Abstract
Background
A nurse practitioner-led dysphagia service was introduced to improve appropriateness of investigations.
Objective
To determine the clinical outcomes and efficacy of this service.
Design and patients
A 7-year prospective audit of the first 2000 patients referred for investigation of dysphagia.
Setting
Royal Cornwall Hospitals NHS Trust.
Intervention
An innovative nurse practitioner-led telephone dysphagia hotline (DHL) assessment service for all patients and consultant review following investigation prior to discharge.
Outcomes
Clinical outcomes, service efficiency and cost effectiveness.
Results
2000 patients (median age 70 years, 48% male) were referred in less than 7 years, 1775 being managed fully through the DHL. 67% patients had gastroscopy only, 13% barium swallow only and 8.8% both and 11.2% had no investigation. Reflux was the commonest cause (41.3%), 9% had peptic stricture, 10% malignancy 1.9% pharyngeal pouches and 0.8% achalasia. The did not attend rate was reduced from 3.9% to 1.1% and 151 patients either refused or did not require investigation saving a potential £53 040. Although some patients with pharyngeal pouches had gastroscopy as initial investigation, no complications resulted.
Conclusions
The nurse practitioner-led DHL service has improved efficiency and resulted in a safe prompt service to patients.
Keywords: Dysphagia, Endoscopy, Health Service Research, Oesophageal Cancer
Introduction
Dysphagia is common, affecting 5%–8% of the population over 50 years.1 There are multiple possible aetiologies, both benign and malignant. It is therefore a criterion for referral under the 2-week fast track system for suspected cancer in the UK2 and one most commonly associated with malignancy. Of patients with dysphagia, 12.2% have a final diagnosis of cancer.3 Because there are many potential aetiologies for dysphagia, it is essential that an adequate history and appropriate investigation is performed to ensure optimal patient management rather than simply gastroscopy to exclude upper gastrointestinal malignancy.
Up to 15% of those referred with dysphagia do not actually have dysphagia,3 which we defined as ‘the sensation of food or drink sticking within 5 seconds of swallowing’. Commonly they have reflux, odynophagia or globus, a foreign body sensation at the pharyngeal level independent of swallowing, rarely associated with malignant disease.4 A further concern is that dysphagia may be the presenting feature of a pharyngeal pouch. A gastroscopy performed by an unwary endoscopist can result in oesophageal perforation.5
Many endoscopy units struggle to meet increasing demands, such as those resulting from bowel cancer screening, while maintaining short waiting times. Ensuring that only appropriate patients are referred for gastroscopy and reducing the number of patients who fail to attend for gastroscopy (did not attend (DNA)), improves endoscopy unit efficiency and shortens waiting lists.
Consequently, we introduced a nurse-practitioner-led dysphagia hotline (DHL), a telephone consultation and triage service to ensure right test first time and improving endoscopy unit efficiency. The DHL incorporates gastroscopy and/or barium swallow as appropriate and postprocedural review and management plan by a gastroenterology consultant. The service was introduced in April 2004 following a 6-month pilot and consultations with primary care colleagues.
The aim of this prospective audit was to determine the clinical outcomes and efficiency of the service for the first 2000 referrals.
Methods
Setting up the service
Local Primary health providers were informed of the DHL by email and by discussion at GP forums.
Telephone consultation and triage were performed by gastroenterology consultants or registrar (HRD, IAM, ED) during the pilot phase, and then by our nurse endoscopist (CW) in one of her non-endoscopy sessions. Training was given by supervising telephone consultations for 2 weeks and then by discussion of outcomes for the next 6 months and thereafter for difficult cases only. This required approximately 15 min consultant time weekly for 6 months, and then discussion of less than one case per 3 months. Our (full-time) nurse endoscopist performs 5.5 endoscopy sessions weekly and two telephone clinics weekly.
All patients with confirmed or suspected malignancy are discussed at our weekly upper gastrointestinal cancer multi-disciplinary meeting. All patients discuss and agree their management plan with a gastroenterology consultant on the day of their investigations and a letter is sent to their referrer. When the nurse endoscopist (or patient) decides that further investigations are not required, the telephone consultation information is reviewed by a consultant gastroenterologist and the referring clinician is informed by letter.
Running the service
The majority of patients are referred to the DHL using a 4-question specific referral fax form (see online supplementary appendix 1). Other referrals for patients with dysphagia including 2-week wait referrals, standard primary and secondary care referrals are also managed through the DHL.
Patients have a telephone consultation either at home or by mobile phone (our endoscopy booking team contact patients to make suitable contact arrangements), within a week of referral. A standardised 11-question proforma is used to obtain a symptom specific history (see online supplementary appendix 2), the nature of investigation is discussed and the patient agrees an appointment for investigation within the required three working days (unless deferred for personal reasons).
Initially, barium swallow was offered to all patients with pharyngeal level dysphagia, although after reviewing the age range of patients diagnosed with pharyngeal pouches after the first 12 months, this was revised to only those over the age of 55, presenting with pharyngeal level dysphagia (younger patients have gastroscopy). However, barium swallow is also offered to those patients declining gastroscopy or if the history indicates a probable neurological aetiology, for example, following stroke, especially if predominantly to liquids.6 Barium swallows are reported on immediately and patients see a gastroenterology consultant with their results. If a barium swallow is abnormal, or at the clinician's discretion, patients have a gastroscopy on the same day. They firstly have diet coke and metoclopramide to clear barium from the upper gastrointestinal tract7
Data collection and analysis
We prospectively collected information for all patients referred to the DHL at Royal Cornwall Hospital from April 2004 to January 2011. This included demographic data (age and sex, etc) and clinical details (procedures performed, outcomes and final diagnosis). All 2000 referrals were audited and differences in waiting times and attendance for procedures for other symptomatic patients referred to our service over the same time period were observed.
Comparison between groups used the χ2 test with a p value <0.05 considered statistically significant.
Follow-up of barium swallow patients
We telephoned those patients who had only had a barium swallow 9–53 months following their initial investigation to determine ongoing symptoms, medication, whether any further investigations for dysphagia had been performed and whether any new diagnoses had been made. Data from the telephone consultation, the procedure results and histology, together with the clinician's final diagnosis, are prospectively collected on a purpose built Excel spreadsheet.
Patient satisfaction
In 2008, we asked 25 consecutive patients to complete and return a patient satisfaction questionnaire, with questions relating to their demographics, their satisfaction with their referral, hospital contact and the service in general.
Ethics
Ethics approval was given by our local ethics committee for the telephone follow-up review of barium swallow patients and for the patient satisfaction questionnaire. The ethics committee confirmed approval was not required for the remainder of the study as it was a service audit.
Results
Patient demographics
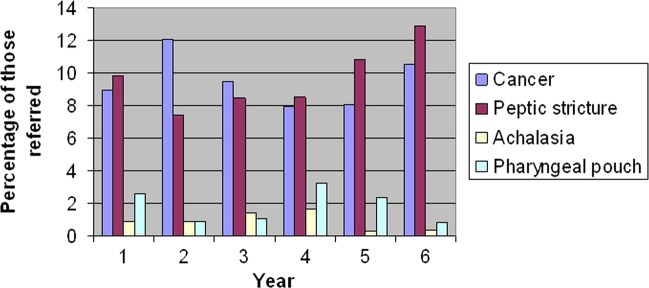
In all, 2000 patients (969 male, median age 70 years, range 17–103 years) were referred to the DHL over 7 years, with little variation between years in numbers referred (figure 1). Of these, 1775 were managed through the DHL. Those not assessed through the DHL are shown in table 1.
Figure 1.
Investigations performed on the first 2000 referrals to the Dysphagia hotline.
Table 1.
Patients referred to the DHL but not investigated by this route
| Reason | Number | Percentage of total referrals (%) |
|---|---|---|
| Unable to contact by phone | 35 | 1.8 |
| Admission for investigation before DHL completed | 31 | 1.6 |
| Refused investigation | 112 | 5.6 |
| Death | 3 | 0.2 |
| Left county | 3 | 0.2 |
| Investigations not indicated or outpatient review required | 39 | 1.9 |
| Data incomplete | 2 | 0.1 |
| Total | 225 |
DHL, dysphagia hotline.
Investigations
The number of referrals averaged 292 per annum or 5.6 per week (range 234–349 per annum). Of the patients referred, 67% had gastroscopy only, 13% barium swallow only, 8.8% both and 11.2% underwent no investigations. In the first year of the DHL, 26.1% had barium swallow only; however, this decreased in subsequent years to between 8.1% and 12.9% of referrals (figure 1).
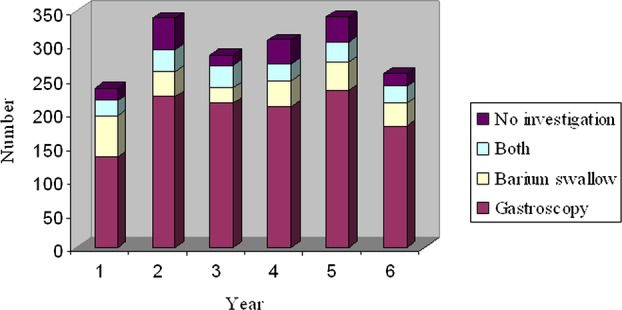
Diagnosis
The commonest diagnosis throughout was gastro-oesophageal reflux disease (n=826: 41.3%), although peptic stricture and malignancy accounted for 9% (n=179) and 10% (n=199) of patients, respectively. A total of 38 patients had pharyngeal pouches (1.9%) and 16 achalasia (0.8%). Some patients had more than one diagnosis including two with both a pharyngeal pouch and oesophageal cancer. The major pathology found varied little on an annual basis (figure 2).
Figure 2.
Major findings on investigation.
Timeliness
The time from referral to first diagnostic test during the first 7 years of the service was 8–13 days. Prior to the DHL, the mean time to investigation for dysphagic patients was 33 days. The maximum waiting time for patients awaiting gastroscopy reduced from 18 months in 2004 to 6 weeks in 2009.
Inappropriate referrals
The number of patients referred without dysphagia was relatively constant throughout the study period. Malignancy was less common in those without dysphagia than those with dysphagia (5.2% vs 11.9%, p<0.05).8 In all, 19.4% of those referred denied dysphagia. The most common indication for inappropriate referral was globus. Other patients had pharyngitis. Some patients had dyspepsia and different alarm symptoms but not dysphagia. All patients were managed according to their symptoms. For those without dysphagia 75.1% had gastroscopy only, 14.2% barium swallow alone, 2.9% both and 7.8% no investigation.
Non-attendance
Of those who agreed to an investigation, 20 (1.1%) in total failed to attend; of these, seven barium swallows, nine gastroscopies and four were unspecified. This compares with the DNA rate for our patients referred for diagnostic endoscopy of 3.4%–5.0% over the entire study period. This rate has not improved despite the introduction of direct booking and improved clerical and clinical validation, and has never been below that of the DHL.
Patient satisfaction
Overall, 17 patients (68%) returned their questionnaire (seven female patients, average age 65.8 years). One thought that they were not seen soon enough. The majority of patients preferred a telephone consultation or had no preference but 24 (n=4) would have preferred a face-to-face consultation. All were highly satisfied or satisfied with telephone consultation, investigation appointment and their follow-up arrangements.
Pharyngeal pouches
In all, 38 patients (1.8%) had pharyngeal pouches. In several cases, a second diagnosis was made which included two patients with both pharyngeal pouch and oesophageal cancer. Of these 38 patients, 33 had a barium swallow as their first line of investigation. Patients with pharyngeal pouches were aged between 58–93 years and most, though not all, had pharyngeal level dysphagia; however, 16% (n=6) described mid-sternal dysphagia. The endoscopist was successful in intubating two of the five patients who had gastroscopy as their initial investigation, the remainder having a barium swallow. No patients either with or without a pharyngeal pouch had any complications, such as perforation or bleeding as a result of diagnostic gastroscopy in the DHL.
After the first year of the DHL, we noted that of the six patients diagnosed with pharyngeal pouch the youngest was 73 years old.
Barium swallow only patients
We attempted to contact the first 126 patients who had barium swallow alone, 9–53 months following their initial investigation. Six patients had died, none through oesophageal pathology, and 83 were successfully contacted (49 female subjects, mean age 71.7 years, range 24–96 years). Of these patients, 49 patients (59.0%) remained symptomatic, 15 were taking proton pump inhibitors (18.1%), and four had had gastroscopies for dysphagia (4.8%). One patient, a 91-year-old man with dementia, had a new diagnosis of oesophageal adenocarcinoma made 9 months after initial investigation (cricopharyngeal spasm on initial barium swallow). Initially he had progressive dysphagia for 8 weeks at the pharyngeal level, with reflux and possible weight gain. The tumour on gastroscopy was at the gastro-oesophageal junction and was not visible on subsequent review of initial fluoroscopy.
Cost effectiveness
The 2010/2011 HRG4 tariff for outpatient diagnostic upper gastrointestinal endoscopy is £255 and £166.52 for barium swallow.9 The potential savings released by reducing the DNA rate from a mean of 3.9% to 1.1% is £14 535 over 7 years (£2076 per annum). However, 151 patients had no investigation either because their symptoms did not warrant investigation or had resolved or through their own choice. Had they received and failed to attend gastroscopy appointments then the DHL has released another £38 505 of savings (£5501 per annum). If all patients had had gastroscopy, the additional number of gastroscopy appointments per annum required is 69. The DHL has therefore improved access to the service for other symptomatic and surveillance patients.
Only those patients presenting with other symptoms, for example, unexplained dyspepsia, or with conditions such as cancer or peptic stricture, require follow-up because they have been seen, assessed and discharged by a consultant gastroenterologist with access to a detailed history of their dysphagia. It was difficult to quantify this reduction in medical clinic follow-up appointments as we had not audited our practice beforehand.
The nurse practitioner performed 0–10 telephone consultations weekly (median 5.0) and maintained the database. The radiology department provided two slots (initially 3) per week which were filled by other patients if not required and the endoscopy unit four slots for DHL patients, again filled by others if not required. Some flexibility was required if we received more referrals in any week. The consultant review was performed by one of two consultants performing an endoscopy list during patient turnover, and no reduction in list size was necessary. When patients had an abnormal barium swallow or if their history indicated that a gastroscopy was required despite a normal barium swallow result, then the list duration was lengthened to accommodate them.
Discussion
The DHL, a nurse-practitioner led telephone consultation service and investigation have enabled excellent outcomes in terms of both safety and efficacy. Overall, 88.8% of patients referred were phoned at a suitable time and place and appropriate investigations organised within 2 weeks of referral, with minimal disruption to the radiology and endoscopy services. The DHL also helps reduce demand on the endoscopy service by 8.5% of referrals, by not giving appointments for gastroscopy to patients who refuse investigation or do not require it. By agreeing an investigation time with the patient, the DNA rate was reduced from 3.9% to 1.1%, reducing costs and improving efficiency. This is similar to the reduction in DNA rate achieved by nurse led preassessment for surveillance colonoscopy patients.10
The referral rate for the DHL service has varied little since the inception of the DHL service, averaging 5.6 referrals per week for a service covering a population of 450 000. However, there is a weekly variation in numbers of referrals (from 0 to 10) requiring flexibility within both the radiology and endoscopy services. It has been relatively easy to fill any unused appointment slots with other referrals, both urgent outpatients and inpatients.
As shown previously,10 telephone preassessment identifies patients with more complex needs, for example, taking anticoagulants and diabetics, and ensures appropriate management of these patients, reducing delays on the day of investigation.
The continuing number of inappropriate referrals (19.4%) despite a specific referral proforma and GP education and feedback is disappointing. Similar issues with 15.2% of inappropriate referrals have been noted previously with dysphagia referrals and further highlight the need for preassessment before arranging invasive investigations for all.3 Some ‘inappropriate’ patients had globus or pharyngitis and had a low incidence of significant pathology while others had other alarm symptoms, for example, dyspepsia and weight loss. It is unclear whether patients changed their history or if Primary Care colleagues appreciated the ease of access, assessment, investigation and management plans provided through the DHL. It could be argued that patients with globus do not require any investigations as a retrospective review of 1145 barium swallow reports of patients with globus failed to diagnose malignancy.4 This would further reduce the costs of investigation and service pressures.
We investigate many patients with pharyngeal level dysphagia who traditionally may have seen by our ENT colleagues. Because of the difficulty of auditing referrals prior to the introduction of the DHL (they may have had multiple routes of access to the gastrointestinal services) it is impossible to determine if the DHL increased the numbers of such referrals. However, we noted a similar percentage of malignancy for patients presenting with pharyngeal level dysphagia compared with those with more distal dysphagia although others have not.11 There is also increasing recognition of eosinophilic oesophagitis as a cause of pharyngeal level dysphagia and the investigation of choice for this condition is a gastroscopy with biopsies taken from multiple levels throughout the oesophagus.12 Hence patients with pharyngeal level dysphagia were appropriately seen and investigated in the DHL.
The percentage of patients presenting to the DHL and found to have pharyngeal pouches was higher than expected. After the first year, we investigated patients with pharyngeal level dysphagia under 55 years old by gastroscopy rather than barium swallow to reduce inefficiencies.8 Several patients with pharyngeal pouches had a gastroscopy rather than a barium swallow for their initial investigation. The main reason for this was presentation only with mid-sternal dysphagia and it demonstrates the need for the endoscopist to be wary of intubating all patients of this age group presenting with dysphagia, even when not classically pharyngeal in site.
It has been recognised previously that barium swallow alone cannot be relied upon to exclude oesophageal malignancy13 although it provides a better functional assessment of oesophageal motility. We found a single 91-year-old patient re-presenting 9 months after his original barium swallow with distal oesophageal adenocarcinoma. This was not visible on review of the original fluoroscopy films and we do not know if it would have been visible 9 months previously at gastroscopy. A negative barium swallow does not necessarily exclude malignancy and a gastroscopy may be appropriate in selected cases. We do not know whether any patients who had gastroscopy alone were subsequently diagnosed with oesophageal malignancy.
The most surprising outcome of our service review has been the number of patients who have refused investigation or who do not require gastroscopy or barium swallow. By avoiding direct-to-test gastroscopy the health community has potentially saved £53 040 (£7577 PA), and our service efficiency is improved by reducing non-attendance.
In conclusion, we have demonstrated that investment in a nurse practitioner-led telephone preassessment service for patients referred with dysphagia and minor changes in the arrangement of our endoscopy and radiology services has enabled a safe, prompt and highly efficient service for these patients.
What is already known on this topic.
Dysphagia is common and is often due to malignancy
Gastroscopy is not always the best investigation or acceptable to all patients
Improving endoscopy unit efficiency is essential to enable units to meet increasing demands
What this study adds.
A nurse-led telephone assessment service for patients with dysphagia is safe and appreciated by patients.
It reduces costs by reducing DNA rates by up to 80%
It ensures that investigations are appropriate and acceptable to patients How might it impact on clinical practice in the foreseeable future
This and other nurse-led pre-assessment clinics will ensure right patient right place first time
Such nurse-led services will improve unit efficiency and safety
Supplementary Material
Acknowledgments
We gratefully acknowledge the assistance of the late Dr Richard Farrow, Consultant Radiologist, in setting up this service.
Footnotes
Contributors: IAM, HRD, RF and GM developed the dysphagia hotline; CW obtained the data and maintained the database; EJD contributed to the initial running and development of the service; JP analysed the data; IAM wrote the paper and HRD and JP extensively edited it; all authors reviewed and agreed with the final version. IAM is responsible for the overall content as guarantor.
Funding: None.
Competing interests: None.
Ethics approval: Cornwall and Plymouth Ethics Committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Lindgren MD, Janzon L. Prevalence of swallowing complaints and clinical findings among 50–79 year old men and women in an urban population. Dysphagia 1991;6:187–92. [DOI] [PubMed] [Google Scholar]
- 2.Health Service Circular 205. Cancer waiting times. Achieving the two week target. London: NHS Executive, 1999. [Google Scholar]
- 3.Melleney EM, Subhani JM, Willoughby CP. Dysphagia referrals to a District General Hospital Gastroenterology unit: hard to swallow. Dysphagia 2004;19:78–82. [DOI] [PubMed] [Google Scholar]
- 4.Alaani A, Vengala S, Johnston MN. The role of barium swallow in the management of the globus pharyngeus. Eur Arch Oto-Rhino-Laryngol 2007;264: 1095–7. [DOI] [PubMed] [Google Scholar]
- 5.Spechler SJ. American gastroenterological association medical position statement on treatment of patients with dysphagia caused by benign disorders of the distal esophagus. Gastroenterol 1999;117:229–33. [DOI] [PubMed] [Google Scholar]
- 6.Esfandyari T, Potter JW, Vaezi MF. Dysphagia: a cost analysis of the diagnostic approach. Am J Gastroenterol 2002;97:2733–7. [DOI] [PubMed] [Google Scholar]
- 7.Mitchell JD, Farrow R, Hussaini SH, et al. Clearance of barium from the oesophagus with diet Cola and metoclopramide: a one stop approach to patients with dysphagia. Clin Radiol 2001;56:64–6. [DOI] [PubMed] [Google Scholar]
- 8.Murray IA, Palmer J, Waters C, et al. Predictive value of symptoms and demographics in diagnosing malignancy or peptic stricture. World J Gastroenterol 2012;18:4357–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Department of Health. 2010/2011 National tariff information. http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/@ps/@sta/@perf/documents/digitalasset/dh_115898.xls (accessed 4 Jul 2012).
- 10.Sarkar S, Duffy U, Haslam N. Improved clinical outcomes and efficacy with a nurse-led colonoscopy surveillance service. Frontline Gastroenterol 2012;3:16–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rhatigan E, Tympas I, Murray G, et al. Scoring system to identify patients at high risk of oesophageal cancer. Brit J Surg 2010;97:1831–7. [DOI] [PubMed] [Google Scholar]
- 12.Furuta GT. Eosinophilic esophagitis: update on clinicopathological manifestations and pathophysiology (review). Curr Opinion Gastroenterol 2011;27:383–8. [DOI] [PubMed] [Google Scholar]
- 13.Grossman TW, Kita MS, Toohill RJ. The diagnostic accuracy of pharyngoesophagram compared to esophagoscopy in patients with head and neck cancer. Laryngoscope 1987;97:1030–2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.