Abstract
A 50-year-old man with end-stage renal failure was referred by his general practitioner with dyspeptic symptoms. On further questioning the patient complained of a 10-year history of frequent belching. This was noticeably worse after meals and during times of stress. He did not have nocturnal belching and episodes of belching were less frequent when the patient was talking or distracted. There was no history of gastro-oesophageal reflux, vomiting, dysphagia, loss of appetite or weight loss. He was diagnosed with excessive, probably supragastric, belching. Further investigation was not deemed necessary. His symptoms have since settled with simple reassurance and explanation of their origin provided during the clinic visit.
Keywords: Dyspepsia, Gastroduodenal Motility
Introduction
Belching, also known as eructation, is the audible escape of air from the oesophagus into the pharynx.1 During each swallow between 8 and 32 mL of air is swallowed and enters the stomach.2 Excessive gastric distension due to swallowed air is avoided through reflux of air during belching. Distension of the stomach leads to transient lower oesophageal sphincter relaxation, a vagally mediated reflex, which allows air to enter the oesophagus through a relaxed sphincter, with subsequent expulsion orally.1 3–5 Therefore, belching is part of daily experience and can only be considered a disorder when the symptoms become frequent and distressing, particularly in social situations, for the patient.1 6 Community surveys suggest people rarely consult their general practitioner with this symptom.7
It had been assumed for many years that excessive belching was due to excessive swallowing of air into the stomach or aerophagia, with reflux of gas from the stomach and belching as a consequence. However, it has become clear that aerophagia and excessive belching are distinct conditions with different pathophysiological mechanisms.1 Excessive belching can be divided into excessive gastric or supragastric belching.8 Gastric belches are usually physiological, involuntary and occur up to 30 times a day.1 Supragastric belches occur as a result of rapid flow of air into the oesophagus that does not reach the stomach.8 Supragastric belches are voluntary and can be considered behavioural.1 Patients presenting with excessive belching as their main symptom usually have an increased frequency of supragastric, but not gastric, belches. Patients with aerophagia, a rarer condition, swallow large quantities of air, have abdominal distension and bloating, and as a result may have an increase in gastric belching.9
Excessive belching can accompany both gastro-oesophageal reflux disease (GORD) and functional dyspepsia with a reported incidence of between 40 and 80%, although other symptoms predominate.5 10 11 It has been proposed that supragastric belching is the patient's response to an unpleasant oesophageal sensation, as supragastric belching may occur a few seconds after the onset of a reflux episode, although belching has also been noted to induce reflux episodes in some patients.12 Aerophagia may complicate continuous positive airway pressure therapy when used for obstructive sleep apnoea.13
Psychological and behavioural factors play a key role in patients with excessive belching. Belching episodes are significantly reduced when patients with excessive belching are unaware that they are being observed and also when they are distracted.14 Symptoms of belching then increase when patients know they are being observed.14 Finally, supragastric belches are almost absent during sleep.15
Clinical features
Patients with excessive supragastric belching may report belching up to 20 times a minute.16 They may additionally describe epigastric discomfort, nausea and vomiting, early satiety, abdominal bloating and abdominal distension.1 16–19 Given the association of belching with GORD, patients may present with typical gastro-oesophageal reflux symptoms of heartburn and regurgitation.5 Patients with excessive supragastric belching characteristically exhibit excessive belching during the consultation. Symptoms are often long standing before a diagnosis is reached with a lack of awareness of particularly supragastric belching a contributory factor.17 19 20 Proposed diagnostic criteria for aerophagia and excessive belching are listed in box 1.
Box 1. Rome III diagnostic criteria for belching disorders6.
Diagnostic criteria for aerophagia*
Must include all of the following:
Troublesome repetitive belching at least several times a week
Air swallowing that is objectively observed or measured
Diagnostic criteria for unspecified excessive belching*
Must include all of the following:
Troublesome repetitive belching at least several times a week
No evidence that excessive air swallowing underlies the symptom
*Criteria fulfilled for the past 3 months, with symptom onset at least 6 months before diagnosis.
Patients with belching disorders report significant anxiety, and excessive belching has been described in patients with psychiatric disorders, such as obsessive compulsive disorder and eating disorders.17 21 22 Patients with supragastric belching have impaired health-related quality of life. This is due to a combination of impaired social functioning and isolation, impaired mental health and vitality and increased body pain. Belching can be loud and socially disruptive, leading to embarrassment and increasing social isolation.16 23
Diagnosis and investigation
A thorough history is usually the key to diagnosing the cause of a patient's excessive belching. The history should focus on the frequency of belching, the occurrence during sleep or other activities—for example, after meals, the effect of stress and the presence of dysphagia, weight loss, gastro-oesophageal reflux symptoms, dyspepsia, abdominal distension and psychiatric comorbidity.1 Box 2 describes a typical plan of investigation for a patient with excessive belching.
Box 2. Clinical investigation for excessive belching1 16.
History
Frequency of belching
Occurrence of belching during sleep or other activities
Effect of stress
Presence of gastro-oesophageal reflux disease (GORD), dyspepsia, dysphagia, weight loss, psychiatric comorbidity
Physical examination
No abnormalities
Abdominal x-ray examination
No abnormalities
Oesophageal impedance studies
Supragastric belches in high frequency
Normal air swallowing
Treatment
Dietary advice
Behavioural therapies
Proton pump inhibitor, if indicated
Upper gastrointestinal endoscopy if indicated to rule out organic pathology
The reported age at diagnosis varies between 46 and 58 years and although the risk of malignancy is very low, upper gastrointestinal endoscopy should be undertaken when excessive belching is accompanied by other upper gastrointestinal symptoms that meet criteria for investigation.17 19 24 Additional investigations may be necessary to exclude other disorders such as GORD or rumination. The most useful investigation when GORD may be contributing and there is no response to a trial of a twice daily proton pump inhibitor (PPI) is ambulatory oesophageal pH and impedance monitoring. Excessive belching may accompany GORD, and in some cases belching may induce GORD, and therefore this is an important diagnosis to rule out and treat appropriately with PPIs.6 10 12 On pH/impedance monitoring patients with GORD characteristically will have an excessive number or duration of acid reflux episodes associated with gas or liquid reflux, whereas patients with supragastric belching will have numerous episodes of swallowed gas being immediately refluxed.
If the diagnosis remains uncertain, the combination of high-resolution manometry (HRM) with impedance monitoring will differentiate between gastric and supragastric belches and rumination.25 Gastric belches are characterised by lower oesophageal sphincter relaxation, retrograde airflow into the oesophagus, simultaneous oesophageal pressure increase (common cavity phenomenon) and upper oesophageal sphincter relaxation after the onset of the retrograde airflow.25
Two mechanisms underlie supragastric belching—air pushing and air sucking. First, contraction and aboral movement of the diaphragm creates an increased negative pressure in the thoracic cavity and the oesophagus, with subsequent relaxation of the upper oesophageal sphincter resulting in inflow of air into the oesophagus followed by the immediate retrograde expulsion of air through straining (air sucking). The second mechanism, found in a minority of patients, involves simultaneous contraction of the muscles of the base of the tongue and the pharynx resulting in inflow of air with subsequent expulsion due to straining (air pushing).1 8 25
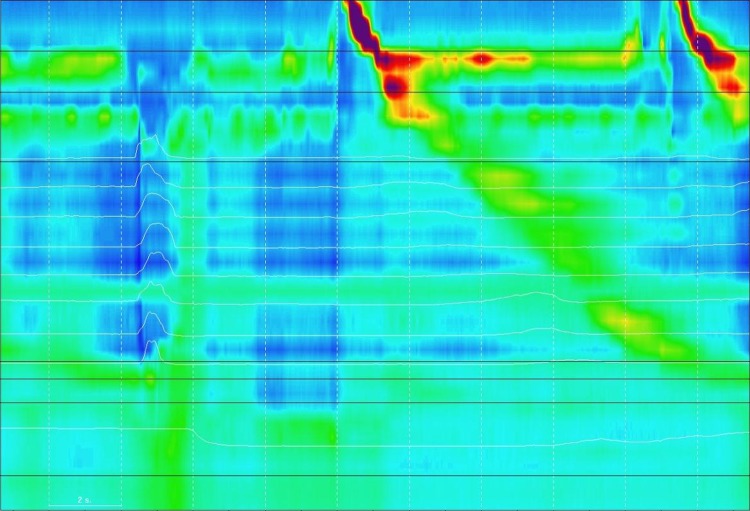
Repetitive supragastric belching occurs in the majority (70%) of patients with excessive belching, with belches occurring up to every 2 s.25 This repetitive pattern is not seen with gastric belching. In rumination, combined HRM with impedance monitoring classically shows an abrupt rise in intragastric pressure (abdomino-gastric strain) of at least 20 mm Hg above baseline with associated retrograde pressure gradient and movement of gastric contents across the lower oesophageal sphincter up to the mouth within 10 s of the strain event. This is followed by primary or secondary oesophageal peristalsis to return oesophageal contents to the stomach.20 Figure 1 is a combined HRM and impedance study in a patient with excess belching and gastro-oesophageal reflux symptoms. Supragastric belching induced multiple acid reflux episodes in this patient.
Figure 1.
Combined high-resolution manometry, pH and impedance monitoring in a patient with excessive belching and gastro-oesophageal reflux symptoms. The upper oesophageal sphincter is at the top of the figure and the lower oesophageal sphincter and stomach at the bottom. Contraction and aboral movement of the diaphragm creates an increased negative pressure in the oesophagus, with subsequent relaxation of the upper oesophageal sphincter. This results in an inflow of air into the oesophagus, seen as a progressive rise in impedance progressing down the oesophagus, followed by the immediate retrograde expulsion of air (air sucking). The supragastric belch is associated with lower oesophageal sphincter relaxation and reflux of acid into the oesophagus on the pH trace (the lowest white line) in the lower part of the figure.
Management
Unfortunately, the evidence for the management of excessive belching is limited. However, a thorough explanation of the cause of the patient's symptoms and reassurance are important parts of the initial management and may be all that is required.
There is some evidence for a role for behavioural therapies in the treatment of patients with excessive belching. Speech therapy focusing on glottal movements and control of breathing led to a significant symptom reduction in over 50% of patients with excessive supragastric belching.19 However, this was a small, open study involving just 11 patients. Other behavioural therapies such as diaphragmatic breathing, cognitive behavioural therapy and biofeedback have been reported to be effective.20 22 26–29 Hypnosis has been reported to be beneficial in a single case report.30 Unfortunately, a shortage of therapists familiar with these therapeutic approaches means that such treatments are not widely available.
More recently however, an office-based behavioural therapy has been reported, with good response rates (80%) in a case series of five patients.31 Patients were positioned supinely and asked to breathe slowly (approximately eight breaths a minute) and diaphragmatically (with their abdomen but not their chest moving as they breathe) with their mouth open wide to prevent swallowing. If this was successful patients were asked to perform the same technique whilst sitting and continue daily practice at home. At home patients were asked to keep their mouth open initially but when in public asked to keep it slightly ajar. Wide mouth opening was used to abort a belching attack.31 Anecdotally, asking a patient to protrude their tongue or keeping their mouth slightly ajar has been noted to stop an attack of belching during a consultation.
Dietary modification is often recommended in patients with excessive belching. This includes the avoidance of chewing gum and carbonated drinks, drinking through a straw, eating slowly and encouraging small swallows.6 Baclofen (an agonist of the γ-aminobutyric acid receptor) has recently been shown to be effective in reducing the symptoms of supragastric belching by increasing lower oesophageal sphincter pressure and decreasing swallowing rate.32 Side effects of drowsiness and difficulties concentrating, although mild, were reported in 33% of patients in the study, limiting its benefit as a potential therapeutic agent. Clonazepam has been successfully used to treat aerophagia in children, with a reported remission rate of 66.7%.33
If it is thought from the patient's symptoms or investigations that GORD might be a contributory factor in excessive belching, then PPI therapy should be started. If belching remains a major concern then the above behavioural measures can also be instituted. Anti-reflux surgery will reduce the frequency of gastric belching but is likely to result in bloating with retained swallowed air owing to the impairment in belching after surgery and is not indicated outside the treatment of GORD.16 23
Conclusions
Excessive belching is the result of excessive supragastric or gastric belches or aerophagia, and can occur as a symptom associated with GORD. When patients present with belching as the predominant symptom, supragastric belches are the main cause with a typical pattern seen on HRM and impedance studies. Excessive belching, especially supragastric, can be considered a behavioural or functional disorder, with organic pathology rarely found. There is a lack of controlled trials of effective treatment, although behavioural therapies appear promising.
Footnotes
Contributors: Both authors contributed equally to the writing of the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; internally peer reviewed.
Web resources: Rome Foundation, http://www.romecriteria.org//.
References
- 1.Bredenoord AJ. Management of belching, hiccups, and aerophagia. Clin Gastroenterol Hepatol 2013;11:6–12. [DOI] [PubMed] [Google Scholar]
- 2.Pouderoux P, Ergun GA, Lin S, et al. Esophageal bolus transit imaged by ultrafast computerized tomography. Gastroenterology 1996;110:1422–8. [DOI] [PubMed] [Google Scholar]
- 3.Sifrim D, Silny J, Holloway RH, et al. Patterns of gas and liquid reflux during transient lower oesophageal sphincter relaxation: a study using intraluminal electrical impedance. Gut 1999;44:47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bredenoord AJ, Weusten BL, Timmer R, et al. Relationships between air swallowing, intragastric air, belching and gastro-oesophageal reflux. Neurogastroenterol Motil 2005;17:341–7. [DOI] [PubMed] [Google Scholar]
- 5.Kessing BF, Bredenoord AJ, Velosa M, et al. Supragastric belches are the main determinants of troublesome belching symptoms in patients with gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2012;35:1073–79. [DOI] [PubMed] [Google Scholar]
- 6.Tack J, Talley NJ, Camilleri M, et al. Functional gastroduodenal disorders. Gastroenterology 2006;130:1466–79. [DOI] [PubMed] [Google Scholar]
- 7.Drossman DA, Li Z, Andruzzi E, et al. U.S. householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig Dis Sci 1993;38:1569–80. [DOI] [PubMed] [Google Scholar]
- 8.Bredenoord AJ, Weusten BL, Sifrim D, et al. Aerophagia, gastric, and supragastric belching: a study using intraluminal electrical impedance monitoring. Gut 2004;53:1561–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hemmink GJ, Weusten BL, Bredenoord AJ, et al. Aerophagia: excessive air swallowing demonstrated by esophageal impedance monitoring. Clin Gastroenterol Hepatol 2009;7:1127–9. [DOI] [PubMed] [Google Scholar]
- 10.Lin M, Triadafilopoulos G. Belching: dyspepsia or gastroesophageal reflux disease? Am J Gastroenterol 2003;98:2139–45. [DOI] [PubMed] [Google Scholar]
- 11.Conchillo JM, Selimah M, Bredenoord AJ, et al. Air swallowing, belching, acid and non-acid reflux in patients with functional dyspepsia. Aliment Pharmacol Ther 2007;25:965–71. [DOI] [PubMed] [Google Scholar]
- 12.Hemmink GJ, Bredenoord AJ, Weusten BL, et al. Supragastric belching in patients with reflux symptoms. Am J Gastroenterol 2009;104:1992–7. [DOI] [PubMed] [Google Scholar]
- 13.Watson NF, Mystkowski SK. Aerophagia and gastroesophageal reflux disease in patients using continuous positive airway pressure: a preliminary observation. J Clin Sleep Med 2008;4:434–8. [PMC free article] [PubMed] [Google Scholar]
- 14.Bredenoord AJ, Weusten BL, Timmer R, et al. Psychological factors affect the frequency of belching in patients with aerophagia. Am J Gastroenterol 2006;101:2777–81. [DOI] [PubMed] [Google Scholar]
- 15.Karamanolis G, Triantafyllou K, Tsiamoulos Z, et al. Effect of sleep on excessive belching: a 24-hour impedance-pH study. J Clin Gastroenterol 2010;44:332–4. [DOI] [PubMed] [Google Scholar]
- 16.Bredenoord AJ. Excessive belching and aerophagia: two different disorders. Dis Esophagus 2010;23:347–52. [DOI] [PubMed] [Google Scholar]
- 17.Chitkara DK, Bredenoord AJ, Rucker MJ, et al. Aerophagia in adults: a comparison with functional dyspepsia. Aliment Pharmacol Ther 2005;22:855–8. [DOI] [PubMed] [Google Scholar]
- 18.Bredenoord AJ, Smout AJ. Impaired health-related quality of life in patients with excessive supragastric belching. Eur J Gastroenterol Hepatol 2010;22:1420–3. [DOI] [PubMed] [Google Scholar]
- 19.Hemmink GJ, Ten Cate L, Bredenoord AJ, et al. Speech therapy in patients with excessive supragastric belching—a pilot study. Neurogastroenterol Motil 2010;22:24–8, e2–3. [DOI] [PubMed] [Google Scholar]
- 20.Tucker E, Knowles K, Wright J, et al. Rumination variations: aetiology and classification of abnormal behavioural responses to digestive symptoms based on high-resolution manometry studies. Aliment Pharmacol Ther 2013;37:263–74. [DOI] [PubMed] [Google Scholar]
- 21.Zella SJ, Geenens DL, Horst JN. Repetitive eructation as a manifestation of obsessive-compulsive disorder. Psychosomatics. 1998;39:299–301. [DOI] [PubMed] [Google Scholar]
- 22.Jones WR, Morgan JF. Eructophilia in bulimia nervosa: a clinical feature. Int J Eat Disord 2012;45:298–301. [DOI] [PubMed] [Google Scholar]
- 23.Bredenoord AJ, Smout AJ. Physiologic and pathologic belching. Clin Gastroenterol Hepatol 2007;5:772–5. [DOI] [PubMed] [Google Scholar]
- 24.National Institute for Health and Care Excellence. Referral for suspected cancer. CG27. London: National Institute for Health and Care Excellence, 2005. [Google Scholar]
- 25.Kessing BF, Bredenoord AJ, Smout AJ. Mechanisms of gastric and supragastric belching: a study using concurrent high-resolution manometry and impedance monitoring. Neurogastroenterol Motil 2012;24:e573–9. [DOI] [PubMed] [Google Scholar]
- 26.Chiarioni G, Whitehead WE. The role of biofeedback in the treatment of gastrointestinal disorders. Nat ClinPractGastroenterolHepatol 2008;5:371–82. [DOI] [PubMed] [Google Scholar]
- 27.Chitkara DK, Bredenoord AJ, Talley NJ, et al. Aerophagia and rumination: recognition and therapy. Curr Treat Options Gastroenterol 2006;9:305–13. [DOI] [PubMed] [Google Scholar]
- 28.Cigrang JA, Hunter CM, Peterson AL. Behavioral treatment of chronic belching due to aerophagia in a normal adult. Behav Modif 2006;30:341–51. [DOI] [PubMed] [Google Scholar]
- 29.Garcia D, Starin S, Churchill RM. Treating aerophagia with contingent physical guidance. J Appl Behav Anal 2001;34:89–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spiegel SB. Uses of hypnosis in the treatment of uncontrollable belching: a case report. Am J Clin Hypn 1996;38:263–70. [DOI] [PubMed] [Google Scholar]
- 31.Katzka DA. Simple office-based behavioral approach to patients with chronic belching. Dis Esophagus 2012. 10.1111/dote.12006. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 32.Blondeau K, Boecxstaens V, Rommel N, et al. Baclofen improves symptoms and reduces postprandial flow events in patients with rumination and supragastric belching. Clin Gastroenterol Hepatol 2012;10:379–84. [DOI] [PubMed] [Google Scholar]
- 33.Hwang JB, Kim JS, Ahn BH, et al. Clonazepam treatment of pathologic childhood aerophagia with psychological stresses. J Korean Med Sci 2007;22:205–8. [DOI] [PMC free article] [PubMed] [Google Scholar]