Supplemental Digital Content is available in the text
Keywords: meta-analysis, pregabalin, spine surgery
Abstract
Background:
We performed a systematic review and meta-analysis of randomized controlled trials (RCTs) to evaluate the efficacy and safety of pregabalin for pain management following spine surgery.
Methods:
In September 2016, a systematic computer-based search was conducted in PubMed, EMBASE, Web of Science, and Cochrane Database of Systematic Reviews. RCTs of patients prepared for spine surgery that compared pregabalin with placebo were retrieved. The primary endpoint was the VAS score with rest or mobilization at 12 hours, 24 hours, and 48 hours and cumulative morphine consumption at 24 hours and 48 hours. The secondary outcomes were complications of nausea, sedation, dizziness, headache, and visual disturbances. After testing for publication bias and heterogeneity between studies, data were aggregated for random-effects models when necessary.
Results:
Ten clinical studies with 535 patients (pregabalin group = 294, control group = 241) were included in the meta-analysis. Pregabalin was associated with reduced pain scores at 12 hours, 24 hours, and 48 hours, corresponding to a reduction of 1.91 points (95% CI, –4.07 to 0.24 point) at 12 hours, 2.66 points (95% CI, –4.51 to –0.81 point) at 24 hours, and 4.33 points (95% confidence interval, –6.38 to –2.99 point) at 48 hours on a 100-point numeric rating scale. There was no significant difference between VAS scores with mobilization at 12 hours, 24 hours, or 48 hours. Similarly, pregabalin was associated with a reduction in cumulative morphine consumption at 24 hours (–7.07, 95% CI –9.84, –4.30) and 48 hours (–6.52, 95% CI –7.78, –5.25, P = 0.000). Furthermore, pregabalin can reduce the occurrence of nausea (RR 0.57, 95% CI 0.41, 0.79, P = 0.001, number needed to treat = 8.4). There were no significant differences in the occurrence of sedation, dizziness, headache, or visual disturbances.
Conclusions:
Preoperative use of pregabalin was efficacious in reduction of postoperative pain, total morphine consumption, and the occurrence of nausea following spine surgery. Because the sample size and the number of included studies were limited, a multicenter RCT is needed to identify the effects and optimal dose of pregabalin for reducing acute pain after spine surgery.
1. Introduction
Spine surgeries are associated with moderate to extreme pain at hospital discharge, thus hampering recovery.[1,2] Appropriate pain control is a prerequisite to promoting early mobilization and functional recovery after spine surgery. Morphines are recommended as the first choice for management of post-surgery pain, but they are associated with many adverse effects.[3,4] Recently, a greater emphasis has been placed on the administration of nonopioid analgesic drugs as part of multimodal anesthesia schedules for relieving pain and reducing morphine-related complications. For surgery, operation-induced neuroplastic changes may induce sensitization and cause postoperative hyperalgesia or allodynia. Therefore, an optimal multimodal analgesic regimen, including antihyperalgesic drugs to attenuate central sensitization, may have beneficial effects for pain control after surgery.
Pregabalin is an anticonvulsant agent that can bind to the alpha2delta subunit of presynaptic voltage-gated calcium channels, thus reducing the calcium influx into presynaptic terminals. However, the efficacy of perioperative pregabalin in spinal surgery has not been determined. A previous meta-analysis has compared gabapentinoids (gabapentin and pregabalin) versus placebo for pain control in lumbar surgery. However, only 2 studies were included in a previous meta-analysis that compared pregabalin versus placebo for pain control after lumbar surgery.[5] Therefore, we searched for relevant studies and performed a meta-analysis comparing pregabalin versus placebo for reducing pain intensity in spinal surgery.
2. Materials and methods
This systematic review was reported according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines.
2.1. Search strategies
The following databases were searched in September 2016 without restriction of regions or publication types: PubMed (1950–September 2016), EMBASE (1974–September 2016), Web of Science (1950–September 2016), and Cochrane Library (September 2016 Issue 3) (Supplement file 1). The Mesh terms and their combinations used in the search were as follows: “analgesia” OR “pain management” OR “anesthetic agents” OR “lumbar surgery” OR “spinal surgery” OR “lumbar spine surgery” AND “pregabalin” [Mesh terms]. The reference lists of related reviews and original articles were searched for any relevant studies, including randomized controlled trials (RCTs) involving adult humans. Only articles originally written in English or translated into English were considered. When multiple reports describing the same sample were published, the most recent or complete report was used. Since this is a meta-analysis, no ethics committee or institutional review board approval was necessary for the study.
2.2. Inclusion criteria and study selection
Patients: adult human subjects (age>18 years) prepared for lumbar surgery (lumbar infusion, lumbar laminectomy, or lumbar discectomy); intervention: perioperative pregabalin as an intervention group; comparison: placebo; outcomes: visual analog scale (VAS) with rest or mobilization at 12 hours, 24 hours, and 48 hours and complications (nausea, sedation, dizziness, headache, and visual disturbances); Study design: RCTs. Two independent reviewers screened the title and abstracts of the identified studies after removing the duplicates of the search results. Any disagreements about the inclusion or exclusion of a study were solved by discussion or consultation with an expert. The reliability of the study selection was determined by Cohen's kappa test, and the acceptable threshold value was set at 0.61.[6,7]
2.3. Data abstraction and quality assessment
A specific extraction was conducted to collect the following data from the included trials: patients’ general characteristics, country, the sample size of the control group and intervention group, the preoperative and postoperative dose, and the timing and frequency of pregabalin use. Outcomes such as VAS score with rest or mobilization at 12 hours, 24 hours, and 48 hours and complications (nausea, sedation, dizziness, headache, and visual disturbances) were abstracted and recorded in a sheet. Postoperative pain intensity was measured by a 100-point VAS. When the numerical rating scale (NRS) was reported, it was converted to a VAS. Additionally, a 10-point VAS was converted to a 100-point VAS.[8] Data in other forms (i.e., median, interquartile range, and mean ± 95% confidence interval [CI]) were converted to the mean ± standard deviation (SD) according to the Cochrane Handbook.[9] If the data were not reported numerically, we extracted these data using “GetData Graph Digitizer” software from the published figures. All the data were extracted by 2 independent reviewers, and disagreements were resolved by discussion. The methodological quality of all included trials was independently assessed by 2 reviewers on the basis of the Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0 (http://www.cochrane-handbook.org/).
2.4. Outcome measures and statistical analysis
Continuous outcomes (VAS with rest or mobilization at 12 hours, 24 hours, and 48 hours) were expressed as the weighted mean differences (WMD) and respective 95% CI. Dichotomous outcomes (the occurrence of nausea, sedation, dizziness, headache, and visual disturbances) were expressed as the risk ratio (RR) with 95% CI. Statistical significance was set at P < 0.05 to summarize the findings across the trials. The meta-analysis was calculated by Stata software, version 12.0 (Stata Corp., College Station, TX). Statistical heterogeneity was tested using the chi-squared test and I2 statistic. When there was no statistical evidence of heterogeneity (I2 < 50%, P > 0.1), a fixed-effects model was adopted; otherwise, a random-effect model was chosen. Publication bias was tested using funnel plots. Publication bias was assessed by the funnel plot and quantitatively assessed by Begg's test. Subgroup analysis was conducted according to the dose of pregabalin (<300 mg/d or ≥300 mg/d). We considered there to be no publication bias if the funnel plot was symmetrical and the P value was > 0.05. In addition, we calculated the number needed to harm (NNH) to examine the risk versus benefits of pregabalin therapy regarding complications.[10]
3. Results
3.1. Search results and quality assessment
In the initial research, a total of 316 papers were identified from the electronic databases (PubMed = 121, Embase = 98, Web of Science = 75, Cochrane Library = 22). The number of articles after duplicates had been removed by Endnote X7 software was 255. After screened the abstracts and title of these 255 studies, 243 papers were excluded because they were irrelevant or did not meet the criteria. One study compared celecoxib, pregabalin, extended-release oxycodone, and acetaminophen as a multimodal anesthesia versus intravenous morphine for lumbar fusion surgery.[11] Another study compared gabapentin versus pregabalin with no control group in patients after lumbar disc herniation surgery.[12] Both studies were excluded. Finally, 10 clinical studies with 535 patients (pregabalin group = 294, control group = 241) were included in the meta-analysis.[13–22] The flow diagram for the included studies can be seen in Fig. 1. Two studies administered pregabalin with 2 different doses, and we thus divided the population into 2 arms.[15,19] The general characteristic of the included studies can be seen in Table 1. The quality assessment of the included studies is summarized in Figs. 2 and 3. Only 2 studies did not describe the random sequence generation procedure; the remaining 8 clinical trials performed appropriate random sequence generation. The quality of the remaining studies was all low risk.
Figure 1.
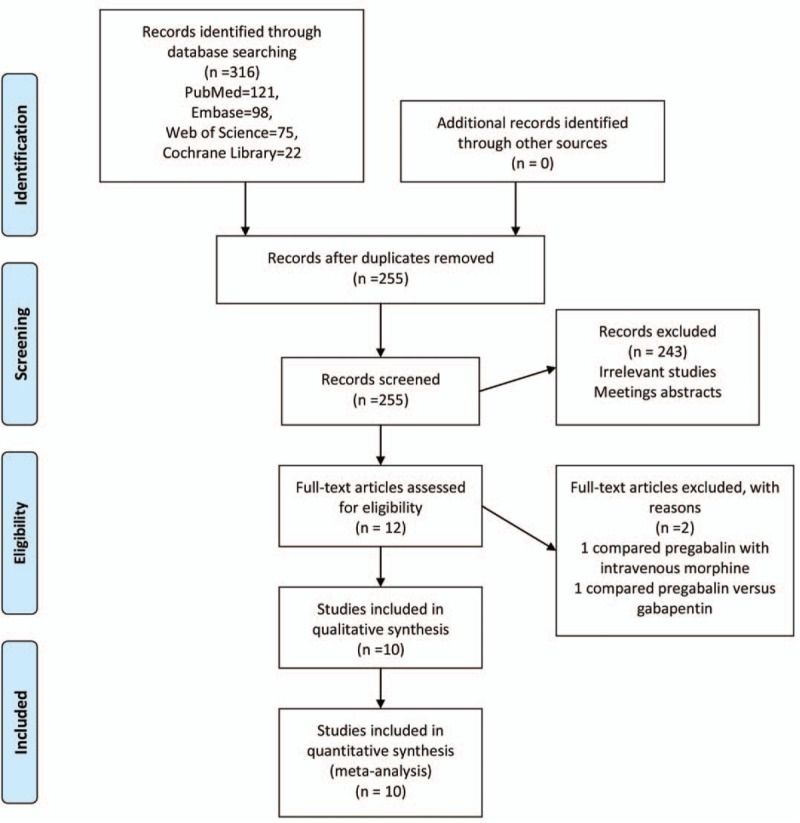
PRISMA flowchart for the included studies. PRISMA = preferred reporting items for systematic reviews and meta-analyses.
Table 1.
The general characteristic of the included studies.
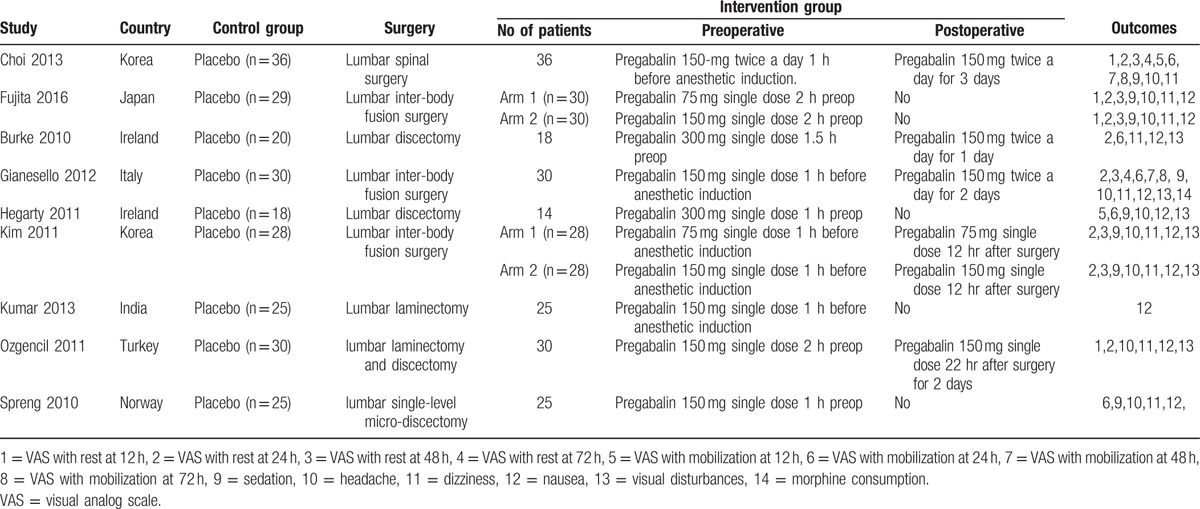
Figure 2.
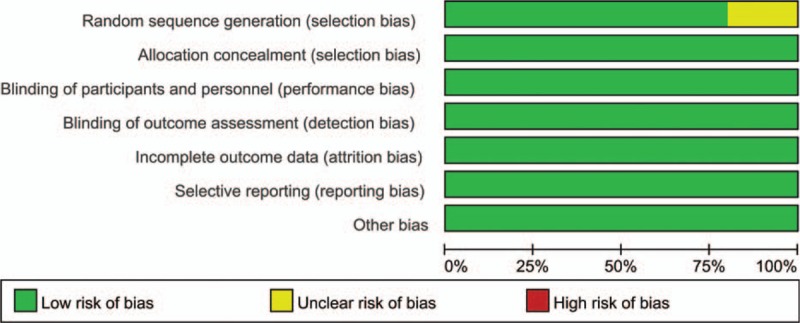
The risk of bias graph for the included studies.
Figure 3.
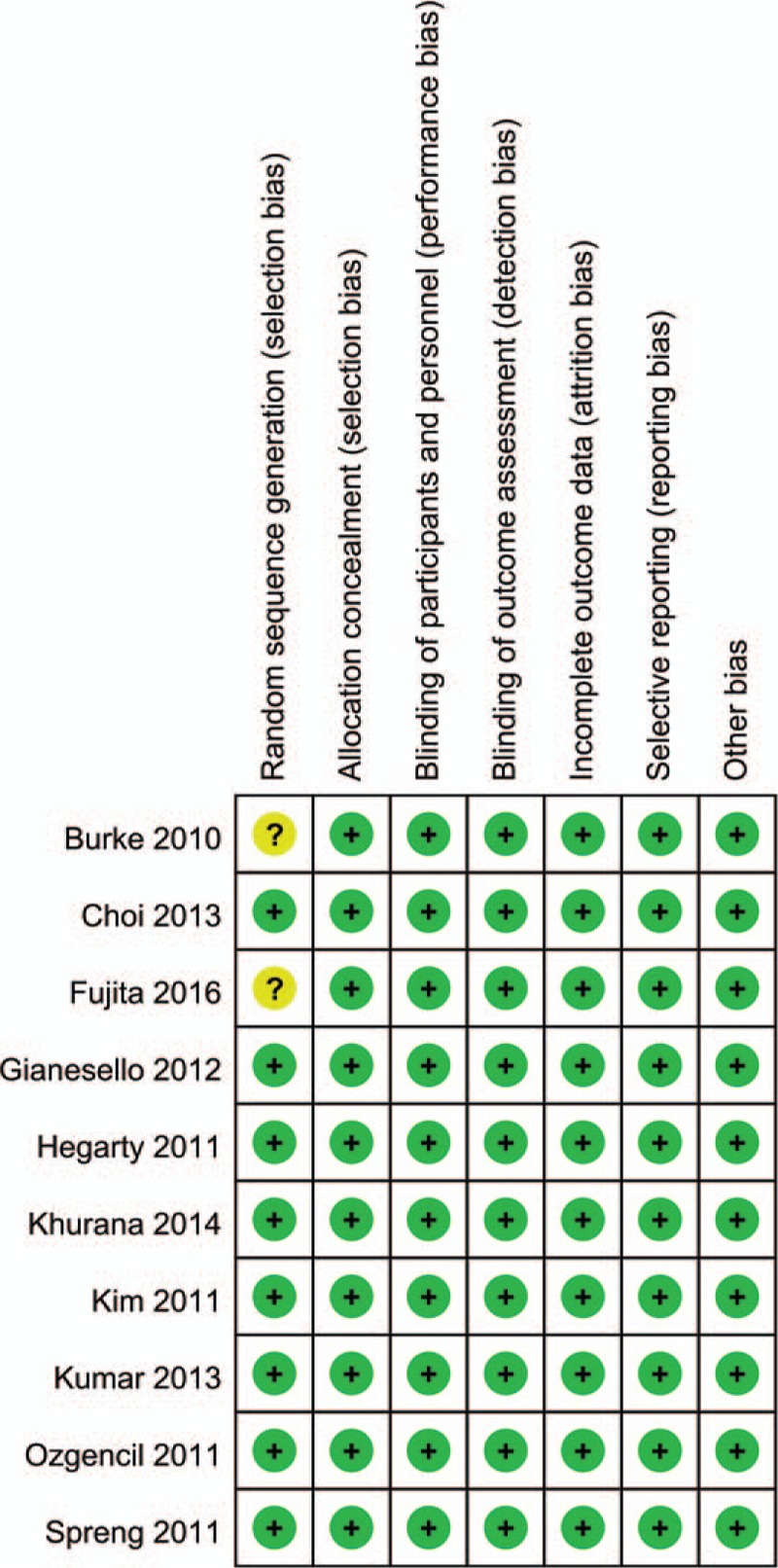
The risk of bias summary for the included studies.
3.2. Results of meta-analysis
3.2.1. VAS with rest at 12 h, 24 h, and 48 h
Postoperative VAS scores with rest at 12 hours were reported in 4 studies, and the pooled results indicated that preoperative administration of pregabalin can decrease VAS score with rest at 12 hours (WMD = –1.91, 95% CI –4.07, 0.24, P = 0.082, Fig. 4). The meta-analysis results indicated that pregabalin can decrease VAS score with rest at 24 hours (WMD = –2.66, 95% CI –4.51, –0.81, P = 0.005, Fig. 4) and at 48 hours (WMD = –4.33, 95% CI –6.38, –2.99, P = 0.000, Fig. 4). Funnel plot and Begg's test were performed, and the results indicated that there was no publication bias between the included studies in terms of VAS score with rest at 12 hours, 24 hours, and 48 hours (Fig. 5).
Figure 4.
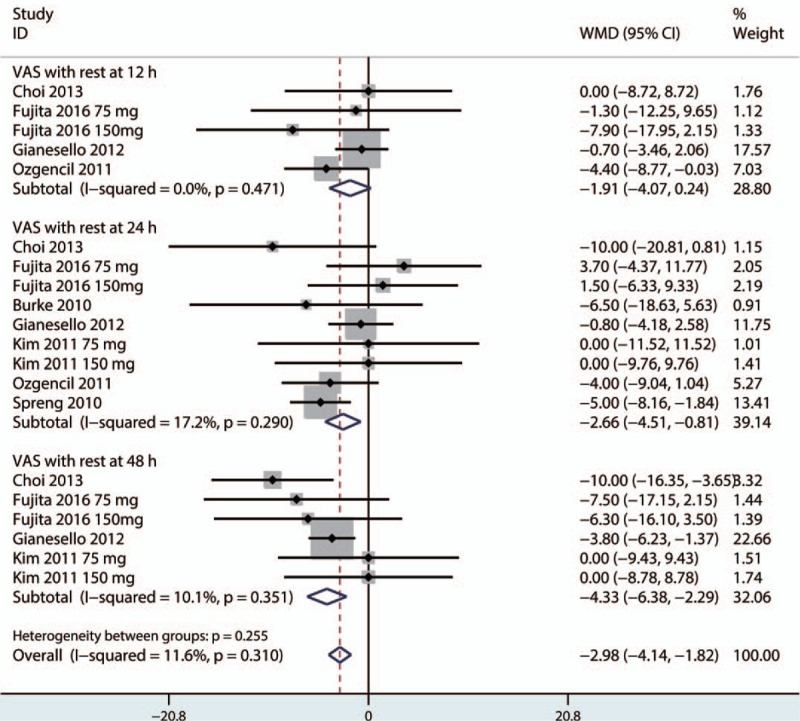
Forest plot comparing VAS scores with rest at 12 h, 24 h, and 48 h. VAS = visual analog scale.
Figure 5.
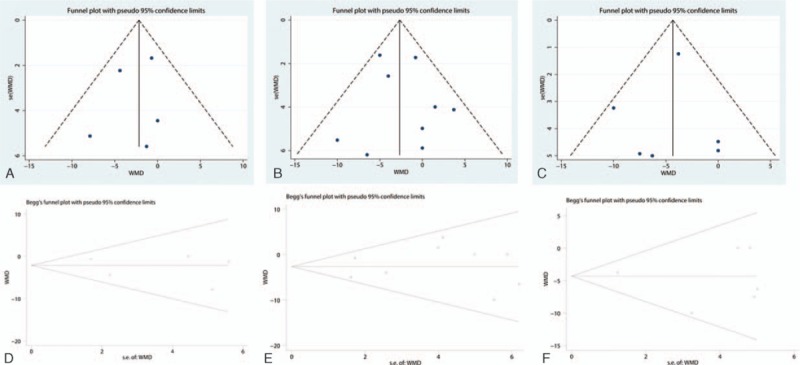
Funnel plot testing the publication bias of the VAS with rest at 12 h (A), 24 h (B), and 48 h (C) and Begg's test for VAS with rest at 12 h (D), 24 h (E), and 48 h (F). VAS = visual analog scale.
3.2.2. VAS with mobilization at 12 h, 24 h, and 48 h
There were no significant differences between the pregabalin group versus control group in the VAS score with mobilization at 12 hours (WMD = –17.85, 95% CI –45.32, 9.62, P = 0.203, Fig. 6) and 24 hours (WMD = –6.70, 95% CI –14.41, 1.01, P = 0.088, Fig. 6). The pooled results indicated that there was no significant difference between pregabalin and the control group in terms of VAS score with mobilization at 48 hours (WMD = –4.36, 95% CI –11.67, 2.94, P = 0.242, Fig. 6).
Figure 6.
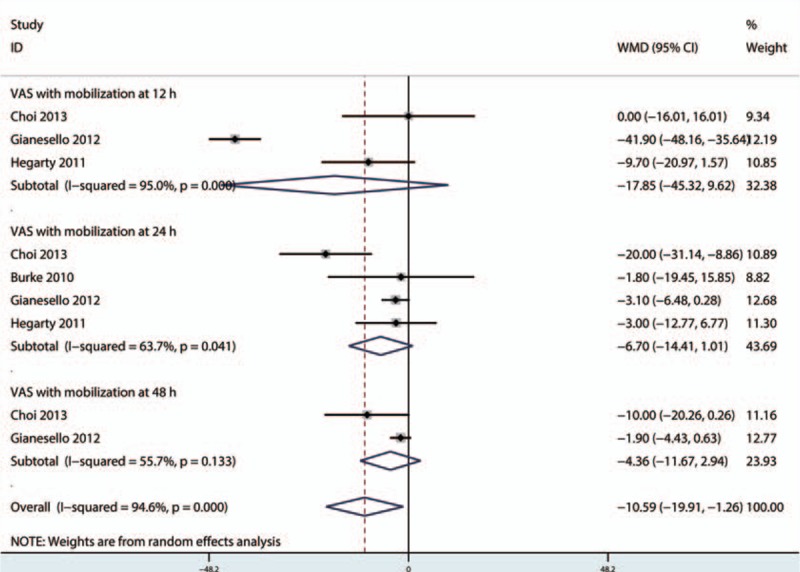
Forest plot comparing the VAS with mobilization at 12 h, 24 h, and 48 h. VAS = visual analog scale.
3.2.3. Cumulative morphine consumption at 24 h and 48 h
The pooled results indicated that pregabalin can reduce the cumulative consumption of morphines at 24 hours (WMD = –7.07, 95% CI –9.84, –4.30, P = 0.000, Fig. 7) and at 48 hours (WMD = –6.52, 95% CI –7.78, –5.25, P = 0.000, Fig. 7).
Figure 7.
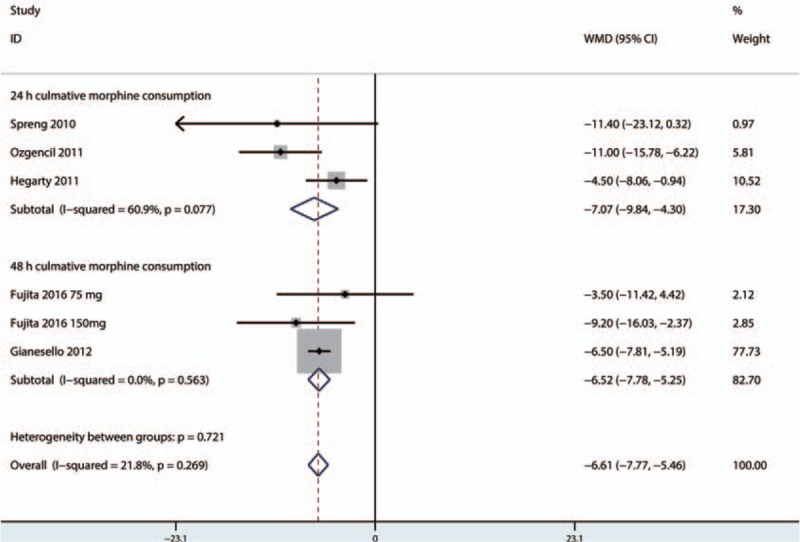
Forest plot of cumulative morphine consumption at 24 h and 48 h between the 2 groups.
3.3. Complications
There were no significant differences between the groups in the occurrence of sedation (RR = 1.17, 95% CI 0.56, 2.42, P = 0.679, Fig. 8A) or headache (RR = 1.19, 95% CI 0.68, 2.08, P = 0.540, Fig. 8B). The NNH for sedation and headache was 109.9 and 116.7, respectively. There was no significant difference between the occurrence of dizziness (RR = 1.37, 95% CI 0.90, 2.07, P = 0.139, Fig. 8 C) or visual disturbances (RR = 2.00, 95% CI 0.79, 5.02, P = 0.142, Fig. 8D). The NNH for dizziness was 25.7 and was 38.9 for visual disturbances.
Figure 8.
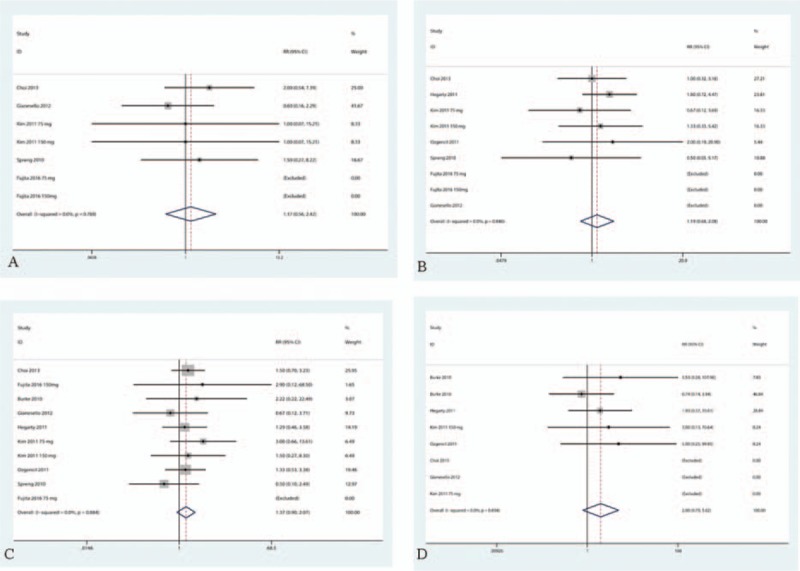
Forest plots comparing the occurrence of sedation, B headache, C dizziness and D visual disturbances between the 2 groups.
Pregabalin can reduce the occurrence of nausea (RR = 0.57, 95% CI 0.41, 0.79, P = 0.001, Fig. 9) with a significant difference, and the NNT was 8.4.
Figure 9.
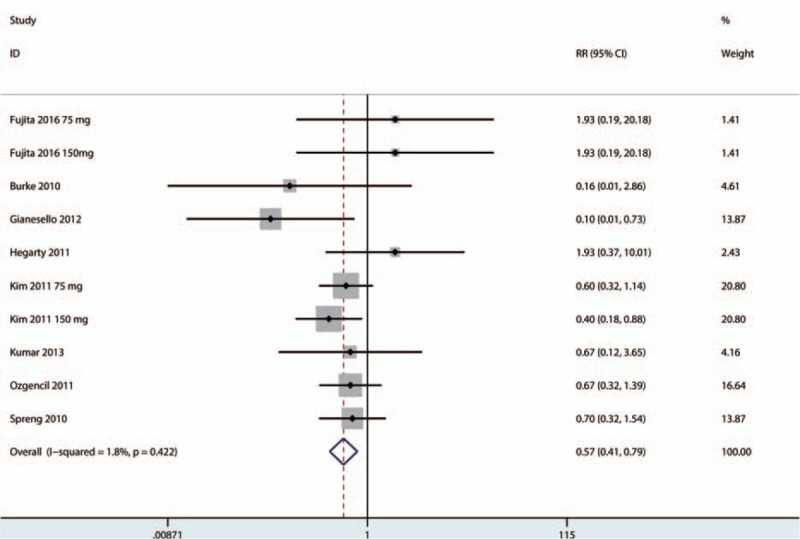
Forest plot comparing the occurrence of nausea between the 2 groups.
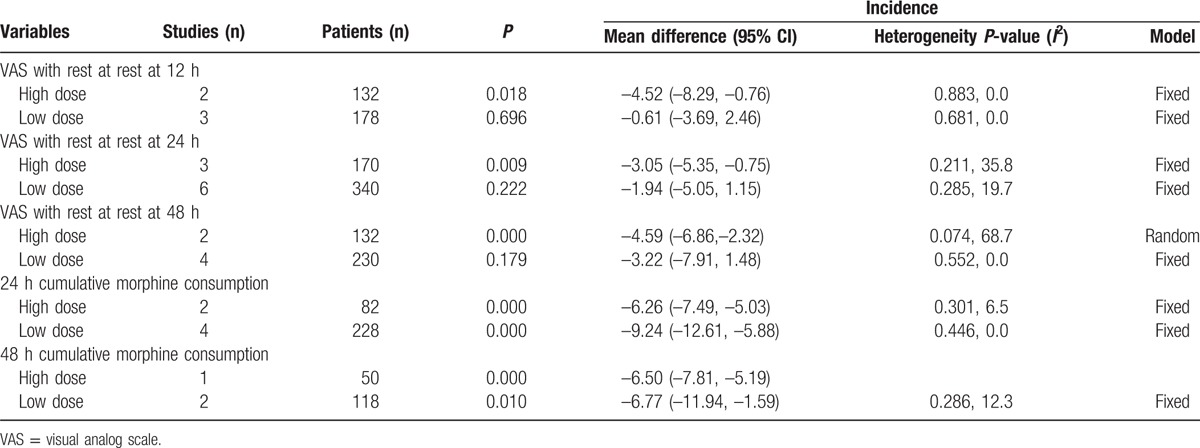
3.4. Subgroup analysis
Subgroup analyses were conducted according to a low dose of pregabalin (<300 mg/d) and a high dose of pregabalin (≥300 mg/d). The detailed results can be seen in Table 2. The pooled results indicated that a high dose of pregabalin can reduce the VAS score with rest at 12 hours, 24 hours, and 48 hours with a significant difference (P < 0.05). Both low doses of pregabalin and high doses of pregabalin can reduce the cumulative morphine consumption at 24 hours and 48 hours (P < 0.05).
Table 2.
The subgroup analysis of the VAS with rest at 12 h, 24 h, and 48 h, 24 h cumulative morphine consumption and 48 h cumulative morphine consumption.
4. Discussion
The current meta-analysis demonstrated that the use of pregabalin is associated with reduced pain scores at 12 hours, 24 hours, and 48 hours with rest, equivalent on a 110-point VAS to 1.91 points at 12 hours, 2.66 points at 24 hours and 4.33 points at 48 hours. For VAS with mobilization, no clinically relevant reductions in pain scores were associated with using pregabalin at any of the time points. The cumulative morphine consumption at 24 hours and 48 hours was reduced in the pregabalin group by approximately 7.07 mg and 6.52 mg, respectively. The most important finding of this meta-analysis was that pregabalin can reduce the occurrence of nausea after spine surgery. However, pregabalin could also increase the occurrence of dizziness and had an NNH of 25.7, which means that of 25.7 patients who receive pregabalin, 1 will suffer from dizziness.
These results are contradict with a previous meta-analysis that compared gabapentinoids versus placebo for managing pain after total knee arthroplasty. In the meta-analysis, the results indicated that no evidence to support the routine use of pregabalin after total knee arthroplasty.[23] Eipe et al[24] included 43 clinical studies in a meta-analysis and found that pregabalin use is small in magnitude and is primarily restricted to surgical procedures associated with pronociceptive mechanisms. Furthermore, pregabalin was most likely to demonstrate efficacy in conditions associated with chronic pain. Choi et al[14] reported that the occurrence of chronic pain after spine surgery was approximately 20%, and this incidence is lower than the 32% following discectomy and up to 85% observed after amputation.[25–27] If the theory proposed by Eipe et al[24] is correct, then the lower incidence of chronic pain after spine surgery may explain why pregabalin failed to demonstrate efficacy in patients undergoing spine surgery.
In a previous meta-analysis of the use of gabapentinoids in the management of postoperative pain after lumbar spinal surgery, the findings suggested that both gabapentin and pregabalin were efficacious in reducing postoperative pain.[5] However, only 2 studies were included in the meta-analysis to compare pregabalin versus placebo for spinal surgery. Dong et al[28] performed a meta-analysis of the use of pregabalin for reducing pain after TKA and found that pregabalin was effective in reducing pain intensity after TKA.
Morphine-related complications were also compared between the pregabalin and control groups. Although a reduction in the incidence of postoperative nausea following spine surgery was observed, this effect was limited (number needed to treat = 8.4). The reduction of the occurrence of nausea may have mainly been due to reductions in the cumulative morphine consumption. Grant et al[29] conducted a meta-analysis and found that preoperative pregabalin was associated with a significant reduction in PONV; however, postoperative analgesia did not improve correspondingly. There were no significant differences in sedation, headache, dizziness, or visual disturbances between the 2 groups. Several studies have linked the use of pregabalin to increased dizziness and sedation.[30] The NNH for dizziness is 25.7 and is lower than that of other complications. This suggests that the complication of dizziness is the least commonly observed complication regarding pregabalin administration.
There were a total of 5 limitations refer to this study: (1) 10 RCTs with relatively small sample size, which might have influence on the precision of the final results; (2) the follow-up for patients in the included studies ranged from 24 hours to 48 hours and this relative short periods follow-up may underestimate the final complications of pregabalin; (3) the dosage and interval of pregabalin administration were differ from each studies and thus may cause large heterogeneity; (4) the different postoperative anesthesia methods (spinal, general, or spinal-epidural) may influence the postoperative pain scores, and this is also the reason for large heterogeneity; and (5) although publication bias was not detected in Begg's test and this outcome need to treat cautiously since the number of included studies was limited.
5. Conclusion
In conclusion, this is the first meta-analysis to compare the preoperative use of pregabalin versus a placebo for the management of pain after spine surgery. Some analgesic efficacy and opioid-sparing effects were observed with the administration of pregabalin. Additionally, a significant decrease in the risk of nausea was associated with the use of pregabalin. Because the sample size and the number of included studies were limited, a multicenter RCT is needed to identify the effects of pregabalin for reducing acute pain after spine surgery.
Supplementary Material
Footnotes
Abbreviations: CI = confidence interval, NNH = number needed to harm, NRS = numerical rating scale, PRISMA = preferred reporting items for systematic reviews and meta-analyses, RCTs = randomized controlled trials, RR = risk ratio, SD = standard deviation, VAS = visual analog scale, WMD = weighted mean differences.
The authors have no funding and conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Cohen BE, Hartman MB, Wade JT, et al. Postoperative pain control after lumbar spine fusion. Patient-controlled analgesia versus continuous epidural analgesia. Spine (Phila Pa 1976) 1997;22:1892–6. discussion 1896–1897. [DOI] [PubMed] [Google Scholar]
- [2].Gottschalk A, Freitag M, Tank S, et al. Quality of postoperative pain using an intraoperatively placed epidural catheter after major lumbar spinal surgery. Anesthesiology 2004;101:175–80. [DOI] [PubMed] [Google Scholar]
- [3].Pavlin DJ, Chen C, Penaloza DA, et al. Pain as a factor complicating recovery and discharge after ambulatory surgery. Anesth Analg 2002;95:627–34. table of contents. [DOI] [PubMed] [Google Scholar]
- [4].Sun XL, Zhao ZH, Ma JX, et al. Continuous local infiltration analgesia for pain control after total knee arthroplasty: a meta-analysis of randomized controlled trials. Medicine (Baltimore) 2015;94:e2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Yu L, Ran B, Li M, et al. Gabapentin and pregabalin in the management of postoperative pain after lumbar spinal surgery: a systematic review and meta-analysis. Spine (Phila Pa 1976) 2013;38:1947–52. [DOI] [PubMed] [Google Scholar]
- [6].Landis JR, Koch GG. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics 1977;33:363–74. [PubMed] [Google Scholar]
- [7].Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–74. [PubMed] [Google Scholar]
- [8].Wang C, Cai X-Z, Yan S-G. Comparison of periarticular multimodal drug injection and femoral nerve block for postoperative pain management in total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty 2015;30:1281–6. [DOI] [PubMed] [Google Scholar]
- [9].Higgins JPT GS. Cochrane handbook for systematic reviews of interventions version 5.1.0. 2011; [http://handbook.cochrane.org/]. [Google Scholar]
- [10].Laupacis A, Sackett DL, Roberts RS. An assessment of clinically useful measures of the consequences of treatment. N Engl J Med 1988;318:1728–33. [DOI] [PubMed] [Google Scholar]
- [11].Kim SI, Ha KY, Oh IS. Preemptive multimodal analgesia for postoperative pain management after lumbar fusion surgery: a randomized controlled trial. Eur Spine J 2016;25:1614–9. [DOI] [PubMed] [Google Scholar]
- [12].Dolgun H, Turkoglu E, Kertmen H, et al. Gabapentin versus pregabalin in relieving early post-surgical neuropathic pain in patients after lumbar disc herniation surgery: a prospective clinical trial. Neurol Res 2014;36:1080–5. [DOI] [PubMed] [Google Scholar]
- [13].Burke SM, Shorten GD. Perioperative pregabalin improves pain and functional outcomes 3 months after lumbar discectomy. Anesth Analg 2010;110:1180–5. [DOI] [PubMed] [Google Scholar]
- [14].Choi YS, Shim JK, Song JW, et al. Combination of pregabalin and dexamethasone for postoperative pain and functional outcome in patients undergoing lumbar spinal surgery: a randomized placebo-controlled trial. Clin J Pain 2013;29:9–14. [DOI] [PubMed] [Google Scholar]
- [15].Fujita N, Tobe M, Tsukamoto N, et al. A randomized placebo-controlled study of preoperative pregabalin for postoperative analgesia in patients with spinal surgery. J Clin Anesth 2016;31:149–53. [DOI] [PubMed] [Google Scholar]
- [16].Gianesello L, Pavoni V, Barboni E, et al. Perioperative pregabalin for postoperative pain control and quality of life after major spinal surgery. J Neurosurg Anesthesiol 2012;24:121–6. [DOI] [PubMed] [Google Scholar]
- [17].Hegarty DA, Shorten GD. A randomised, placebo-controlled trial of the effects of preoperative pregabalin on pain intensity and opioid consumption following lumbar discectomy. Korean J Pain 2011;24:22–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Khurana G, Jindal P, Sharma JP, et al. Postoperative pain and long-term functional outcome after administration of gabapentin and pregabalin in patients undergoing spinal surgery. Spine (Phila Pa 1976) 2014;39:E363–368. [DOI] [PubMed] [Google Scholar]
- [19].Kim JC, Choi YS, Kim KN, et al. Effective dose of peri-operative oral pregabalin as an adjunct to multimodal analgesic regimen in lumbar spinal fusion surgery. Spine (Phila Pa 1976) 2011;36:428–33. [DOI] [PubMed] [Google Scholar]
- [20].Kumar KP, Kulkarni DK, Gurajala I, et al. Pregabalin versus tramadol for postoperative pain management in patients undergoing lumbar laminectomy: a randomized, double-blinded, placebo-controlled study. J Pain Res 2013;6:471–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ozgencil E, Yalcin S, Tuna H, et al. Perioperative administration of gabapentin 1,200 mg day-1 and pregabalin 300 mg day-1 for pain following lumbar laminectomy and discectomy: a randomised, double-blinded, placebo-controlled study. Singapore Med J 2011;52:883–9. [PubMed] [Google Scholar]
- [22].Spreng UJ, Dahl V, Raeder J. Effect of a single dose of pregabalin on post-operative pain and pre-operative anxiety in patients undergoing discectomy. Acta Anaesthesiol Scand 2011;55:571–6. [DOI] [PubMed] [Google Scholar]
- [23].Hamilton TW, Strickland LH, Pandit HG. A meta-analysis on the use of gabapentinoids for the treatment of acute postoperative pain following total knee arthroplasty. J Bone Joint Surg Am 2016;98:1340–50. [DOI] [PubMed] [Google Scholar]
- [24].Eipe N, Penning J, Yazdi F, et al. Perioperative use of pregabalin for acute pain-a systematic review and meta-analysis. Pain 2015;156:1284–300. [DOI] [PubMed] [Google Scholar]
- [25].Beswick AD, Wylde V, Gooberman-Hill R, et al. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open 2012;2:e000435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Parker SL, Xu R, McGirt MJ, et al. Long-term back pain after a single-level discectomy for radiculopathy: incidence and health care cost analysis. J Neurosurg Spine 2010;12:178–82. [DOI] [PubMed] [Google Scholar]
- [27].Hsu E, Cohen SP. Postamputation pain: epidemiology, mechanisms, and treatment. J Pain Res 2013;6:121–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Dong J, Li W, Wang Y. The effect of pregabalin on acute postoperative pain in patients undergoing total knee arthroplasty: a meta-analysis. Int J Surg 2016;34:148–60. [DOI] [PubMed] [Google Scholar]
- [29].Grant MC, Betz M, Hulse M, et al. The effect of preoperative pregabalin on postoperative nausea and vomiting: a meta-analysis. Anesth Analg 2016;123:1100–7. [DOI] [PubMed] [Google Scholar]
- [30].Mishriky BM, Waldron NH, Habib AS. Impact of pregabalin on acute and persistent postoperative pain: a systematic review and meta-analysis. Br J Anaesth 2015;114:10–31. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


