Abstract
Background:
To investigate the radiation dose and image quality for iterative reconstruction combined with the CARE kV technique in chest computed tomography (CT) scanning for physical examination.
Methods:
A total of 130 patients who underwent chest CT scanning were randomly chosen and the quality reference value was set as 80 mAs. The scanning scheme was set and the patients were randomly divided into groups according to the scanning scheme. Sixty patients underwent a chest scan with 100 kV using the CARE kV technique and SAFIRE reconstruction (value=3) (experimental group) and the other 70 patients underwent chest scanning with 120 kV (control group). The mean CT value, image noise (SD), and signal-to-noise ratio (SNR) of the apex of the lung, the level of the descending aorta bifurcation of the trachea, and the middle area of the left atrium were measured. The image quality was assessed on a 5-point scale by two radiologists and results of the two groups were compared. The CT dose index of the volume (CTDIvol), dose length product (DLP), and effective dose (ED) were compared.
Results:
All the images for both groups satisfied the diagnosis requirement. There was no statistical difference in the image quality between the two methods (P > 0.05). The mean CT value of the apex of the lung, the level of the descending aorta bifurcation of the trachea, and the middle area of the left atrium were not significantly different for both groups (P > 0.05), while the image noise (SD) and the signal-to-noise ratio (SNR) of the apex of the lung, the level of the descending aorta bifurcation of the trachea, and the middle area of the left atrium were statistically different for both groups (P < 0.05). The CTDIvol was 3.29 ± 1.17 mGy for the experimental group and 5.30 ± 1.53 mGy for the control group. The DLP was 114.9 ± 43.73 mGy cm for the low-dose group and 167.6 ± 44.59 mGy cm for the control group. The ED was 1.61 ± 0.61 mSv for the low-dose group and 2.35 ± 0.62 mSv for the control group (P < 0.05).
Conclusion:
The CARE kV technique combined with iterative reconstruction for chest CT scanning for physical examination could reduce the radiation dosage and improve CT image quality, which has a potential clinical value for imaging the thorax.
Keywords: CARE kV, chest, iterative reconstruction, radiation dosage, tomograph, x-ray computed
1. Introduction
With the improvement in living standards, health check-ups are receiving increasing attention. Chest computed tomography (CT) is superior to conventional chest radiography for detecting lesions and determining their position and qualitative aspects, making it the prime choice for lesion detection. However, the radiation associated with the process is becoming a problem. The ICRP advocates the principle of “as low as reasonably achievable (ALARA),” which requires CT examination be on the premise of image quality to meet the demand of diagnosis as far as possible to reduce the radiation dose.[1] Previously, the chest low-dose scanning techniques mainly used a fixed pipe and voltage, low current, and real-time dynamic exposure dose to regulate the tube current, but methods to further reduce the radiation dose are being studied. The CARE kV technique combined with iterative reconstruction is a new technique with lower radiation dose that the conventional techniques, which has attracted the attention of medical radiation workers. In this paper, we discuss the application of the CARE kV technique combined with iterative reconstruction to chest CT scanning for health examination patients.
2. Materials and methods
2.1. General information
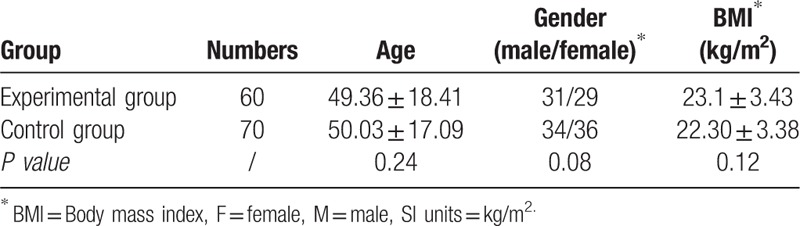
A total of 130 patients suspected with chest disease undergoing a chest CT examination from Dec, 2012 to April, 2013 in our hospital were randomized into two groups: the experimental group and control group. The former consisted of 60 patients; 31 were males and 29 were females. The average age was 49.36 + 18.41 years and the average body mass index (BMI; BMI= weight/height2 (kg/m2)) was 23.1 ± 3.43. The latter consisted of 70 patients; 34 were males and 36 were females. The average age was 50.03 ± 17.09 years and the BMI was 22.56 ± 3.38. There were no significant differences in gender and age in the two groups (P > 0.05) (Table 1).The clinical trial was approved by the Institute's Medical Ethics Committee of Kunming Medical University, and consent forms were signed by all the examination patients.
Table 1.
Patients characteristics.
2.2. CT protocols
Siemens Somatom Definition Flash CT system (SOMATONM Definition Flash, Siemens Healthcare, Forchheim, Germany) was used to perform a scan from the thoracic inlet to the end of the lung.
Scanning parameters for the experimental group: The reference kV and mAs were 100 kV and 80 mAs, respectively. Real-time dynamic exposure dose adjustment tube current was used (CARE Dose 4D) pitching 3.0. The tube rotation time was 0.28 s. The collimation was 64 × 0.6 mm. The layer thickness and spacing were 8 mm. CARE kV scanning technology was first used followed by SAFIRE iterative reconstruction of the experimental raw data (value = 3). Convolution kernel: Window of lung fields I70f very sharp ASA, mediastinal window I31f medium smooth.
Scanning parameters for the control group: The reference kV and mAs were 120 kV and 80 mAs, respectively. The CARE kV scanning technology and SAFIRE iterative reconstruction were not used. The rest of the scanning parameters are the same as for the experimental group.
2.3. Imaging analysis
“Viewing” software on the Siemens CT postprocessing workstation, the 8 mm thick layer of cross-sectional images of each patient were loaded into the software. The region of interest (ROI) in the mediastinum window was defined in three levels: the apex level on the right side of the pectoralis major, tracheal bifurcation level of the descending aorta, and left atrium level. Artifacts, calcification, and other regions of interference were excluded. The measurement area was ∼60 mm2; hence, each ROI area was set at the maximum and location was equal. Different levels for the determination of the average CT value and background noise (SD) were measured. The SNR and CNR were calculated as follows:
SNR = mean CT value/SD and CNR = (descending aorta average CT value – muscle average CT value)/SD.[2]
2.4. Image quality analysis
Two attending physicians analyzed the obtained images independently, following the double-blind principle, and experienced doctors were called to reach an agreement in case of a disagreement. The main observable elements were the mediastinum, great vessels, pleura, chest wall tissue, and lung segments. The definition of the bronchial segment revealed anatomical details, particle size, and artifacts. The subjective image-quality scores were as follows:[3] 5 points: Anatomical details and lesions are simple and clearly defined; 4 points: Anatomical structure and details and lesions are less clear and can be defined, but not very well; 3 points: Most of the anatomic structures and lesions can satisfy diagnosis requirements, but a few images cannot be defined; 2 points: Anatomic structures and lesions are unclear and details cannot be obtained; and 1 point: Anatomical structures and lesions are too fuzzy to diagnose. A score of 3 points or higher meets the diagnostic requirements. The anatomical details used in the mediastinal and pulmonary window analysis included the lesion form display, size, and edge.
2.5. Radiation dose
The effective current, effective voltage, CT dose index of the volume (CTDIvol), and dose length product (DLP) for each patient were automatically generated during scanning and recorded. The CTDIvol reflected the average dose of the whole scanning volume. The DLP was used to evaluate the total radiation dose for a patient undergoing complete CT scanning. The effective dose (ED) was calculated using ED = DLP × K, where K is the conversion factor, using the European standard guidelines of CT quality. The chest average value was 0.014.[4]
2.6. Displayed lesion results
[Normal, nodule, effusion and (or) consolidation, fiber cords, calcification, cavity, pleural effusion and lymph node] of the two groups were used for statistical analysis.
2.7. Statistical analysis
An SPSS 17.0 statistical package was used. The image quality, CTDIvol, DLP, mean CT value of the image, SD, and SNR of the two groups were compared with two independent sample tests. For P < 0.05, there were statistically significant differences. The Kappa test was used to measure the consistency of the grading results of different doctors; ≥0.75 showed a good consistency; 0.4–0.76 showed an average consistency, and <0.4 showed a poor consistency.
3. Results
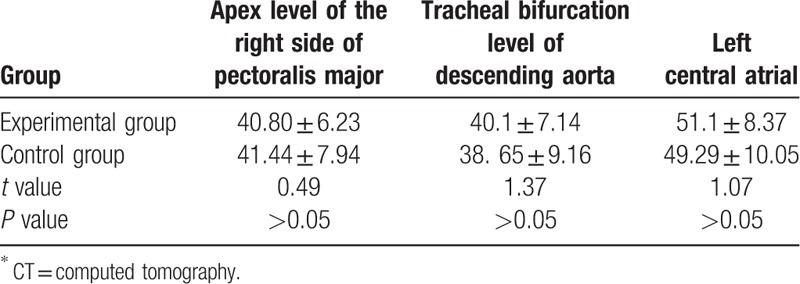
3.1. Comparison of mean CT value
The mean CT values at the apex level of the right pectoralis major, tracheal bifurcation level of the descending aorta, and left central atrial of the experimental group were compared with those of the control group (Table 2). No statistical difference was found (P > 0.05).
Table 2.
Comparison of mean CT∗ values of experimental group and control group.
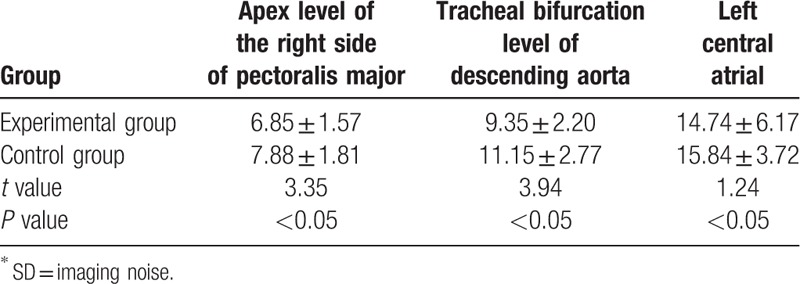
3.2. Comparison of SD
The SDs of the apex level of the right pectoralis major, tracheal bifurcation level of the descending aorta, and left central atrial of the control group are higher than those of the experimental group (Table 3). The difference in the SD was found to have statistical significance (P > 0.05).
Table 3.
Comparison of SD∗ of experimental group and control group.
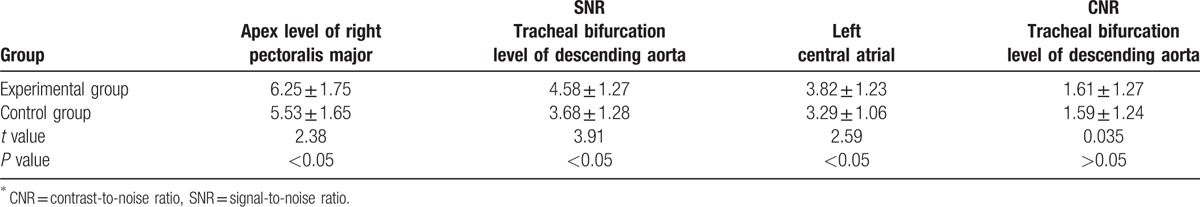
3.3. Comparison of SNR and CNR
The SNRs of the apex level of the right pectoralis major, tracheal bifurcation level of the descending aorta, and left central atrial of the experimental group are higher than those in the control group (Table 4). The difference in the SNR is of statistical significance (P<0.05). The difference in the CNR of the tracheal bifurcation level of the descending aorta of the two groups has no statistical significance (P > 0.05).
Table 4.
Comparison of SNR∗ and CNR∗ of experimental group and control group.
3.4. Comparison of subjective scoring of image quality
The image-quality scores of the mediastinal window in the experimental group and control group were 4.75 ± 0.07 and 4.62 ± 0.09 (t = 1.12, P = 0.248), respectively. The scores for the pulmonary window were 4.87 ± 0.08 and 4.75 ± 0.11 (t = 2.02, P = 0.056), respectively. There was no statistically significant difference in the two groups and all the image-quality scores were greater than 4.5 points, which meets the requirement of diagnosis according to the image-quality score given by two attending physician (Kappa = 0.786) (Fig. 1A and B).
Figure 1.
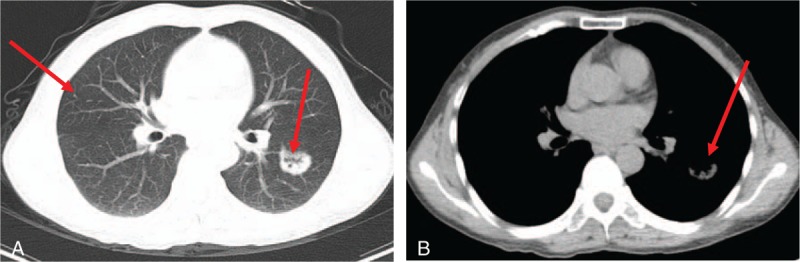
(A, B). Images of a 51-year-old female with a BMI of 19.0 kg/m2, obtained using CARE kV scanning technology and SAFIRE iterative reconstruction with an effective voltage of 100 kV. Chest transection CT scanning results of the lung and mediastinal window showed a soft tissue shadow in the dorsal segment in the left lower lobe and multiple nodules in right middle lobe (arrowheads). BMI = body mass index, CT = computed tomography, SAFIRE = sinogram-affirmed iterative reconstruction.
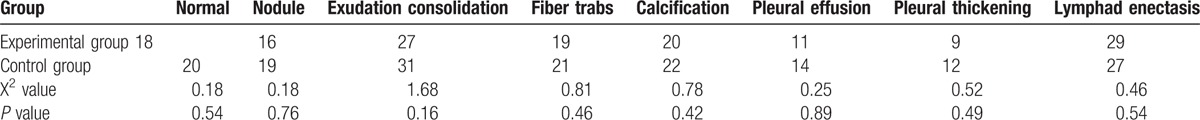
3.5. Lesions in the display picture
The difference in the constituent ratio of lesions in the experimental group and control group has no statistical significance (Table 5).
Table 5.
Comparison of lesion of experimental group and control group.
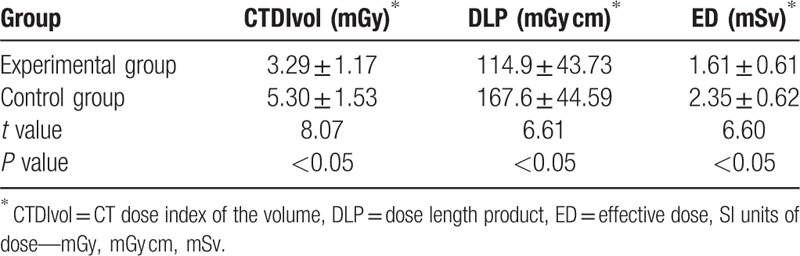
3.6. Comparison of radiation dose
In the experimental group, 48 patients were subject to 80-kV tube voltage scanning and 12 were subject to 100-kV tube voltage scanning (Table 6). In the control group, a tube voltage of 120 kV was used for all patients. Compared with that of the control group, the CTDIvol of the experimental group was 2.01 mGy (37.92%) less; the DLP was ∼52.70 mGy cm (31.44%) less; and the ED was ∼0.74 mSv (31.49%) less. All the differences are statistically significant.
Table 6.
Comparison of radiation dose.
4. Discussion
Although the radiation dose received by a patient in one CT scan is negligible, a cancer risk may exist for frequent scanning or large dosage.[5] In 1990, Naidich et al[6] first proposed the concept of low-dose CT, that is, reduce the radiation dose and radiation hazard, but still obtain the same image quality. Currently, dose-reduction includes the use of real-time dynamic exposure dose adjustment tube current, fixed low tube voltage, fix low tube current, and big pitch heart switch control technology, which lower the radiation dose in different levels.[7–9] CARE kV technology and SAFIRE iterative reconstruction—new methods to reduce radiation dose—are breaking new ground for radiation dose control.
CARE kV technology can automatically lower the radiation dose by setting conditions corresponding to the areas and purpose of different settings, which in turn can be used to set the standard quality reference voltage according to the image quality. CARE kV technology can automatically calculate the reference values and variation curve for different tube voltages according to the automatically defined body type, calculate the CTDIvol, compare, vary the tube voltage from low to high, and chose the lowest voltage scanning if CT ball pipe system hardware is allowed.[10] To guarantee and improve the image quality, a constant or increased CNR as the standard in CARE kV technology must be used to lower the tube voltage and increase the tube current simultaneously. Reduction of the tube voltage will result in an increased photoelectric effect of x-rays on patients, which will increase the absorption by organs with different densities, especially tissues with a high atomic number will increase the contrast of blood vessels and the CT values of image, significantly reduce the radiation dose, and improve the image quality.[11] Winklehne et al[10] scanned the head and chest of which body mass index (BMI) in the same level using CARE kV scanning technology. Their results showed that the contrast of the image increased by 21%, the CNR increased by 17.3% without the increase of image noise of background. Meanwhile, the radiation dose reduced by 58% and 25.3%. Although lowering the tube voltage can significantly reduce the radiation dose, a low tube voltage reduces x-ray penetration; hence, fewer photons reach the detector, which results in increased image noise. In order to reduce the image artifacts caused by noise, which can affect the image density resolution, this study combined CARE kV scanning technology with the SAFIRE iterative reconstruction technique. SAFIRE iterative reconstruction technology uses a support noise model of the original data, which can be applied into the image noise and inhibit and eliminate it in each iteration. The image is a combination of iterative reconstructions; hence, the technique can improve the image quality and reduce the image noise with the potential of reducing the radiation dose.[12,13] This study used CARE kV scanning technology for the chest scanning, but SAFIRE iterative reconstruction techniques were applied to the experimental group. The SD of the experimental groups is lower than that of the control group and the SNR is higher than that of the control group, indicating that the SAFIRE iterative reconstruction algorithm can reduce the noise level and improve the SNR simultaneously. Furthermore, the CT value and image quality score of the lesions of the experimental group and control group showed no statistical differences. All the image scores were greater than 4.5 points, which meets the diagnosis requirements. The reason for this is that the lung is a gas-filled organ, which results in a tissue natural contrast, and structural differences and overlapping within intrathoracic tissues lead to density distribution, making it a good anatomical basis for CARE kV chest scanning technology.
The differences in the CTDIvol, DLP, and ED for the experimental group and control group all have statistical significance. The radiation dose with the CTDIvol of the experimental group was ∼2.01 mGy (38%) less than that of the control group. In the experimental group, all 60 patients were subjected to 100-kV scanning, while the control group did not use CARE kV technology and all 70 patients were subjected to 120-kV scanning, further proving that CARE kV scanning technology can significantly reduce the radiation dose.
In conclusion, in chest CT scanning of health examination patients, CARE kV scanning technology alone will cause increased noise and reduced SNR, and scanning dose reduction without improving the algorithm may lead to diagnostic information loss and enhance increase the risk of incorrect diagnosis. However, SAFIRE iterative reconstruction alone can result in higher quality images with the potential of reducing the radiation dose, even though the reduction it limited. Hence, for chest CT scanning, CARE kV technology combined with SAFIRE iterative reconstruction technology can significantly reduce the radiation dose and improve the image quality, which has potential clinical application.
However, this study has some limitations. For example, no measurement and analysis of the detailed morphology of lesions and CT value were performed. In addition, the results were not classified according to the features of the lesions. Finally, group studies on the relationship between the BMI and voltage were not included, which needs to be further investigated.
Footnotes
Abbreviations: ALARA = as low as reasonably achievable, BMI = body mass index, CNR = contrast-to-noise ratio, CT = computed tomography, CTDIvol = CT dose index of the volume, DLP = dose length product, ED = effective dose, ICRP = International Commission on Radiological Protection, SAFIRE = sinogram-affirmed iterative reconstruction, SNR = signal-to-noise ratio.
BY and Z-LL contributed equally to this work.
Sources of funding: Medical Imaging Department, the First Affiliated Hospital, Kunming Medical University, key subjects for medical imaging
The authors have no conflicts of interest to disclose.
References
- [1].Slovis TL. The ALARA concept in pediatric CT: myth or reality. J Radiol 2002;223:5–6. [DOI] [PubMed] [Google Scholar]
- [2].Price RR, Axel L, Morgan T, et al. Quality assurance methods and phantoms for magnetic resonance imaging: report of AAPM nuclear magnetic resonance task group no. 1. Med Phys 1990;17:287–95. [DOI] [PubMed] [Google Scholar]
- [3].Behrendt FF, Schmidt B, Plumhans C, et al. Image fusion in dual energy computed tomography: effect on contrast enhancement, signal-to-noise ratio and image quality in computed tomography angiography. Invest Radiol 2009;44:1–6. [DOI] [PubMed] [Google Scholar]
- [4].Menzel HG, Schibilla H, Teunen D. European Guidelines on Quality Criteria for Computed Tomography. 2000;Luxembourg: European Commission, 16262. [DOI] [PubMed] [Google Scholar]
- [5].Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med 2007;357:2277–84. [DOI] [PubMed] [Google Scholar]
- [6].Naidich DP, Marshall CH, Gribbin C, et al. Low-dose CT of the lungs: preliminary observation. Radiology 1990;175:729–31. [DOI] [PubMed] [Google Scholar]
- [7].Mulkens TH, Bellinck P, Baeyaert M, et al. Use of an automatic exposure control mechanism for dose optimization in multi-detector row CT examinations: clinical evaluation 1. Radiology 2005;237:213–23. [DOI] [PubMed] [Google Scholar]
- [8].Lee CH, Goo JM, Ye HJ, et al. Radiation dose modulation techniques in the multidetector CT era: from basics to practice. Radiographics 2008;28:1451–9. [DOI] [PubMed] [Google Scholar]
- [9].McCollough CH, Bruesewitz MR, Kofler JM., Jr CT dose reduction and dose management tools: overview of available potions. Radiographics 2006;26:503–12. [DOI] [PubMed] [Google Scholar]
- [10].Winklehner A, Goetti R, Baumueller S, et al. Automated attenuation-based tube potential selection for thoracoabdominal computed tomography angiography: improved dose effectiveness. Invest Radiol 2011;46:767–73. [DOI] [PubMed] [Google Scholar]
- [11].Qiong LI, Hong YU, et al. The effect of iterative reconstruction on image quality of contrast-enhanced chest CT with low tube voltage settings. J Pract Radiol 2012;28:1615–8. [Google Scholar]
- [12].Gosling O, Loader R, Venables P, et al. A comparison of radiation doses between state-of-the-art multislice CT coronary angiography with iterative reconstruction, multislice CT coronary angiography with standard filtered back-projection and invasive diagnostic coronary angiography. Heart 2010;96:922–6. [DOI] [PubMed] [Google Scholar]
- [13].Prakash P, Kalra MK, Ackman JB, et al. Diffuse lung disease: CT of the chest with adaptive statistical iterative reconstruction technique 1. Radiology 2010;256:261–9. [DOI] [PubMed] [Google Scholar]


