the current study, rather than mitigating the detrimental effects of highly stressful environments (as initially hypothesized), greenspace appeared to synergize with more positive psychosocial environments; that is, when both greenspace was high and parent-child relationships were good, children exhibited the best asthma profiles. Thus, positive family relationships may serve as a resilience factor that helps to promote the benefits of greenspace (or vice versa). We cannot infer causal relationships from these data, but they suggest the possibility that children may gain the most from environments that are positive across multiple dimensions, including both the physical and the social.
In our study, patterns differed depending on whether harsh/inconsistent parenting or children’s perceptions of parent hostility were used as the family relationships measure. The pattern of interactions was consistent across psychosocial variables. However, associations with specific asthma outcomes varied by family relationships measure. Although the reasons for these differences are unclear, harsh/inconsistent parenting and children’s perceptions of parent hostility were not significantly correlated (r = 0.15), suggesting that these variables reflect 2 different psychosocial processes. Children who perceive their parents as hostile toward them may feel unsupported or unloved by parents, which may translate into the children being less likely to do activities in greenspaces together with their parent. Thus, even if these children are living in high greenspace areas, because of their difficult relationships at home, these children may not be interacting with these greenspaces together with their families as much as those in more supportive family environments, meaning that the benefits of greenspace for inflammatory processes50 and for activity5 are not accruing as readily. Although speculative, this may explain interaction effects of parent hostility and greenspace on children’s airway inflammation and asthma functional limitations. This explanation also would be consistent with the broader literature on neighborhood environments and children’s health that has documented that neighborhood conditions (eg, dilapidated housing) are associated with parent reports of children’s health status via effects on family functioning (eg, difficulties in parenting).51
Harsh/inconsistent parenting practices interacted with greenspace to predict asthma control and the abundance of GR within T-helper cells. This parenting variable is more about the predictability with which parents act; for example, whether parents punish one time but not another for the same behavior. Over time, this type of day-to-day unpredictability may create the type of chronic stress that has been found to reduce immune cell responsiveness to the anti-inflammatory properties of cortisol,30,52 and hence potentially to worsen asthma control. Here, the effects of chronic stress may overwhelm the benefits of greenspace, thus resulting in greenspace being associated with beneficial effects under conditions of low, but not high, harsh/inconsistent parenting.
Strengths of the current study include the interdisciplinary approach of studying psychological factors in conjunction with physical environment factors when trying to better understand child health. In addition, the objective measure of residential greenness derived from satellite images is another strength. A third strength is the assessment of immunologic mechanisms within the context of a chronic disease. This allowed us to test hypotheses that exposure to greenspace promotes better regulation of inflammatory processes.50 Limitations of the current study include the study design, which prevents conclusions about causality or directionality. Hence alternative explanations (eg, child psychological traits that covary with difficult family relationships, or neighborhood characteristics that covary with greenspace) are always possible. Future studies that can manipulate either greenspace or family environments would provide stronger evidence about causality. Other limitations include greenspace measures not informing us about actual time spent by participants in green areas, or about the specific characteristics of those greenspaces (eg, what percentage are parks, what types of allergenic trees are present). Further, residual exposure misclassification is always a possibility. Although we specified a rationale for the 250-m circular buffer, the radius and shape of this buffer is still somewhat arbitrary.
Future studies that are able to assess daily personal exposures to greenspace, as well as daily interactions between parents and their children, could provide additional information about the timing of the relationship of these 2 factors to childhood asthma. With questionnaires, there is always the possibility of self-report biases, such as parents being unlikely to report themselves as harsh parents; however, this was why we included a child report as well. In addition, future studies also may want to include observed behavioral measures of parenting. We also note that our conclusions largely center around individual-level implications of family relationship difficulties and greenspace, rather than implications for population-level associations of greenspace with asthma. Finally, this study was not able to address alternative mechanisms by which greenspace might have effects on asthma, such as through pollution-buffering effects (although evidence for these effects is somewhat mixed53), or exposure to microbial diversity.18,50
Conclusions
The current study demonstrated interactions between residential greenspace and difficult family relationships. As family relationships became less negative, associations became stronger between greenspace and better asthma control, fewer functional limitations, less airway inflammation, and greater abundance of GR in T-helper cells. Although conclusions are preliminary, given the observational data, these findings suggest that for children with asthma to benefit from high greenspace areas, positive family relationships may need to be present. If validated in future research through experimental designs, it would suggest that to maximize our ability to improve asthma outcomes in children, researchers and clinicians may need to develop multimodal interventions that target not only children’s experiences in their physical environment but their family environments as well.
Supplementary Material
Glossary
- FeNO
fractional concentration of exhaled nitric oxide
- GR
glucocorticoid receptor
Footnotes
Dr Chen conceptualized and designed the study, conducted data analyses, and drafted the initial manuscript; Dr Miller conceptualized and designed the study, provided critical feedback on data interpretation, and revised the manuscript; Drs Shalowitz and Story coordinated data recruitment, contributed to data interpretation, and critically reviewed the manuscript; Dr Levine and Ms Hayen assisted with the design of data collection instruments, coordinated data collection, and critically reviewed the manuscript; Drs Sbihi and Brauer carried out greenspace analyses, gave input on data analyses and interpretation, and critically reviewed the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Funded by National Institutes of Health grant R01 HL108723. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Bowler DE, Buyung-Ali LM, Knight TM, Pullin AS. A systematic review of evidence for the added benefits to health of exposure to natural environments. BMC Public Health. 2010;10:456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McCurdy LE, Winterbottom KE, Mehta SS, Roberts JR. Using nature and outdoor activity to improve children’s health. Curr Probl Pediatr Adolesc Health Care. 2010;40(5):102–117 [DOI] [PubMed] [Google Scholar]
- 3.Maas J, Verheij RA, de Vries S, Spreeuwenberg P, Schellevis FG, Groenewegen PP. Morbidity is related to a green living environment. J Epidemiol Community Health. 2009;63(12):967–973 [DOI] [PubMed] [Google Scholar]
- 4.Bell JF, Wilson JS, Liu GC. Neighborhood greenness and 2-year changes in body mass index of children and youth. Am J Prev Med. 2008;35(6):547–553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cohen DA, Ashwood JS, Scott MM, et al. Public parks and physical activity among adolescent girls. Pediatrics. 2006;118(5). Available at: www.pediatrics.org/cgi/content/full/118/5/e1381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wolch J, Jerrett M, Reynolds K, et al. Childhood obesity and proximity to urban parks and recreational resources: a longitudinal cohort study. Health Place. 2011;17(1):207–214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Villeneuve PJ, Jerrett M, Su JG, et al. A cohort study relating urban green space with mortality in Ontario, Canada. Environ Res. 2012;115:51–58 [DOI] [PubMed] [Google Scholar]
- 8.Tsunetsugu Y, Park BJ, Ishii H, Hirano H, Kagawa T, Miyazaki Y. Physiological effects of Shinrin-yoku (taking in the atmosphere of the forest) in an old-growth broadleaf forest in Yamagata Prefecture, Japan. J Physiol Anthropol. 2007;26(2):135–142 [DOI] [PubMed] [Google Scholar]
- 9.Li Q, Morimoto K, Kobayashi M, et al. Visiting a forest, but not a city, increases human natural killer activity and expression of anti-cancer proteins. Int J Immunopathol Pharmacol. 2008;21(1):117–127 [DOI] [PubMed] [Google Scholar]
- 10.Gascon M, Triguero-Mas M, Martínez D, et al. Mental health benefits of long-term exposure to residential green and blue spaces: a systematic review. Int J Environ Res Public Health. 2015;12(4):4354–4379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hartig T, Kahn PH Jr. Living in cities, naturally. Science. 2016;352(6288):938–940 [DOI] [PubMed] [Google Scholar]
- 12.James P, Hart JE, Banay RF, Laden F. Exposure to greenness and mortality in a nationwide prospective cohort study of women. Environ Health Perspect. 2016;124(9):1344–1352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaplan S. The restorative benefits of nature: towards an integrative framework. J Environ Psychol. 1995;16:169–182 [Google Scholar]
- 14.Fan Y, Das KV, Chen Q. Neighborhood green, social support, physical activity, and stress: assessing the cumulative impact. Health Place. 2011;17(6):1202–1211 [DOI] [PubMed] [Google Scholar]
- 15.Lovasi GS, Quinn JW, Neckerman KM, Perzanowski MS, Rundle A. Children living in areas with more street trees have lower prevalence of asthma. J Epidemiol Community Health. 2008;62(7):647–649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sbihi H, Tamburic L, Koehoorn M, Brauer M. Greenness and incident childhood asthma: a 10-year follow-up in a population-based birth cohort. Am J Respir Crit Care Med. 2015;192(9):1131–1133 [DOI] [PubMed] [Google Scholar]
- 17.Fuertes E, Markevych I, Bowatte G, et al. ; MACS . Residential greenness is differentially associated with childhood allergic rhinitis and aeroallergen sensitization in seven birth cohorts. Allergy. 2016;71(10):1461–1471 [DOI] [PubMed] [Google Scholar]
- 18.Lovasi GS, O’Neil-Dunne JP, Lu JW, et al. Urban tree canopy and asthma, wheeze, rhinitis, and allergic sensitization to tree pollen in a New York City birth cohort. Environ Health Perspect. 2013;121(4):494–500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pilat MA, McFarland A, Snelgrove A, Collins K, Waliczek TM, Zajicek J. The effect of tree cover and vegetation on incidence of childhood asthma in metropolitan statistical areas of Texas. HortTechnology. 2012;22(5):631–637 [Google Scholar]
- 20.Dadvand P, Villanueva CM, Font-Ribera L, et al. Risks and benefits of green spaces for children: a cross-sectional study of associations with sedentary behavior, obesity, asthma, and allergy. Environ Health Perspect. 2014;122(12):1329–1335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wright RJ, Rodriguez M, Cohen S. Review of psychosocial stress and asthma: an integrated biopsychosocial approach. Thorax. 1998;53(12):1066–1074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen E, Miller GE. Stress and inflammation in exacerbations of asthma. Brain Behav Immun. 2007;21(8):993–999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Klinnert MD, Nelson HS, Price MR, Adinoff AD, Leung DY, Mrazek DA. Onset and persistence of childhood asthma: predictors from infancy. Pediatrics. 2001;108(4). Available at: www.pediatrics.org/cgi/content/full/108/4/e69 [DOI] [PubMed] [Google Scholar]
- 24.Strunk RC, Mrazek DA, Fuhrmann GS, LaBrecque JF. Physiologic and psychological characteristics associated with deaths due to asthma in childhood. A case-controlled study. JAMA. 1985;254(9):1193–1198 [PubMed] [Google Scholar]
- 25.Wright RJ, Finn P, Contreras JP, et al. Chronic caregiver stress and IgE expression, allergen-induced proliferation, and cytokine profiles in a birth cohort predisposed to atopy. J Allergy Clin Immunol. 2004;113(6):1051–1057 [DOI] [PubMed] [Google Scholar]
- 26.Jones SL, Kittelson J, Cowan JO, et al. The predictive value of exhaled nitric oxide measurements in assessing changes in asthma control. Am J Respir Crit Care Med. 2001;164(5):738–743 [DOI] [PubMed] [Google Scholar]
- 27.Beck-Ripp J, Griese M, Arenz S, Köring C, Pasqualoni B, Bufler P. Changes of exhaled nitric oxide during steroid treatment of childhood asthma. Eur Respir J. 2002;19(6):1015–1019 [DOI] [PubMed] [Google Scholar]
- 28.Busse WW, Lemanske RF Jr. Asthma. N Engl J Med. 2001;344(5):350–362 [DOI] [PubMed] [Google Scholar]
- 29.Miller GE, Chen E. Harsh family climate in early life presages the emergence of a proinflammatory phenotype in adolescence. Psychol Sci. 2010;21(6):848–856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cohen S, Janicki-Deverts D, Doyle WJ, et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proc Natl Acad Sci U S A. 2012;109(16):5995–5999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Herring JW. Measuring vegetation (NDVI & EVI). 2000. Available at:http://earthobservatory.nasa.gov/Features/MeasuringVegetation/. Accessed June 13, 2016
- 32.World Health Organization Urban Green Spaces and Health. Copenhagen, Denmark: WHO Regional Office for Europe; 2016 [Google Scholar]
- 33.Dadvand P, de Nazelle A, Figueras F, et al. Green space, health inequality and pregnancy. Environ Int. 2012;40:110–115 [DOI] [PubMed] [Google Scholar]
- 34.Sbihi H, Koehoorn M, Tamburic L, Brauer M. Asthma trajectories in a population-based birth cohort: impacts of air pollution and greenness [published online ahead of print September 8, 2016]. Am J Respir Crit Care Med. http://dx.doi.org/10.1164/rccm.201601-0164OC [DOI] [PubMed] [Google Scholar]
- 35.Cusack L, Larkin A, Carozza S, Hystad P. Associations between residential greenness and birth outcomes across Texas. Environ Res. 2017;152:88–95 [DOI] [PubMed] [Google Scholar]
- 36.Rhew IC, Vander Stoep A, Kearney A, Smith NL, Dunbar MD. Validation of the normalized difference vegetation index as a measure of neighborhood greenness. Ann Epidemiol. 2011;21(12):946–952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brody GH, Ge X, Conger R, et al. The influence of neighborhood disadvantage, collective socialization, and parenting on African American children’s affiliation with deviant peers. Child Dev. 2001;72(4):1231–1246 [DOI] [PubMed] [Google Scholar]
- 38.Brody GH, Yu T, Beach SR, Kogan SM, Windle M, Philibert RA. Harsh parenting and adolescent health: a longitudinal analysis with genetic moderation. Health Psychol. 2014;33(5):401–409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Miller GE, Brody GH, Yu T, Chen E. A family-oriented psychosocial intervention reduces inflammation in low-SES African American youth. Proc Natl Acad Sci U S A. 2014;111(31):11287–11292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brody GH, Yu T, Chen YF, et al. Cumulative socioeconomic status risk, allostatic load, and adjustment: a prospective latent profile analysis with contextual and genetic protective factors. Dev Psychol. 2013;49(5):913–927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nathan RA, Sorkness CA, Kosinski M, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol. 2004;113(1):59–65 [DOI] [PubMed] [Google Scholar]
- 42.Juniper EF, Guyatt GH, Feeny DH, Ferrie PJ, Griffith LE, Townsend M. Measuring quality of life in the parents of children with asthma. Qual Life Res. 1996;5(1):27–34 [DOI] [PubMed] [Google Scholar]
- 43.Miller GE, Murphy MLM, Cashman R, et al. Greater inflammatory activity and blunted glucocorticoid signaling in monocytes of chronically stressed caregivers. Brain Behav Immun. 2014;41:191–199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. London, UK: Sage Publications; 1991 [Google Scholar]
- 45.Wright RJ, Subramanian SV. Advancing a multilevel framework for epidemiologic research on asthma disparities. Chest. 2007;132(Suppl 5):757S–769S [DOI] [PubMed] [Google Scholar]
- 46.Shankardass K, McConnell R, Jerrett M, Milam J, Richardson J, Berhane K. Parental stress increases the effect of traffic-related air pollution on childhood asthma incidence. Proc Natl Acad Sci U S A. 2009;106(30):12406–12411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen E, Schreier HMC, Strunk RC, Brauer M. Chronic traffic-related air pollution and stress interact to predict biologic and clinical outcomes in asthma. Environ Health Perspect. 2008;116(7):970–975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Clougherty JE, Levy JI, Kubzansky LD, et al. Synergistic effects of traffic-related air pollution and exposure to violence on urban asthma etiology. Environ Health Perspect. 2007;115(8):1140–1146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fan Y, French SA, Das KV. Family structure and park use among parents. Am J Prev Med. 2012;43(5):520–526 [DOI] [PubMed] [Google Scholar]
- 50.Rook GA. Regulation of the immune system by biodiversity from the natural environment: an ecosystem service essential to health. Proc Natl Acad Sci U S A. 2013;110(46):18360–18367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fan Y, Chen Q. Family functioning as a mediator between neighborhood conditions and children’s health: evidence from a national survey in the United States. Soc Sci Med. 2012;74(12):1939–1947 [DOI] [PubMed] [Google Scholar]
- 52.Rohleder N, Marin TJ, Ma R, Miller GE. Biologic cost of caring for a cancer patient: dysregulation of pro- and anti-inflammatory signaling pathways. J Clin Oncol. 2009;27(18):2909–2915 [DOI] [PubMed] [Google Scholar]
- 53.Vos PEJ, Maiheu B, Vankerkom J, Janssen S. Improving local air quality in cities: to tree or not to tree? Environ Pollut. 2013;183:113–122 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.