Supplemental Digital Content is available in the text
Keywords: all-arthroscopic, clinical trial, mini-open, rotator cuff repair, shoulder
Abstract
Background:
The aim of the study was to compare the clinical outcomes of patients undergoing all-arthroscopic (AA) or mini-open (MO) rotator cuff repair.
Methods:
The present study evaluated 50 patients who had undergone AA repair and 50 patients who had undergone MO repair with a minimum 1-year follow-up. Every patient was asked to complete the Disabilities of the Arm, Shoulder and Hand (DASH) and visual analog scale (VAS) questionnaires. Constant–Murley score (CMS) and active ranges, forward flexion and external rotation, were also evaluated and documented. One year after surgery, ultrasound evaluation was done to determine the integrity of the rotator cuff for each patient.
Results:
The average age of enrolled patients at the time of surgery was 53.0 years (range, 40–59 years), and average follow-up was 16.6 months (range, 12–24 months). At 2 weeks, the range of forward flexion in the AA group was larger than that in the MO group (136.5 ± 10.2 vs 132.5 ± 7.7, P = 0.03). On postoperative day 1, the VAS in the MO group was significantly higher than that in the AA group (6.5 ± 0.6 vs 6.1 ± 0.6, P < 0.01). At 1 month, the difference in VAS between both groups reappeared (2.9 ± 0.6 vs 2.6 ± 0.6, P = 0.03). At 1 month, the CMS score of patients in the AA group was higher than that in the MO group (52.8 ± 3.6 vs 50.9 ± 5.0, P = 0.03). At 3 and 6 months, the DASH score of patients in the AA group was lower than that in the MO group (43.8 ± 8.2 vs 47.8 ± 4.4, P < 0.01 and 38.6 ± 4.3 vs 42.7 ± 9.9, P < 0.01, respectively). Mean operative time was longer in the AA group compared with that in the MO group (71.9 ± 17.6 vs 64.7 ± 12.7 minutes, P < 0.01). Five patients (10.0%) in the AA group and 4 patients (8.2%) in the MO group had rotator cuff retear, and 6 patients (12.0%) in the AA group and 8 patients (16.3%) in the MO group had adhesive capsulitis by the end of follow-up. There is no significant difference between the 2 groups in the incidence of complications. We also found that joint exercising at least 3 times per week was associated with better short- and long-term joint function recovery.
Conclusions:
The AA approach was associated with less pain and lower DASH score as well as higher CMS score in the early recovery period. No difference was found between the 2 groups in primary and secondary outcomes in the long term, or incidence of complications such as adhesive capsulitis and rotator cuff retear. In conclusion, we consider that the AA procedure has better recovery at short-term follow-ups, while both techniques are equivalent regarding long-term outcomes.
1. Introduction
Repair of the rotator cuff was first described by Codman over a century ago.[1] One of the current procedures, mini-open (MO) repair, has been regarded as the gold standard for rotator cuff tear repair for decades; it has been proved to achieve good to excellent results in 90% of patients.[2–5] It has been the first choice for many surgeons due to its stronger suture fixation and shorter learning curve.[6–8] Over the past decade with advances in surgical instrument and operative technique, there has been a shift from MO to all-arthroscopic (AA) technique in rotator cuff repair surgery. Faster recovery and better cosmetic results have led many surgeons to prefer the arthroscopic approach.[9,10] However, the most effective method of repair is yet to be determined given that both techniques are associated with good clinical outcomes.[5,11,12] According to previous comparisons of the 2 approaches, the MO procedure is associated with smaller skin incisions, less soft tissue dissection, and decreased chance of deltoid muscle detachment,[7–9,13–15] while the AA procedure is associated with decreased postoperative pain, low deltoid morbidity, shorter hospital stay, and faster rehabilitation.[16,17]
Several systematic reviews and meta-analyses conducted years earlier found no significant differences between arthroscopic and MO repairs.[6,18] However, most of those studies included were of low quality in that samples were not randomized and follow-up was retrospective in nature. Limited number of randomized controlled trials have been published, some of which have shown a shorter surgery time and greater range of motion at the end of follow-up,[19,20] as well as reduced pain during the midterm period of postoperative rehabilitation. Nevertheless, there are still insufficient studies evaluating short- and long-term outcomes of both approaches. We hypothesize that the AA procedure has better clinical outcomes than the MO procedure. To evaluate the early and late clinical outcomes of AA versus MO repair technique in patients with full-thickness rotator cuff tears, we designed a study involving 100 patients with a minimum 1-year follow-up.
2. Methods
2.1. Study design
A randomized clinical trial in patients undergoing rotator cuff repair using AA or MO technique was conducted in a large tertiary teaching hospital. Patients visiting our outpatient clinic with shoulder pain were evaluated for the presence of a full-thickness rotator cuff tear on the basis of history, clinical examination, standard anteroposterior and scapular Y-view radiographs of the shoulder, and magnetic resonance arthrography in a 1.5-T scanner.
Inclusion criteria were patients with age between 40 and 60 years and those who had a supraspinatus and/or infraspinatus tendon tear with stage <3 fatty muscle infiltration based on magnetic resonance imaging findings; for better follow-up compliance, we included only the patients who have the medical or life insurance coverage for at least 3 years.
Exclusion criteria were patients with glenohumeral instability or restricted glenohumeral movement (forward flexion [FF] <90°) as a result of adhesive capsulitis, glenohumeral arthritis, rheumatoid arthritis, or trauma; a history of shoulder surgery; diabetes and other severe metabolic comorbidities; or a high risk of noncompliance, such as insufficient insurance coverage.
From March 2013 to June 2014, all patients fulfilling the inclusion criteria were enrolled in the study with an intention-to-treat analysis. After being placed under general anesthesia in the operating room, patients were assigned to an AA or MO repair procedure using a computer-generated randomization sequence; to protect the integrity of the randomization scheme, an independent biostatistician ensured that the block sizes were confidential. Patients were divided into 2 gender subgroups, and then randomization employed variable permuted block sizes in a 1:1 ratio. This study was approved by the medical ethics committee of our hospital. An informed consent form was signed by all patients before participating in the study. Patients were evaluated using the simplified Chinese version of the Disabilities of the Arm, Shoulder and Hand (DASH)[21,22] and Constant–Murley score (CMS)[23] after their admission, as well as 1, 3, 6, and 12 months postoperatively. CMS is the recommended scoring system for shoulder disorders developed by the European Society for Surgery of the Shoulder and the Elbow. It includes rating of pain, daily activities, motility, and strength, ranging from 0 to 100.[24]
2.2. Surgical technique
The surgeries were performed by 2 senior shoulder surgeons experienced in both the AA and MO repair techniques.
For the AA group, the arthroscope was placed in the subacromial space through a standard posterior portal; lateral and posterolateral working portals were subsequently established. The tear was adequately mobilized and repaired by attaching the supraspinatus to the prepared greater tuberosity using either the single-row or the double-row repair technique with a suture anchor. The number of anchors and sutures used depended on the tear size and pattern, which was reevaluated during the surgeries.
For the MO group, the approach was initiated with a 5-cm lateral incision starting at the anterior border of the acromion. The fibers of the deltoid muscle were split by blunt dissection, and maximal visualization was established using a soft tissue retractor. Care was taken not to damage the axillary nerve running close to the distal edge of the incision and to minimize detachment of deltoid muscle fibers from the lateral part of the acromion. Partial bursectomy was performed using dissection scissors. The rest of the procedure was basically the same for both techniques.
2.3. Postoperative pain management
For postoperative pain control, immediate-release oxycodone, acetaminophen, and a cyclooxygenase-2 selective inhibitor were administered orally until postoperative day 2. From postoperative days 3 to 5, a tablet containing a combination of 37.5 mg of tramadol and 325 mg of acetaminophen was prescribed, along with a cyclooxygenase-2 inhibitor. For additional postoperative pain control beyond that provided by the authors’ regular regimen, intramuscular diclofenac was added if required.
Pain was rated using a self-rated visual analog scale (VAS) ranging from 0 (no pain) to 10 (unbearable pain) preoperatively[25]; postoperative days 1 and 3; at 1 and 2 weeks; and 1, 3, 6, and 12 months postoperatively. Range of shoulder motion was checked preoperatively and postoperatively at time points same as those in VAS score, using a continuous passive motion machine.
2.4. Postoperative rehabilitation
The postoperative rehabilitation protocol was the same for both groups. Wearing an abduction brace, patients engaged in pendulum and continuous passive motion machine exercises until postoperative day 5, and then passive range-of-motion exercises were started. Active range-of-motion exercises were started at 6 weeks postoperatively, muscle-strengthening exercises were started at 3 months, and occupational or sports activities were started at 6 months.
2.5. Patient outcomes
Preoperative (<2 months prior to surgery) and postoperative (day 3, weeks 1 and 2, and months 1, 3, 6, and 12) outcome measurements were collected by the research coordinator. The primary outcome measure was the DASH, CMS, active FF and external rotation (ER), and the VAS pain score. Secondary outcome measures were length of hospitalization, operation time, hospital cost, and training times per week. Twelve months postoperatively, a standardized ultrasonogram of the operated shoulder was obtained by an independent, experienced musculoskeletal ultrasonographer to evaluate the integrity of the repaired tendons.[26] As no ultrasound-based classification system for rotator cuff repairs is available, the repairs were scored as intact or retear. As a result of the obvious incision pattern, the patient and the examiner could not be blinded postoperatively.
2.6. Statistical analysis
With a power of 0.8 (1 − β) and a significance level (α) of 0.05, each treatment arm required 45 patients. Given the anticipated dropout rate of 10%, 100 patients were included in the study. Each arm contains 25 male and 25 female patients. Measured values are reported as means with standard deviations; estimates are presented as means with 95% confidence intervals. Postoperative outcome measures were analyzed according to the intention-to-treat principle. Statistical analysis was performed using SPSS Statistical Software 18.0 (SPSS Inc, Chicago, IL). Frequency and descriptive statistics were analyzed to examine baseline characteristics, and t and χ2 tests were used to determine the significance of differences between the 2 groups. Statistical significance was set at a P value <0.05. We used independent t tests approach as Dupont and Plummer[27] described to perform power analysis variable used. Take DASH, for example, in a previous study the response within each subject group was normally distributed with standard deviation 4. If the true difference in the experimental and control means is 3, we will be able to reject the null hypothesis that the population means of the experimental and control groups are equal with a probability (power) of 0.958.
3. Results
3.1. Patient characteristics
Figure 1 is a flow diagram of the enrollment, allocation, and follow-up of the patients. Overall, the average age of the 99 patients at the time of surgery was 53.0 years (range, 40–59 years), and the average follow-up was 16.6 months (range, 12.0–24.0 months). Patient characteristics were comparable between the 2 groups and are summarized in Table 1. Biceps tenotomy was performed in 12 cases: 5 cases in the AA group and 7 cases in the MO group. Acromioplasty was performed in 35 cases: 19 in the AA group and 16 in the MO group.
Figure 1.
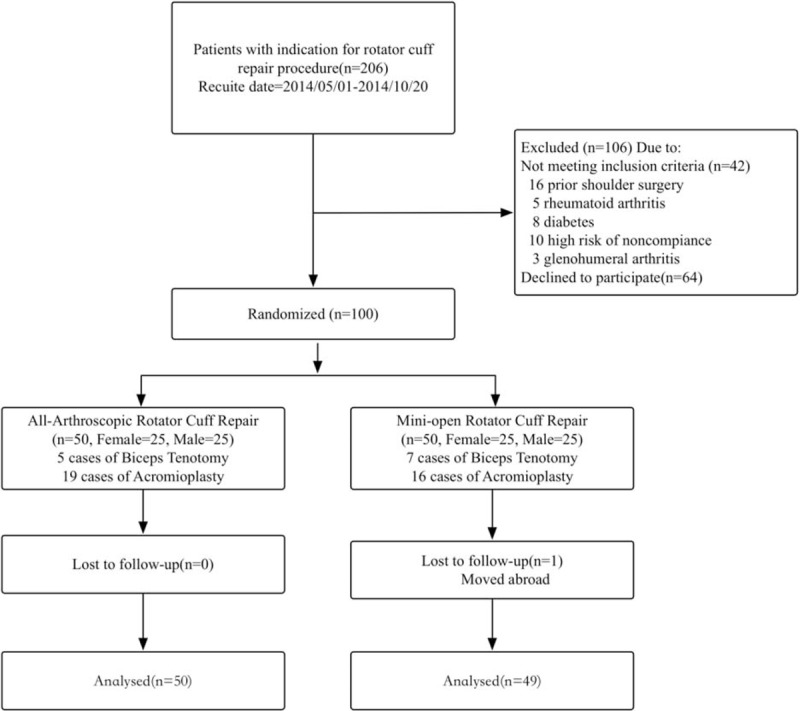
Flow diagram of the enrollment, allocation, and follow-up of the patients.
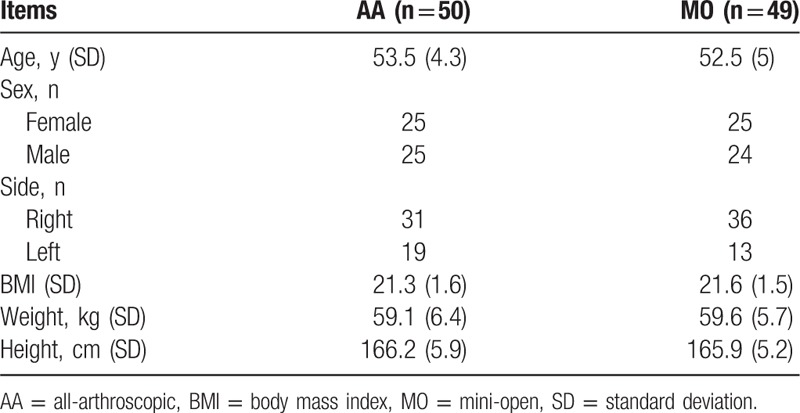
Table 1.
Patient characteristics for group AA and group MO repairs.
3.2. Primary outcomes
3.2.1. DASH score
The mean preoperative DASH scores were 50.9 ± 8.6 in the AA group and 52.6 ± 7.5 in the MO group, with no difference between the 2 groups. There is a trend toward decreasing DASH score at different postoperative time points. At 3 and 6 months postoperatively, the DASH score in the AA group was significantly lower than that in the MO group (Table 2; Fig. 2).
Table 2.
Results of primary outcome measures (mean, SD).
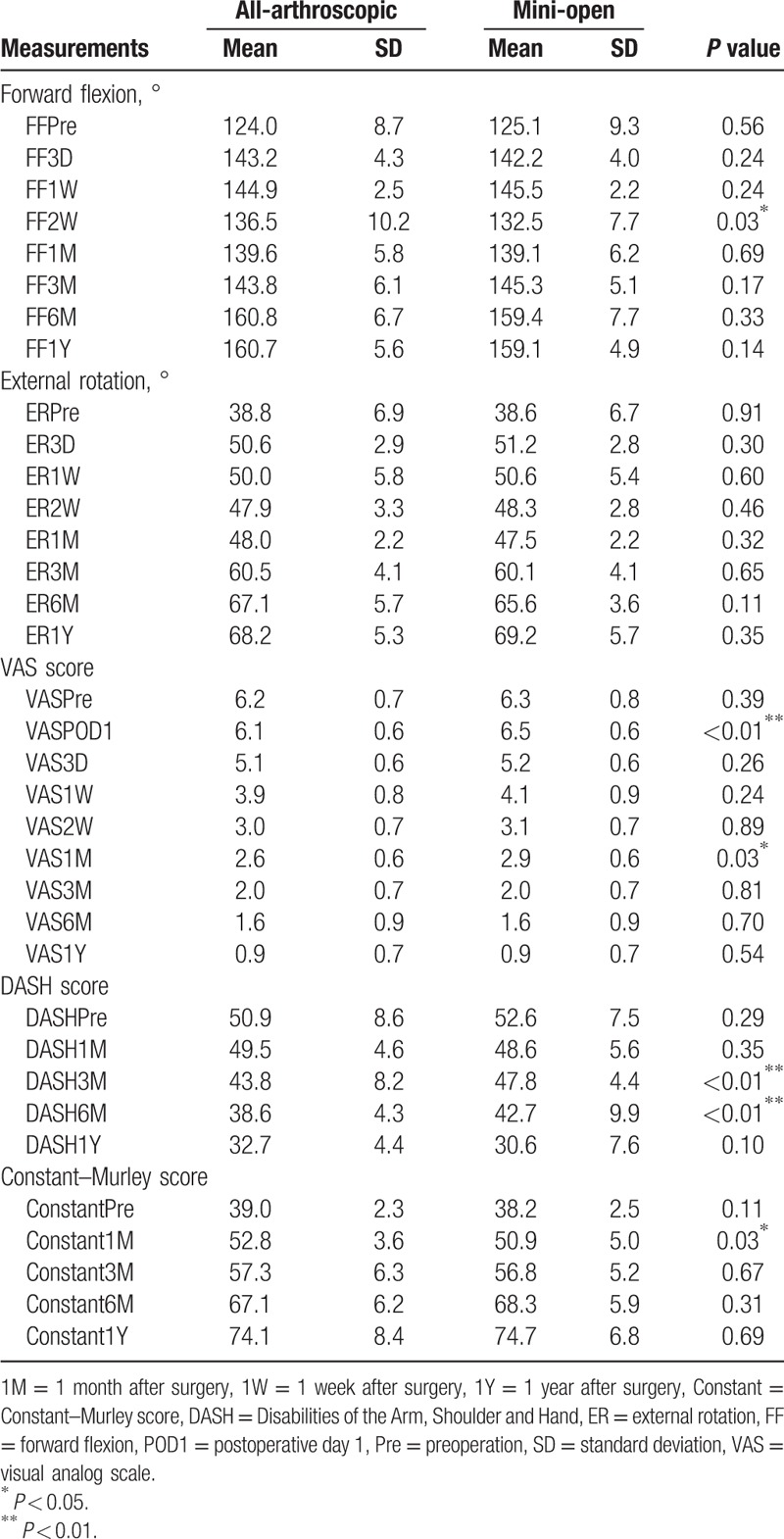
Figure 2.
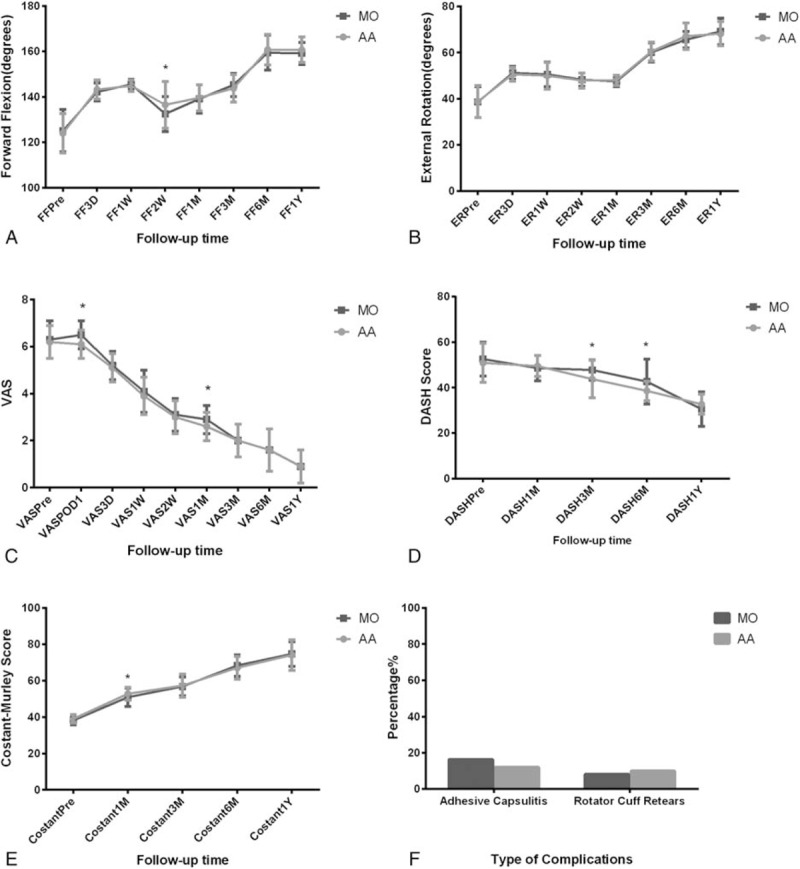
Comparisons of clinical outcomes between all-arthroscopic and mini-open groups: (A and B) forward flexion and external rotation of the 2 groups after surgery; (C–E) VAS, DASH, and CMS of the 2 groups after surgery; (F) morbidity of the 2 complications. AA = all-arthroscopic, CMS = Constant–Murley score, DASH = Disabilities of the Arm, Shoulder and Hand, MO = mini-open, VAS = visual analog scale.
3.2.2. Constant–Murley score
The CMS in both groups of patients increased postoperatively, and this trend remained along with the length of follow-up. At 1 month, the score of patients in the AA group was higher than that in the MO group (52.8 ± 3.6 vs 50.9 ± 5.0, P = 0.03). No difference in the score was found at other time points during follow-up between the 2 groups (Table 2; Fig. 2).
3.2.3. Range of motion
The range of motion, that is, FF and ER, of the shoulder joint in both groups was improved postoperatively. Within the 1-year period, the range of motion showed an increasing trend with time. At 2 weeks, the range of FF in the AA group was larger than that in the MO group (136.5 ± 10.2 vs 132.5 ± 7.7, P = 0.03). No difference in the score was found at other time points during follow-up between the 2 groups (Table 2; Fig. 2).
3.2.4. VAS score
The preoperative VAS scores were comparable between AA and MO groups. On postoperative day 1, the VAS score in the MO group was significantly higher than that in the AA group (6.5 ± 0.6 vs 6.1 ± 0.6, P < 0.01). At 1 month, the difference between both groups reappeared (2.9 ± 0.6 vs 2.6 ± 0.6, P = 0.03). No difference in the score was found at other time points during follow-up between the 2 groups (Table 2; Fig. 2).
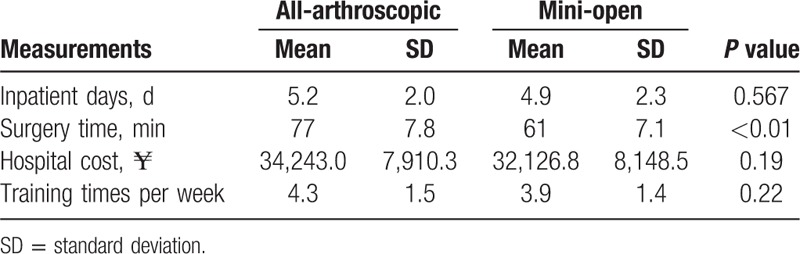
3.3. Secondary outcomes
Mean operative time was longer in the AA group compared with that in the MO group (71.9 ± 17.6 vs 64.7 ± 12.7 minutes, P < 0.01). No significant difference between the 2 groups was found in other secondary outcome measures such as length of hospitalization, hospital cost, and training time per week (Table 3). Five patients (10.0%) in the AA group and 4 patients (8.2%) in the MO group had rotator cuff retear, and 6 patients (12.0%) in the AA group and 8 patients (16.3%) in the MO group had adhesive capsulitis in the end. But there was no significant difference in the complications between the 2 groups (Fig. 2). In addition, we also identified the correlation between rehabilitation training frequency and clinical outcomes.
Table 3.
Results of secondary outcome measures (mean, SD).
4. Discussion
In the present study, primary outcomes including DASH, CMS, VAS score, FF, and ER, and secondary outcomes involving hospital charges, in-hospital days, surgery time, and complication rates were evaluated and compared between the 2 approaches. We found that after the short time rehabilitation, patients in the AA group had less postoperative VAS score and higher DASH and CMS scores in some periods (Fig. 2), amid higher (about ¥2000 higher) hospital costs. The present study also collected the follow-up outcomes of previously published studies that compared 2 different treatment choices for rotator cuff tears, which are shown in Table 4.
Table 4.
Studies comparing all-arthroscopy and mini-open repair of rotator cuff tears.
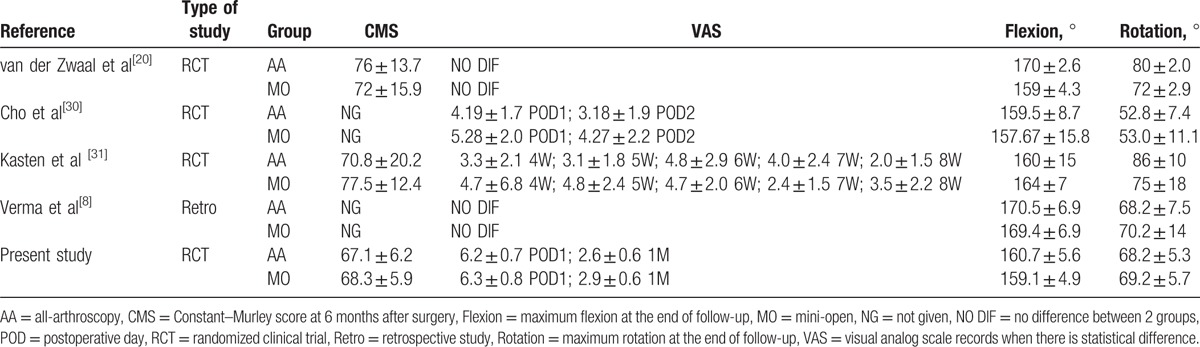
Shoulder arthroscopy is an increasingly popular modality for rotator cuff repair in China as arthroscopic techniques and surgeons’ experience continue to improve.[28,29] MO repair is an alternative surgery pattern to combine the advantages of arthroscopic and open repair without taking down the deltoid origin. The arthroscopic technique is believed to cause less pain and allows for better recovery in the earlier postoperative period, which can reduce the patients’ off-work period and thereby reduce the disease-associated costs. With less pain during shoulder activity, patients were more willing to do rehabilitation exercises that help them recover joint functions. Some researchers[2,20,30] demonstrated that patients who opted for the AA procedure obtained faster rehabilitation in terms of function score, VAS pain, and range of motion compared with patients in the MO group. Our study also observed that the AA group had better VAS score on the first postoperative day and 1 month later, as well as range of FF after 2 weeks postoperatively, while some studies[7,8,14,15] did not identify significant difference on rehabilitation or pain between the 2 groups (Table 4).
In our study, the DASH and CMS were used to reflect the satisfaction of the patients. We found that at months 3 and 6, the DASH of patients in the AA group was higher than that in the MO group (43.8 ± 8.2 vs 47.8 ± 4.4, P < 0.01 and 38.6 ± 4.3 vs 42.7 ± 9.9, P < 0.01, respectively), and at 1 month, the CMS of patients in the AA group was higher than that in the MO group (52.8 ± 3.6 vs 50.9 ± 5.0, P = 0.03). Similarly, several studies[1,8,14,16,32] investigating DASH, CMS, or other scales evaluating shoulder function showed higher scores in the arthroscopy group than those in the MO repair group in short and long terms (Table 4). During the study, we found that this difference not only is due to less pain and better range of motion but may also be associated with the frequency of rehabilitation training. Our study showed that the training times per week might affect the CMS. Better functional recovery was achieved in patients with more frequent shoulder exercises. Patients who had at least 3 times of rehabilitation training had better CMS at 1 year (Supplemental Tables), while other factors, tear size and acromioplasty, had no correlation with CMS or DASH via univariate analysis of variance.
The early rehabilitation of patients who had all-arthroscopy may result from less deltoid muscle tissue injury and less detachment of muscle fiber from the acromion.[33] But several studies report that with a long-term follow-up, there were no statistically significant differences in postoperative functional or VAS pain between groups.[11,18,20,34] In our study, the statistical differences were observed only on postoperative day 1 and 1 month after surgery.
Repair of the rotator cuff via all-arthroscopy needs highly skilled technics and requires a long learning curve for surgeons to become specialists in this field. Besides, as only the implantable suture anchor devices can be used in AA surgery, it also results in more time for surgeons to complete surgery. Because the MO method has various repair choices from bone tunnels to implantable suture anchors, it is apparently easy to learn and consumes less operative time. Our experience showed that the MO procedure takes approximately 15 minutes less than the AA procedure. Similarly, van der Zwaal et al[20] and Cho et al[30] reported that all-arthroscopy surgeries need more time than MO ones on average, but neither of these studies reported any significant difference about surgery time.
Adhesive capsulitis and rotator cuff retears are the 2 most common complications. In terms of postoperative rehabilitation, all-arthroscopy has advantages over MO repair with less soft tissue injury. Although the deltoid origin is preserved, MO approach still requires a split in the deltoid fibers extending into the subdeltoid bursa to expose the surgery area, which may lead to subacromial scarring and stiffness.[35] In China, a few patients take the help of postoperative rehabilitation advices from special physical therapists. Technically speaking, patients undergoing MO surgery would face a higher rate of adhesive capsulitis, whereas there is no significant difference in rates of side effects in our study or others.
No difference in the incidence of recurrent tears was found in our study comparing the 2 groups. Some studies reported that patients with larger tears had a higher incidence of persistent defects, and Verma found that retear rate was higher for open group for tears <3 cm, and retear rate was higher for arthroscopic groups for tears >3 cm with no statistically significant difference. Some important factors exist influencing the incidence of rotator cuff retear, including tear size, preoperative duration of symptoms, degeneration of cuff, fixation technique, and the hardware used.[28]
5. Limitations
There are several limitations of this study. First, the sample of the present study was not large enough to get statistical difference of some outcomes. For instance, each group should include 3000 subjects for a power of 80% (α = 0.05) to be attained if the difference in retearing proportions of 3% can be observed in the study. Second, the study was not double-blinded for the obvious difference in surgical incision between both groups of patients. LF and YZ were responsible for collecting and analyzing data separately to minimize the bias. Third, no standardized rehabilitation program was used for all patients. Patients’ self-reported training times per week were recorded during each follow-up, which is associated with possible recall bias. Fourth, in the study, we analyzed several factors including surgery methods, tear size, and training frequency that are relevant to CMS and DASH score. But there are still some confounding factors incompletely recorded such as single-row or double-row repair techniques, acromioplasty, type of rehabilitation training, and characteristics of patients, which need to be further evaluated. Taken together, further research with a larger number of patients and standard rehabilitation procedure is still necessary.
6. Conclusions
In the present study, we found that the AA approach was associated with less pain, lower DASH score, and higher CMS in the early recovery period. No difference was found between the 2 groups in primary and secondary outcomes in the long term, or incidence of complications such as adhesive capsulitis and rotator cuff retear. Besides, we consider that the AA procedure has better recovery at short-term follow-ups, while both techniques are equivalent regarding the long-term outcomes.
Supplementary Material
Footnotes
Abbreviations: AA = all-arthroscopic, CMS = Constant–Murley score, DASH = Disabilities of the Arm, Shoulder and Hand, ER = external rotation, FF = forward flexion, MO = mini-open, VAS = visual analog scale.
JL, LF, and YZ contributed equally to the work.
The authors have no funding and conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Codman EA. Complete rupture of the supraspinatus tendon. Operative treatment with report of two successful cases. 1911. J Shoulder Elbow Surg 2011;20:347–9. [DOI] [PubMed] [Google Scholar]
- [2].Baker CL, Liu SH. Comparison of open and arthroscopically assisted rotator cuff repairs. Am J Sports Med 1995;23:99–104. [DOI] [PubMed] [Google Scholar]
- [3].Paulos LE, Kody MH. Arthroscopically enhanced “miniapproach” to rotator cuff repair. Am J Sports Med 1994;22:19–25. [DOI] [PubMed] [Google Scholar]
- [4].Park JY, Levine WN, Marra G, et al. Portal-extension approach for the repair of small and medium rotator cuff tears. Am J Sports Med 2000;28:312–6. [DOI] [PubMed] [Google Scholar]
- [5].Shinners TJ, Noordsij PG, Orwin JF. Arthroscopically assisted mini-open rotator cuff repair. Arthroscopy 2002;18:21–6. [DOI] [PubMed] [Google Scholar]
- [6].Nho SJ, Shindle MK, Sherman SL, et al. Systematic review of arthroscopic rotator cuff repair and mini-open rotator cuff repair. J Bone Joint Surg Am 2007;89(suppl 3):127–36. [DOI] [PubMed] [Google Scholar]
- [7].Sauerbrey AM, Getz CL, Piancastelli M, et al. Arthroscopic versus mini-open rotator cuff repair: a comparison of clinical outcome. Arthroscopy 2005;21:1415–20. [DOI] [PubMed] [Google Scholar]
- [8].Verma NN, Dunn W, Adler RS, et al. All-arthroscopic versus mini-open rotator cuff repair: a retrospective review with minimum 2-year follow-up. Arthroscopy 2006;22:587–94. [DOI] [PubMed] [Google Scholar]
- [9].Kang L, Henn RF, Tashjian RZ, et al. Early outcome of arthroscopic rotator cuff repair: a matched comparison with mini-open rotator cuff repair. Arthroscopy 2007;23:573–82. 582.e571–582.e572. [DOI] [PubMed] [Google Scholar]
- [10].Pearsall AW, 4th, Ibrahim KA, Madanagopal SG. The results of arthroscopic versus mini-open repair for rotator cuff tears at mid-term follow-up. J Orthop Surg Res 2007;2:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Kim SH, Ha KI, Park JH, et al. Arthroscopic versus mini-open salvage repair of the rotator cuff tear: outcome analysis at 2 to 6 years’ follow-up. Arthroscopy 2003;19:746–54. [DOI] [PubMed] [Google Scholar]
- [12].Burkhart SS, Danaceau SM, Pearce CE., Jr Arthroscopic rotator cuff repair: analysis of results by tear size and by repair technique-margin convergence versus direct tendon-to-bone repair. Arthroscopy 2001;17:905–12. [DOI] [PubMed] [Google Scholar]
- [13].Severud EL, Ruotolo C, Abbott DD, et al. All-arthroscopic versus mini-open rotator cuff repair: a long-term retrospective outcome comparison. Arthroscopy 2003;19:234–8. [DOI] [PubMed] [Google Scholar]
- [14].Youm T, Murray DH, Kubiak EN, et al. Arthroscopic versus mini-open rotator cuff repair: a comparison of clinical outcomes and patient satisfaction. J Shoulder Elbow Surg 2005;14:455–9. [DOI] [PubMed] [Google Scholar]
- [15].Warner JJ, Tetreault P, Lehtinen J, et al. Arthroscopic versus mini-open rotator cuff repair: a cohort comparison study. Arthroscopy 2005;21:328–32. [DOI] [PubMed] [Google Scholar]
- [16].Buess E, Steuber KU, Waibl B. Open versus arthroscopic rotator cuff repair: a comparative view of 96 cases. Arthroscopy 2005;21:597–604. [DOI] [PubMed] [Google Scholar]
- [17].Gartsman GM, Brinker MR, Khan M. Early effectiveness of arthroscopic repair for full-thickness tears of the rotator cuff: an outcome analysis. J Bone Joint Surg Am 1998;80:33–40. [PubMed] [Google Scholar]
- [18].Morse K, Davis AD, Afra R, et al. Arthroscopic versus mini-open rotator cuff repair: a comprehensive review and meta-analysis. Am J Sports Med 2008;36:1824–8. [DOI] [PubMed] [Google Scholar]
- [19].Shinoda T, Shibata Y, Izaki T, et al. A comparative study of surgical invasion in arthroscopic and open rotator cuff repair. J Shoulder Elbow Surg 2009;18:596–9. [DOI] [PubMed] [Google Scholar]
- [20].van der Zwaal P, Thomassen BJ, Nieuwenhuijse MJ, et al. Clinical outcome in all-arthroscopic versus mini-open rotator cuff repair in small to medium-sized tears: a randomized controlled trial in 100 patients with 1-year follow-up. Arthroscopy 2013;29:266–73. [DOI] [PubMed] [Google Scholar]
- [21].Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med 1996;29:602–8. [DOI] [PubMed] [Google Scholar]
- [22].Chen ZB, Hong GX, Wang FB. Instruction DASH (Disability of Arm Shoulder and Hand). Chinese Journal of Reparative and Reconstructive Surgery 2004;18:520–1. [Google Scholar]
- [23].Ge YS. The Research and Development of a Shoulder Functional Scale System in Chinese [Postgraduate]. Shanghai, China: Fudan University; 2007. [Google Scholar]
- [24].Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 1987. 160–4. [PubMed] [Google Scholar]
- [25].Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health 1990;13:227–36. [DOI] [PubMed] [Google Scholar]
- [26].Godinho GG, Franca Fde O, Alves FJ, et al. Evaluation of anatomical integrity using ultrasound examination, and functional integrity using the Constant & Murley score, of the rotator cuff following arthroscopic repair. Rev Bras Ortop 2010;45:174–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Dupont WD, Plummer WD., Jr Power and sample size calculations. A review and computer program. Control Clin trials 1990;11:116–28. [DOI] [PubMed] [Google Scholar]
- [28].Shan L, Fu D, Chen K, et al. All-arthroscopic versus mini-open repair of small to large sized rotator cuff tears: a meta-analysis of clinical outcomes. PLoS One 2014;9:e94421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Shen C, Tang ZH, Hu JZ, et al. Does immobilization after arthroscopic rotator cuff repair increase tendon healing? A systematic review and meta-analysis. Arch Orthop Trauma Surg 2014;134:1279–85. [DOI] [PubMed] [Google Scholar]
- [30].Cho CH, Song KS, Jung GH, et al. Early postoperative outcomes between arthroscopic and mini-open repair for rotator cuff tears. Orthopedics 2012;35:e1347–52. [DOI] [PubMed] [Google Scholar]
- [31].Kasten P, Keil C, Grieser T, et al. Prospective randomised comparison of arthroscopic versus mini-open rotator cuff repair of the supraspinatus tendon. Int Orthop 2011;35:1663–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Callegari E, Elamin BK, Giannone F, et al. Liver tumorigenicity promoted by microRNA-221 in a mouse transgenic model. Hepatology 2012;56:1025–33. [DOI] [PubMed] [Google Scholar]
- [33].Wright RW, Baumgarten KM. Shoulder outcomes measures. J Am Acad Orthop Surg 2010;18:436–44. [DOI] [PubMed] [Google Scholar]
- [34].Ji X, Bi C, Wang F, et al. Arthroscopic versus mini-open rotator cuff repair: an up-to-date meta-analysis of randomized controlled trials. Arthroscopy 2015;31:118–24. [DOI] [PubMed] [Google Scholar]
- [35].Mormino MA, Gross RM, McCarthy JA. Captured shoulder: a complication of rotator cuff surgery. Arthroscopy 1996;12:457–61. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


