Abstract
Objective
Gastrointestinal conditions requiring surgical intervention are becoming increasingly frequent in adults with cystic fibrosis (CF) as life expectancy increases. In addition, patients with CF are at risk of specific gastrointestinal complications associated with their disease. This includes distal intestinal obstruction syndrome (DIOS), which may affect up to 15% of patients, and can present diagnostic and therapeutic challenges. The aim of this study was to determine the nature and frequency of general surgical procedures undertaken in a large cohort of adult CF patients so as to guide future care.
Design
The medical records of all surviving adult CF patients followed at a large tertiary referral centre in the UK were scrutinised and details retrieved on those who had undergone abdominal surgery after the age of 16 years.
Results
A total of 377 patients with CF were identified from the prospectively held database. Thirty-three patients had undergone 43 abdominal operations. The median age at surgery was 22.7 years (range 16–58 years). The three most commonly performed operations were: surgery for DIOS (n=9); cholecystectomy (n=8) and fundoplication (n=6). A past history of surgically treated meconium ileus at birth was a significant risk factor for requiring surgery for DIOS as an adult.
Conclusions
The treatment of DIOS-related complications is one of the main reasons for abdominal surgery in the adult CF population. The general surgical community needs to be increasingly aware of the existence of disease-related gastrointestinal conditions in adult CF patients so that treatment can be optimised.
Keywords: CONSTIPATION, GASTROESOPHAGEAL REFLUX DISEASE, GASTROINTESTINAL BLOOD FLOW, IRRITABLE BOWEL SYNDROME, ANORECTAL DISORDERS
Introduction
Cystic fibrosis (CF) is the commonest life-shortening autosomal recessive disorder seen in Caucasians, with an incidence in the UK of one in 2500 live births.1 2 Survival for CF patients has improved, with the median survival in the UK being 34.4 years. This dramatic change in life expectancy has been brought about by the centralisation of specialist care, advances in medical management of respiratory complications and aggressive nutritional support.3 4 However, as the proportion of patients surviving into adulthood increases, non-respiratory complications such as diabetes and distal intestinal obstruction syndrome (DIOS) are becoming more common.
Adults with CF are more likely than the general population to come into contact with a general surgeon. In addition to those gastrointestinal conditions experienced by the general population, CF patients are at risk of disease-specific gastrointestinal complications. DIOS and its complications is one of the most common reasons for the involvement of a general surgeon. It occurs in over 15% of the adult CF population,5 and is characterised by complete or incomplete obstruction of the small bowel and/or right colon by abnormal viscid mucofaeculent material. Clinical presentation may be chronic with symptoms of recurrent subacute obstruction or emergent with acute small bowel obstruction and signs of peritonism and sepsis.6 7 Initial management in the absence of acute signs is non-surgical with fluid rehydration and combinations of stimulant and osmotic laxatives in an attempt to dislodge the inspissated material and relieve the obstruction.8 With timely and aggressive medical management, the need to resort to surgery is infrequent.6 8 The role of surgery is mainly if medical management fails to control chronic symptoms or in the acute presentation if the patients develops signs of peritonitis and sepsis.9
The aim of this study was to document the nature and frequency of surgical procedures undertaken in adult CF patients for gastrointestinal complaints, so as to better inform the general surgical community about this special cohort of patients who are increasingly likely to come to their attention. This series of patients presented and were treated in a CF centre; however, with increasing longevity, a significant number of presentations may occur in any hospital treating adult patients.
Methods
The Leeds Adult Cystic Fibrosis Unit is a tertiary referral centre in the UK. Details of all patients under follow-up at the unit are prospectively entered into an electronic database, which acts a comprehensive medical record. Any surgical procedure is coded and linked to the patient history. The database was searched for all current patients who had undergone gastrointestinal surgery over the age of 16 years. When necessary, the electronic dataset was supplemented with a review of paper medical records, which were the source of surgical operation notes. Data were collected on patient demographics, genetic mutations, other clinical manifestations of CF, details of presentation, medical management, investigations and surgical procedures. The complete dataset was analysed using SPSS Statistics software, Version 11. The χ2 test was used to determine which factors were likely to be associated with the occurrence of DIOS in adult life.
Results
The database contained details of 377 adult CF patients, of whom 33 (8.8%) had undergone a total of 43 abdominal operations. Of these 33 patients, the median age of diagnosis of CF was 0.2 years (range 0–55 years). The predominant mutation was p.Phe508del (84.8% of mutation 1 and 39.4% of mutation 2). Thirty-one patients (93.9%) had pancreatic insufficiency and were on pancreatic enzyme replacement therapy. Nine patients (27.3%) had CF-related diabetes and seven patients (21.2%) had CF-related liver disease. Ten patients (30.3%) had a history of meconium ileus at birth, with six requiring surgery. Four of these six (66.7%) needed further surgery for DIOS as adults.
The median age at the time of surgery was 22.7 years (range 16–58 years). A range of general surgical procedures was undertaken (figure 1). The three main surgical interventions, accounting for almost half of the operations, were surgery for complications of DIOS (n=9), cholecystectomy (n=8) and fundoplication (n=6).
Figure 1.
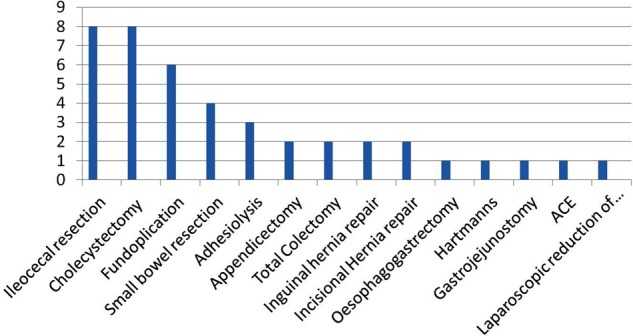
General surgical procedures in adult cystic fibrosis patients.
Operations for general abdominal conditions
The majority of surgical interventions were for abdominal conditions common to the general population. In addition to cholecystectomy and fundoplication, other operations included appendicectomy, inguinal hernia repair and adhesiolysis. Acute appendicectomy can be particularly difficult to differentiate from an acute episode of DIOS. One patient in our series underwent appendicectomy at another institution, with transfer to our unit when symptoms failed to improve. Subsequent CT scan showed classic radiological features of DIOS and the condition settled on appropriate medical management. Total colectomy was required in two patients with inflammatory bowel disease and a Hartmann's procedure for perforated diverticular disease in a 55-year-old patient. Two patients required repair of an incisional hernia.
Operations for conditions related to CF
A variety of operations was undertaken for gastrointestinal complications specific to CF. By far the most common interventions were those undertaken for complications of DIOS. In total, 14 operations were undertaken in 11 patients for treatment of presumed complications of DIOS. Following histopathology analysis, two patients were found to have pathologies other than DIOS. Therefore, out of our whole cohort of 377 patients, nine (2.4%) patients underwent a total of 12 operations for DIOS. All nine patients had previously been diagnosed and treated for DIOS, and included six women. All patients had at least one p.Phe508del mutation, with 63.6% being homozygous. All patients had pancreatic insufficiency and were on pancreatic enzyme replacement. None of the patients had CF-associated liver disease.
Presenting symptoms included abdominal pain, vomiting and constipation. A mass was palpable in the right iliac fossa in six patients. Six patients had a history of meconium ileus at birth, with four requiring surgery as a neonate. A history of surgically treated meconium ileus at birth was associated with an increased risk of requiring surgery for DIOS in adult life on univariate analysis (χ2 test, p<0.05).
Six patients presented acutely and after resuscitation and a trial of medical management went on to surgery. Five patients presented with chronic symptoms and required surgery for DIOS resistant to medical management.
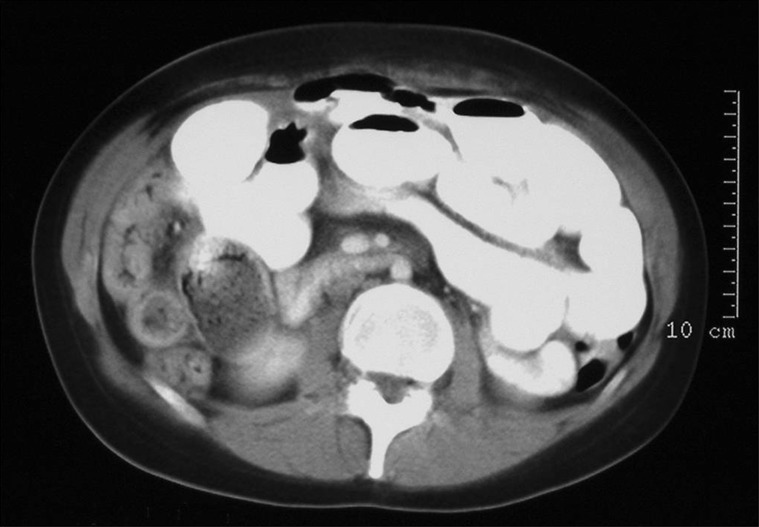
All patients were investigated by CT scan of the abdomen. Nine CT scans showed impacted faeces in the small bowel and/or colon with proximal bowel dilatation, consistent with DIOS (figure 2). One CT scan showed a small bowel inflammatory mass with faecal loading, which was initially thought to be DIOS, but subsequently proven to be Crohn's disease. A further CT scan showed small bowel intussusception and faecal loading attributable to DIOS, but was subsequently shown to be secondary to Yersinia infection (figure 3).
Figure 2.
Impacted faeces and small bowel dilatation consistent with DIOS.
Figure 3.
Small bowel intussusception.
The median age at the time of first surgery for DIOS was 21 years (range 16–24.1 years). The most common procedure undertaken, in both the acute and chronic setting, was resection of the affected bowel segment either as an ileo-colic/right hemicolectomy or as a small bowel resection. Attempts at bowel preservation, by performing enterotomy with lavage, were largely unsuccessful due to the viscosity of the faecal material that sticks avidly to the bowel mucosa (figure 4). Other attempts at bowel preservation in the chronic setting included procedures for antegrade colonic lavage. In one notable success this was achieved by means of ileal segment exteriorisation due to the patient having undergone earlier appendicectomy.10
Figure 4.

Thick mucofaeculent material in distal intestinal obstruction syndrome.
There was no mortality, but three patients had delayed discharge due to respiratory complications.
The median length of follow-up was 6.42 years (range 2.58–14.83 years). Re-operation for further complications of DIOS was required in three patients (33%); two small bowel resections and one ileo-caecectomy. At last follow-up, six patients were asymptomatic and not requiring laxatives, two patients were controlling their symptoms with regular laxatives, and one patient who had undergone right hemicolectomy had chronic diarrhoea secondary to bile salt malabsorption.
Discussion
Appreciation of the gastrointestinal manifestations of CF is becoming increasingly important as the proportion of patients surviving into adulthood increases. The spectrum of disease encompasses almost every gastrointestinal organ,3 but in our series by far the most common conditions requiring surgery were complications of DIOS, gall bladder disease and gastro-oesophageal reflux.
CF patients appear to develop hepatobiliary disease earlier than the general population, and may have cholelithiasis, gall bladder dyskinesia, micro-gallbladder and atretic cystic duct.11 Cholelithiasis is believed to be particularly common, affecting between 6% and 28% of patients,12 although only 4% are believed to be symptomatic.13 Cholecystectomies comprised 18.6% of operations in our series, which is similar to rates of 26.5% reported by others.14 Laparoscopic cholecystectomy can be safely performed provided the usual arrangements are made to optimise postoperative recovery, ie, good postoperative rehydration, non-constipating analgesics, chest physiotherapy, early mobilisation and nutritional support with pancreatic enzyme replacement as necessary.
Gastro-oesophageal reflux disease is very common in CF patients, with one study reporting an incidence of 62% in 500 children investigated by pH studies.15 This is reflected in our series, with fundoplication being one of the three most frequent operations performed. While many patients are well controlled on medical management, others can experience failure to thrive with progressive decline in lung function.16 In addition to the control of reflux symptoms, fundoplication plays a role in halting the advancement of Barrett's oesophagus with its inherent malignant potential. Indeed, one patient in our series required an Ivor Lewis oesophagectomy for oesophageal cancer.
CF carries an increased risk of gastrointestinal and pancreatic malignancies.17–19 These occur at an earlier age20 and their incidence, along with other malignancies, increases following lung transplantation and immunosuppression.21 In addition to the patient who developed oesophageal cancer, we are aware of two patients with hepatobiliary carcinoma and one patient with small bowel carcinoma; these patients did not undergo surgery within the time frame of the current study.
As the adult population with CF tends to be relatively young, consideration should always be given to gastrointestinal pathology commonly encountered in this age group. In the acute situation, this includes acute appendicitis in patients presenting with lower abdominal pain, while in the chronic situation, pain and a mass in the right iliac fossa may be indicative of underlying Crohn's disease. In our series, one patient with DIOS turned out to have Crohn's disease. With the benefit of hindsight, the patient with Crohn's disease might have been diagnosed preoperatively given the finding of an inflammatory mass on CT scan, but it is likely that surgery would have been necessary in any event. The incidence of Crohn's disease is believed to be slightly increased in CF,22 while that of appendicitis is actually lower compared with the general population, with incidences of 1.5% and 8.6%, respectively.23 Both conditions are readily confused with an acute episode of DIOS.5 8 24 A CT scan is probably the most useful investigation, but in patients with DIOS the appendix is often markedly thickened, as is the affected segment of terminal ileum, making reliance on radiology a potential diagnostic trap.
Intussusception occurs in 1–2% of adult CF patients and is commonly ileo-colic, although ileo-ileal, caeco-colic and colo-colic presentations occur.5 24 Symptoms may be intermittent, with colicky abdominal pain and a mass in the right iliac fossa, making differentiation from DIOS difficult. Indeed, the thickened mucous and tenacious faeces are believed to act as the lead point for intussusception. However, intussusception can usually be readily differentiated on CT scan5 24 (figure 3).
DIOS is an increasing cause of morbidity in the adult CF population. It usually presents with symptoms of subacute small bowel obstruction and is most reliably diagnosed on CT scan, with classic features of faecal loading in the terminal ileum and right colon, thickening of the distal small bowel wall, proximal bowel dilatation and in the absence of any other mechanical obstruction. Aggressive medical management is usually successful in alleviating acute episodes, but close monitoring by specialist physicians is required. The development of local signs of sepsis with peritonism, pyrexia and raised white cell count should precipitate an urgent surgical opinion, as in a minority DIOS will be resistant to medical management and surgery will be required.
Although surgery for DIOS is not often required, it still forms one of the largest categories of surgical intervention undertaken in adult CF patients. In our series, only nine of 377 patients (2.4%) underwent surgery for complications of DIOS. Approximately half of these interventions were performed in the acute setting. Over the years, a variety of surgical approaches has been tried. In the acute setting, enterotomy and lavage has largely been abandoned in favour of resection of the affected bowel segment. In the authors’ opinion, the use of colonoscopy to clear the bowel is futile, given the viscosity of the occluding material, although it is accepted that this option has been described elsewhere.25 As the terminal ileum, caecum and ascending colon are most often affected, resection usually takes the form of an ileocaecectomy or right hemicolectomy, depending on the extent of colonic involvement, although on occasion small bowel resection alone has been possible. Patients with DIOS are known to have prolonged oro-caecal transit times,26 and inclusion of the ileocaecal valve in the resection specimen may help to normalise transit and so reduce the risk of future episodes of DIOS. The extent of resection is often difficult to determine as there is a tendency for impacted faeces to extend proximally up the small bowel. Too extensive a resection will put the patient at risk of vitamin B12, folate and iron deficiency, together with deficiency of the fat-soluble vitamins. It may also precipitate chronic diarrhoea from bile salt malabsorption. We have adopted a policy of closely inspecting the bowel at operation to determine which segment is most responsible for the obstruction. We do not attempt to resect all small bowel containing faeculent content as this is unnecessary. Rather, it is more important that the distal extent of the obstruction is cleared so that safe primary anastomosis can be achieved. We have never resorted to a stoma, even in the immunosuppressed patient, although this is an option if the patient is septic or unstable. It is the authors’ preference to perform a stapled side-to-side anastomosis with a wide anastomotic lumen in an attempt to minimise future DIOS episodes. With this policy, all but one of our patients have managed their bowels satisfactorily, albeit it with approximately half still requiring regular laxatives; only one patient has developed chronic diarrhoea due to bile salt malabsorption. In the elective setting, segmental resection remains the preferred surgical option, although success has been achieved with an ACE procedure for DIOS resistant to medical management.10 27
A previous history of surgical treatment for meconium ileus was a significant risk factor for DIOS-related surgery in adult life in our series. This is consistent with reports from others,28 and may reflect a more aggressive form of the disease.29 All patients in our series who underwent surgery for DIOS had pancreatic insufficiency and were on pancreatic enzyme replacement. Interestingly, our cohort did not contain any patients with fibrosing colonopathy. This condition is characterised by a stricturing process, usually involving the right colon. It is associated with high-dose pancreatic enzyme supplementation, but has also been reported with low-dose preparations. The incidence of pancreatic insufficiency is known to be higher in CF patients with DIOS, although there is no correlation between the dose of pancreatic replacement30 and DIOS severity.
Traditionally, CF patients have been treated in dedicated centres; however, the increasing median age is likely to result in patients presenting to non-specialty centres with surgical issues. Pulmonary manifestations of CF are the predominant cause of morbidity and mortality and may be exacerbated in the perioperative period.31 Thorough pulmonary evaluation including respiratory symptoms, exercise tolerance and pulmonary function testing is essential before surgery. Viscid mucous secretions with reduced mucociliary clearance can lead to atelectasis, airway inflammation and a risk of infection. Awareness of these complications, along with perioperative chest physiotherapy including breathing exercises, flutter valves and chest percussion, may avoid complications.32 It is essential to maintain minimum ventilatory depression during anaesthesia with early tracheal extubation. Postoperative pain management to facilitate early mobilisation, and chest physiotherapy is also essential.31
Conclusion
The proportion of CF patients surviving into adulthood is increasing. The general surgeon needs to be aware of the range of conditions with which these patients can present. These include gastrointestinal complaints common to the general population as well as disease-related pathologies. The most frequently performed surgical interventions are those for complications of DIOS, gall bladder disease and fundoplication for gastroesophageal reflux.
Key messages.
What is already known on this topic
There is improved survival in CF patients.
DIOS may occur in up to 15% of the adult CF population.
What this study adds
Most frequently performed surgical interventions in adult CF patients are for complications of DIOS, gall bladder disease and fundoplication for gastroesophageal reflux.
How might it impact on clinical practice in the foreseeable future
General surgeons will increasingly need to be aware of the abdominal manifestations of CF in order to optimise outcomes.
Footnotes
Contributors: Initial concept: DJ and DP; data collection: AS and AM; data analysis: AS, AM, DP amd DJ; manuscript preparation and editing: AS, AM, DP and DJ.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hanosh A, FitzSimmons SC, Macek M, et al. Comparison of the clinical manifestations of cystic fibrosis in black and white patients. J Pediatric 1998;132:255–9. [DOI] [PubMed] [Google Scholar]
- 2.Cystic Fibrosis Trust. UK CF Registry Annual Data Report 2009, Cystic Fibrosis Trust, Kent, 2011. [Google Scholar]
- 3.Barr HL, Britton J, Smyth AR, et al. Association between socioeconomic status, sex, and age at death from cystic fibrosis in England and Wales (1959 to 2008): cross sectional study. BMJ 2011. Aug 23;343d4662. 10.1136/bmj.d4662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilschanski M, Durie PR. Patterns of GI disease in adulthood associated with mutations in the CFTR gene. Gut 2007;56:1153–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agrons GA, Corse WR, Markowitz RI, et al. Gastrointestinal manifestations of cystic fibrosis: radiologic–pathologic correlation. Radiographics 1996;16:871–93. [DOI] [PubMed] [Google Scholar]
- 6.Dray X, Bienvenu T, Desmazes-Dufeu N, et al. Distal intestinal obstruction syndrome in adults with cystic fibrosis. Clin Gastroenterol Hepatol 2004;2:498–503. [DOI] [PubMed] [Google Scholar]
- 7.Colombo C, Ellemunter H, Houwen R, et al. ECFS. Guidelines for the diagnosis and management of distal intestinal obstruction syndrome in cystic fibrosis patients. J Cyst Fibros 2011;10(Suppl. 2):S24–8. [DOI] [PubMed] [Google Scholar]
- 8.van der Doef HP, Kokke FT, van der Ent CK, et al. Intestinal obstruction syndromes in cystic fibrosis: meconium ileus, distal intestinal obstruction syndrome, and constipation. Curr Gastroenterol Rep 2011;13:265–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Speck K, Charles A. Distal intestinal obstructive syndrome in adults with cystic fibrosis: a surgical perspective. Arch Surg 2008;43:601–3. [DOI] [PubMed] [Google Scholar]
- 10.Clifton IJ, Morton AM, Ambrose NS, et al. Treatment of resistant distal intestinal obstruction syndrome with a modified antegrade continence enema procedure. J Cyst Fibros 2004;3:273–5. [DOI] [PubMed] [Google Scholar]
- 11.Roy CC, Weber AM, Morin CL, et al. Hepatobiliary disease in cystic fibrosis: a survey of current issues and concepts. J Pediatr Gastroenterol Nutr 1982;1:469–78. [DOI] [PubMed] [Google Scholar]
- 12.Cogliandolo A, Patania M, Currò G, et al. Postoperative outcomes and quality of life in patients with cystic fibrosis undergoing laparoscopic cholecystectomy: a retrospective study. Surg Laparoec Endosc Percutan Tech 2011;21:179–83. [DOI] [PubMed] [Google Scholar]
- 13.Stern RC, Rothstein FC, Doershuk CF. Treatment and prognosis of symptomatic gallbladder disease in patients with cystic fibrosis. J Pediatr Gastroenterol Nutr 1986;5:35–40. [DOI] [PubMed] [Google Scholar]
- 14.Saltzman DA, Johnson EM, Feltis BA, et al. Surgical experience in patients with cystic fibrosis: a 25-year perspective. Pediatr Pulmonol 2002;33:106–10. [DOI] [PubMed] [Google Scholar]
- 15.Andze GO, Brandt ML, St Vil D, et al. Diagnosis and treatment of gastroesophageal reflux in 500 children with respiratory symptoms: the value of pH monitoring. J Pediatr Surg 1991;26:295–9; discussion 299–300. [DOI] [PubMed] [Google Scholar]
- 16.Button BM, Roberts S, Kotsimbos TC, et al. Gastroesophageal reflux (symptomatic and silent): a potentially significant problem in patients with cystic fibrosis before and after lung transplantation. J Heart Lung Transplant 2005;24:1522–9. [DOI] [PubMed] [Google Scholar]
- 17.Schöni MH, Maisonneuve P, Schöni-Affolter F, et al. Cancer risk in patients with cystic fibrosis: the European data. CF/CSG Group. J R Soc Med 1996;89:38–43. [PMC free article] [PubMed] [Google Scholar]
- 18.Maisonneuve P, Marshall BC, Lowenfels AB. Risk of pancreatic cancer in patients with cystic fibrosis. Gut 2007;56:1327–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johannesson M, Askling J, Montgomery, et al. Cancer risk among patients with cystic fibrosis and their first-degree relatives. Int J Cancer 2009;125:2953–6. [DOI] [PubMed] [Google Scholar]
- 20.Neglia JP, FitzSimmons SC, Maisonneuve P, et al. The risk of cancer among patients with cystic fibrosis. Cystic Fibrosis and Cancer Study Group. N Engl J Med 1995;332:494–9. [DOI] [PubMed] [Google Scholar]
- 21.Maisonneuve P, FitzSimmons SC, Neglia JP, et al. Cancer risk in nontransplanted and transplanted cystic fibrosis patients: a 10-year study. J Natl Cancer Inst 2003;95:381–7. [DOI] [PubMed] [Google Scholar]
- 22.Lloyd-Still JD. Crohn's disease and cystic fibrosis. Dig Dis Sci 1994;39:880–5. [DOI] [PubMed] [Google Scholar]
- 23.Shields MD, Levison H, Reisman JJ, et al. Appendicitis in cystic fibrosis. Arch Dis Child 1991;66:307–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Robertson MB, Choe KA, Joseph PM. Review of the abdominal manifestations of cystic fibrosis in the adult patient. Radiographics 2006;26:679–90. [DOI] [PubMed] [Google Scholar]
- 25.Shidrawi RG, Murugan N, Westaby D, et al. Emergency colonoscopy for distal intestinal obstruction syndrome in cystic fibrosis patients. Gut 2002;51:285–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dalzell AM, Heaf DP. Oro-caecal transit time and intra-luminal pH in cystic fibrosis patients with distal intestinal obstruction syndrome. Acta Univ Carol Med 1990;36:159–60. [PubMed] [Google Scholar]
- 27.Stanton MP, Shin YM, Hutson JM. Laparoscopic placement of the Chait cecostomy device via appendicostomy. J Pediatr Surg 2002;37:1766–7. [DOI] [PubMed] [Google Scholar]
- 28.Morton JR, Ansari N, Glanville AR, et al. Distal intestinal obstruction syndrome (DIOS) in patients with cystic fibrosis after lung transplantation. J Gastrointest Surgn 2009;13:1448–53. [DOI] [PubMed] [Google Scholar]
- 29.Blackman SM, Deering-Brose R, McWilliams R, et al. Relative contribution of genetic and nongenetic modifiers to intestinal obstruction in cystic fibrosis. Gastroenterology 2006;131:1030–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baker SS, Borowitz D, Duffy L, et al. Pancreatic enzyme therapy and clinical outcomes in patients with cystic fibrosis. J Pediatr 2005;146:189–93. [DOI] [PubMed] [Google Scholar]
- 31.Huffmyer JL, Littlewood KE, Nemergut EC. Perioperative management of the adult with cystic fibrosis. Anesth Analg 2009;109:1949–61. [DOI] [PubMed] [Google Scholar]
- 32.Yankaskas JR, Marshall BC, Sufian B, et al. Cystic fibrosis adult care: consensus conference report. Chest 2004;125(1 Suppl.):1S–39S. [DOI] [PubMed] [Google Scholar]